Abstract
Introduction
There is a lot of interest towards creating therapies and vaccines for Bacillus anthracis, a bacterium which causes anthrax in humans and which spores can be made into potent biological weapons. Systemic injection of lethal factor (LF), edema factor (EF), and protective antigen (PA) in mice produces toxicity and this protocol is commonly used to investigate the efficacy of specific antibodies in passive protection and vaccine studies. Availability of toxins labeled with imagable radioisotopes would allow to demonstrate their tissue distribution after intravenous injection at toxin concentration that are below pharmacologically significant to avoid masking by toxic effects.
Methods
LF, EF and PA were radiolabeled with 188Re and 99mTc and their performance in vitro was evaluated by macrophages and CHO cells toxicity assays and by binding to macrophages. Scintigraphic imaging and biodistribution of IV injected 99mTc- and 123I-labeled toxins was performed in BALB/c mice.
Results
Radiolabeled toxins preserved their biological activity. Scatchard-type analysis of the binding of radiolabeled PA to the J774.16 macrophage-like cells revealed 6.6 × 104 binding sites per cell with a dissociation constant of 6.7 nM. Comparative scintigraphic imaging of mice injected intravenously with either 99mTc- or 123I-labeled PA, EF, and LF toxins demonstrated similar biodistribution patterns with early localization of radioactivity in the liver, spleen, intestines and excretion through kidneys. The finding of renal excretion shortly after IV injection strongly suggests that toxins are rapidly degraded which could contribute to the variability of mouse toxigenic assays. Biodistribution studies confirmed that all three toxins concentrated in the liver and the presence of high levels of radioactivity again implied rapid degradation in vivo.
Conclusions
The availability of 188Re and 99mTc-labeled PA, LF and EF toxins allowed us to confirm the number of PA binding sites per cell, to provide an estimate of the dissociation constant of PA for its receptor, and to demonstrate tissue distribution of toxins in mice after intravenous injection.
Keywords: anthrax, protective antigen, lethal factor, edema factor, 188-Rhenium, scintigraphic imaging
INTRODUCTION
There is a lot of interest towards creating therapies and vaccines for Bacillus anthracis, a bacterium which causes anthrax in humans and which spores can be made into potent biological weapons. We are interested in radiolabeling the components of the tripartite toxin secreted by B. anthracis, namely: protective antigen (PA), named for its ability to elicit protective immunity, lethal factor (LF) which is a zinc-dependent protease that cleaves mitogen-activated protein kinase kinase, and edema factor (EF) - an adenylate cyclase capable of impairing host defenses [1]. Systemic injection of LF, EF, and PA in mice produces toxicity and this protocol is commonly used to investigate the efficacy of specific antibodies in passive protection and vaccine studies [2–5]. Although this assay is not physiological considering the pathogenesis of anthrax, it provides a means to test some aspects of toxin function. Availability of toxins labeled with imagable radioisotopes would allow to demonstrate their tissue distribution after intravenous injection. The important advantage of using radiolabeled toxins would also be the fact that since imaging is performed at toxin concentration that are below pharmacologically significant, these observations would show metabolism patterns not masked by toxic effects. We have recently radiolabeled PA and LF with 188Re in order to study the binding of these toxins to macrophages in vitro in the presence of PA-specific monoclonal antibody [6]. Here we investigate in vitro and vivo behavior of 188Re-or 99mTc-labeled LF, EF, and PA which provide new insights into the biological properties of these toxins.
MATERIALS AND METHODS
Toxins and cells
Recombinant protective PA, LF and EF expressed in E. coli as described [7] were obtained from Wadsworth Laboratories, NYS Department of Health (Albany, NY). Murine J774.16 macrophage-like cells were grown in DMEM supplemented with 10% FCS, 10% NCTC-109 and 1% nonessential amino acids. The J774.16 cell line was originally obtained from Dr. Barry Bloom (Boston, MA) and has been extensively used in our laboratories in phagocytosis assays [8].
Radioisotopes
99mTc in form of sodium pertechnetate Na99mTcO4 was procured from GE Healthcare; 123I in form of sodium 123I-iodide - from MDS Nordion (Canada). 188Re in form of sodium perrhenate Na188ReO4 was eluted from 188W/188Re generator (Oak Ridge National Laboratory, Oak Ridge, TN). Radiolabeling of LF, EF, and PA was performed as described in [6].
Macrophage toxicity assay
To investigate whether labeling with 188Re affected the biological properties of the various toxins, the toxicity of a 188Re-labeled lethal toxin towards macrophages was assessed. Lethal toxin (LeTx) is a mixture of PA and LF. 188Re-labeled lethal (188Re-LeTx) is a mixture of 188Re-PA and LF. MTT (3,(4,5-dimethylthiazol-2-yl)2,5-diphenyltetra-zolium bromide) (Sigma, St. Louis, MO) was dissolved at 5 mg/mL in sterile PBS at room temperature. The solution was sterilized by passage through a 0.22 um filter and stored in a dark bottle at 4°C. The MTT assay involves the oxidation of MTT to an insoluble pigment by live cells. J774.16 macrophage-like cells (6 × 104) were incubated in a 96-well plate with 100 ng of 188Re-LeTx for 4 hours at 37°C. Unlabeled LeTx or only 188Re-PA were used as controls. In a dose response experiment 12.5 – 400 ng of 188Re-LeTx were used. A 25 µL volume of 5 mg/mL stock-solution of MTT was added to each well and after 2 h incubation at 37°C, 100 µL of the extraction buffer (12.5% SDS, 45% DMF) was added and cells were incubated overnight at 37°C. Absorbance was measured at 570 nm (Labsystem Multiskan, Franklin, MA).
CHO cells toxicity assay
In combination with PA, EF (an adenylate cyclase) is activated by calmodulin to catalyze the synthesis of cAMP in host cells [9]. Edema toxin (PA + EF, EdTx) induces an increase in the intracellular cAMP levels in sensitive cells. Chinese hamster ovary (CHO) cells were maintained in DMEM supplemented with 10% heat inactivated fetal bovine serum, 1% nonessential amino acids and 10% NTCC. CHO cells (105) were incubated with various dilutions of 188Re-EdTx (PA and 188Re-EF mixture) for 2 h at 37°C. Total cAMP levels were measured using the cAMP Biotrak enzyme immunoassay (EIA) system as described by the manufacturer’s instructions (Amersham Biosciences, Piscataway, NJ).
Binding of labeled toxins to macrophages
J774.16 cells were washed twice and re-suspended in 1 mL PBS at a density of 2.8 × 106 cells/mL. The binding studies were done in low retention siliconized microcentrifuge tubes (Fischer Scientific, Pittsburgh, PA). The microcentrifuge tubes were blocked overnight with 1% BSA to prevent non-specific binding of protein to the plastic. To determine the PA receptor density in J774.16 cells, 188Re-PA was added to the tubes in the increasing amounts (0.28 – 1.92 nM). The cells were incubated for 1 hr at 4°C and the radioactivity measured using a gamma counter. Macrophages were collected by centrifugation at 1,200 rpm at 4°C for 6 min and radioactivity counts were measured. From the total and bound radioactivity we inferred the amount of toxin binding and used Scatchard-type analysis [10] to calculate the toxin dissociation constant KD and the number of PA-binding receptors per cell.
In another series of experiments, we measured the binding of LF toxin to macrophages incubated with and without PA. The cells were incubated at 4°C for 1 hr with 188Re-LF (0.28 – 1.92 nM), and in some experiments, a large molar excess (20 nM) of unmodified or DTT-treated LF was also added to the cells. The binding of 188Re-LF to normal macrophages was calculated as the ratio of activity in the pellet versus activity in the tube before collecting the cells and was expressed as a percentage. For assessing the binding of LF to macrophage-bound PA, cells were first incubated with increasing amounts (0.28 – 1.92 nM) of "cold" PA for 1 hr at 4°C, followed by addition of equimolar amounts of radiolabeled LF (1:1), with an additional incubation for 1 h at 4°C. Radioactivity was measured and percent binding was calculated as described above.
Scintigraphic imaging and biodistribution of 99mTc- and 123I-labeled toxins
Initially we investigated the in vivo localization of 99mTc-labeled toxins. For these studies, 99mTc was utilized instead of 188Re because it has superior imaging characteristics - the abundance of its 140 keV photons is 89% versus 15% for 155 keV photons emitted by 188Re. Tc and Re metals are chemical analogues which react with proteins in a similar way. Toxins were radiolabeled with 99mTc as described above. All animal studies were carried out in accordance with the guidelines of the Albert Einstein College of Medicine Institute for Animal Studies. Five groups of 3 female BALB/c mice (NCI) were injected IV with: 200 µCi (4.5 µg) 99mTc-PA; 200 µCi (4.5 µg) 99mTc-LF; 200 µCi (4.5 µg) 99mTc-EF; 40 µCi (1.5 µg) 99mTc-LF co-injected with 4.5 µg "cold" PA; or 40 µCi (1.5 µg) 99mTc-EF co-injected with 4.5 µg "cold" PA. At 1 and 3 hr post-injection the animals were anesthetized with Isoflurane and imaged for 1 or 2 min on a gamma-camera (Siemens) equipped with ICON image-processing software. At 24 h post-injection the animals were sacrificed, their organs removed, blotted to remove excess blood, weighed and counted in a gamma counter. The percentage of injected dose of toxin per gram of organ tissue (ID/g, %) was calculated.
To confirm the biodistribution results, the experiment was repeated with 123I-labeled toxins. PA, LF and EF were labeled with 123I using Iodobeads iodination reagent (Pierce Biotechnology, Rockford, IL) by incubating 100 µg of each toxin with two Iodobeads and 50 µL (2 mCi) of sodium 123I-iodide in PBS for 15 min at room temperature. Iodinated toxins were purified from unreacted 123I-iodide on Centricon-30 microconcentrators, diluted with PBS and imaging and biodistribution study was performed as above.
Statistical analysis
Student’s t-test for unpaired data was employed to analyze differences in the percent survival of macrophages or CHO cells treated with radiolabeled LeTx or EdTx versus unlabeled ones and in the organ uptake in the biodistribution studies. Differences were considered statistically significant when P values were < 0.05. The binding data for the Scatchard plot were analyzed by linear regression (Prism software, GraphPad, San Diego, CA).
RESULTS AND DISCUSSION
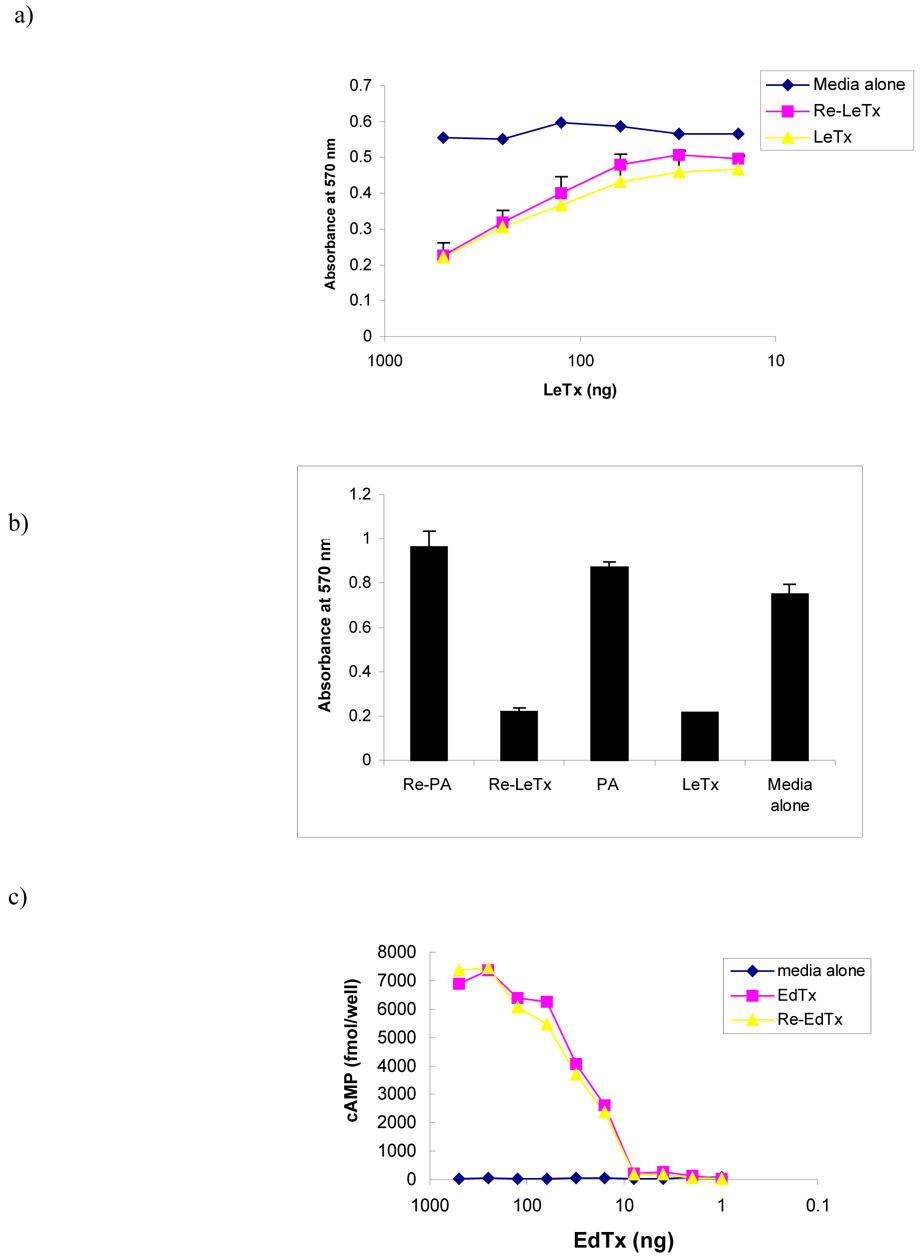
The specific activity of labeled toxins was approximately 10 mCi/mg, which was sufficiently high for utilization in the variety of biological experiments. To assess if labeling with 188Re affected the biological properties of toxins, we assayed the toxicity of radiolabeled PA followed by addition of unmodified LF for murine macrophages using the MTT assay. Addition of 188Re-labeled lethal toxin (188Re-LeTx) in the form of 188Re-PA and LF mixture to cell monolayers in increasing doses resulted in a significant reduction in cell viability The effect of 188Re-LeTx on the cells was dose dependent in the same way as for unlabeled LeTx (Fig. 1a). We considered the possibility that the 188Re emissions would be contributing to cellular death. Hence, we repeated the cellular assay with 188Re-PA alone and no effects on cells were noted (Fig. 1b).
Fig. 1.
Evaluation of biological activity of 188Re-labeled lethal toxin and edema toxin in toxicity assays. Lethal toxin (LeTx) is a mixture of PA and LF. 188Re-labeled lethal toxin (188Re-LeTx) is a mixture of 188Re-PA and LF. Edema toxin (EdTx) is a mixture of PA and EF. 188Re-labeled edema toxin (188Re-EdTx) is a mixture of PA and 188Re-EF. a) dose response experiment showing MTT assay of J774.16 macrophage-like cells treated with the increasing doses of LeTx or 188Re-LeTx; b) investigation of possible influence of 188Re radiation on J774.16 macrophage-like cells in the MTT assay; c) cAMP assay of CHO cells treated with EdTx or 188Re-EdTx. The values shown are the averages of 3 measurements and the brackets denote the standard deviation of the measurement.
The preservation of biological activity for EF after labeling with 188Re was assessed by treating CHO cells with 188Re-labeled edema toxin (188Re-EdTx, PA plus 188Re-EF) and measuring total cAMP levels in treated cells. No difference was noted in total cAMP levels for CHO cells treated with 188Re-EdTx and unlabeled EdTx (Fig. 1c). Thus, radiolabeling PA and EF with 188Re did not have an effect on the biological activity of LeTx and EdTx, respectively.
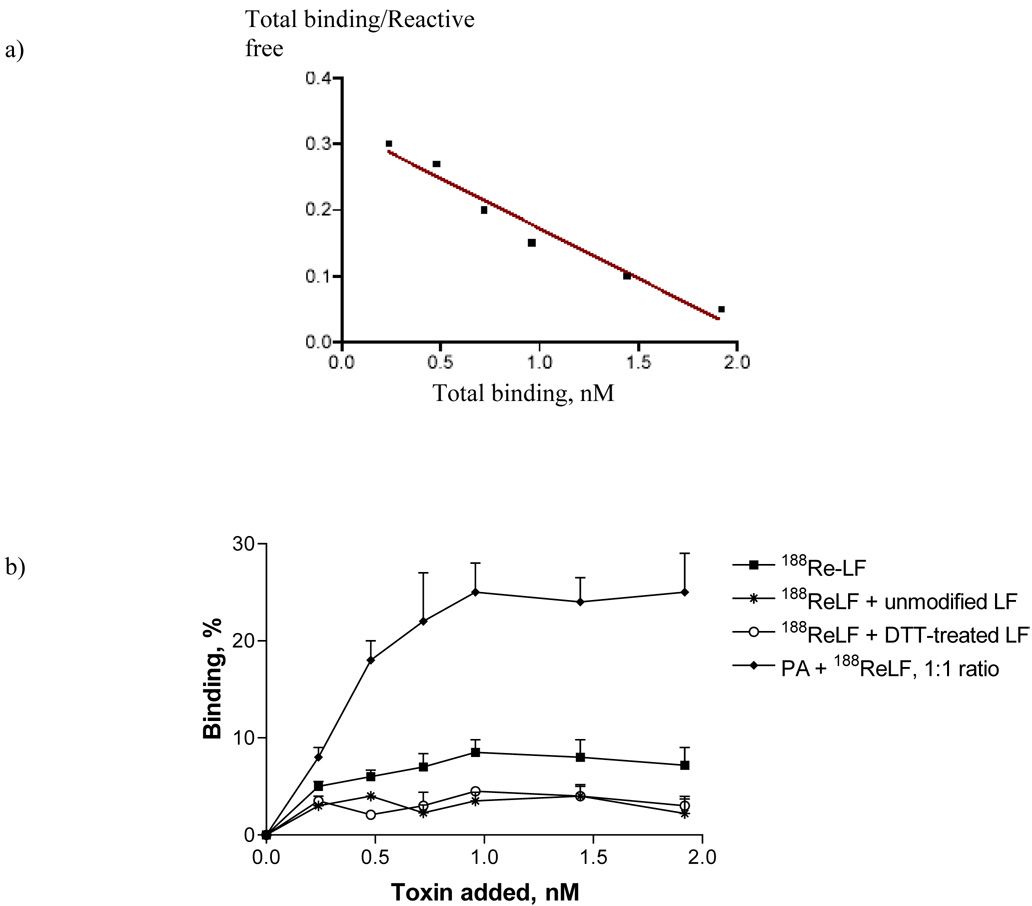
As radiolabeling allows to trace the proteins in vitro and in vivo, we used the labeled toxins in several experiments. First, we measured the binding of 188Re-PA to the J774.16 macrophages. For binding studies and calculation of the number of binding sites we used the technique described in the classical paper by Lindmo et. al. [10]. Previously we used this technique for the calculation of the number of binding sites on cryptoccocal cells [11] and on melanin in the melanoma cells [12]. The specific activity of 10 mCi/mg allowed us to use picomolar concentrations of labeled toxins while the counts per sample were at least 10,000 cpm due to the contribution of high energy beta-particles emitted by 188Re to the counting rate. The concentrations of labeled toxins used in the binding assays were also below toxic levels as per macrophage and CHO cells toxicity assays. The binding data are presented as Scatchard plot (Fig. 2a). From these data, we calculated the number of the PA-binding receptors as 6.6 × 104 per macrophage cell, taking into consideration the fact that PA forms heptamers on the surface of the cells, and a dissociation constant of 6.7 nM. Prior studies of macrophage cell lines using different techniques have measured 3 × 104 receptors per cell [2]. Our KD value in low nanomolar range is in good agreement with the 0.9 nM value measured by Escuyer and Collier for the binding of radioiodinated PA to CHO-K1 cells [13]. The difference between the measured KD's may reflect subtle differences in expressed PA and/or species differences in receptor structure. Nevertheless, our measured number confirms the literature data by independent technique and is consistent with the notion that 188Re-PA behaved similarly to unmodified PA molecule.
Fig. 2.
Binding of 188Re-labeled toxins to macrophages: a) Scatchard transformation of 188Re-PA binding to macrophages; b) binding of 188Re-LF to normal macrophages and to macrophage-bound PA with or without large molar excess of unmodified or DTT-treated LF. The percentage binding on Y axis shows the percentage of total 188Re-LF radioactive counts in the sample which are bound to the cells. The values shown in panel b are the average of 3 measurements and the brackets denote the standard deviation of the measurement.
In another series of experiments, we assessed the binding of 188Re-LF to normal macrophage cells and to macrophage-bound PA. The binding of 188Re-LF to macrophage-bound PA was more than two fold higher than that to the non-PA-treated cells (Fig. 2b), in agreement with the data on LF and EF binding to PA heptamer on the cell surface, which then carries them into the cell. However, our data also shows significant binding of labeled LF to the cells in the absence of PA suggesting the existence of other mechanisms for LF binding to these cells (Fig. 2b).
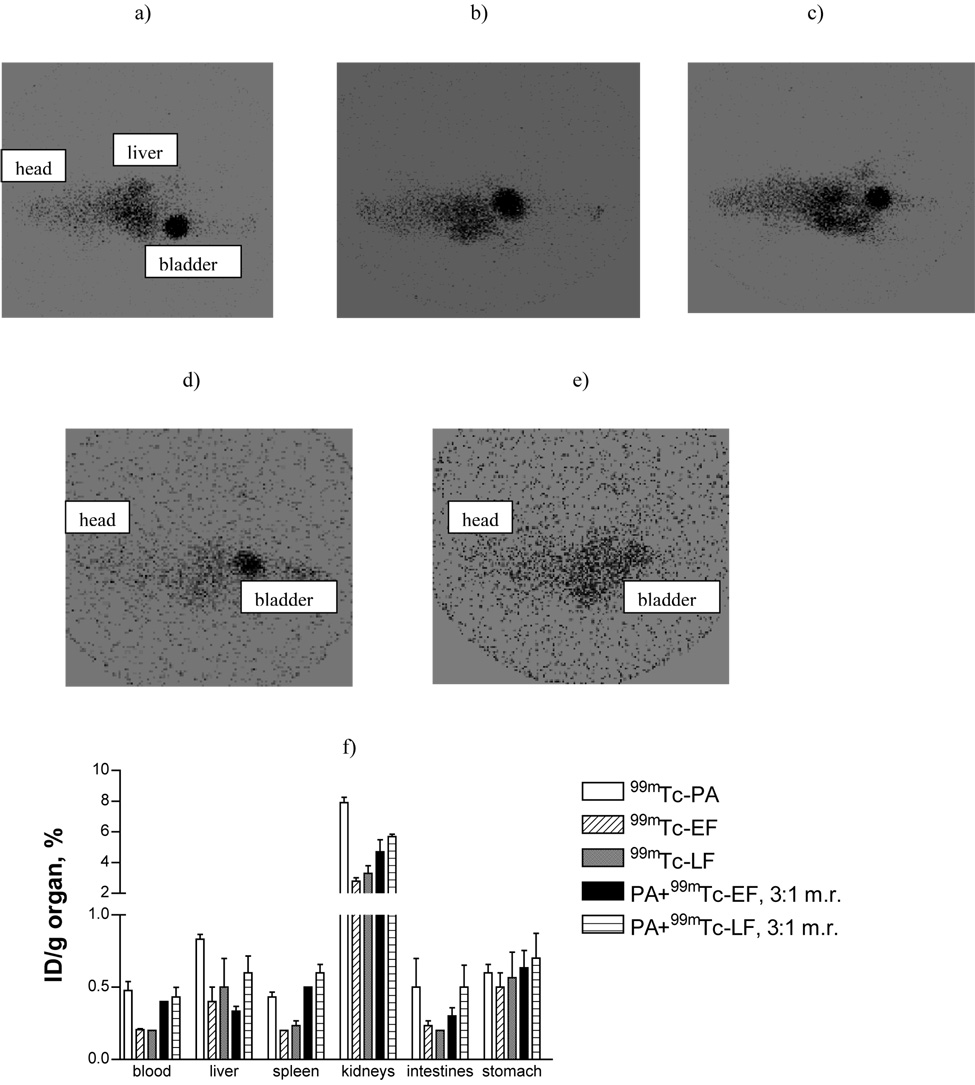
Systemic administration of LF, EF, and PA toxins in mice produces toxicity and this protocol is commonly used to investigate the efficacy of specific antibodies in passive protection and vaccine studies [2–5]. Although this assay is not physiological considering the pathogenesis of anthrax, it provides a means to test some aspects of toxin function. The availability of labeled toxins allowed us to scintigraphically evaluate the preferential localization of toxin proteins injected into mice. Toxins were labeled with 99mTc using the same protocol as for labeling with 188Re. Though 188Re can be successfully imaged with a gamma camera from the emission of 155 keV photons with 15% abundance, 99mTc is a more suitable radionuclide for imaging applications because it has a much higher photon flux. The biodistribution studies were done with trace amounts of labeled compounds, well below lethal concentrations: a small dose (4.5 µg of PA and 1.5 µg of either 99mTc-LF or 99mTc-EF) was chosen to monitor the distribution of a compound in the tissues while avoiding any obvious toxic effects in mice. According to the detailed study by Moayeri et. al. [3] of anthrax toxins effects on inbred mice, 10 µg of toxins did not have any effect on sensitive BALB/c mice and even at 50 µg doses there were no toxic effects observed up to 15 hours post-administration of toxins with only 10% of mice showing some toxicity at 24 hrs. We were interested in biodistribution of toxins during the early time points on which the information in literature is lacking.
Intravenous administration of labeled toxin revealed predominant liver and spleen localization as early as 1 and 3 h with significant clearance through the kidneys as manifested by very high uptake in the bladder (Fig. 3a–e). The observation of renal clearance for toxins that are > 80 kDa may be explained by enzymatic degradation of toxins in the blood. Moayeri et al. reported that following bolus injection, PA was rapidly cleaved in the blood by protease that was not cell associated [14]. Very little activity was seen in the thoracic area for all three toxins when injected alone or in combination. These results reflect the distribution of labeled toxins, as the diffusion of 99mTc label from the toxins would result in the pronounced uptake of free radionuclide in thyroid and stomach, which are target organs for 99mTc-pertechnetate [15]. The results of biodistribution performed 24 hr post-injection confirmed the renal clearance of toxin-derived radioactivity as well as the uptake in the liver, spleen and intestines (Fig. 3f). Our results are consistent with a preliminary report of organ localization of 125I-PA which identified liver and spleen followed by the lungs as target organs for IV injected 125I-PA [16]. The finding of renal excretion shortly after injection strongly suggests that toxins are rapidly degraded after intravenous injection and this could contribute to the variability of mouse toxigenic assays. Co-injection of "cold" PA with 99mTc-EF or 99mTc-LF in 3:1 molar ratio, a dose chosen to reflect the stoichiometry of toxin binding to the macrophages altered the biodistribution of both 99mTc-EF and 99mTc-LF: at 24 hr post-injection there was significantly more (P≤0.02) 99mTc-EF+PA and 99mTc-LF+PA in the blood, spleen, kidneys and intestines than 99mTc-EF and 99mTc-LF, respectively, which is consistent with a preserved ability of labeled toxins to bind to PA. The difference in liver uptake between 99mTc-EF and 99mTc-LF and their combination with PA was not statistically significant. Furthermore, our results help to explain the observations made by Moayeri et. al. [3] who injected LeTx systemically into mice and detected liver necrosis by 18–24 hr post-administration of 100 µg of toxins and significant damage to the spleen and intestines at 18 hr and later. Their study also noted a relative absence of damage to the lungs and kidneys. Consistent with this observation we noted very low uptake of the toxins in the thoracic area. The absence of kidney damage despite significant renal and bladder uptake can be explained by clearance of degraded toxin that is unable to mediate tissue damage. Our study showed that anthrax toxins localized at the reported major sites of organ damage shortly after infusion and supports the view that local damage to abdominal organs sets forth a cascade of events that leads to lethal toxicity even after the toxin is largely degraded and cleared.
Fig. 3.
Scintigraphic imaging and biodistribution of BALB/c mice injected IV with 99mTc-labeled anthrax toxins. Scintigraphic imaging at 1 hr post-injection (a–e): a) 99mTc-EF; b) 99mTc-LF; c) 99mTc-PA; d) 99mTc-LF+PA; e) 99mTc-EF+PA; f) biodistribution at 24 hr. On the images shown all mice are laying on their backs, with the heads on the left and the tails on the right. BALB/c mice were injected IV with: 200 µCi (4.5 µg) 99mTc-PA; 200 µCi (4.5 µg) 99mTc-LF; 200 µCi (4.5 µg) 99mTc-EF; 40 µCi (1.5 µg) 99mTc-LF co-injected with 4.5 µg "cold" PA; or 40 µCi (1.5 µg) 99mTc-EF co-injected with 4.5 µg "cold" PA. ID/g - injected dose per gram tissue. Three mice per group were used and the brackets denote the standard deviation of the measurement. M.r. - molar ratio.
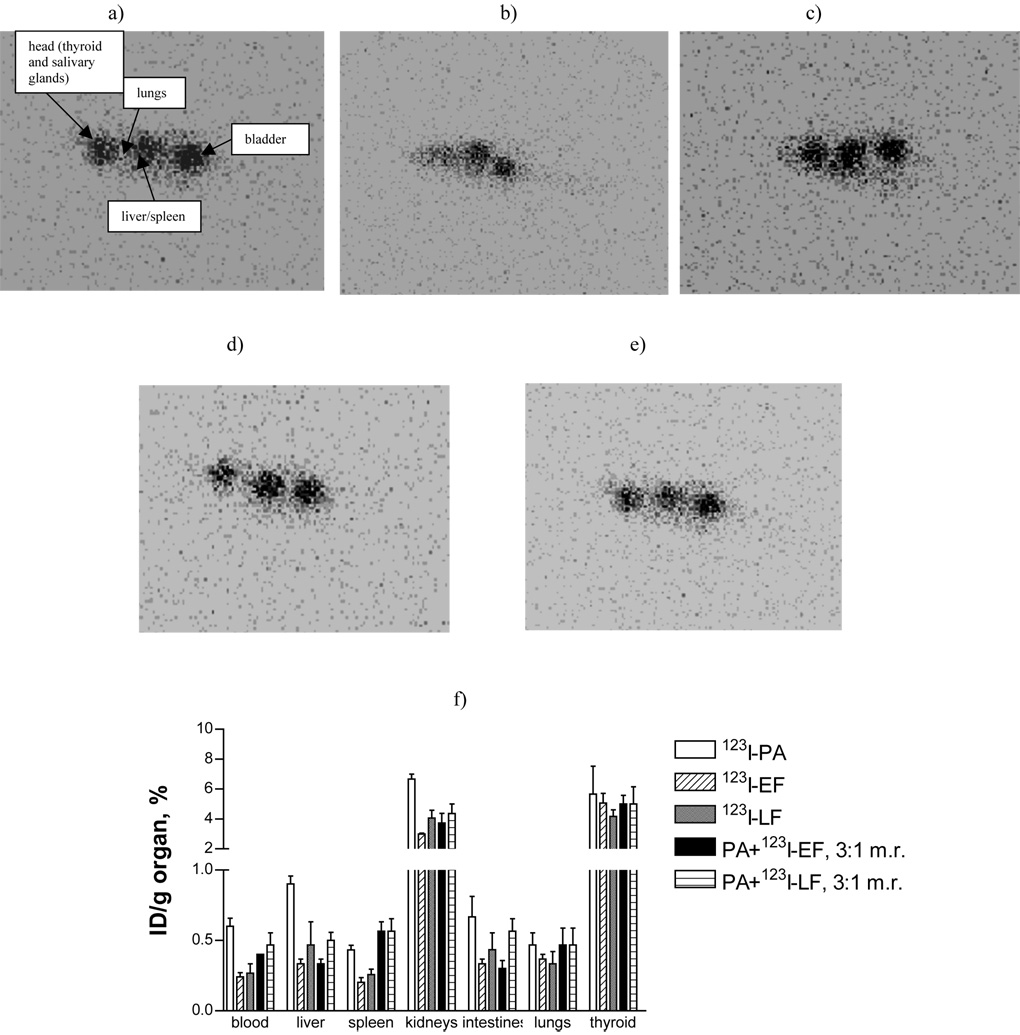
To confirm the results observed with the 99mTc-labeled toxins, we repeated the study with 123I labeling. Imaging at 1 and 3 hr post IV injection and the biodistribution at 24 hr (Fig. 4) demonstrated that except for thyroid and salivary glands uptake - the distribution patterns of iodinated toxins were similar to those of 99mTc-labeled ones with radioactivity concentrated in the liver, spleen and intestines, and being excreted through the kidneys. The absence of any significant lung uptake is apparent as a “gap” in uptake in the chest area on the early images (Fig. 4a–e) and the scintigraphic imaging data was confirmed by biodistribution data at 24 hr (Fig. 4f). We also noted considerable uptake in the thyroid and salivary glands (organs expressing sodium iodide symporter) for all preparations which is due to dehalogenation – an observation consistent with the reported biodistribution results in [16]. For that reason, administration of any radioiodinated molecule to patients is accompanied by blocking their thyroids with Lugol to prevent radioiodine uptake. Interestingly, in spite of relative instability of iodine label, iodination is still considered a useful method of radiolabeling.
Fig. 4.
Scintigraphic imaging and biodistribution of BALB/c mice injected IV with 123I-labeled anthrax toxins. Scintigraphic imaging at 1 hr post-injection (a – e): a) 123I - EF; b) 123I - LF; c) 123I - PA; d) 123I - LF+PA; e) 123I - EF+PA; f) biodistribution at 24 hr. On the images shown all mice are laying on their backs, with the heads on the left and the tails on the right. BALB/c mice were injected IV with: 100 µCi (4.5 µg) 123I-PA; 100 µCi (4.5 µg) 123I-LF; 100 µCi (4.5 µg) 123I-EF; 20 µCi (1.5 µg) 123I - LF co-injected with 4.5 µg "cold" PA; or 20 µCi (1.5 µg) 123I - EF co-injected with 4.5 µg "cold" PA. ID/g - injected dose per gram tissue. Three mice per group were used and the brackets denote the standard deviation of the measurement. M.r. - molar ratio.
In conclusion, the availability of 188Re and 99mTc-labeled PA, LF and EF toxins allowed us to confirm the number of PA binding sites per cell, to provide an estimate of the dissociation constant of PA for its receptor, and to demonstrate tissue distribution of toxins after intravenous injection. Also, since imaging is performed at toxin concentration that below pharmacologically significant, these observations revealed metabolism patterns that are not masked by toxic effects.
ACKNOWLEDGEMENTS
The research was funded by NIH grants 5U54AI057158-03 (AC) and AI60507 (ED). E. Revskaya was supported by NIH Postdoctoral Immunooncology and Immunology Training Award. We thank Dr. V. Pazo (Jacobi Medical Center, NY) for help with the biodistribution.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Bradley KA, Mogridge J, Mourez M, Collier RJ, Young JA. Identification of the cellular receptor for anthrax toxin. Nature. 2001;414:225–229. doi: 10.1038/n35101999. [DOI] [PubMed] [Google Scholar]
- 2.Friedlander AM, Bhatnagar R, Leppla SH, Johnson L, Singh Y. Characterization of macrophage sensitivity and resistance to anthrax lethal toxin. Infect. Immun. 1993;61:245–252. doi: 10.1128/iai.61.1.245-252.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moayeri M, Haines D, Young HA, Leppla SH. Bacillus anthracis lethal toxin induces TNF-alpha-independent hypoxia-mediated toxicity in mice. J. Clin. Invest. 2003;112:670–682. doi: 10.1172/JCI17991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Price BM, Liner AL, Park S, Leppla SH, Mateczun A, Galloway DR. Protection against anthrax lethal toxin challenge by genetic immunization with a plasmid encoding the lethal factor protein. Infect. Immun. 2001;69:4509–4515. doi: 10.1128/IAI.69.7.4509-4515.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawada-Hirai R, Jiang I, Wang F, Sun SM, Nedellec R, Ruther P, Alvarez A, Millis D, Morrow PR, Kang AS. Human anti-anthrax protective antigen neutralizing monoclonal antibodies derived from donors vaccinated with anthrax vaccine adsorbed. J. Immune Based Ther. Vaccines. 2004;2:5–7. doi: 10.1186/1476-8518-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rivera J, Nakouzi A, Abbouds N, Revskaya E, Goldman D, Collier RJ, Dadachova E, Casadevall A. A monoclonal antibody to Bacillus anthracis protective antigen defines a neutralizing epitope in domain 1. Infect Immun. 2006;74:4149–4156. doi: 10.1128/IAI.00150-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blaustein RO, Koehler TM, Collier RJ, Finkelstein A. Anthrax toxin: channel-forming activity of protective antigen in planar phospholipid bilayers. Proc. Natl. Acad. Sci. USA. 1989;86:2209–2213. doi: 10.1073/pnas.86.7.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mukherjee S, Lee SC, Casadevall A. Antibodies to Cryptococcus neoformans glucuronoxylomannan enhance antifungal activity of murine macrophages. Infect. Immun. 1995;63:573–579. doi: 10.1128/iai.63.2.573-579.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leppla SH. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc. Natl. Acad. Sci. U S A. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn PA., Jr. Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J. Immunol. Methods. 1984;72:77–89. doi: 10.1016/0022-1759(84)90435-6. [DOI] [PubMed] [Google Scholar]
- 11.Dadachova E, Bryan RA, Apostolidis C, Morgenstern A, Zhang T, Moadel T, Torres M, Huang X, Revskaya E, Casadevall A. Interaction of radiolabeled antibodies with fungal cells and components of immune system in vitro and during radioimmunotherapy of experimental fungal infection. J. Infect. Dis. 2006;193:1427–1436. doi: 10.1086/503369. [DOI] [PubMed] [Google Scholar]
- 12.Schweitzer AD, Rakesh V, Revskaya E, Datta A, Casadevall A, Dadachova E. Computational model predicts effective delivery of 188-Re-labeled melanin-binding antibody to the metastatic melanoma tumors with wide range of melanin concentrations. Melanoma Res. 2007;17:291–303. doi: 10.1097/CMR.0b013e3282eeeae7. [DOI] [PubMed] [Google Scholar]
- 13.Escuyer V, Collier RJ. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect. Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moayeri M, Wiggins JF, Leppla SH. Anthrax protective antigen cleavage and clearance from the blood of mice and rats. Infec. Immun. 2007;75:5175–5184. doi: 10.1128/IAI.00719-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuckier LS, Dohan O, Li Y, Carrasco N, Dadachova E. Kinetics of perrhenate uptake and comparative biodistribution of perrhenate, pertechnetate and iodide by NIS-expressing tissues in vivo. J. Nucl. Med. 2004;45:500–507. [PubMed] [Google Scholar]
- 16.Hay RV, Duesbery NS, Skinner RS, VanBrocklin MW, Vande Woude GF, Gross MD. Biodistribution of radiolabeled anthrax lethal factor in mice; Society of Nuclear Medicine 2005 Annual Meeting; 2005. Abst. # 1289. [Google Scholar]