Abstract
Objective
To evaluate the impact of rigorous WalkRounds on frontline caregiver assessments of safety climate, and to clarify the steps and implementation of rigorous WalkRounds.
Data Sources/Study Setting
Primary outcome variables were baseline and post WalkRounds safety climate scores from the Safety Attitudes Questionnaire (SAQ). Secondary outcomes were safety issues elicited through WalkRounds. Study period was August 2002 to April 2005; seven hospitals in Massachusetts agreed to participate; and the project was implemented in all patient care areas.
Study Design
Prospective study of the impact of rigorously applied WalkRounds on frontline caregivers assessments of safety climate in their patient care area. WalkRounds were conducted weekly and according to the seven-step WalkRounds Guide. The SAQ was administered at baseline and approximately 18 months post-WalkRounds implementation to all caregivers in patient care areas.
Results
Two of seven hospitals complied with the rigorous WalkRounds approach; hospital A was an academic teaching center and hospital B a community teaching hospital. Of 21 patient care areas, SAQ surveys were received from 62 percent of respondents at baseline and 60 percent post WalkRounds. At baseline, 10 of 21 care areas (48 percent) had safety climate scores below 60 percent, whereas post-WalkRounds three care areas (14 percent) had safety climate scores below 60 percent without improving by 10 points or more. Safety climate scale scores in hospital A were 62 percent at baseline and 77 percent post-WalkRounds (t=2.67, p=.03), and in hospital B were 46 percent at baseline and 56 percent post WalkRounds (t=2.06, p=.06). Main safety issues by category were equipment/facility (A [26 percent] and B [33 percent]) and communication (A [24 percent] and B [18 percent]).
Conclusions
WalkRounds implementation requires significant organizational will; sustainability requires outstanding project management and leadership engagement. In the patient care areas that rigorously implemented WalkRounds, frontline caregiver assessments of patient safety increased. SAQ results such as safety climate scores facilitate the triage of quality improvement efforts, and provide consensus assessments of frontline caregivers that identify themes for improvement.
Keywords: WalkRounds, patient safety, safety culture, safety climate, quality improvement, senior leader partnerships
WalkRounds were introduced in 1999 as a program for hospital leadership to sustain good relations with frontline caregivers, promote conversations to identify hazards, and gather information to enhance decision making around patient safety. In the wake of the IOM report (Institute of Medicine 1999), the demand for WalkRounds and other patient safety improvement efforts quickly outpaced rigorous research efforts, which resulted in widespread adoption of interventions with relatively little supporting evidence (Frankel et al. 2005; Haig, Sutton, and Whittington 2006). Not surprisingly, the extent to which health care leaders and managers reported that they are doing WalkRounds did not coincide with frontline caregiver's awareness of WalkRounds (Thomas et al. 2005).
To be effective stewards of limited patient safety resources, health care leaders must be informed consumers of available interventions, and select and rigorously implement these interventions. In our experience, few hospitals differentiate rounding to evaluate patient satisfaction, compliance with policies, or showcasing of excellent employees from WalkRounds that elicit caregiver concerns about patient safety, near misses, and adverse events. Even fewer rigorously compile the information elicited during WalkRounds, and fewer still embrace the wisdom of frontline caregivers by eliciting their assessments of patient safety relative to the WalkRounds intervention. Evaluating the impact of WalkRounds requires standardized and rigorous implementation of the program, and a validated tool to capture frontline caregiver assessments of patient safety, such as the safety climate scale of the Safety Attitudes Questionnaire (SAQ).
In high reliability (i.e., very safe) industries such as commercial aviation (Sexton and Thomas 2004) and nuclear power (Carroll 1998), safety climate is a proactive metric of safety that complements traditional retrospective metrics (e.g., number of fatalities and accidents). The specific aims of this study were to evaluate the impact of rigorous WalkRounds on frontline caregiver assessments of safety climate, and to clarify the steps and implementation of rigorous WalkRounds.
METHODS
Seven acute care hospitals and one Ambulatory Center in Massachusetts were invited to participate in a prospective study of the impact of Patient Safety Leadership WalkRounds on safety climate. Because of resource limitations, we targeted a representative sample of health care facilities based on size (i.e., large, small) and scope (e.g., acute tertiary care institution to a small rural hospital) to capture unique issues in implementing our project. Each invited institution agreed to participate. Results of the Ambulatory Center will be presented elsewhere.
To participate, a hospital senior executive had to commit to championing the WalkRounds project and following the criteria outlined in the WalkRounds Guide (Table 1). The project period was August 2002 to April 2005. Participating sites began in staggered fashion in the summer and early fall of 2002 and assessed their safety climate at baseline and approximately 18 months after implementing the WalkRounds project. This was a hospital-wide effort supported by senior leaders and administration, with all clinical areas (e.g., pharmacy, intensive care unit, medical floor, etc.) in each hospital included in the project.
Table 1.
WalkRounds Guide (Health Research and Educational Trust)
| Seven steps are required for effectively implementing WalkRounds: |
| Preparation— Ensure commitment and regular participation by leadership, secure dedicated resources from quality and safety departments, and clearly communicate process, scheduling, and feedback mechanisms for the rest of the organization |
| Scheduling— Set WalkRounds months in advance and accommodate schedules of executive team members, supporting patient safety staff, and other participants |
| Conducting WalkRounds— Decide where to conduct the sessions. Sessions should include opening and closing statements and a series of specific questions |
| Tracking— Set up a robust process for tracking and ranking collected data |
| Reporting— Share WalkRounds data with a multidisciplinary committee so that action items may be assigned to management personnel |
| Feedback— Establish a clearly delineated and formal structure for feedback to frontline providers who participate in WalkRounds and to executive boards about findings and actions taken to address them |
| Measurement— Evaluate whether WalkRounds are effective in improving the organization's culture |
Reprinted with permission from the Health Research and Educational Trust (Frankel, Grillo, and Pittman 2006).
Patient Safety Leadership WalkRounds
WalkRounds training was done on-site at each institution in a half-day session. This session included a 2-hour presentation of the Patient Safety Leadership WalkRounds project to senior leaders, quality and patient safety personnel, and clinical area managers/directors. Following this presentation, a subset of interested leaders who would shepherd the program forward were oriented to the underlying theories and concepts of WalkRounds, a framework and timeline for implementation, and a process to manage the data and provide feedback to those involved in rounds. The training also included recommendations for linking safety concerns identified during WalkRounds to the hospital's existing operations committee, which could ensure actions were taken and changes instituted. Hospital leaders were specifically instructed how to conduct weekly rounds, integrate rounds into their routine, and use rounds to surface and address concerns or defects related to patient safety. Investigators (A. F., M. P., S. P. G.) did on-site debriefings with those senior leaders who conducted weekly or bi-weekly WalkRounds on clinical floors. Thereafter, coaching calls were done every 2 months for 2 years with this core group of leaders.
Senior leaders targeted for inclusion in WalkRounds were the Chief Executive Officer, Chief Operating Officer, Chief Medical Officer, Chief Nursing Officer, or their equivalents. Other Board-level or senior clinical administrators were invited to participate, including Chief Financial and Chief Information Officers. The quality and patient safety personnel were charged with organizing the WalkRounds, and managing the database of safety concerns, recommendations, and actions taken to address the issues elicited through the rounding process. A Microsoft Access database was provided by the research team to manage the data.
Safety Climate Domain of the SAQ
This manuscript reports results from the safety climate domain of the psychometrically validated SAQ (Sexton et al. 2006). The six domains of the SAQ are safety climate, perceptions of management, teamwork climate, job satisfaction, stress recognition, and working conditions. A recent review of safety climate instruments in health care highlighted the SAQ as the leading instrument because it meets 22 of 23 essential criteria (e.g., content, validity, and reliability) (Colla et al. 2005). The safety climate scale is valid (Sexton et al. 2006), sensitive to interventions (Defontes and Surbida 2004; Thomas et al. 2005), and the attitudes elicited associated with patient length of stay and error rates (Pronovost et al. 2005). Safety climate scores vary widely among patient care areas within a given hospital. Therefore, we assessed safety climate at the patient care area level rather than the hospital level (Pronovost and Sexton 2005). The SAQ safety climate scale is calculated using seven items, each rated on a five-point scale from disagree strongly to agree strongly, including:
I am encouraged by my colleagues to report any patient safety concerns I may have.
The culture in this clinical area makes it easy to learn from the mistakes of others.
Medical errors are handled appropriately in this clinical area.
I know the proper channels to direct questions regarding patient safety in this clinical area.
I receive appropriate feedback about my performance.
I would feel safe being treated here as a patient.
In this clinical area, it is difficult to discuss mistakes (reverse scored).
Safety climate scale scores were computed by taking the mean of the seven items for each respondent. Given the significant variability in safety climate scores among clinical areas, the longitudinal climate goal for a given unit is twofold: (1) improve your safety climate score by 10 points or more; or (2) maintain a positive safety climate consensus score of 60 percent or higher. In other words, the goal for a unit with good culture (60 percent or more of staff reporting good safety climate) is to maintain or improve it, whereas the goal for a unit with poor culture (<60 percent reporting good safety climate) is to improve it by 10 points or more.
SAQ Participants and Administration
All staff with a 50 percent or greater commitment to their patient care area for at least the 4 consecutive weeks before survey administration were invited to complete the SAQ regardless of their involvement in the WalkRounds project. This included staff physicians, registered nurses (RN), charge nurses, nurse managers, physician assistant/nurse practitioners, licensed vocational nurses (LVN)/licensed practicing nurses (LPN), hospital aides, physical therapists, occupational therapists, pharmacists, respiratory therapists, technicians, ward clerks/unit secretaries, medical administration, and other. Senior leadership (CEO, CFO, CNO, etc.) were not surveyed because the SAQ applies to clinical and nonclinical personnel more directly involved in the delivery of care to patients. Each participating patient care area administered the voluntary survey during preexisting staff meetings, with a pencil and return, sealable envelope to maintain confidentiality. Survey packets were hand-delivered to staff that were missed in preexisting meetings.
The criteria for inclusion of a patient care area in this analysis of safety climate were twofold: (1) the participating hospital was required to conduct weekly methodologically rigorous WalkRounds, according to the criteria outlined in Table 1 and (2) the patient care area needed a response rate of 50 percent or greater for baseline and post-WalkRounds administrations of the SAQ.
Statistical Methods
The percent positive, or “percent reporting good safety climate” for a patient care area was the percent of respondents in a care area with an average (mean of the seven items) safety climate scale score of agree slightly or higher. We adopted the convention of reporting percent agreement (“how good is the safety climate?”) rather than means (“how average is the safety climate?”) when presenting SAQ results to caregivers, managers, executives, and board members because percents are easier for these stakeholders to interpret (Pronovost and Sexton 2005). To test for improvement in safety climate assessments within patient care areas from baseline to post-WalkRounds, we used paired sample t-tests for each hospital to control for patient care areas nested within a hospital. Statistical analyses were performed using SPSS, version 13.0 (Chicago, IL).
RESULTS
Study Population
Of seven hospitals, two underwent a change in leadership or had limited resources that precluded them from implementing WalkRounds, and one hospital implemented WalkRounds intermittently without a leader to drive the project. Four hospitals conducted rigorous weekly WalkRounds; two of these four complied with intensive collection and use of data. Results from these latter two hospitals are reported in this paper. Hospital A was an academic teaching institution, and hospital B a community facility; both had approximately 250 beds.
Two SAQ administrations with a 50 percent or higher response rate were completed in nine of 20 patient care areas in hospital A, and 12 of 24 patient care areas in hospital B; 21 units in total with ample response rates. In the 21 patient care areas, surveys were received from 790 of 1,265 (62 percent) at baseline, and 741 of 1,256 (60 percent) post-WalkRounds. Most respondents were female (74 percent baseline and 77 percent post) and RN (39 percent and 45 percent) (Table 2). Mean age was 39±12 at baseline and 40±12 post-WalkRounds, and years in same hospital 9.9±9.7 at baseline and 10.7±10.2 post.
Table 2.
SAQ Respondent Demographics for Baseline and Post-WalkRounds
| Baseline | % of Total | Post-WalkRounds | % of Total | |
|---|---|---|---|---|
| Registered nurse | 308 | 39 | 336 | 45.3 |
| Nurse manager/charge nurse | 13 | 1.6 | 24 | 3.2 |
| PCA/hospital aid/care partner | 17 | 2.2 | 16 | 2.2 |
| PA/NP | 6 | 0.8 | 12 | 1.6 |
| LVN/LPN | 5 | 0.6 | 9 | 1.2 |
| Staff physician | 117 | 15 | 64 | 8.6 |
| Therapist (PT/OT) | 2 | 0.3 | 0 | 0 |
| Respiratory therapist | 11 | 1.4 | 22 | 3 |
| Pharmacist | 14 | 1.8 | 8 | 1.1 |
| Unit Asst/clerk/secretary | 29 | 3.7 | 44 | 5.9 |
| Technician | 151 | 19 | 96 | 13 |
| Medical administration | 6 | 0.8 | 9 | 1.2 |
| Other | 62 | 7.8 | 62 | 8.4 |
| Total | 741 | 94 | 702 | 94.7 |
| Missing | 49 | 6.2 | 39 | 5.3 |
| Total | 790 | 100 | 741 | 100 |
| Female | 588 | 74.4 | 571 | 77.1 |
| Male | 157 | 19.9 | 131 | 17.7 |
| Missing | 45 | 5.7 | 39 | 5.3 |
| Mean years in hospital | 9.9 | 10.7 | ||
| SD years in hospital | 9.7 | 10.2 | ||
| Mean years age | 39.2 | 40.3 | ||
| SD years age | 12 | 11.8 |
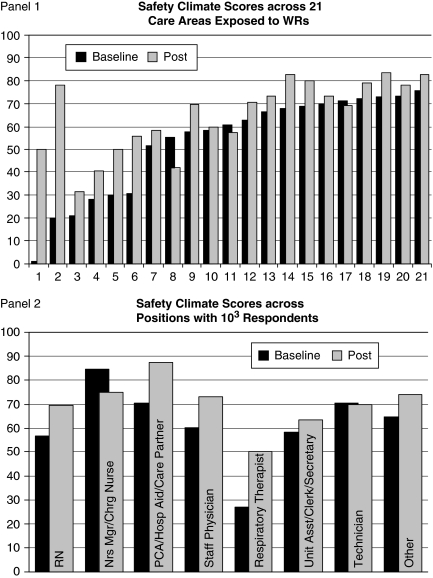
Percent reporting positive safety climate across these 21 clinical areas at baseline ranged from 0 to 76 percent, and post-WalkRounds from 32 to 83 percent (Figure 1, Panel 1). At baseline, 10 of 21 care areas (48 percent) were below the 60 percent consensus safety climate score, whereas post-WalkRounds 3 care areas (14 percent) were below 60 percent consensus and did not improve their score by the minimum 10 points. Figure 1, Panel 2 shows how the safety climate scores changed for each caregiver type. RN perceptions improved from 57 to 70 percent reporting positive safety climate, whereas nurse managers/charge nurses decreased from 85 to 75 percent. Similarly, hospital aides, staff physicians, and respiratory therapists each improved the percent reporting positive safety climate by 10 points or more.
Figure 1.
Panel 1: Percent of Respondents in Each Clinical Area Reporting Positive Safety Climate Pre- and Post-WalkRounds Intervention. Panel 2: Percent of Respondents in Each Caregiver Category Reporting Positive Safety Climate Pre- and Post-WalkRounds Intervention
Comparison of Baseline and Post-WalkRounds Safety Climate Scores
In hospital A, safety climate scale scores were 62 percent at baseline and 77 percent post-WalkRounds (t=2.67, p=.03). In hospital B, safety climate scale scores were 46 percent at baseline and 56 percent post-WalkRounds (t=2.06, p=.06). Four items in the scale significantly improved post-WalkRounds in hospitals A and B: feeling encouraged by colleagues to report patient safety concerns, knowing proper channels to direct patient safety questions, easily learning from the errors of others, and easily discussing errors that occur in their clinical area (Table 3).
Table 3.
Paired Samples t-test Results for Safety Climate Items across Hospitals A and B
| 2004 % Positive | 2005 % Positive | Mean Difference | SD | t | df | Significance (2 Tailed) | |
|---|---|---|---|---|---|---|---|
| I am encouraged by my colleagues to report any patient safety concerns I may have | |||||||
| Hospital A | 81.23 | 88.04 | −6.81 | 7.85 | −2.60 | 8 | .032 |
| Hospital B | 67.85 | 80.62 | −12.77 | 12.18 | −3.63 | 11 | .004 |
| The culture in this clinical area makes it easy to learn from the errors of others | |||||||
| Hospital A | 64.38 | 78.98 | −14.59 | 16.76 | −2.61 | 8 | .031 |
| Hospital B | 50.32 | 60.06 | −9.75 | 17.11 | −1.97 | 11 | .074 |
| In this clinical area, it is difficult to discuss errors (note % positive here is the % disagree due to negative wording) | |||||||
| Hospital A | 58.95 | 68.58 | −9.63 | 14.81 | −1.95 | 8 | .087 |
| Hospital B | 41.88 | 52.08 | −10.20 | 12.89 | −2.74 | 11 | .019 |
| I know the proper channels to direct questions regarding patient safety in this clinical area | |||||||
| Hospital A | 81.22 | 90.04 | −8.82 | 9.16 | −2.89 | 8 | .020 |
| Hospital B | 74.38 | 84.59 | −10.20 | 8.61 | −4.11 | 11 | .002 |
| I would feel safe being treated here as a patient | |||||||
| Hospital A | 92.35 | 92.95 | −0.60 | 8.79 | −0.20 | 8 | .843 |
| Hospital B | 71.83 | 72.55 | −0.72 | 15.27 | −0.16 | 11 | .873 |
| Medical errors are handled appropriately in this clinical area | |||||||
| Hospital A | 87.54 | 92.43 | −4.89 | 6.97 | −2.10 | 8 | .069 |
| Hospital B | 73.48 | 80.30 | −6.81 | 20.44 | −1.16 | 11 | .273 |
| I receive appropriate feedback about my performance | |||||||
| Hospital A | 64.03 | 74.13 | −10.10 | 19.27 | −1.57 | 8 | .155 |
| Hospital B | 58.25 | 58.93 | −0.68 | 15.23 | −0.15 | 11 | .880 |
There were two hospitals that did not conduct rigorous WalkRounds but collected safety climate data and met the 50 percent cutoff in a total of 18 clinical areas. The paired sample t-tests were not significant for this group overall or by hospital.
Patient Safety Issues Elicited through WalkRounds
The issues raised during WalkRounds have a qualitative richness that is muted when attempting to quantify or categorize data. For example, in an inpatient psychiatric unit WalkRounds elicited that metal and glass objects continued to enter the unit on meal trays despite a surveillance mechanism. The solution was to change all utensils and cups to plastic and paper. On the same unit, inadequate information about a patient's assault history was identified, and resolved by establishing a screening log during crisis evaluations that was eventually added to the electronic medical record system. In an emergency room, adolescents testing positive for a sexually transmitted disease were uniformly lost to follow-up because this information was not provided to ambulatory clinics. As a temporary fix, residents in the ambulatory clinic were paged and the electronic medical record modified to enable consistent access to patient information.
Equipment/facility (hospital A 26 percent, hospital B 33 percent) and communication (hospital A 24 percent, hospital B 18 percent) were areas most often cited as safety concerns that could potentially harm a patient (Table 4). Typical examples for equipment/facility were:
Table 4.
Patient Safety Issues Elicited through WalkRounds
| Hospital A (N=464) | Hospital B (N=358) | |
|---|---|---|
| Communication related total | 115 (24.8%) | 64 (18%) |
| Communication between MD | 3 (0.6%) | 5 (1.4%) |
| Communication between MDs/RNs | 10 (2.2%) | 6 (1.7%) |
| Communication between staff and patient | 6 (1.3%) | 1 (0.3%) |
| Communication between units/areas/pods | 35 (7.5%) | 3 (0.8%) |
| Incomplete/inconsistent documentation | 36 (7.8%) | 37 (10.3%) |
| Involvement/availability/responsiveness | 8 (1.7%) | 3 (0.8%) |
| MD coverage | 9 (1.9%) | 6 (1.7%) |
| RN/pharmacy communication | 0 (0%) | 1 (0.3%) |
| Team communication | 8 (1.7%) | 2 (0.6%) |
| Department specific total | N/A | N/A |
| Admitting | 1 (0.2%) | |
| Food service | 0 (0%) | 3 (0.8%) |
| Housekeeping | 13 (2.8%) | 2 (0.6%) |
| Infection control | 1 (0.2%) | 7 (2%) |
| Interpreter service | 9 (1.9%) | 0 (0%) |
| Radiology | 2 (0.4%) | 5 (1.4%) |
| Security | 12 (2.6%) | 1 (0.3%) |
| Equipment/supply/facility related total | 121 (26%) | 119 (33%) |
| Equipment availability/organization | 14 (3%) | 34 (9.5%) |
| Equipment functionality/maintenance | 11 (2.4%) | 28 (7.8%) |
| Facilities (structural) | 25 (5.4) | 13 (3.6%) |
| Facilities (maintenance) | 23 (5%) | 15 (4.2%) |
| Space/storage | 42 (9.1%) | 18 (5%) |
| Supply availability/organization | 6 (1.3%) | 10 (2.8%) |
| Supply functionality | 0 (0%) | 1 (0.3%) |
| IS related total | 40 (8.6%) | 7 (2%) |
| IS | 40 (8.6%) | 5 (1.4%) |
| Telecommunications | 0 (0%) | 2 (0.6%) |
| Lab related total | 1 (0.2%) | 9 (2.5%) |
| Lab (other) | (0%) | 8 (2.2%) |
| Stat labs | 1 (0.2%) | 0 (0%) |
| Phlebotomy | 0 (0%) | 1 (0.3%) |
| Misc total | N/A | N/A |
| Education/training | 14 (3%) | 12 (3.4%) |
| Families/visitors | 3 (0.6%) | 3 (0.8%) |
| Incident reporting | 2 (0.4%) | 1 (0.3%) |
| Organizational structure/responsibility | 2 (0.4%) | 1 (0.3%) |
| Parking/transportation | 16 (3.4%) | 1 (0.3%) |
| Policies/procedures/protocols | 29 (6.3%) | 21 (5.9%) |
| Patient related total | N/A | N/A |
| Monitoring | 0 (0%) | 5 (1.4%) |
| Patient flow | 26 (5.6%) | 18 (5%) |
| Patient issues | 6 (1.3%) | 4 (1.1%) |
| Patient identification | 1 (0.2%) | 12 (3.4%) |
| Patient transport | 2 (0.4%) | 11 (3.1%) |
| Pharmacy related total | 13 (2.8%) | 21 (5.9%) |
| Look alike/sound alike/wrong drug | 0 (0%) | 2 (0.6%) |
| Pharmacy | 13 (2.8%) | 19 (5.3%) |
| Staff related total | 35 (7.5%) | 30 (8.4%) |
| Staff inexperience/attrition/turnover | 2 (0.4%) | 5 (1.4%) |
| Work overload | 33 (7.1%) | 25 (7%) |
Otoscopes and ophthalmoscopes are not present in patient rooms.
Wheelchairs do not work properly.
Supplies located at the back of the unit are difficult for staff to access.
IV pumps do not hold a charge long enough for patient transport for testing.
It is difficult to transport patients from the ICU to testing because the corridor is cluttered with stored equipment resulting from no storage space.
Typical examples for communication were:
There is no electronic communication between the ED and the ambulatory clinics, and positive test results are often not documented.
Preoperative notes and anesthesia consult records are not available online.
Operating room staff members do not consistently call before they send patients to the unit.
It is difficult to know if a critical value that has been communicated to the inpatient nurse has also reached the physician who will address it; an electronic system to notify the doctors directly is needed.
DISCUSSION
Frontline caregiver assessments of patient safety improved in both hospitals after implementing the WalkRounds project. This study builds upon previous WalkRounds research, which assessed safety climate among nurses present during the intervention (Thomas et al. 2005), by including all types of caregivers within a patient care area during WalkRounds. In addition, this study conducted WalkRounds weekly for 18 months, rather than monthly for 3 months.
We found that WalkRounds provided a formal structure and ongoing mechanism for caregivers to surface and address patient safety defects. In fact, the paired sample t-test results demonstrated significant improvement in the items that specifically dealt with discussing local patient safety concerns. Discussing and learning from errors, feeling encouraged by colleagues to report concerns, and knowing how to report concerns were themes from the four items that improved the most, and may be a result of senior leaders connecting with frontline workers to reveal and resolve concerns. In particular, improvement in the safety climate item “I am encouraged by my colleagues to report any patient safety concerns I may have,” indicates that WalkRounds bolstered a shared sense of patient safety interconnectedness among the caregivers in a given patient care area.
The types of problems elicited during WalkRounds were influenced by the type of providers who participated. Nurses preferentially discussed operational problems, while physicians tended to focus on clinical decision-making issues. In both cases, the WalkRounds leader's skill in directing conversation and making participants feel safe determined whether the concerns elicited included a discussion of real adverse events.
Anecdotally, issues raised during WalkRounds fell into three categories; those that could be resolved locally, those that required cross-departmental collaboration, and those that required significant resources demanding new budget allocations. It is unlikely that the impact of organizational actions on perceptions of safety is directly related to these categories or to the cost or resource components of the action. Instead, a reasonably frugal action such as changing metal utensils to plastic may have an enormous impact on safety and perceptions of safety.
WalkRounds may empower caregivers with a stronger sense of responsibility for patient safety, coupled with a stable and predictable partnership with upper management to provide resources and remove barriers relevant to improve patient safety. Specific examples in two patient care areas with strong changes in safety climate scores support this suggestion. In one care area, the first WalkRounds elicited a discussion about poorly functioning wheelchairs that led to their replacement. In the second area, a serious adverse event was discussed during WalkRounds that led to a consensus that errors could be discussed in a supportive environment.
Analyses from other industries suggest that improving frontline assessments of safety increases actions that promote safety and minimize risk taking behaviors (Roberts 1990). The implication for health care organizations is that WalkRounds, by comparison to monies spent on other efforts to improve safety especially in the realm of informatics, is an inexpensive mechanism through which leaders can positively influence and document safety and quality over time. Moreover, WalkRounds in conjunction with a cultural assessment provides a clear picture of patient care areas with low safety climate scores that would benefit the most from WalkRounds. This is important given the limited resources for patient safety interventions. Using a validated cultural assessment tool, such as the SAQ , to diagnose strengths and weaknesses at the patient care area level is a powerful way to harness the wisdom and insights of frontline caregivers while helping direct the attention, resources, and responsiveness of hospital leaders to care areas that need it most. To be better stewards of dwindling resources and availability of leaders, the SAQ could be used to diagnose and triage assistance in the form of WalkRounds to units that need help.
Notable in this study is that only two of the seven hospitals were successful at broad and sustained implementation of WalkRounds. Commitment from leadership, a champion trained in quality or safety, and time and resources to manage the data and feedback are the three components that these two institutions had when compared with the other five hospitals. All three components appear to be necessary for success.
Implications of Recruiting Clinical Areas to Participate versus Using Early Adopters
Similar to the lesson learned by the U.S. armed services after the Vietnam War, there is a significant difference in performance and outcome when using a mandatory draft versus a volunteer army. Most of our collective experience using WalkRounds and the SAQ has been with early adopters who were ahead of their contemporaries in thinking about and addressing patient safety defects. We have found that hospitals recruited to rigorously conduct WalkRounds or administer a cultural assessment survey have a significantly lower level of engagement and sustainment than hospitals who seek our guidance to conduct these interventions as a result of their own progressive thinking.
Albeit anecdotal, early adopters have consistently garnered higher levels of participation, more rigorous follow-through, and higher SAQ response rates than their recruited counterparts. For example, our study achieved a 60 percent response rate for the SAQ , whereas it typically garners a response rate of over 80 percent for hospital-wide (Pronovost and Sexton 2005). In this sense, our results may be an underestimation relative to the results achieved by some hospitals that chose to rigorously implement WalkRounds and refine the process on their own (Pronovost et al. 2005). In addition, hospital systems, such as Ascension, that were early adopters of safety culture assessment have garnered system-wide SAQ response rates of over 80 percent (across 60 hospitals and 24,000 respondents), and have integrated their results with decisions to choose patient safety interventions that are most appropriate for specific patient care areas (Rose et al. 2006). Unlike previous WalkRounds research that used an experiment/control group design, we chose a less sophisticated pre–post design, whereby each patient care area served as its own control. Prior work has demonstrated that control groups are easily contaminated by experimental group participants who float between patient care areas (Thomas et al. 2005). To compensate, we used a longer exposure period for WalkRounds (approximately 2 years) than previous work.
There were potential limitations to this study. First, detecting improvements in safety climate scores were limited by the small number of participating patient care areas, which resulted in statistical power limitations. Nevertheless, the separately conducted paired samples t-tests indicated significant improvement in safety climate scores for hospital A, and approached significance ( p=.06) for hospital B. Second, including only two hospitals limited our ability to generalize more broadly to hospital across the U.S. However, our sample did include an academic teaching and community facility. Third, a pre–post study design limited our ability to conclusively say that the WalkRounds caused the improvement in safety climate. While WalkRounds were the most visible effort during this period, the improvements might have been due to a more general temporal trend toward improved safety climate or other patient safety activities.
In conclusion, WalkRounds are not a patient safety panacea. Rather, they should be considered in the context of organizational readiness as a function of available leadership time, organizational resources, and patient safety-related priorities. The intent of WalkRounds is to implement a patient safety infrastructure that bridges the gap between leaders and frontline caregivers. The end result reported here is a significant improvement in frontline caregiver assessments of patient safety, and a narrowing of the apparent disconnect between RN and nurse managers/charge nurses. The spread and adoption of WalkRounds worldwide (Budrevics and O'Neill 2005; Verschoor et al. 2007) (http://www.npsa.nhs.uk/sevensteps) suggests that the process meets a need not yet met, which is eliciting caregiver concerns to identify local hazards within a framework that allows for the removal of barriers that impede actionable steps to make improvements. Assessing safety climate with the validated SAQ , affords leadership and frontline caregiver alike, the ability to empirically identify specific care areas that are struggling. In turn, WalkRounds can be implemented to identify and address local concerns, and track progress over time. Taken together, safety climate assessment and WalkRounds allow hospitals to diagnose, target, and treat the patient care areas in need of resources and leadership attention.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We would like to thank the Health Resources & Services Administration for the original WalkRounds grant, and the Health Research and Educational Trust for the opportunity to significantly refine the process and supporting materials related to WalkRounds. We would like to acknowledge Lou Woolf, Robert Norton, Alex Ferraro, Jennifer Costain, Eileen Sporing, James Mandel, and Sandra Fenwick for their participation in developing WalkRounds in their institutions, and Christine G. Holzmueller for her assistance in editing this manuscript. Dr. Eric Thomas was supported by AHRQ grant #1PO1HS1154401, and Dr. Bryan Sexton was supported by RWJ Foundation grant 58292.
Disclosures: Allan Frankel, Bryan Sexton, and Sarah Grillo are members of Lotus Forum Inc., a company dedicated to developing benchmark safety metrics for the health care industry.
Disclaimers: None.
Supporting Information
The following supporting information for this article is available online:
Author matrix.
This material is available as part of the online article from: http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2008.00878.x (this link will take you to the article abstract).
Please note: Blackwell Publishing is not responsible for the content or functionality of any supplementary materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Budrevics G, O'Neill C. Changing a Culture with Patient Safety Walkarounds. Healthcare Quarterly (Toronto, Ont.) 2005;8 Spec No: 20-5. [PubMed] [Google Scholar]
- Carroll J S. Safety Culture as an Ongoing Process: Culture Surveys as Opportunities for Inquiry and Change. Work and Stress. 1998;12:272–84. [Google Scholar]
- Colla J, Bracken A, Kinney L, Weeks W. Measuring Patient Safety Climate: A Review of Surveys. Quality and Safety in Health Care. 2005;14:364–6. doi: 10.1136/qshc.2005.014217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defontes J, Surbida S. Preoperative Safety Briefing Project. Permanente Journal. 2004;8(2):21–7. doi: 10.7812/tpp/04.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankel A, Grillo S P, Baker E G, Huber C N, Abookire S, Grenham M, Console P, O'Quinn M, Thibault G, Gandhi T K. Patient Safety Leadership WalkRounds at Partners Healthcare: Learning from Implementation. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2005;31(8):423–37. doi: 10.1016/s1553-7250(05)31056-7. [DOI] [PubMed] [Google Scholar]
- Frankel A S, Grillo S, Pittman M A. Patient Safety Leadership WalkRounds(™) Guide. Chicago: Health Research and Educational Trust; 2006. [Google Scholar]
- Haig K M, Sutton S, Whittington J. SBAR: A Shared Mental Model for Improving Communication between Clinicians. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2006;32(3):167–75. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999. [Google Scholar]
- Pronovost P, Weast B, Rosenstein B, Sexton J B, Holzmueller C G, Paine L, Davis R, Rubin H R. Implementing and Validating a Comprehensive Unit-Based Safety Program. Journal of Patient Safety. 2005;1(1):33–40. [Google Scholar]
- Pronovost P J, Sexton J B. Assessing Safety Culture: Guidelines and Recommendations. Quality and Safety in Health Care. 2005;14:231–3. doi: 10.1136/qshc.2005.015180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts K H. Managing High Reliability Organizations. California Management Review. 1990;32(4):101–13. [Google Scholar]
- Rose J S, Thomas C S, Tersigni A, Sexton J B, Pryor D. A Leadership Framework for Culture Change in Health Care. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2006;32(9):433–42. doi: 10.1016/s1553-7250(06)32057-0. [DOI] [PubMed] [Google Scholar]
- Sexton J B, Helmreich R L, Neilands T B, Rowan K, Vella K, Boyden J, Roberts P R, Thomas E J. The Safety Attitudes Questionnaire: Psychometric Properties Benchmarking Data, and Emerging Research. BioMed Central Health Services Research. 2006;6:34. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton J B, Thomas E. Measurement: Assessing a Safety Culture. Chicago: Health Administration Press; 2004. [Google Scholar]
- Thomas E J, Sexton J B, Neilands T B, Frankel A, Helmreich R L. The Effect of Executive Walk Rounds on Nurse Safety Climate Attitudes: a Randomized Trial of Clinical Units. BioMed Central Health Services Research. 2005;5(1):28. doi: 10.1186/1472-6963-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verschoor K N, Taylor A, Northway T L, Hudson D G, Van Stolk D E, Shearer K J, McDougall D L, Miller G. Creating a Safety Culture at the Children's and Women's Health Centre of British Columbia. Journal of Pediatric Nursing. 2007;22(1):81–6. doi: 10.1016/j.pedn.2006.08.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author matrix.