Abstract
Background
Catheter-related bacteremia (CRB) is a frequent complication of tunneled dialysis catheters, and Enterococcus is a common infecting organism. CRB may be treated by instilling an antibiotic lock into the catheter lumen, in conjunction with systemic antibiotics. The efficacy of this approach in Enterococcus bacteremia is unknown.
Design
Quality improvement report.
Setting and participants
64 catheter-dependent hemodialysis outpatients with vancomycin-sensitive Enterococcus bacteremia treated with a uniform antibiotic lock protocol. Clinical outcomes were tracked prospectively.
Quality improvement plans
Patients received intravenous vancomycin for 3 weeks, in conjunction with a vancomycin lock instilled into both catheter lumens after each dialysis session.
Measures
Treatment failure was defined as persistent fever 48 hours after initiation of antibiotics or recurrent Enterococcus bacteremia within 90 days. A clinical cure was defined as fever resolution without recurrent bacteremia. Major infection-related complications within 6 months were documented.
Results
Treatment failure occurred in 25 patients (39%), due to persistent fever in 10, and recurrent bacteremia in 15. Treatment success occurred in 39 patients (61%). A serious complication of Enterococcus CRB occurred in 4 of 64 patients (6%), endocarditis in 1 and osteomyelitis in 3. The frequency of serious complications was 16% (4/25) in patients with treatment failure, as compared with 0% (0/39) in those with treatment success (P=0.01).
Limitations
This was a single-center study. We did not measure serum vancomycin levels.
Conclusions
An antibiotic lock protocol permits catheter salvage in 61% of hemodialysis patients with Enterococcus CRB. Serious complications occur in 6% of patients, and are more common in those with treatment failure.
Introduction
Catheter-related-bacteremia (CRB) is a common complication in catheter-dependent hemodialysis patients, and may be caused by a variety of Gram-positive and Gram-negative organisms [1]. The standard treatment of CRB entails administration of systemic antibiotics, as well as removal of the infected catheter [2]. As an alternative to catheter removal, a number of investigators have instilled a concentrated antibiotic-anticoagulant solution into the catheter lumens during the inter-dialytic period (“antibiotic lock”). By sterilizing the biofilm on the inner surface of the catheter lumens, this approach achieves a clinical cure in about two-thirds of patients with CRB, while permitting catheter salvage [3-7].
A major advantage of using an antibiotic lock to treat CRB is the ability to salvage the catheter in many cases. A potential drawback of this approach is that a delay in removing the infected catheter may expose the patient to serious complications, such as endocarditis, osteomyelitis, septic arthritis, or epidural abscess.
The success rate of the antibiotic lock varies by organism type, being quite high for Gram-negative and Staphylococcus epidermidis infections, and quite poor in those caused by Staphylococcus aureus [4, 6-8]. There are limited published data addressing the potential risks and benefits of routinely employing antibiotic locks for treatment of Enterococcus CRB, and the efficacy of an antibiotic lock in this context has not been reported in large series. In a previous study evaluating antibiotic locks at our institution, 12 hemodialysis patients with vancomycin-sensitive Enterococcus CRB were treated with 3 weeks of systemic vancomycin and gentamicin, in conjunction with a vancomycin-gentamicin-heparin catheter lock [5]. In that study, 5 of 12 patients (42%) treated with this regimen grew Candida from their surveillance blood cultures obtained one week after completing the antibiotic course. We speculated that this complication was a consequence of prolonged exposure to broad-spectrum antibiotics. To minimize this complication, we subsequently revised the antibiotic protocol for Enterococcus CRB to comprise vancomycin alone, in conjunction with a vancomycin-heparin lock.
The goal of the present study was to evaluate the clinical outcomes of hemodialysis patients with vancomycin-sensitive Enterococcus CRB treated with a vancomycin lock, and to quantify the frequency of serious complications.
Methods
Setting
The University of Alabama at Birmingham (UAB) provides medical care for approximately 450 hemodialysis patients, under the supervision of 10 full-time clinical nephrologists. About 25% of these patients are catheter-dependent at any given time. Over 95% of all hospitalizations of our dialysis patients occur at UAB Hospital, allowing for comprehensive follow-up of any complications. Two full-time access coordinators schedule all access procedures, and maintain a prospective, computerized database of all vascular access procedures and complications, including microbiology reports and clinical outcomes [9]. The access database was first implemented at UAB in 1996 to track vascular access outcomes at our dialysis centers and to facilitate continuous quality improvement initiatives.
Function
We have been using antibiotic locks to treat all patients with dialysis CRB at our institution since June 2000. The dialysis nurses implement a standard protocol, which has been approved by all the clinical nephrologists. The purpose of this program is to track prospectively all episodes of CRB, including type of organism, antibiotics administered, response to therapy, hospitalizations, and all infection-related complications.
Interventions
CRB was suspected whenever fever (>38.0 C) or rigors developed in a catheter-dependent dialysis patient, in the absence of an alternative source of infection [1]. Two sets of blood cultures were obtained, one from the dialysis catheter and a second set from a peripheral vein or from the dialysis circuit. The patient received empiric vancomycin (loading dose of 20 mg/kg, followed by 500 mg after each dialysis treatment) and ceftazidime (1 gm after each dialysis treatment). The antibiotic regimen was modified to vancomycin alone, once the culture was identified as growing Enterococcus. The total duration of systemic antibiotics was 3 weeks. Serum vancomycin levels were not measured, as our freestanding dialysis units used a remote central laboratory and rapid turnaround of serum drug levels was not available. In conjunction with the systemic antibiotics, a vancomycin-heparin lock was instilled into the catheter lumens after each dialysis session. The vancomycin-heparin lock was prepared by mixing 1 ml of vancomycin (5 mg/ml) with 1 ml of heparin (10,000 units/ml) for a final vancomycin concentration of 2.5 mg/ml and heparin concentration of 5000 units/ml. We have previously reported that vancomycin is compatible with heparin at these concentrations when incubated at 37°C for 72 hours [5]. A standard heparin lock was resumed once the course of systemic antibiotics was completed. Blood cultures were repeated 1 week after completing the course of antibiotics or if the patient developed recurrent fever or chills. Patients with treatment failures (persistent fever or recurrent bacteremia) had their catheter removed.
Measures
The dialysis access coordinators tracked prospectively clinical information on all patients with suspected CRB, including the organism grown, whether the fever resolved by the next dialysis session (2-3 days), any changes in antibiotics, the results of follow-up blood cultures, any catheter procedures, and any infection-related hospitalizations. Most patients with CRB were treated as outpatients, but those with severe sepsis or serious complications were hospitalized. The diagnosis of endocarditis required demonstration of valvular vegetations by a trans-thoracic or trans-esophageal echocardiogram. Osteomyelitis was diagnosed by computerized tomography or magnetic resonance imaging. Patients with serious complications of bacteremia received a 6-week course of intravenous antibiotics.
The patients were classified into two major groups according to the clinical outcomes of their infection: (1) treatment success (resolution of fever and no recurrent Enterococcus bacteremia within 90 day); or (2) treatment failure (persistent fever or recurrent Enterococcus bacteremia within 90 days).
Analytic methods
Permission was obtained from the UAB Institutional Review Board to review each patient's medical records for research purposes. We retrospectively queried the prospective, computerized vascular access database to identify 824 episodes of CRB during a 3-year period (8/1/04 – 7/31/07). Of these, 109 episodes, representing 13% of all CRB's, were due to Enterococcus. Only the first episode of Enterococcus bacteremia in each patient was included (N=79). Patients with vancomycin-resistant Enterococccus bacteremia (N=8) were excluded. In addition, episodes with concurrent Staphylococcus aureus bacteremia (N=6) or Candidemia (N=1) were excluded, as these were routinely managed with catheter removal. The current study analyzed further the 64 patients remaining after these exclusions.
Baseline patient demographic and clinical features were compared between the two outcome groups by the Student t-test for continuous variables, and by the Chi square test for categorical variables. The electronic medical record of each study patient was reviewed to identify any serious infection-related complications occurring within 6 months of the episode of CRB, such as endocarditis, osteomyelitis, septic arthritis, or epidural abscess. The frequency of major complications between patient sub-groups was compared by the Chi square test. A P value < 0.05 was considered statistically significant.
Results
Situation analysis
All dialysis patients with CRB were treated by a uniform protocol with objective outcome measures. The use of a consistent protocol and prospective documentation of outcomes permitted us to perform a formal analysis of the success rate and complication rate in the subset of patients with Enterococcus bacteremia
Outcomes
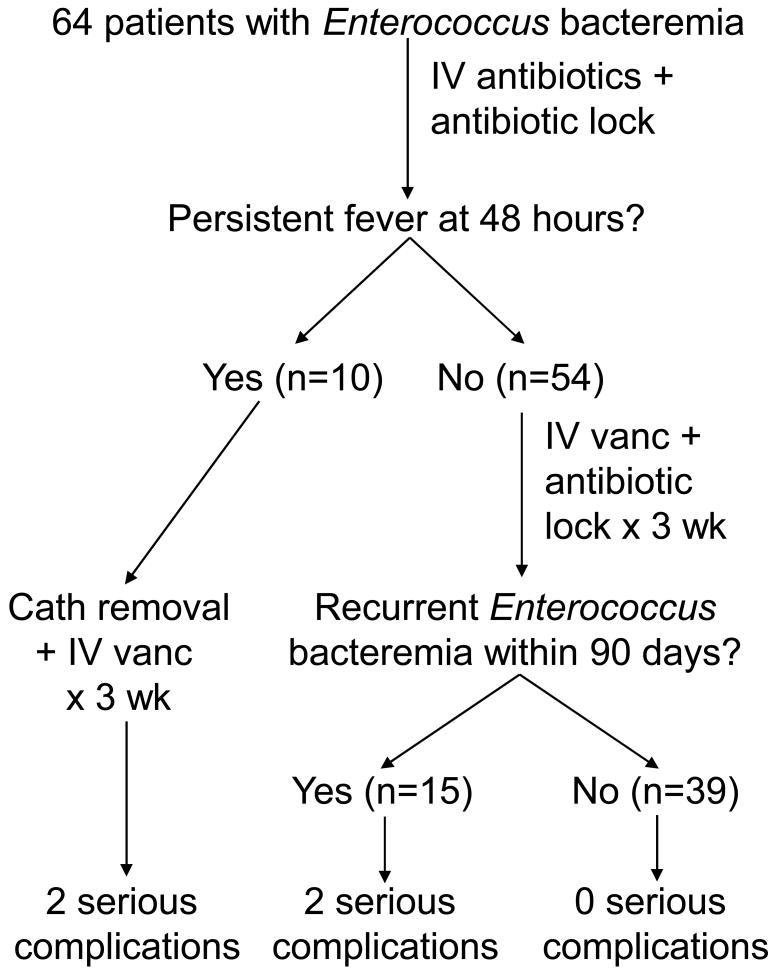
Among the 64 patients with Enterococcus CRB treated with an antibiotic lock, the fever persisted in 16% of patients, and their infected catheters were removed promptly (Figure 1). In an additional 23% of patients, the fever resolved initially, but Enterococcus bacteremia recurred within 90 days of the initial CRB. Thus, 61% of the patients had a clinical cure, as defined by rapid resolution of fever and absence of recurrent Enterococcus bacteremia. The two outcome groups (clinical success and clinical failure) were similar in terms of age, sex, race, diabetes, hypertension, and vascular disease (Table 1).
Figure 1.
Clinical outcomes of 64 patients with Enterococcus catheter-related bacteremia treated with an antibiotic lock protocol.
Cath, catheter, IV, intravenous; vanc, vancomycin; wk, week
Table 1. Clinical features of treatment success vs. treatment failure patients.
| Treatment success | Treatment failure | P value | |
|---|---|---|---|
| N pts | 39 | 25 | |
| Age, years | 55 ± 16 | 54 ± 13 | 0.8 |
| Sex, N (%) women | 28 (72%) | 14 (56%) | 0.3 |
| Race, N (%) African-American | 33 (85%) | 23 (92%) | 0.5 |
| Diabetes | 25 (64%) | 17 (68%) | 0.8 |
| Hypertension | 39 (100%) | 24 (96%) | 0.4 |
| Coronary artery disease | 14 (36%) | 4 (16%) | 0.09 |
| Peripheral vascular disease | 11 (28%) | 5 (20%) | 0.6 |
Treatment success = resolution of fever and absence of recurrent Enterococcus bacteremia within 90 days
Treatment failure = persistent fever at 2-3 days OR recurrent Enterococcus bacteremia within 90 days.
A serious complication was observed in 6% (4 of 64) of all patients with Enterococcus CRB, including 1 case of endocarditis and 3 of osteomyelitis (Table 2). The case of endocarditis and 2 cases of osteomyelitis were diagnosed within 1 week of the presentation with Enterococcus CRB; the third case of osteomyelitis was diagnosed after 6 weeks. The frequency of serious complications differed substantially among the treatment outcome groups, being 16% in those with treatment failure, as compared with 0% in those with a clinical cure (P = 0.01)(Table 2, Figure 1). Patient survival at 6 months was similar in both groups. Among the patients with a clinical cure the median time to loss of catheter patency was 78 days.
Table 2. Comparison between the main two groups.
| Treatment success | Treatment failure | P value | |
|---|---|---|---|
| N patients | 39 | 25 | |
| N (%) with serious complications | 0/39 (0%) | 4/25 (16%)
Endocarditis (1 week) Osteomyelitis (1 week, 1 week, and 6 weeks) |
0.01 |
| N (%) alive at 6 months * | 32/34 (94%) | 23/25 (92%) | 0.5 |
Excludes 5 patients who transferred to an outside unit.
Ten of the 64 patients had a second episode of CRB within 6 months of their initial Enterococcus CRB. Eight of these second infections occurred in patients in whom the antibiotic lock had failed. The causative organism for the second CRB was vancomycin-sensitive Enterococcus faecalis in 3 patients, Staphylococcus epidermidis in 2 patients, Staphylococcus aureus in 1 patient, Enterobacter cloacae in 1 patient, and Candida in 1 patient. Two patients with a previous clinical cure had a subsequent CRB within 6 months, one with Staphylococcus epidermidis and one with Klebsiella pneumoniae.
Discussion
The present study found a relatively high success rate (61%) of a vancomycin lock treatment in salvaging the infected catheter in a large population of hemodialysis patients with Enterococcus CRB. This cure rate was lower than that previously observed at our institution for Gram-negative CRB (87%) and Staphylococcus epidermidis CRB (75%), but higher than that for Staphylococcus aureus CRB (41%) [6, 8]. The reason for the treatment failures cannot be determined from the present study. Two potential explanations are a biofilm that was resistant even to high levels (∼100-fold higher than therapeutic plasma concentrations) of vancomycin, or formation of a biofilm on the exterior aspect of the catheter, where the antibiotic lock has no potential action.
In a previous study from our institution using a vancomycin-gentamicin-heparin lock for treatment of Enterococcus CRB, the surveillance blood cultures obtained one week after completing the 3-week course of antibiotics grew Candida in 5 of 12 patients (42%)[5]. Fortunately, with the revised protocol using vancomycin alone, none of the 64 patients grew Candida from their post-treatment surveillance cultures, and only one patient developed Candidemia 10 weeks after the initial Enterococcus CRB.
Serious complications (endocarditis or osteomyelitis) occurred in 6% of the patients with Enterococcus CRB, and were observed exclusively in those patients in whom the antibiotic lock was unsuccessful (16% vs. 0%). We previously reported a 10% rate of serious complications in patients with Staphylococcus aureus CRB, but in that study the treatment success rate was only 40% [8]. Thus, as compared to patients with Staphylococcus aureus CRB, those with Enterococcus CRB had a higher clinical cure rate and a lower rate of serious complications. There have not been any publications addressing the clinical cure rate or the frequency of serious complications in hemodialysis patients with Enterococcus CRB treated with routine early catheter removal. Thus, it is not possible to compare the clinical success rate or the risk of serious complications using the 2 treatment strategies. However, 3 of the 4 serious complications observed in the current study were diagnosed within one week of presentation, suggesting that they would have occurred regardless of the treatment strategy.
Among those patients achieving a clinical cure with an antibiotic lock protocol, a subsequent episode of CRB occurred within 6 months in 2 of 39 patients (5%). The rate of second infection was higher in the group with treatment failures, occurring in 8 of 25 patients (32%). This high frequency of second CRB is not surprising, and has previously been reported by us even among patients whose CRB was managed with early catheter removal or guidewire exchange [10].
The present study has some limitations. First, this was a retrospective study. However, given the meticulous prospective data collection on all episodes of CRB by dedicated vascular access coordinators, it is unlikely that we missed clinical failures or serious complications of CRB. Second, all the patients were treated at a single medical center, and the outcomes may not generalize to some dialysis facilities. Finally, we did not measure serum vancomycin levels, so some treatment failures may have been due to subtherapeutic antibiotic concentrations. However, serum drug levels were not readily available from the remote central laboratory used by our dialysis units. For this reason, we used previously validated empiric vancomycin dosing for hemodialysis patients [11].
In conclusion, an antibiotic lock protocol permits catheter salvage in 61% of patients with Enterococcus CRB. Serious complications occurred in 6% of patients, and were significantly more common in those with treatment failure. Further studies are needed to evaluate the long-term safety of an antibiotic lock strategy to treat dialysis CRB.
Acknowledgments
Portions of this manuscript were presented in abstract form at the Clinical Meeting of the National Kidney Foundation; April 2-6, 2008; Dallas, TX.
Support: This research was supported in part by grant number 1 K24 DK59818-01 from the National Institute of Diabetes and Digestive and Kidney Diseases to Dr. Allon.
Footnotes
Financial Disclosure: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Allon M. Dialysis catheter-related bacteremia: Treatment and prophylaxis. Am J Kidney Dis. 2004;44:779–791. [PubMed] [Google Scholar]
- 2.KDOQI clinical practice guidelines and clinical practice recommendations for vascular access 2006. Am J Kidney Dis. 2006;48(suppl 1):S176–S322. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Capdevilla JA, Segarra A, Planes AM, Ramirez-Arellano M, Pahissa A, Piera L, Martinez-Vazquez JM. Successful treatment of hemodialysis catheter-related sepsis without catheter removal. Nephrol Dial Transplant. 1993;8:231–234. [PubMed] [Google Scholar]
- 4.Fernandez-Hidalgo N, Almirante B, Calleja R, Ruiz I, Planes AM, Rodriguez D, Pigrau C, Pahissa A. Antibiotic-lock therapy for long-term intravascular catheter-related bacteremia: results of an open, non-comparative study. J Antimicrob Chemother. 2006;57:1172–1180. doi: 10.1093/jac/dkl103. [DOI] [PubMed] [Google Scholar]
- 5.Krishnasami Z, Carlton D, Bimbo L, Taylor ME, Balkovetz DF, Barker J, Allon M. Management of hemodialysis catheter related bacteremia with an adjunctive antibiotic lock solution. Kidney Int. 2002;61:1136–1142. doi: 10.1046/j.1523-1755.2002.00201.x. [DOI] [PubMed] [Google Scholar]
- 6.Poole CV, Carlton D, Bimbo L, Allon M. Treatment of catheter-related bacteremia with an antibiotic lock protocol: effect of bacterial pathogen. Nephrol Dial Transplant. 2004;19:1237–1244. doi: 10.1093/ndt/gfh041. [DOI] [PubMed] [Google Scholar]
- 7.Vardhan A, Davies J, Daryanani I, Crowe A, McClelland P. Treatment of haemodialysis catheter-related infections. Nephrol Dial Transplant. 2002;17:1149–1150. doi: 10.1093/ndt/17.6.1149. [DOI] [PubMed] [Google Scholar]
- 8.Maya ID, Carlton D, Estrada E, Allon M. Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis. 2007;50:289–295. doi: 10.1053/j.ajkd.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 9.Allon M, Bailey R, Ballard R, Deierhoi MH, Hamrick K, Oser R, Rhynes VK, Robbin ML, Saddekni S, Zeigler ST. A multidisciplinary approach to hemodialysis access: prospective evaluation. Kidney Int. 1998;53:473–479. doi: 10.1046/j.1523-1755.1998.00761.x. [DOI] [PubMed] [Google Scholar]
- 10.Tanriover B, Carlton D, Saddekni S, Hamrick K, Oser R, Westfall A, Allon M. Bacteremia associated with tunneled dialysis catheters: comparison of two treatment strategies. Kidney Int. 2000;57:2151–2155. doi: 10.1046/j.1523-1755.2000.00067.x. [DOI] [PubMed] [Google Scholar]
- 11.Barth RH, DeVincenzo N. Use of vancomycin in high-flux hemodialysis: experience with 130 courses of therapy. Kidney Int. 1996;50:929–936. doi: 10.1038/ki.1996.393. [DOI] [PubMed] [Google Scholar]