Abstract
Previously researchers identified a behavioral profile that predicted treatment response of children with autism to a specific behavioral intervention, Pivotal Response Training (PRT). This preliminary investigation sought to refine this profile by obtaining six participants matching the original nonresponder profile on all but one of the profile behaviors (toy contact or avoidance) and then assessing their response to PRT. In addition, participants received a course of Discrete Trial Training (DTT) to determine whether the profile predicted child response to this intervention. Altering the original profile behavior of toy contact led to improved response to PRT while, altering the profile behavior of high avoidance had little impact on treatment response, and the profile was not predictive of response to DTT.
Keywords: Autism, Behavioral Intervention, Behavioral Profile, Early Intervention, Pivotal Response Training
The results of a growing amount of research show that with early behavioral intervention a large number of children with autism show substantial improvement (e.g., Howard, Sparkman, Cohen, Green, & Stanislaw, 2005; Sallows & Graupner, 2005; Cohen, Dickens, & Smith, 2006; Ben-Itzchak & Zachor, 2007; Eikeseth, Smith, Jahr, & Eldevik, 2007). The finding that early intervention can make a significant difference in treatment outcome presents us with the opportunity to greatly increase the overall positive outcome rate for these children. However, as has always been the case, there remains a good deal of variability in outcome in children with autism, even with the most supported evidence-based treatments. This variability in outcome suggests the necessity of understanding other variables, such as child characteristics, that act to affect treatment responsiveness. This would allow us to tailor treatment for specific children. This individualization of treatment has two distinct advantages. First, such individualization should increase the overall treatment effectiveness rate among children with autism. Second, given the importance of early intervention we want to be certain to apply the most effective treatment at the outset.
Sherer and Schreibman (2005) addressed the issue of child characteristics and identified a behavioral profile that successfully predicted child outcome to a specific naturalistic behavioral intervention, Pivotal Response Training (PRT). The profile included five behaviors: Toy contact, social approach, social avoidance, nonverbal self-stimulatory behavior, and verbal self-stimulatory behavior. (Interestingly, language, a behavior commonly cited as predictive of treatment outcome did not distinguish responders from responders in this study.) Those children who had the best outcome with PRT (“responders”) were those who exhibited comparatively high levels of toy contact, social approach, and verbal stereotypy and low levels of social avoidance, and nonverbal stereotypy. When provided the same type and intensity of treatment children who exhibited the opposite behavioral profile (“nonresponders”) showed no or minimal gains.
While Sherer and Schreibman (2005) offered a predictive profile for response to the PRT treatment, two main questions remained. First, is the profile specific? That is, does the profile predict treatment response to PRT in particular or to any treatment in general? Second, while it was demonstrated that the 5-behavior profile was predictive of PRT outcome it remains to be seen which (if not all) of the specific behaviors are required for the profile to be predictive. Therefore we wished to ascertain whether it was necessary, or even desirable, to base treatment decisions on the aggregate of all five behaviors in the original profile.
In the current preliminary investigation we studied 6 young children with autism whose assessed behavioral profile matched the Sherer and Schreibman (2005) “nonresponder” profile except for one behavior, either toy contact or avoidance. Screening of children with autism indicated that these were the most common profiles. Toy contact behavior was defined as the child appropriately interacting with a toy in the room for 5 or more consecutive seconds. Examples of toy contact behavior include the child pushing a car across the floor, manipulating puzzle pieces, looking at pictures in a book, or wrapping a baby doll in a blanket. Avoidance behavior was defined as the child moving away from the adult out of arms reach. Examples of avoidance behavior include the child pulling away from the adult’s touch, resisting eye contact when the adult is initiating a look, crawling under a table, or the child covering their eyes or ears in response to adult speaking. Examining toy contact and avoidance separately allowed us to determine the importance of these two individual behaviors on the predictive value of the profile. Further, to examine specificity, we assessed response to a more highly-structured form of behavioral intervention, Discrete Trial Training (DTT).
Method
Nonresponder screening
The behavioral profile (Sherer & Schreibman, 2005) was used to screen potential participants for responsiveness to PRT. Child behavioral profiles were determined through a structured laboratory observation that took place in a large treatment room containing a couch, a loveseat, 2 tables, and a one-way observation mirror. A standardized set of developmentally appropriate toys was available. Each child was observed for 15-min with their primary care provider. During the first 5-min the caregiver was asked not to initiate any interactions with the child, allowing observation of independent and spontaneous behaviors. During the second 5-min the caregiver attempted to elicit language from the child. During the third 5-min the caregiver attempted to engage the child in play. The entire 15 minutes were then coded for the occurrence of the profile behaviors: toy contact, social approach, social avoidance, nonverbal self-stimulatory behavior, and verbal self-stimulatory behavior. See Table 1 for behavioral definitions of profile behaviors.
Table 1.
Behavioral Definitions for Response Profile
| Profile Behavior | Definition |
|---|---|
| Toy Contact | The child interacts with a toy in the room appropriately for 5 or more consecutive seconds. |
| Approach Behavior | The child moves to within arms reach of the adult. Examples include spontaneously looking at adult’s face, reaching to the adult, or approaching to take a toy. |
| Avoidant Behavior | The child moves away from the adult out of arms reach. Examples include the child pulling away from the adult’s touch, resisting eye contact when the adult is initiating a look, crawling under a table, or the child covering eyes or ears in response to adult speaking. |
| Verbal Self- Stimulatory Behavior | The child emits nonsensical sounding utterances; these may include long and short utterances, may be high pitched screams not associated with a tantrum, repetitive sounds, and will vary from child to child. |
| Nonverbal Self-Stimulatory Behavio | Varies from child to child; examples include hand-flapping, rocking, facial grimacing, head shaking, jumping up and down, and body posturing. |
Participants
Participants were 6 children with autism between the ages of 2 and 4 years. Each child had a diagnosis of Autistic Disorder, provided by an outside professional, according to the criteria of the American Psychiatric Association DSM-IV (APA, 1994). Diagnoses were confirmed using the Autism Diagnostic Interview, Revised (ADI-R, Lord, Rutter & Le Couteur, 1994) and the Autism Diagnostic Observation Schedule (ADOS, Lord, Rutter, DiLavore & Risi, 1999).
Three of the children (Joey, Kevin, and Lisa) matched the nonresponder profile on all categories except toy contact, indicating that they interacted with many toys during the assessment. Their behavior matched the nonresponder profile in all other areas. The other 3 children (George, Nathan, and Chris) matched the nonresponder profile on all categories except avoidance, indicating that they were less avoidant of adults who approached them than the children in the other group. This group of children also met the nonresponder profile in all other areas of the profile.
Additional assessments were administered by the authors and included: the Childhood Autism Rating Scale (CARS, Schopler, Reichler & Renner, 1988), the Vineland Adaptive Behavior Scales (VABS, Sparrow, Balla & Cicchetti, 1984), the Bayley Scales of Infant Development, 2nd Ed. (Bayley, 1993), and the MacArthur Communicative Developmental Index (Fenson, et al., 1993). Children in both groups had similar levels of cognitive and adaptive functioning and autism severity, with the exception of George who had lower cognitive and adaptive skills and higher CARS scores, indicating greater impairment. The children in the low avoidance group were slightly older than the children in the high toy contact group (see Table 2).
Table 2.
Participant Demographics
| Child | Chronological Age (mo) | Nonverbal MA- Bayley (mo) | CARS | Vineland Adaptive Behavior Composite (standard score) | Profile Behavior NR profile except for: |
|---|---|---|---|---|---|
| Joey | 28 | 13 | 31 | 71 | Toy Contact |
| Kevin | 26 | 12 | 33.5 | 61 | Toy Contact |
| Lisa | 24 | 16 | 36.5 | 70 | Toy Contact |
| Mean | 26 | 13.67 | 33.67 | 67.33 | |
| George | 47 | 11 | 40.5 | 51 | Avoidance |
| Nathan | 31 | 15 | 31.5 | 60 | Avoidance |
| Chris | 26 | 12 | 33 | 69 | Avoidance |
| Mean | 34.67 | 12.67 | 35 | 60 |
Baseline
We employed a single-subject multiple baseline design across participants. As noted by Yoder and Compton (2004) single-subject designs are particularly well-suited to examining individual response to treatment and thus helpful towards identifying predictors of treatment effectiveness. During baseline, children attended sessions in the laboratory 3 days a week for 2 hours each day. Baseline sessions ranged from 1 to 6 weeks, and consisted of the child playing alone with a therapist in a treatment room containing a variety of toys to which the child had free access. The therapist provided the child with an opportunity to respond on average once per minute (e.g., “Chris, what do you have?” or “Do you want this ball?”), however, no consequences were provided contingent upon the child’s behavior.
Independent Variables
Pivotal Response Training (PRT)
PRT is a naturalistic, play-based, child-directed behavioral intervention designed to enhance the child’s motivation and responsivity to the environment (Koegel, Schreibman, Good, Cerniglia, Murphy & Koegel, 1989). Key components of PRT that have been shown to increase motivation (Koegel & Egel, 1979; Koegel, Dyer & Bell, 1987; Koegel & Williams, 1980; O’Dell, Dunlap & Koegel, 1983; O’Dell & Koegel, 1981) include: providing a clear instruction or question relevant to the task, interspersal of maintenance (already mastered) tasks among more difficult (acquisition) tasks, following the child’s lead and using toys or activities the child chooses, using reinforcers directly related to the child’s response, reinforcing goal directed attempts, and taking turns with the toys. The treatment goal of this study was to increase expressive verbal communication skills. Children in this study had few vocalizations so the therapist began with the reinforcement of any vocalizations, followed by reinforcement of contingent vocalizations, and reinforcement of specific sound imitation. For a more comprehensive description of PRT see Koegel et al., 1989 http://www.education.ucsb.edu/autism/behaviormanuals.html.
Discrete Trial Training (DTT)
DTT is a highly structured behavioral treatment that breaks down target behaviors into smaller components and trains these components one at a time. Training procedures and curricula were implemented for each child based on Behavioral Intervention for Children with Autism (Maurice, Green, & Luce, 1997). The main components included: providing a clear discriminative stimulus, providing graded levels of prompting (systematically faded from most to least restrictive), waiting for a child’s response (or lack of response) and providing an appropriate consequence (positive or neutral). Intertrial intervals of 5–10 seconds were used.
The curriculum involved introductory DTT programs, including eye contact (for 1 second, for 5 seconds, while playing, from a distance, and in response to “look at me”), gross motor imitation (“clap hands”, “wave”, “place arms up”, “shake head”, “tap knees”, and “tap head”), imitation with objects (“roll car”, “blocks in container”, “ring bell”, “shake maraca”, “hold phone to ear”, “hammer peg”, and “scribble with crayon”), one-step instructions (“stand up”, “sit down”, “come here”, “wave bye-bye”, and “give me five”), and verbal imitation (increasing any vocalization, bringing vocalizations under temporal control, and imitation of sounds). Although it was not consistent with the curriculum order, we included a verbal imitation task for each child in order to compare DTT and PRT more directly in this area. All children spent approximately the same percentage of DTT treatment time completing drills in each curriculum area: eye contact (M=19% range=16–21%); gross motor imitation (M=20% range=18–23%); one-step instructions (M=20%; range=16–25%); object imitation (M=20%; range=19–22%) and verbal imitation (M=20%; range=18–23%). Tasks were considered mastered once a child completed the task with at least 80% accuracy across two teaching blocks of 10 trials each. Tasks were dropped if the child did not make progress on the task after 10 teaching blocks of 10 trials each at the same prompt level.
Procedure
Children were screened using the profile and assessments. Each participant had a differing length of baseline. Once baseline was completed, each child received 18 hours of PRT. This time period was chosen based on previous data indicating that children who respond well to PRT demonstrate some clear positive response by that time period (Sherer, 2002). Materials for PRT included toys the participants enjoyed and varied based on child preference. Preference for specific toys was determined by providing choices to the child and/or following the child to toys chosen spontaneously. Once children completed PRT, they entered DTT. Materials used for DTT varied based on the programs, but typically included familiar objects and both edible and tangible reinforcers. The first 2 participants received 18 hours of DTT. However, we had some concerns that this was not enough time to see an effect of treatment, therefore the remaining participants received 36 hours of DTT. For both conditions, children received treatment in the laboratory 3 days a week for 2 hours each day until they reached 18 or 36 hours of treatment. Treatment was provided by trained undergraduate students blind to the study hypotheses. All sessions were videotaped.
Once both PRT and DTT training were completed, the profile assessment was readministered. One of the children, Nathan, had a profile shift and after treatment met criteria as a responder to PRT. In order to further investigate the sensitivity of the profile, Nathan received an additional 36 hours of PRT. Two children whose profiles did not change after both treatment phases, Lisa and Chris, also received an additional 36 hours of PRT.
Dependent Measures
Communication
Contingent communication was coded for all children. Spontaneous vocalizations were defined as instances where the child used appropriate vocalizations with communicative intent separated from both a verbal and non-verbal cue by more then 7 seconds. Cued vocalizations were defined as instances where the child verbally responded to the therapist’s verbal prompt or nonverbal cue (e.g. pointing to or tapping a desired object). This category included immediate echolalia. The definitions were identical to those used by Sherer and Schreibman, (2005) excepting that immediate echolalia, verbally and nonverbally cued speech were collapsed into one category. Five minutes (chosen randomly) of each 20 minute-session were coded by trained undergraduate students. Behaviors were scored in 10-sec intervals for occurrence/non-occurrence of each behavior. Behavior is reported as percent occurrence.
DTT Program Mastery
Trial-by-trial data were collected during DTT sessions. Both number of tasks each child mastered and number of tasks dropped from each child’s program were recorded.
Interrater Reliability
Undergraduate students naïve as to the purpose and hypotheses of the study were trained to score the videotaped sessions based on the communication definitions described above. Thirty-three percent of all sessions were scored for interobserver agreement and calculated based on the percent of agreements divided by the sum of agreements and disagreements. Raters were required to maintain at least 80% reliability. Interobserver agreement for cued vocalizations was 84% occurrence (range = 71%–97%) and 99% nonoccurrence (range = 98%–100%). For spontaneous vocalizations, interobserver agreement was 67% occurrence (range = 53%–67%) and 99% nonoccurrence (range = 97%–100%). Using Cohen’s kappa coefficient (k) to control for chance, reliability coefficients were: cued vocalizations kappa =.90 (range =.86 –.98) and for spontaneous vocalizations kappa =.81 (range =.75 –.95).
Fidelity of Implementation
All therapists were trained in PRT and DTT by the authors. To assess fidelity of implementation of each treatment, undergraduate therapists were rated by naïve coders after every 10 hours of treatment they provided. Therapists were required to demonstrate 80% correct implementation of all components of PRT or DTT before providing treatment. Thirty-three percent of sessions were scored for treatment implementation based on definitions developed in the Autism Research Laboratory (available from the authors). Trial by trial data were collected on the specific components of either DTT or PRT during a random 10 min period of treatment. All therapists met and maintained 80% accuracy for both treatments.
Results
Communicative Behavior
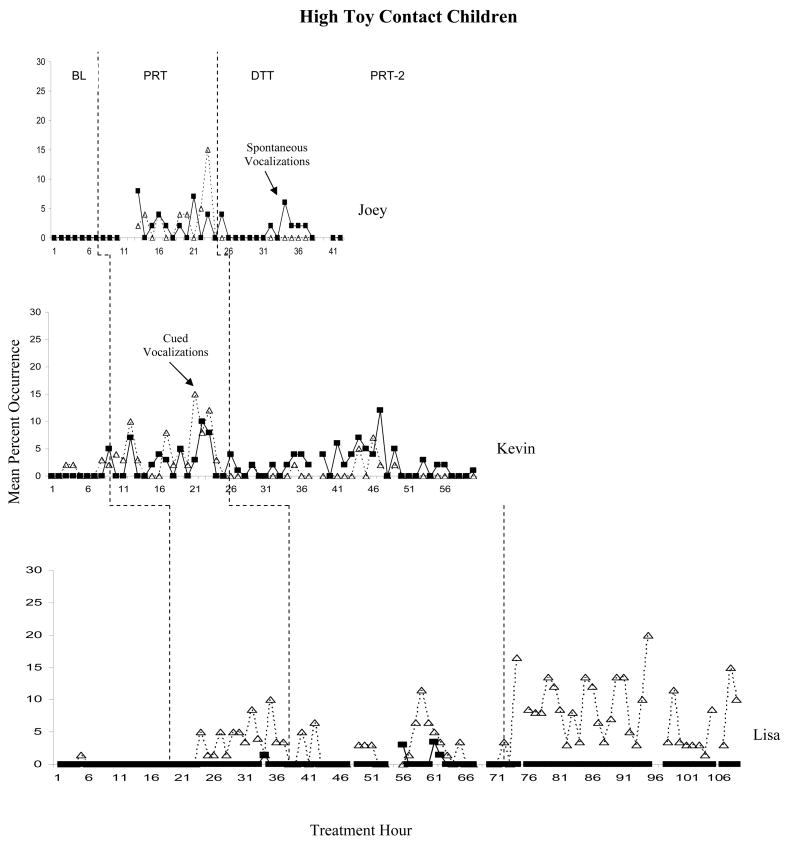
Figure 1 presents data for the children who had high toy contact. (Missing data points in all graphs are due to technical difficulties resulting in no sound recording.) Depicted are each child’s vocalizations, both spontaneous and cued, throughout the course of both treatment procedures (None of the children exhibited echolalia.). None of the children exhibited any spontaneous, purposeful vocalizations during baseline. Kevin and Lisa both had minimal instances of cued vocalizations, while Joey had none. After 18 hours of PRT Joey was engaging in some vocalization, although typically this occurred in fewer than 10% of intervals. Joey had only limited vocalization during DTT. Kevin began to vocalize soon after PRT training began, and was engaging in both spontaneous and cued vocalizations during 10–12% of intervals by the end of PRT training. Vocalizations decreased somewhat during DTT, however they remained higher than baseline levels. Lisa began to engage in some cued vocalizations after approximately 5 hours of PRT. She continued to have some cued verbal responding during DTT. During her second PRT trial her cued vocalizations increased to approximately 10–15% of intervals.
Figure 1.
Percent occurrence of cued and spontaneous vocalizations across Baseline, PRT, DTT and PRT2 (Lisa only) for high toy contact children.
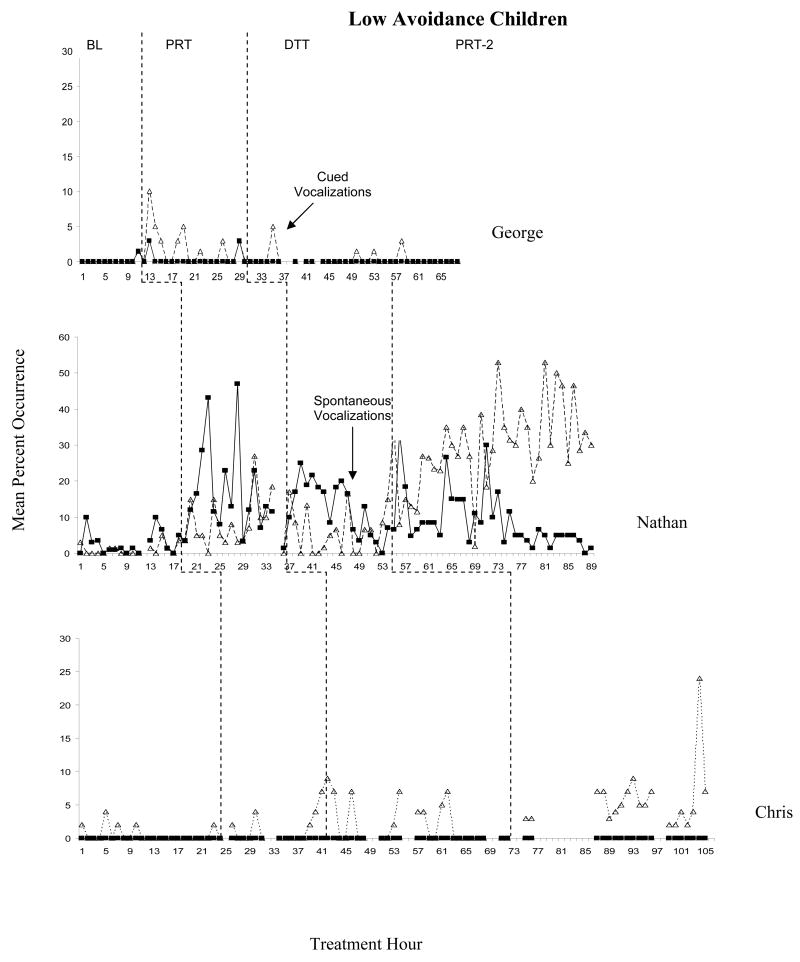
Vocalizations for the children who had low avoidance are presented in Figure 2. George and Chris had few vocalizations during baseline. George had minimal response to PRT, exhibiting only a few cued vocalizations during training. In general, his purposeful vocalizations did not increase in either PRT or DTT. Chris also had some minimal response to PRT in terms of cued vocalizations. He exhibited limited cued vocalizations during DTT. During his second PRT session, he continued to engage in cued vocalizations for fewer than 10% of intervals except on one occasion.
Figure 2.
Percent occurrence of cued and spontaneous vocalization across Baseline, PRT, DTT and PRT2 (Nathan and Chris only) for low avoidance children.
Nathan (see Figure 2, note differing scale on the y axis) had a different response to treatment. First, he engaged in more purposeful, spontaneous vocalizations during his baseline sessions than any of the other children. Second, his response to PRT was substantial, as both his spontaneous and cued vocalizations increased from the beginning of training. He continued to vocalize during 10–20% of intervals in DTT. During his second PRT trial (after he met the responder profile criteria) his ability to imitate language sounds increased dramatically. Nathan used several words during his second PRT phase; however these were limited to fewer than one word per session and are not depicted on the figure.
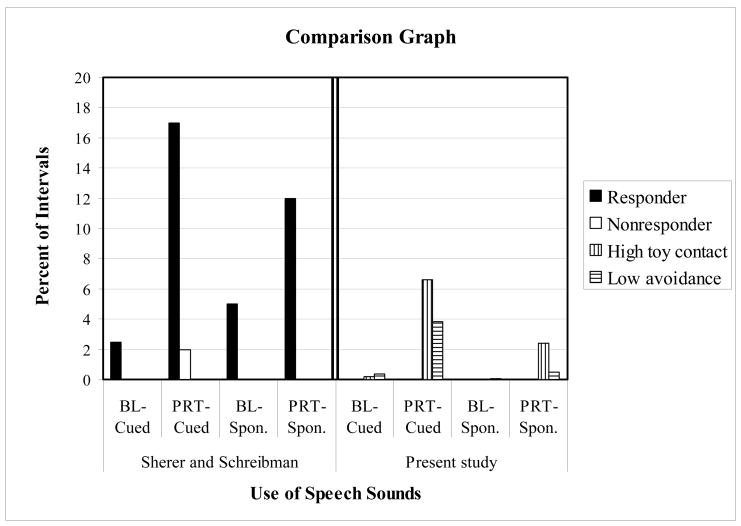
To determine overall level of responding of our present participants in relation to the responding of children in the original Scherer and Schreibman (2005) study, we compared level of responding after 18 hours of PRT. Responding for all of the children was averaged over the baseline period and the last three hours of PRT treatment (see Figure 3). Nathan’s data are not included in this figure due to his positive response to PRT which was not consistent with the other two children in his group. Data indicate that the responder group from the original study clearly showed enhanced response over the nonresponder group in the original study. Children in the present study (except Nathan) engaged in very few cued or spontaneous vocalizations during baseline. After 18 hours of PRT the children in both groups showed some minimal response to PRT (between that shown by the original responder and nonresponder groups) with high toy contact engaging in slightly more cued and spontaneous vocalizations. Nathan responded well to PRT.
Figure 3.
Group comparison of cued and spontaneous vocalizations for children in the current study and children in the original Sherer & Schreibman (2005) study. Average performance during Baseline and the last 3 hours (of 18 hours total) of PRT.
Discrete Trial Training
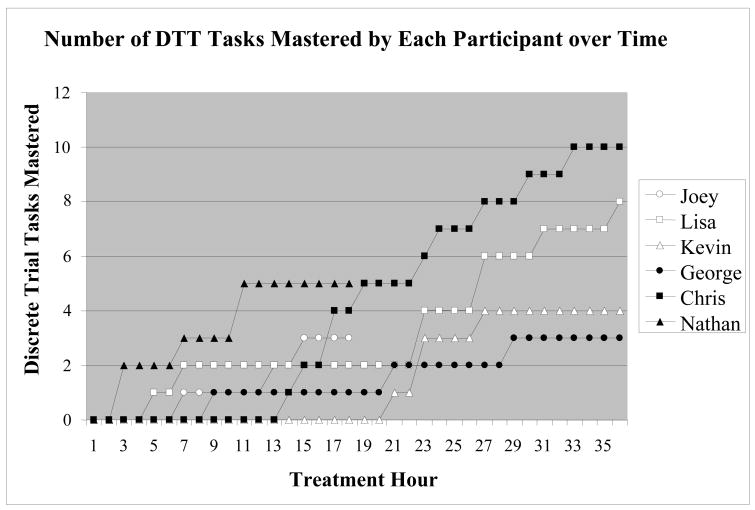
The PRT profile did not appear to predict response to DTT. For the three children who had higher toy play, after 18 hours of treatment Lisa mastered two DTT tasks (one-step instructions “sit down” and verbal imitation “any sound in 5 seconds”) and Joey mastered three DTT tasks (one-step instructions, “sit down” and “stand up” and imitation with an object, “roll car”). Kevin did not master any tasks after 18 hours (see Figure 4). Kevin did go on to master four tasks (one-step instructions “stand up” and “come here” and verbal imitation “any sound” and the sound “ba”) by 36 hours of treatment, and Lisa mastered six more tasks (one-step instructions “tap knees”, “stand up”, “come here”, and “give me five”; and imitation with objects “blocks in container” and “bang hammer”) in that time.
Figure 4.
Number of mastered tasks across 18–36 hours of DTT for all participating children.
The PRT profile also did not predict response to DTT for the low avoidance children. After 18 hours of DTT Nathan mastered five tasks (eye contact for 1 second, eye contact for 3 seconds, imitation with an object “roll car” and “ring bell”, and verbal imitation of any sound in 3 seconds), George one task (one-step instruction “sit down”) and Chris four tasks (eye contact for 1 second; one-step instruction “sit down”; imitation with objects “roll car” and “blocks in container”). After 36 hours of treatment, George mastered a total of two more tasks (gross motor imitation “clap hands”; and imitation with an object “blocks in container”) and Chris six more tasks (eye contact for 2 seconds; gross motor imitation “clap hands”; one-step instruction “stand up”, and “come here”; imitation with objects “ring bell”, and “phone to ear”). Three tasks were dropped from Lisa’s program. Two tasks were dropped from both George’s and Kevin’s programs. One task was dropped from Nathan’s program.
Discussion
The results of this preliminary study suggest that the predictive behavioral profile identified by Sherer and Schreibman (2005) is specific to PRT in that it did not predict responsiveness to another, more highly-structured, behavioral intervention, DTT. This was the case even though the children did not meet all of the behavioral criteria of the original study. Nathan showed a substantial positive response to PRT (especially after his profile changed to a “responder”), yet his response to DTT was very similar to that of Chris, who had almost no response to PRT. Similarly, Kevin took a good deal of time to show any response to DTT even though he had the best response to PRT of the three children with high toy contact.
Children with a high interest in toy contact, as a group, performed better than children who did not have an interest in toys (excluding Nathan). One limitation is that George may have responded differently due to more severe symptoms as evinced by his slightly older chronological age, more severe CARS scores, and lower adaptive behavior scores. However, it does seem clear that PRT may be a helpful component of a child’s program for children interested in objects. The profile is robust in that these children did not do as well as children identified as “responders” in all areas in the original study and might be characterized as minimal responders. These children may take longer to respond to PRT. It may be that object interest is a key characteristic for treatment responders. In contrast, low social avoidance did not appear to help children respond to PRT. This group performed essentially identically to the nonresponders in the original study, suggesting that low avoidance is not a behavior that can compensate for other areas that predict reduced response to PRT. We did have one case, Nathan, who appeared to respond very differently from the other children. Nathan was highly avoidant upon beginning treatment. He had been cared for exclusively in the home and did not have a great deal of exposure to new people or environments. Once he became used to the setting (which took several weeks) he became more interested and interactive. It is possible that his extreme difficulty adjusting to the environment affected the original assessment. Therefore, in practice, it is important to reassess children as their behavior changes.
This investigation is best considered preliminary because of several limitations. First, because of our desire to replicate the original profile prediction for PRT, all participants were exposed to this condition first. Thus we have a possible order effect. We did introduce a return to PRT for three of the participants however the data do not lead to easy interpretation. Second, the short time for the intervention does not allow us to determine effects that may have occurred over a longer period of treatment. Third, we cannot directly compare vocalizations during PRT and DTT since the DTT programs often did not include verbal tasks. Finally, one participant, George, had more severe deficits than other participants. His did not appear to benefit greatly from either treatment method, although he did eventually master several DTT programs. His data provide information regarding treatment response for more severely affected children, but the differences between his pre-treatment skills and those of the other participants should be noted when interpreting the results.
The overall purpose of the present investigation was to provide more detailed understanding of the predictive properties of a particular behavioral profile in the hopes of refining the utility of such a profile. The possibilities for increasing our ability to provide individualized intervention for young children merit such investigation. While we are in the infancy of such research, we are hopeful that continued work in this area will greatly increase the overall effectiveness of our treatments for children with autism.
Acknowledgments
This research was funded by a research grant from the Doug Flutie, Jr. Foundation and the Autism Society of America. The authors would like to thank the families of the children with autism who participated in this project, and the students who assisted with videotaped coding.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Bayley N. Bayley scales of infant development. 2. San Antonio, Tx: Harcourt Brace & Co; 1993. [Google Scholar]
- Ben-Itzchak E, Zachor DA. The effects of intellectual functioning and autism severity on outcome of early behavioral intervention for children with autism. Research in Developmental Disabilities. 2007;28:207–303. doi: 10.1016/j.ridd.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Cohen H, Amerine-Dickens M, Smith T. Early intensive behavioral treatment: Replication of the ucla model in a community setting. Journal of Developmental and Behavioral Pediatrics. 2006;27:S145–S155. doi: 10.1097/00004703-200604002-00013. [DOI] [PubMed] [Google Scholar]
- Eikeseth S, Smith T, Jahr E, Eldevik S. Outcome for children with autism who began intensive behavioral treatment between ages 4 and 7: A comparison controlled study. Behavior Modification. 2007;31:264–278. doi: 10.1177/0145445506291396. [DOI] [PubMed] [Google Scholar]
- Fenson L, Dale PS, Reznick JS, Thal D, Bates E, Hartung JP, et al. MacArthur Communicative Development Inventories: User’s guide and technical manual. San Diego: Singular Publishing Group; 1993. [Google Scholar]
- Howard JS, Sparkman CR, Cohen HG, Green G, Stanislaw H. A comparison of intensive behavior analytic and eclectic treatments for young children with autism. Research in Developmental Disabilities. 2005;26:359–383. doi: 10.1016/j.ridd.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Koegel RL, Schreibman L, Good AB, Cerniglia L, Murphy C, Koegel LK. How to teach pivotal behaviors to autistic children. University of California; Santa Barbara: 1989. [Google Scholar]
- Koegel RL, Dyer K, Bell LK. The influence of child preferred activities on autistic children’s social behavior. Journal of Applied Behavior Analysis. 1987;20:243–252. doi: 10.1901/jaba.1987.20-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel RL, Egel A. Motivating autistic children. Journal of Abnormal Psychology. 1979;88:418–426. doi: 10.1037//0021-843x.88.4.418. [DOI] [PubMed] [Google Scholar]
- Koegel RL, Williams J. Direct vs. indirect response-reinforcer relationships in teaching autistic children. Journal of Abnormal Child Psychology. 1980;4:536–547. doi: 10.1007/BF00916505. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 1999. [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Maurice C, Green G, Luce SC, editors. Behavioral intervention for young children with autism: A manual for parents and professionals. Austin, TX, US: PRO-ED, Inc; 1996. [Google Scholar]
- O’Dell MC, Dunlap G, Koegel RL. The importance of reinforcing verbal attempts during speech training with nonverbal children. Paper presented at the Annual convention of the American Psychological Association; Los Angeles, CA. 1983. [Google Scholar]
- O’Dell MC, Koegel RL. The differential effects of two methods of promoting speech in nonverbal autistic children. Paper presented at the American Speech-Language-Hearing Association; Los Angeles, CA. 1981. [Google Scholar]
- Rogers SJ. Brief report: early intervention in autism. Journal of Autism and Developmental Disorders. 1996;26:243–246. doi: 10.1007/BF02172020. [DOI] [PubMed] [Google Scholar]
- Sallows GO, Graupner TD. Intensive behavioral treatment for children with autism: Four-year outcome and predictors. American Journal on Mental Retardation. 2005;110:417–438. doi: 10.1352/0895-8017(2005)110[417:IBTFCW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Sherer M. Individual behavioral profiles and predictors of treatment effectiveness for children with autism. Unpublished doctoral dissertation, University of California; San Diego: 2002. [DOI] [PubMed] [Google Scholar]
- Scherer MR, Schreibman L. Individual behavioral profiles and predictors of treatment effectiveness for children with autism. Journal of Consulting and Clinical Psychology. 2005;75:525–538. doi: 10.1037/0022-006X.73.3.525. [DOI] [PubMed] [Google Scholar]
- Schopler E, Reichler RJ, Renner B. Western Psychological Services. 1988. The Childhood Autism Rating Scale. [Google Scholar]
- Sparrow S, Balla D, Cicchetti D. Vineland scales of adaptive behavior: Interview Edition, Survey Form. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- Yoder P, Compton D. Identifying predictors of treatment response. Mental Retardation and Developmental Disabilities Research Reviews. 2004;10:162–168. doi: 10.1002/mrdd.20013. [DOI] [PubMed] [Google Scholar]