Abstract
Purpose
To examine if custom wavefront-guided soft contact lenses provide visual and optical performance equivalent to habitual gas permeable (GP) corrections in three keratoconus subjects.
Methods
Custom wavefront-guided soft contact lenses were produced and evaluated at the Visual Optics Institute, College of Optometry, University of Houston for three habitual GP-wearing keratoconus subjects. Photopic high and mesopic low contrast logMAR visual acuity and residual 2nd–10th order optical aberrations experienced with these custom soft lenses were recorded and compared to the subjects’ habitual GP correction.
Results
All three subjects wearing custom soft lenses reached the established exit criterion of photopic high contrast logMAR VA equal to or better than values recorded with their habitual GP lens. High contrast logMAR VA for GP and custom soft lens correction was 0.01±0.05 and 0.00±0.02 for KC1, 0.20±0.02 and 0.14±0.02 for KC2 and 0.04±0.09 and −0.05±0.05 for KC3 respectively. Additionally, KC2 reached the exit criterion of high order aberration levels equal to or less than values with their habitual GP lens (GP lens: 0.394 ± 0.024μm, custom lens: 0.381 ± 0.074μm).
Conclusions
Custom wavefront-guided soft contact lenses have been demonstrated to provide equivalent photopic high contrast logMAR VA to that achieved with habitual GP correction in three keratoconus subjects. Future emphasis will be placed on surpassing habitual GP performance and reaching a normal age-matched criterion for both visual acuity and aberration measures. Achieving these goals may require a more thorough understanding of the relationship between visual performance and residual aberration experienced during custom lens wear through the use of image quality metrics predictive of visual performance.
Keywords: keratoconus, Zernike, wavefront, wavefront-guided, soft contact lens, rigid contact lens, aberration
Elevated levels of both lower and higher order aberrations present in the eye disease keratoconus make it difficult for subjects to achieve excellent optical and visual performance with traditional soft contact lenses or spectacles. Consequently, rigid contact lenses have become the current gold standard for the correction of keratoconus, with approximately 65% of keratoconus subjects being fitted with some form of rigid lens correction in both eyes.1 Rigid lenses reduce unwanted aberrations where conventional soft lenses and spectacles fail due to the ability of the rigid lens to maintain its shape during wear. This results in the formation of a tear lens between the aberrated cornea and rigid lens which masks a portion of the aberration present in these highly aberrated eyes. However, prescribing a rigid lens may not decrease higher order aberration to normal levels, and the elevated levels of residual aberration may continue to have a negative impact on visual performance.2–4
Simulation work in the area of customization has demonstrated that customized correction of lower and higher order aberrations in the keratoconic eye would be beneficial, and that this benefit would remain in the presence of typical lens movements.5–8 Simulation has also been used in an effort to determine what subset of optical aberrations is visually significant in keratoconus. Earlier simulation work by this research group demonstrated that correction of aberration through the 5th radial order may return visual performance in the majority of keratoconic subjects to near-normal levels.9
Work from multiple laboratories has demonstrated that the technology exists to implement both high and low order optical corrections in a custom wavefront-guided soft contact lens modality.10–13 Further, the use of custom soft lenses to treat the aberrations in keratoconus subjects has demonstrated both the hypothesized reduction of lower and higher order aberrations in keratoconic eyes and a resulting visual benefit for the patient.11,12 These previous demonstrations compared custom soft contact lens performance to second order corrections for three subjects as well as to one subject’s habitual gas permeable (GP) correction11 and to one subject’s habitual soft contact lens correction.12 In the current report, the clinical relevance of custom wavefront guided soft contact lenses is investigated by comparing custom wavefront-guided soft contact lens performance to performance achieved with GP lens performance in three keratoconus subjects.
METHODS
University Institutional Review Board and informed consent approvals were obtained prior to initiating data collection. One eye of three GP wearing subjects with clinically diagnosed keratoconus was included in this custom soft contact lens study. General information including steep simulated keratometry measurements (Sim Ks), disease severity and corneal toricity were recorded over the central 7mm on the Keratron corneal topographer (Optikon, Rome Italy).
A series of custom soft contact lenses was designed and produced for each of the 3 eyes enrolled in the study. The goal of the initial lens in the series (L0) was to provide a soft contact lens correction that targeted the majority of the patient’s second order aberrations. Each baseline soft lens had a custom toric posterior surface defined by the subject’s corneal astigmatism determined from topography, a spherical anterior surface whose spherical power was determined from the subject’s habitual correction and prism ballasting to minimize rotation. This design philosophy targets low order aberrations and stabilizes the lens allowing future lens iterations to focus on intelligently correcting any residual low order aberrations as well as high order aberrations. Three alignment marks were placed on the anterior surface of each lens (one at each 0°, 180° and 270°) to facilitate monitoring of lens orientation. Marks were placed on the lens surface using a computer controlled pneumatic boring tool integrated into the manufacture process. If the lens was stable on the eye and fit properly, the macro lens properties (base curve, posterior astigmatic axis, posterior astigmatic magnitude, prism, edge radius) of L0 were conserved in successive lens designs. If the lens was not stable, did not fit properly or did not correct the bulk of lower order aberration terms, changes were made to the macro properties of the lens.
After insertion of any given lens (Lx), the subject was given 15–20 minutes for lens equilibration. The lens was examined on-eye to assure adequate lens movement, centration, coverage and relocation after blink. Rotation and translation of a custom lens Lx on the eye were determined by quantifying the position of the three alignment marks on the anterior surface of the eye relative to the pupil center using a slit lamp with an incorporated digital camera. This slit lamp used a conventional Zeiss (Jena, Germany) 20 SL slit lamp base, ImagingSource (Charlotte, NC) DMK 21F04 monochromatic video camera with Cosmicar B2518 lens, ImagingSource 5mm extension tube and IC Capture 2.0 (Charlotte, NC) image processing software for the recording of images of the custom lens on the eye. Up to 20 images were captured (one every 30 seconds for 10 minutes). These digital images were processed with UTHSCSA (San Antonio, TX) ImageTool 3.0 image processing software, resulting in rotation and translation data for the lens in each image in the series. The rotation and translation data was digitally stored and processed using a custom Matlab program to determine the average rotation, x-displacement and y-displacement (Δθ, Δx, Δy) of the lens relative to the pupil center over the given time interval.
Guirao et. al. have demonstrated that in the presence of rotations and translations, partial correction of all aberration terms can yield improvements in optical quality superior to those experienced when a full correction is implemented.14 In this method, a partial correction ( , ranging from 0 to 1) is applied to each Zernike term. The value of is determined mathematically as a function of translation, rotation, pupil size radial order and angular frequency.
The definition of a custom wavefront-guided aberration structure (ASx where x>0) to cut into lens Lx, was accomplished in the following manner. Five separate wavefront measurements were recorded through the 10th radial order with lens Lx-1 on the eye. Data were collected with a COAS HD wavefront sensor (Wavefront Sciences, Albuquerque, NM). The operator realigned the wavefront sensor to the subject between each measurement. The average of each term across the 5 measurements was calculated over the largest common pupil size and defined the residual wavefront aberration (WFx-1) of the eye/Lx-1 system.a. WFx-1 was then mathematically combined with ASx-1, the Zernike coefficients describing the cut pattern of lens Lx-1 and scaled by , which optimized the magnitude of each Zernike aberration term based on the movement of Lx-1. This new quantity, ASx, defined the cut pattern in lens Lx.
The posterior surface and edges of each lens (Lx) were designed and cut using a standard DAC International posterior-side contact lens algorithm. Design of all aspects of the anterior surface of the lenses (which included the aberration structure ASx) was accomplished using a custom Matlab program written by the authors at the University of Houston, College of Optometry. This design was converted into a part file and implemented on the DAC 2X-ALM using custom software written for UHCO by DAC International. Lenses were implemented in BENZ (Sarasota, FL) Methafilcon A contact lens material, sent to Metro Optics (Austin, TX) for hydration, sterilization and packaging and then returned to UHCO for testing.
Subjective over-refraction was recorded with the habitual GP correction in place. This over-refraction quantified sphere and cylinder present for the subjects under habitual conditions. Visual performance testing was conducted on the subject’s GP correction as well as each custom lens produced in the study. Both photopic high contrast (PHC) and mesopic low contrast (MLC) visual acuity measurements were collected. All acuity charts were generated using Visual Optics Laboratory (VOL v-6.89, Sarver and Associates, Carbondale IL). Contrast was quantified using a LS-110 luminance meter (Minolta, Tokyo Japan). The contrast level of the LC charts used was the lowest testable contrast level where the subject read at least 10 letters with their habitual correction. The Weber contrast level of the HC charts was constant at 91%. In summary, visual acuity data were recorded through the contact lens and physiological pupil with head stabilized in the UHCO HeadSpot forehead and chin rest (UHCO technical services, Houston, TX). Each eye read each acuity chart until five letters were missed. The number of letters correctly identified up to the fifth miss was recorded. The average number of letters correct for the three trials was calculated and the corresponding logMAR visual acuity recorded.15–17 After visual performance testing was complete with each custom contact lens, the lens was removed and optically profiled in a ClearWave contact lens aberrometer (Wavefront Sciences, Albuquerque NM). This device is a specialized Shack Hartmann Wavefront Sensor capable of quantifying and reporting the Zernike aberration structure of the custom soft contact lens.
The purpose of the study was to examine if custom wavefront-guided soft contact lenses manufactured using this process can provide equivalent visual and optical performance as habitual gas permeable (GP) corrections in keratoconus. To examine this, exit criteria for the study were established as 1) a subject reached high-contrast logMAR visual acuity levels with a custom wavefront-guided soft contact lens that was equal or superior to their habitual GP correction 2) a subject obtained higher order aberration levels equal or lower than their habitual GP correction or 3) three custom lenses were implemented and neither exit criteria 1) nor 2) was achieved. All subjects (KC1–KC3) were clinically diagnosed keratoconus subjects who habitually wear GP lenses, and custom lens performance was compared to the subject’s habitual GP-corrected performance. Student’s t-test was used to compare the performance for the exit criterion reached with the custom lens to that of the habitual correction.
RESULTS
Table 1 reports the general subject information of age, eye studied, steep simulated keratometry measurements (Sim Ks) from corneal topography, corneal toricity and corneal anomalies recorded at the slit lamp. Subjects are listed in order of increasing steep K measurements. Table 2 contains the subjective over-refraction obtained for the three subjects while wearing GPs.
Table 1.
Reports the age, eye under study, steep keratometry measurement (K), corneal toricity and corneal anomalies recorded at the slit lamp.
| Subject | Age (yrs) | Eye | Steep K (D) | Corneal Toricity (D) | Corneal Anomalies |
|---|---|---|---|---|---|
| KC1 | 56 | OD | 45.18 | 1.25 | mild paracentral sub-epithelial opacity |
| KC2 | 50 | OS | 48.03 | 3.41 | None |
| KC3 | 28 | OS | 55.45 | 3.66 | sub-epithelial scar 0.3mm inferior/nasal |
Table 2.
Reports the subjective refractive error for each subject while wearing the habitual GP correction.
| Subject | Type of Habitual Correction | Subjective Over- Refraction SPEC: sph(D) cyl(D) ax(°) |
|---|---|---|
| KC1 | GP | −0.50 |
| KC2 | GP | +0.50 −0.50 022 |
| KC3 | GP | +0.75 −1.00 078 |
Table 3 contains the macro lens design parameters for each custom lens studied. While the goal was to hold macro lens parameters constant for any given subject, two modifications were made to macro lens parameters in this study based on examination of the lens on the eye. First, an increase of prism from 1.50 to 1.75 prism diopters in the series for KC2 was implemented in an attempt to better stabilize the rotational characteristics of one lens for KC2. Second, an increase in power from −9.60D to −16.5D was implemented for KC3 after noting a severe under-correction of myopia in lens L0. Table 3 also contains the number of Zernike orders integrated into the correction. L0 for each subject contains 2nd order correction. L1 for KC1 and KC2 incorporate 2nd–5th order correction using the method of Guirao as described above. Lens L1 for KC3 contains only custom 2nd order correction.
Table 3.
Displays the design variables Zernike orders corrected, base curve (mm), diameter (mm), posterior toric power (D), prism ballast (Δ) and anterior sphere power for each lens studied.
| Subject | Lens Iteration | Zernike Orders Corrected | Base Curve (wet,mm) | Diameter (wet,mm) | Posterior Toric Power (wet,D) | Prism (Δ) | Anterior Sphere Power (wet,D) |
|---|---|---|---|---|---|---|---|
| KC1 | L0 | 2 | 8.30 | 14.50 | −1.23 | 1.50 | −3.95 |
| L1 | 5 | 8.30 | 14.50 | −1.23 | 1.50 | −3.95 | |
|
| |||||||
| KC2 | L0 | 2 | 8.30 | 14.50 | −3.47 | 1.50 | −2.23 |
| L1 | 5 | 8.30 | 14.50 | −3.47 | 1.75 | −2.23 | |
|
| |||||||
| KC3 | L0 | 2 | 8.10 | 14.50 | −3.72 | 1.50 | −9.60 |
| L1 | 2 | 8.10 | 14.50 | −3.72 | 1.50 | −16.50 | |
Table 4 reports both the LC and HC logMAR VA data recorded with the GP lens and each successive custom lens through a physiological pupil. In all cases, high contrast logMAR VA with the final custom lens is equal or superior to levels obtained with the habitual GP. Low contrast logMAR VA levels for the final custom lens as compared to the GP were equivalent for subjects KC2 and KC3, but were reduced in subject KC1. Table 4 also lists an interval encompassing 67% of a normal age-matched sample for the exit criterion reached by each subject.18 The 67% interval was chosen because it makes it more difficult for the subjects to be considered within normal limits than the 95% interval. While all subjects did reach the high contrast logMAR VA exit criterion, all are still outside of this age-matched normal interval.
Table 4.
HC and LC visual acuity data recorded with the GP lens and each successive custom lens are reported. In all cases, high contrast logMAR VA with the final custom lens is equal or superior to levels obtained with the habitual GP, but still does not achieve normal levels. Average and standard deviation are reported.
| Subject | Lens Iteration | HC VA | LC VA | Weber Contrast of LC VA Chart | Criteria Reached with Lens | P | HC VA Range for 67% of Age-Matched Normals | In Normal Interval? |
|---|---|---|---|---|---|---|---|---|
| KC1 | GP | 0.01 ± 0.05 | 0.49 ± 0.04 | 52% | HC VA, L1 | 0.69 | −0.14 – −0.06 | no |
| L0 | 0.01 ± 0.02 | 0.60 ± 0.03 | ||||||
| L1 | 0.00 ± 0.02 | 0.58 ± 0.07 | ||||||
|
| ||||||||
| KC2 | GP | 0.20 ± 0.02 | 0.58 ± 0.04 | 37% | HC VA, L1 | 0.02 | −0.16 – −0.04 | no |
| L0 | 0.31 ± 0.05 | 0.72 ± 0.06 | ||||||
| L1 | 0.14 ± 0.02 | 0.59 ± 0.04 | ||||||
|
| ||||||||
| KC3 | GP | 0.04 ± 0.09 | 0.58 ± 0.04 | 52% | HC VA, L1 | 0.2 | −0.22 – −0.10 | no |
| L0 | 0.27 ± 0.05 | 0.91 ± 0.10 | ||||||
| L1 | −0.05 ± 0.05 | 0.61 ± 0.04 | ||||||
Table 5 reports the low order RMS, high order RMS and pupil size for each eye/contact lens correction studied (These are on-eye measurements of lens performance). Each initial custom lens studied in each series, L0, reduces the low order aberration of the uncorrected eye. Only one subject, KC2, reached the established exit criterion for aberration of high order RMS equal or less than that experienced in GP wear. Data showed GP and final custom lens high order RMS correction respectively of 0.394 μm and 0.381μm for KC2. Subjects KC2 and KC3 experienced a reduction in high order aberration as compared to the uncorrected eye from 0.609μm to 0.381μm for KC2 and from 1.565μm to 0.758μm for KC3.
Table 5.
Residual low order RMS and high order RMS levels measured with each lens on the eye are reported. Average and standard deviation are reported.
| Subject | Lens Iteration | Average Low Order RMS (um) | Average High Order RMS (um) | Pupil Size (dia, mm) |
|---|---|---|---|---|
| KC1 | uncorrected | 2.616 ± 0.040 | 0.214 ± 0.015 | 4.25 |
| GP | 0.160 ± 0.036 | 0.280 ± 0.010 | ||
| L0 (629) | 0.520 ± 0.094 | 0.268 ± 0.082 | ||
| L1 (646) | 0.333 ± 0.027 | 0.314 ± 0.040 | ||
|
| ||||
| KC2 | uncorrected | 2.714 ± 0.056 | 0.609 ± 0.018 | 4.25 |
| GP | 0.484 ± 0.087 | 0.394 ± 0.024 | ||
| L0 (630) | 1.708 ± 0.251 | 0.556 ± 0.082 | ||
| L1 (649) | 0.123 ± 0.146 | 0.381 ± 0.074 | ||
|
| ||||
| KC3 | uncorrected | 10.709 ± 0.362 | 1.565 ± 0.027 | 4.50 |
| GP | 0.536 ± 0.267 | 0.496 ± 0.154 | ||
| L0 (627) | 3.129 ± 0.146 | 1.062 ± 0.040 | ||
| L1 (644) | 1.790 ± 0.097 | 0.758 ± 0.033 | ||
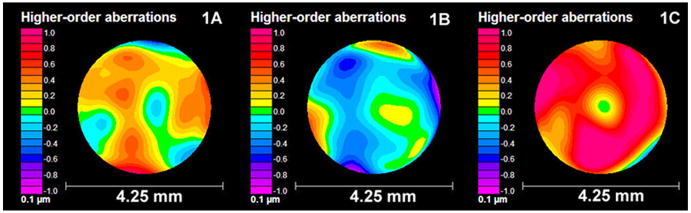
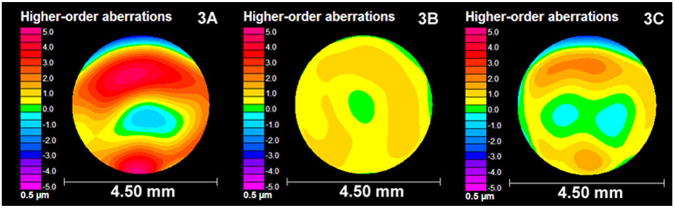
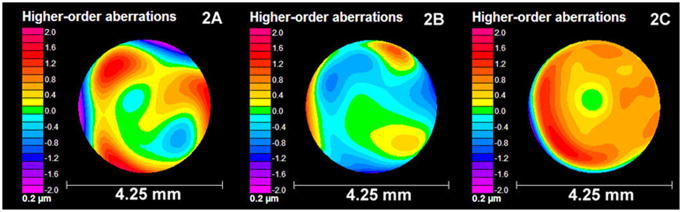
Higher order aberration data for the uncorrected eye as captured on a COAS HD wavefront sensor, higher order aberration structure in the final custom contact lens as captured on the ClearWave optical profiler and higher order aberration structure measured with the final lens on the eye captured on the COAS HD wavefront sensor are presented pictorially in Figures 1–3. Figure 1 reports higher order aberration data for subject KC1. Figure 1a shows the uncorrected higher order aberration map for KC1, figure 1b shows the higher order aberration structure of the final lens in the series (L1) and figure 1c shows the higher order aberration structure of the eye + final lens in the series. The same series of data plots is presented for KC2 in figure 2 and KC3 for figure 3. All maps included in a given figure are plotted with a common scale, however the step size increases from figure 1 to figure 3, noting an increase in disease severity in the eyes studied. Examination of figure 1 shows a compensating higher order optical aberration structure for the eye of subject KC1 (figure 1a) in the optical profile of lens L1 for KC1 (figure 1b). This eye has relatively low higher order RMS for a keratoconus subject, and the aberration structure in the eye-lens system (figure 1c) is not significantly reduced as compared to the uncorrected eye. A compensating higher order optical aberration structure for the uncorrected eye of subject KC2 (figure 2a) can be observed in the optical profile of L1 for KC2 (figure 2b). This eye has elevated higher order RMS, and the aberration structure in the eye-lens system (figure 2c) is well corrected as compared to the uncorrected eye (figure 2a). Residual spherical aberration is the dominant aberration remaining in the eye-lens system. A compensating higher order optical aberration structure for the eye of subject KC3 (figure 3a) was not implemented for KC3 (figure 3b) as the subject reached exit criterion with a custom sphero-cylindrical lens. However, when this lens is worn on the eye (figure 3c) and the aberration data compared to the uncorrected eye of KC3 (figure 3a), it is noted that the higher order aberration is reduced by 51%. This manifests as similarities between the aberration structures of figure 3a and 3c, with figure 3c having a smaller amplitude.
Figure 1.
Figure 1a shows the uncorrected higher order aberration map for KC1, figure 1b shows the higher order aberration structure of lens L1 and figure 1c shows the higher order aberration structure of the eye + final lens in the series. The aberration structure in figure 1a can be seen as represented in figure 1b, but with an opposite (compensating) color scheme.
Figure 3.
Figure 3a shows the uncorrected higher order aberration map for KC3, figure 3b shows the higher order aberration structure of lens L1 and figure 3c shows the higher order aberration structure of the eye + final lens in the series. The lens in figure 3b contains no intended higher order aberration compensation for 3a, and is intended to be only a custotm sphero-cylindrical correction. Despite this, higher order aberration in figure 3c is reduced by 51% as compared to the uncorrected eye in figure 3a when wearing the custom soft contact lens.
Figure 2.
Figure 2a shows the uncorrected higher order aberration map for KC2, figure 2b shows the higher order aberration structure of lens L1 and figure 2c shows the higher order aberration structure of the eye + final lens in the series. The aberration structure in figure 2a can be seen as represented in figure 2b, but with an opposite (compensating) color scheme.
DISCUSSION
The current study extended the clinical observations of custom wavefront guided soft contact lenses by focusing on three GP-wearing keratoconic subjects and comparing performance of the custom lenses to the subjects’ habitual GP corrections. Results show that custom wavefront-guided soft contact lenses provided this sample of keratoconus subjects with high contrast logMAR visual acuity equivalent to habitual gas permeable (GP) corrections under laboratory conditions.
The act of placing a soft lens with low order correction on the eye has been shown to reduce higher order aberration experienced by the keratoconic eye. Masking of higher order aberration via this mechanism was seen in earlier work conducted on keratoconus subjects with a series of soft contact lenses, but the effect is poor in comparison to rigid lenses.19 Subject KC3 reached the exit criterion with lens L1, which in this subject was a second custom sphero-cylindrical correction with no higher order aberration correction, suggesting that in this case, the soft contact lens is masking higher order aberration. Table 5 demonstrates that over a 4.5mm pupil, lens L1 reduces total HORMS from 1.565μm for the uncorrected eye to 0.758μm, while the higher order RMS experienced by this eye with the GP is 0.496μm. Both values are well above the normal level for an age and pupil size matched normal of 0.127.20 Subject KC3 also experienced elevated lower order aberration (low order RMS: 1.790μm, or 2.50D spherical equivalent) of which the majority comes from the defocus term (−1.786μm). Due to the fact that this subject is young and accommodation was not paralyzed for this experiment, it is possible that this defocus error is negated by accommodation, reducing the visual impact of the residual defocus under these conditions. Had the exit criteria not been reached with this lens, these elevated low and high order aberrations would have been targeted in future lenses by the iterative nature of the process.
For every subject studied, the uncorrected low order RMS is larger than the uncorrected high order RMS. Custom corrections are touted based on their ability to selectively correct high order aberrations, but they also have the ability to correct the residual low order aberrations in a targeted, customized fashion. For instance, the low order aberration structure of subject KC2 is reduced for the final custom lens studied, while the higher order aberration remains relatively equivalent to GP performance. The ability to select and target low order correction below 0.25D has been identified in the literature as an important advantage of custom lenses.21
Iteration in this study ceased because subjects reached the established exit criteria, which was based on high contrast VA. This raises the question of the appropriateness of using high contrast VA as a visual task when refining custom wavefront guided soft contact lens designs. Photopic high contrast VA is known to be insensitive to a wide range of RMS wavefront error22,23 and prior reports demonstrate that retinal image quality metrics based on wavefront error predict mesopic low contrast visual performance.22,24 Achieving an exit criteria based on a metric of retinal image quality known to predict a difficult visual performance task may lead to better visual performance. Perhaps a more appropriate exit criterion would favor using age-matched normal values for performance in the place of the subject’s habitual performance. If such an exit criterion were used, additional lens iterations would have been necessary for all three subjects.
These results highlight a few of the challenges associated with implementation of custom wavefront-guided soft contact lenses for keratoconus subjects (pupil size, movement, sensitive visual performance task, residual aberration). Additional problems will also need to be addressed if this type of correction is to be made clinically relevant. As the pupil gets larger, aberration increases. In keratoconus, this can lead to difficulty obtaining good measurements using clinically available wavefront sensors. Scarring may also increase the difficulty of achieving maximum visual potential, and this difficulty is experienced with both the habitual GP correction and a custom correction. Variability of corneal shape over time, both from disease progression and cessation of rigid lens wear would need to be considered in a longitudinal study. These problems are non-trivial, as the severity of their impact on the correction will vary by individual. Further, it has been demonstrated that interactions between aberrations can result in variation in visual performance.16 These complex interactions make it difficult to predict resultant visual performance strictly from RMS levels. So, while reduction of higher order aberration remains a preliminary goal of this process, future directions include integrating metrics of retinal image quality into the design process in order to gain insight into how a specific combination of aberrations may impact resultant visual performance. It has also been reported that there is a stability benefit associated with carving the back surface of the lens to approximately mirror the anterior surface of the cornea.13,25
Although wavefront guided soft lens corrections have not been demonstrated to reliably address the concerns of a large, varied population of keratoconus subjects and are not yet in a clinically optimized form, work in this area from multiple research teams now demonstrates their ability to address the needs of a small number of patients in the laboratory environment. Future directions include examination of wavefront guided soft lenses using more strict exit criteria, conducting studies to determine if comfort and wear time can be extended and if the design can be further refined for ease of fitting to a large number of keratoconus subjects.
Acknowledgments
NEI P30 EY07551-UHCO, NEI T32 EY07024-JDM, NEI ROI EY08520-RAA.
AOF soft contact lens research grant-JDM.
National Keratoconus Foundation research grant-JDM.
The authors thank Wavefront Sciences (Albuquerque, NM), DAC International (Carpinteria, NM) and Metro Optics (Austin, TX) for their assistance in this project.
Footnotes
As with all reports of aberration data, pupil size is critically important. While it is commonplace for studies in the literature to report wave aberration and visual performance data across subjects using a common pupil size (for example 5mm), the authors here have chosen to use a patient-dependent, physiological pupil size for evaluation of custom contact lenses. This avenue was chosen because of an interest in examining resultant aberration and visual performance changes for an individual relative to their habitual, real world correction. This implies the use of the habitual pupil size. Use of an artificial pupil size would not allow comparison to habitual performance. Rather, a common pupil size that would likely not correspond to any individuals’ habitual pupil size would have to be chosen. It was deemed more interesting at this early stage to investigate changes on an intra-subject rather than inter-subject basis.
This paper was presented at The American Academy of Optometry, October 27, 2007.
References
- 1.Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, Shin JA, Sterling JL, Wagner H, Gordon MO. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39:2537–46. [PubMed] [Google Scholar]
- 2.Kosaki R, Maeda N, Bessho K, Hori Y, Nishida K, Suzaki A, Hirohara Y, Mihashi T, Fujikado T, Tano Y. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007;48:3062–8. doi: 10.1167/iovs.06-1285. [DOI] [PubMed] [Google Scholar]
- 3.Marsack JD, Parker KE, Pesudovs K, Donnelly WJ, 3rd, Applegate RA. Uncorrected wavefront error and visual performance during RGP wear in keratoconus. Optom Vis Sci. 2007;84:463–70. doi: 10.1097/OPX.0b013e31802e64f0. [DOI] [PubMed] [Google Scholar]
- 4.Negishi K, Kumanomido T, Utsumi Y, Tsubota K. Effect of higher-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens. Am J Ophthalmol. 2007;144:924–9. doi: 10.1016/j.ajo.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Guirao A, Williams DR, Cox IG. Effect of rotation and translation on the expected benefit of an ideal method to correct the eye’s higher-order aberrations. J Opt Soc Am (A) 2001;18:1003–15. doi: 10.1364/josaa.18.001003. [DOI] [PubMed] [Google Scholar]
- 6.Guirao A, Porter J, Williams DR, Cox IG. Calculated impact of higher-order monochromatic aberrations on retinal image quality in a population of human eyes. J Opt Soc Am (A) 2002;19:1–9. doi: 10.1364/josaa.19.000001. [DOI] [PubMed] [Google Scholar]
- 7.de Brabander J, Chateau N, Marin G, Lopez-Gil N, Van Der Worp E, Benito A. Simulated optical performance of custom wavefront soft contact lenses for keratoconus. Optom Vis Sci. 2003;80:637–43. doi: 10.1097/00006324-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Williams D, Yoon GY, Porter J, Guirao A, Hofer H, Cox I. Visual benefit of correcting higher order aberrations of the eye. J Refract Surg. 2000;16:S554–9. doi: 10.3928/1081-597X-20000901-12. [DOI] [PubMed] [Google Scholar]
- 9.Marsack JD, Pesudovs K, Sarver EJ, Applegate RA. Impact of Zernike-fit error on simulated high- and low-contrast acuity in keratoconus: implications for using Zernike-based corrections. J Opt Soc Am A Opt Image Sci Vis. 2006;23:769–76. doi: 10.1364/josaa.23.000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez-Gil N, Castejon-Mochon JF, Benito A, Marin JM, Lo-a-Foe G, Marin G, Fermigier B, Renard D, Joyeux D, Chateau N, Artal P. Aberration generation by contact lenses with aspheric and asymmetric surfaces. J Refract Surg. 2002;18:S603–9. doi: 10.3928/1081-597X-20020901-21. [DOI] [PubMed] [Google Scholar]
- 11.Sabesan R, Jeong TM, Carvalho L, Cox IG, Williams DR, Yoon G. Vision improvement by correcting higher-order aberrations with customized soft contact lenses in keratoconic eyes. Opt Lett. 2007;32:1000–2. doi: 10.1364/ol.32.001000. [DOI] [PubMed] [Google Scholar]
- 12.Marsack JD, Parker KE, Niu Y, Pesudovs K, Applegate RA. On-eye performance of custom wavefront-guided soft contact lenses in a habitual soft lens-wearing keratoconic patient. J Refract Surg. 2007;23:960–4. doi: 10.3928/1081-597X-20071101-18. [DOI] [PubMed] [Google Scholar]
- 13.Chen M, Sabesan R, Ahmad K, Yoon G. Correcting anterior corneal aberration and variability of lens movements in keratoconic eyes with back-surface customized soft contact lenses. Opt Lett. 2007;32:3203–5. doi: 10.1364/ol.32.003203. [DOI] [PubMed] [Google Scholar]
- 14.Guirao A, Cox IG, Williams DR. Method for optimizing the correction of the eye’s higher-order aberrations in the presence of decentrations. J Opt Soc Am (A) 2002;19:126–8. doi: 10.1364/josaa.19.000126. [DOI] [PubMed] [Google Scholar]
- 15.Applegate RA, Sarver EJ, Khemsara V. Are all aberrations equal? J Refract Surg. 2002;18:S556–62. doi: 10.3928/1081-597X-20020901-12. [DOI] [PubMed] [Google Scholar]
- 16.Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction between aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003;29:1487–95. doi: 10.1016/s0886-3350(03)00334-1. [DOI] [PubMed] [Google Scholar]
- 17.Applegate RA, Ballentine C, Gross H, Sarver EJ, Sarver CA. Visual acuity as a function of Zernike mode and level of root mean square error. Optom Vis Sci. 2003;80:97–105. doi: 10.1097/00006324-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Elliott DB, Yang KC, Whitaker D. Visual acuity changes throughout adulthood in normal, healthy eyes: seeing beyond 6/6. Optom Vis Sci. 1995;72:186–91. doi: 10.1097/00006324-199503000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths M, Zahner K, Collins M, Carney L. Masking of irregular corneal topography with contact lenses. CLAO J. 1998;24:76–81. [PubMed] [Google Scholar]
- 20.Applegate RA, Donnelly WJ, 3rd, Marsack JD, Koenig DE, Pesudovs K. Three-dimensional relationship between high-order root-mean-square wavefront error, pupil diameter, and aging. J Opt Soc Am A Opt Image Sci Vis. 2007;24:578–87. doi: 10.1364/josaa.24.000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thibos LN, Cheng X, Bradley A. Design principles and limitations of wave-front guided contact lenses. Eye Contact Lens. 2003;29:S167–70. doi: 10.1097/00140068-200301001-00046. [DOI] [PubMed] [Google Scholar]
- 22.Applegate RA, Marsack JD, Thibos LN. Metrics of retinal image quality predict visual performance in eyes with 20/17 or better visual acuity. Optom Vis Sci. 2006;83:635–40. doi: 10.1097/01.opx.0000232842.60932.af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pepose JS, Applegate RA. Making sense out of wavefront sensing. Am J Ophthalmol. 2005;139:335–43. doi: 10.1016/j.ajo.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 24.Pesudovs K, Marsack JD, Donnelly WJ, 3rd, Thibos LN, Applegate RA. Measuring visual acuity--mesopic or photopic conditions, and high or low contrast letters? J Refract Surg. 2004;20:S508–14. [PubMed] [Google Scholar]
- 25.Marsack J, Milner T, Rylander G, Leach N, Roorda A. Applying wavefront sensors and corneal topography to keratoconus. Biomed Sci Instrum. 2002;38:471–6. [PubMed] [Google Scholar]