Abstract
Background and Objective
Cardiopulmonary Resuscitation (CPR) with adequate chest compression depth appears to improve first shock success in cardiac arrest. We evaluate the effect of simplification of chest compression instructions on compression depth in dispatcher-assisted CPR protocol.
Methods
Data from two randomized, double-blinded, controlled trials with identical methodology were combined to obtain 332 records for this analysis. Subjects were randomized to either modified Medical Priority Dispatch System (MPDS) v11.2 protocol or a new simplified protocol. The main difference between the protocols was the instruction to “push as hard as you can” in the simplified protocol, compared to “push down firmly 2 inches (5cm)” in MPDS. Data were recorded via a Laerdal® ResusciAnne® SkillReporter™ manikin. Primary outcome measures included: chest compression depth, proportion of compressions without error, with adequate depth and with total release.
Results
Instructions to “push as hard as you can”, compared to “push down firmly 2 inches (5cm)”, resulted in improved chest compression depth (36.4 vs 29.7 mm, p<0.0001), and improved median proportion of chest compressions done to the correct depth (32% vs <1%, p<0.0001). No significant difference in median proportion of compressions with total release (100% for both) and average compression rate (99.7 vs 97.5 per min, p<0.56) was found.
Conclusions
Modifying dispatcher-assisted CPR instructions by changing “push down firmly 2 inches (5cm)” to “push as hard as you can” achieved improvement in chest compression depth at no cost to total release or average chest compression rate.
Keywords: Bystander CPR, Cardiac arrest, Chest compression
1. INTRODUCTION
Background
Heart diseases are a significant cause of death in the United States, with sudden cardiac death (SCD) alone accounting for more than 5% of overall deaths in the community. 1, 2, 3 Out-of-hospital cardiac arrests (OOH-CA) comprise >60% of SCDs.4 High incidence coupled with a low survival rate of 2 – 4% make OOH-CA a significant public health issue.5 Even though rapid defibrillation is the treatment of choice for cardiac arrest, it has been observed that provision of good quality early cardiopulmonary resuscitation (CPR) by bystanders is a likely determinant of blood flow preceding defibrillation.6, 7 Good quality CPR produces a shockable rhythm, increasing first shock success and improving survival in OOH-CA.8–14 Wik et al observed that good quality CPR improved outcomes by as much as 17%. Additionally, they found no differences in outcome between patients receiving no CPR and those receiving poor quality CPR.14
In particular, recent data suggest a relationship between adequate chest compression depth during CPR and first shock success.7 Gallagher et al observed no difference between the survival rates for patients with poorly performed chest compressions and those who received no chest compressions. However, patients who received better quality CPR had increased survival (4.6% versus 1.4%, OR=3.4, p<0.02).9 In a recent porcine study, Ristagno et al found that the quality of chest compressions was the overriding determinant of successful resuscitation rather than whether defibrillation or chest compressions were done initially after sudden cardiac arrest.15 They observed that when effective chest compressions were given, defibrillation could be delayed without compromising outcomes.
It is believed that telephone instructions provided by emergency medical dispatchers to bystanders increase the chances of the OOH-CA victims getting early CPR, and may improve survival.16–18 However, the quality of out-of hospital CPR has often been found to be poor, with chest compression depth usually shallower than recommended by American Heart Association (AHA) and Advanced Cardiac Life Support (ACLS) guidelines.19, 20
The AHA considers early bystander CPR to be one of the four links in the “chain of survival” following OOH-CA. A 2008 AHA scientific statement encourages the development of dispatcher-assisted “telephone CPR” because it provides CPR instructions in “real-time”, and may be helpful even in those cases in which the bystander did not receive prior CPR training. The statement also recommends improving the quality of CPR by implementing continuous quality improvement in Emergency Medical Services (EMS) and community lay rescuer training programs.21 Previous work has demonstrated that specific simplified instructions, to perform chest compression-only cardiopulmonary resuscitation (CC-CPR), delivered by dispatchers to bystanders can positively influence the quality of CPR.22 The 2008 AHA statement also points out the importance of CC-CPR under some conditions, as this has the potential to encourage layperson participation.21
Given the impact of OOH-CA on the population, more effort towards early provision of effective emergency medical measures is warranted.4 AHA recommends further research to explore methods for increasing bystander CPR performance.21 The objective of this report is to describe the comparative effect of instructing the bystanders to “push as hard as you can” versus “push down firmly 2 inches (5cm)”, on the quality of chest compression depth in simulated CC-CPR performed by laypersons in simulated out-of-hospital setting.
2. METHODS
Study Design and Population
This report represents combined data from two prospective randomized controlled, double-blinded, field trials with identical methodology but with different dispatcher-assisted CPR instruction sets as described in earlier reports.22, 23 After careful screening, following the inclusion and exclusion criteria described elsewhere, the remaining population of local trained and untrained adult laypersons is expected to represent the most likely responders who would perform dispatcher-assisted CC-CPR on cardiac arrest victims in the community.22, 23 All protocols were approved by the University of Alabama at Birmingham (UAB) Institutional Review Board (IRB). After full disclosure of possible risks and benefits associated with the study, subjects gave written informed consent in accordance with local IRB regulations.
Materials and Measurements
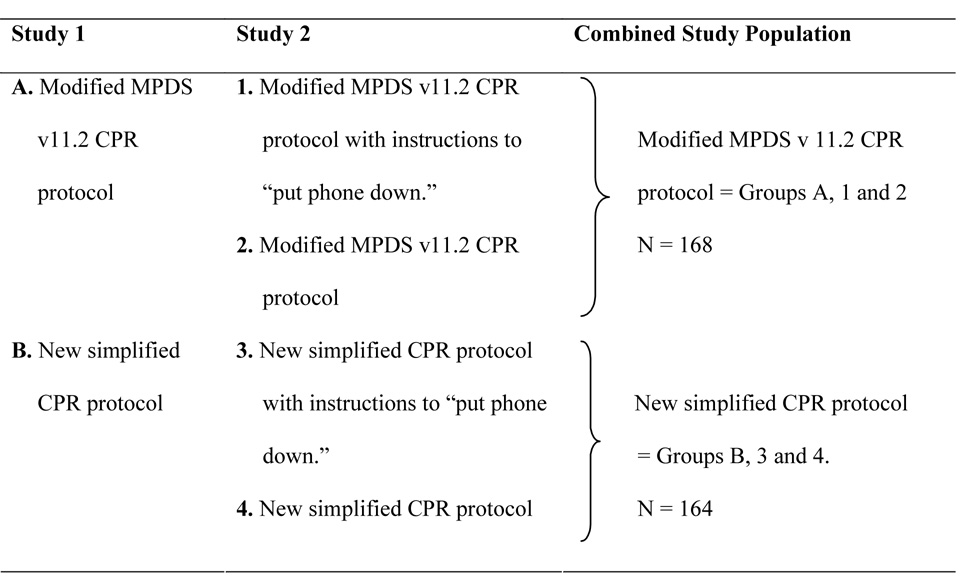
We used a CPR simulation manikin and a standardized scenario to assess the quality of single-rescuer adult CPR.22, 23 After enrollment, the subjects were randomized to one of six subgroups across both studies, two in the first and four in the second, using a constrained block randomization scheme (Figure 1). The recruiter was blinded to the randomization scheme, and the dispatcher was blinded to the study subjects. The six groups comprised of two control and four intervention groups divided as follows: in the first study, the control group was exposed to a modified CC-CPR version of the Medical Priority Dispatch System (MPDS) version 11.2 instructions [recommended by National Academy of Emergency Dispatchers (NAED)], and the intervention group received instructions from a new simplified CC-CPR protocol.22, 23 In the second study, one of the groups was exposed to the modified MPDS v11.2 CC-CPR instructions recommended by NAED (control), and another to the same modified MPDS protocol with additional instructions to “put the phone down” (intervention). Two additional intervention groups in the second study were exposed to simplified sets of CPR instructions with or without instructions to “put the phone down”. These instructions were added after the point where the dispatcher instructs to “push as hard as you can” and reassures the rescuer that she will stay on the line. The MPDS v11.2 protocol used as the control is designed as a chest compressions first protocol. We sequentially linked instructions from MPDS v11.2 panels as described in earlier reports.22, 23 The simplified CC-CPR guidelines, used as the intervention, were developed by the research team and modified based on observations gained from an earlier study.22
Figure 1.
Groups of CPR instruction protocols used in the two studies.
Data Collection and Processing
Data were collected using the Laerdal® PC SkillReporting System - a software used with the adult size Laerdal® Resusci®Anne SkillReporter™ manikin to collect the subjects’ CPR performance data into a computerized database.23 Survey forms developed for these studies collected demographics and data about prior training.
Outcome Measures
Prospectively defined primary outcome measures included: chest compression rate and depth; proportion of compressions without error, with correct hand position, with adequate depth and with total release. Additional variables included time to start of CPR and total hands-off-chest time.
Data Management
The methods for both trials were identical, so we feel that combining the data to yield the data set for this analysis is reasonable (Figure 1). Results and methods from both trials are published elsewhere.22, 23 Both studies were randomized controlled, double-blinded, field trials. In both studies, participants were recruited at public sites throughout central Alabama, and had similar exclusion criteria. Additionally, the researchers followed identical methods for delivery of instructions and data collection. The protocols differed only in the specific CPR instruction sets used in the two studies.22, 23
The protocols used in the second study were designed to test whether instruction to put the telephone down could improve CPR, and to attempt to improve hand positioning on the chest wall. We found no significant difference between the quality of CPR performed whether the subjects were instructed to put the phone down or not (results reported elsewhere).23 Another difference in the two versions of our simplified protocol (used in the two studies) was a slight difference in instructions relating to hand position, with the addition of “with the other hand on top”, in the second study protocol. This instruction was added at the point where the dispatcher explained hand placement to the rescuer. To determine whether these differences might confound chest compression depth, we compared whether there were any differences in proportion correct hand position between the three groups exposed to simplified protocols across the two studies. This comparison used the Wilcoxon Rank Sum Test. We found no difference in proportion of correct hand position across any of the simplified protocols (p=0.26). Combining the data yielded 2 groups: one was exposed to MPDS v11.2 protocol and the other to the new simplified CC-CPR protocol with the instruction to push “as hard as you can”.
The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the manuscript as written.
Data analysis
Our first study collected performance data of 117 subjects, and the second collected 215 records.22, 23 Thus, a total of 332 subjects were randomized in two studies. After combining the data from the two studies, 164 subjects were in the group which received the new simplified CC-CPR instructions and 168 received the modified MPDS v11.2 instructions. Statistical analysis was performed on pre-selected variables felt most influential in affecting CPR performance. Age was compared using the t-test, and gender and prior CPR training were compared using chi-squared tests. Chest compression rate and depth were normally distributed, therefore, these were analyzed with Analysis of Variance (ANOVA). Proportion of compressions without error, correct depth, and total release of chest wall were non-normally distributed and were analyzed with the Wilcoxon Rank Sum Test; time variables were analyzed with ANOVA. Tests were two-sided, and statistically significant findings were concluded from p<0.05. Data were analyzed using JMP IN® version 5.1.2 statistical software.
3. RESULTS
Table 1 shows characteristics of each sample relevant to the depth of chest compressions: age, gender, and prior CPR training. There were no statistical differences between the study samples across these variables. Table 2 displays the outcomes of interest for this analysis. Subjects instructed to “push as hard as you can” achieved significantly greater average chest compression depth, a greater proportion of compressions done to the correct depth, and a greater proportion of compressions without error. Chest compression rate was equivalent in both groups. Additionally, despite superior chest compression depth, subjects told to “push as hard as you can” allowed complete chest wall recoil as effectively as those told to “push down firmly 2 inches (5cm)”. This was shown by no significant difference (p = 0.14) between the two groups in the proportion of total chest wall release. Other variables collected individually for the separate studies are reported elsewhere.22 Furthermore, we found no difference in proportion of correct hand position across any of the simplified protocols (p = 0.26). The modified MPDS protocols, however, resulted in consistently better hand position (data reported elsewhere).22
Table 1.
Comparison between selected variables from the combined data
| “Push down firmly 2 inches (5cm)” N = 168 |
“Push as hard as you can” N = 164 |
|
|---|---|---|
| Mean Age in years (SD) | ||
| 30.0 (12.9) | 31.1 (13.6) | |
| Male n (%) | 55 | 58 |
| CPR training n (%) | ||
| Ever trained | 59 | 59 |
| Ever certified | 41 | 41 |
Table 2.
Effect of old and new protocol on the quality of chest compressions-only CPR
| Outcome variable | “Push down firmly 2 inches (5cm)” | “Push as hard as you can” | P-value |
|---|---|---|---|
| Average compression depth (mm)1 | 29.7 (10.2) | 36.4 (11.6) | <0.0001 |
| Compression rate (min−1)1 | 97.5 (34.3) | 99.7 (35.3) | 0.56 |
| Proportion of compressions done without error2 | 0 (0–0.17) | 0.05 (0–0.38) | 0.003 |
| Proportion of compressions done to correct depth2 | 0.01 (0–0.39) | 0.32 (0–0.78) | <0.0001 |
| Proportion of compressions done with full release2 | 1.0 (0.99–1) | 1.0 (0.99–1) | 0.14 |
mean (SD)
median (interquartile range)
4. DISCUSSION
Early initiation of good quality CPR by laypersons is hindered by the complexity of CPR instructions.22 Therefore, there has been a shift to a new approach to dispatcher-assisted CPR instructions which follows the mantra “push hard, push fast”.24 The new guidelines also favor complete recoil, and minimal interruptions in chest compressions. Simplified dispatcher-assisted CPR instructions have been shown to improve quality of bystander CPR.22, 25
Our analysis suggests that instructions to “push as hard as you can” are superior to instructions to “push down firmly 2 inches (5cm)” in achieving improvement in chest compression depth (Table 2). There are several possible explanations for this observation, for instance it is difficult to judge, even for trained professionals, how much force leads to a 2 inch (5 cm) compression depth. Even with correct knowledge and feedback, rescuers often do not achieve adequate depth.19, 26, 27 Therefore, it may be difficult for laypersons to ascertain correct depth while performing CPR. Instructions to “push as hard as you can” eliminate the need for making this judgment and lets the rescuer focus on delivering deep, forceful chest compressions. Furthermore, research on attitudes regarding CPR has shown that rescuers fear the possibility of chest wall injuries, and are often hesitant to push very hard.28 It is possible that instructions to “push down as hard as you can” underscored the importance of pushing hard to the participants, who were therefore less wary of injuring the manikin, and were able to achieve greater depth than those who were instructed to push down to a depth of “2 inches”. Whether this finding of manikin simulation will be observed with actual victims, where chest wall injury is a real possibility, remains to be seen.
The importance of these results is underscored by finding that better compression depth was achieved at no cost to total release or chest compression rate (Table 2). Despite increase in depth, subjects told to “push as hard as you can” allowed complete chest wall recoil as effectively as those told to “push down firmly 2 inches (5cm)”. In addition, subjects were also able to maintain adequate chest compression rate in both the groups.
Our findings are also significant because the experimental simplified instructions take less time and are easily understood. The results of our first study showed that short and simple protocols save time. We found that there was significant improvement in the time to start of compressions by those who were provided with the new simplified instructions (Standard protocol = 78.6s; Simplified protocol = 60.9s and p < 0.0001).22
Even though our results show significantly better performance of at least two parameters, as compared to the standard MPDS v11.2 protocol, the overall quality of CPR was still poor. In our second trial, the group given the simplified CPR instructions delivered only 5% chest compressions without error (Table 2). Additionally, the average compression depth of 36.38 mm observed by following the new simplified protocol was lower than the acceptable range based on Basic Life Support guidelines: 40 mm – 50 mm.29 Therefore, further effort is needed to simplify the bystander CPR instruction protocols to improve performance.
Though our study shows the effectiveness of the simplified protocol in achieving deeper chest compressions, a number of diverse factors may affect the success of dispatcher-assisted CC-CPR. These factors include: interval between onset of cardiac arrest and the start of CPR, whether or not the bystander had prior training, the interval between patient’s collapse and the arrival of trained medical personnel, and the patient’s age and place of cardiac arrest.30 Some other influencing factors include: whether the arrest was witnessed or not, the dispatcher’s ability to identify cardiac arrest, whether dispatcher offered CPR instructions to the caller, and the dispatcher’s ability to follow the protocol for providing the instructions. Additionally, the caller’s willingness to perform CPR, physical ability to perform correctly, and the ability to understand and closely follow the instructions may also have significant effect on the quality of performance.9, 18, 31, 32 The effect of rescuer fatigue on compression depth is also a possible factor. Odegaard et al found that laypersons delivering continuous chest compression-only CPR delivered a significantly increased rate of chest compressions per minute, but at the cost of decreased compression depth quality, compared to those performing CPR following the 15:2 and 30:2 (compressions:ventilations) protocols.33 The findings of this study suggest that fatigue during the later part of CPR may reduce the average chest compression depth over the entire CPR episode. Unfortunately, our data set does not let us explore this factor. We have data over the entire CPR episode for each subject. It is not possible for us to divide each record into shorter increments and compare the performance during the first 90 seconds of CPR to that of the subsequent 90 seconds, to explore the effect on depth over time. Future studies may consider assessing the effect of fatigue by comparing the chest compression depth among different intervals of a CPR episode.
5. LIMITATIONS
Manikin simulation is a major limitation of our study. A simulation cannot exactly replicate the complexity, urgency and constraints of a real life scenario. We used standardized protocols and tools to ensure consistency in our methodology. Males over age 60 are most likely to require dispatcher-assisted CPR delivered by an adult of a similar age.34 Although, the age range of our sample was 19 to 83 years, most of our subjects were young and healthy. Therefore, our results may not be generalizable to the populations most likely to perform dispatcher-assisted CC-CPR, such as spouses of the elderly.
The MPDS v11.2 protocol was not designed as a chest compressions only protocol. For our study purposes, we sequentially linked instructions in the standard protocol to eliminate the instructions for ventilation. The effect of this slight modification on the results is unclear. Finally, we attempted to combine two datasets generated from studies of virtually identical methodology, performed by the same group of researchers. The samples did not differ across pre-selected important variables of age, gender, and prior CPR training. There were minor differences in the instruction sets, relating chiefly to hand position that could have biased the compression depth we observed. However, the minor nature of these differences and the fact that the proportion of correct hand positioning was not statistically different among any of our simplified protocol followers suggest that such bias is unlikely.
6. CONCLUSION
Modifying dispatcher-assisted CC-CPR instructions, by changing “push down firmly 2 inches (5cm)” to “push as hard as you can”, achieved improvement in average compression depth and proportion of compressions to correct depth at no cost to proportion of compressions with total release or average chest compression rate. We recommend adoption of this phraseology into dispatcher-assisted CC-CPR instructions. However, even these instructions do not yield a high proportion of good quality chest compressions. Therefore, further effort is needed to simplify the bystander CC-CPR instruction protocols to improve performance. We also recommend improved instructions for hand position in the simplified protocol.
Supplementary Material
ACKNOWLEDGEMENTS
The authors are grateful for the support of Thomas E. Terndrup, MD.
Source of support: Partial support for this project was provided by the National Heart Lung and Blood Institute, through the Resuscitation Outcomes Consortium (5-U01-HL077881) and the Department of Emergency Medicine at the University of Alabama at Birmingham. Additional funds provided by the National Library of Medicine, National Institutes of Health, under Contract No. N01-LM-3-3513.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest.
REFERENCES
- 1.National Center for Health Statistics. [[Cited 2007 June 3]];Death and Mortality statistics. 2006 [web page on the Internet]. Available from http://www.cdc.gov/nchs/fastats/deaths.htm.
- 2.American Heart Association. Heart Disease and Stroke Statistics — 2005 Update. Dallas, Texas: American Heart Association; 2005. [Google Scholar]
- 3.Chugh SS, Jui J, Gunson K, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 4.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. State specific mortality from sudden cardiac death -- United States, 1999. MMWR. 2002;51:123–126. [PubMed] [Google Scholar]
- 6.Jacobs I, Nadkarni V, Bahr J, et al. International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa. ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation. Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 7.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and preshock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Cummins RO, Eisenberg MS. Prehospital cardiopulmonary resuscitation. Is it effective? JAMA. 1985;253:2408–2412. [PubMed] [Google Scholar]
- 9.Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274:1922–1925. [PubMed] [Google Scholar]
- 10.Swor RA, Jackson RE, Cynar M, et al. Bystander CPR, ventricular fibrillation, and survival in witnessed, unmonitored out-of-hospital cardiac arrest. Ann Emerg Med. 1995;25:780–784. doi: 10.1016/s0196-0644(95)70207-5. [DOI] [PubMed] [Google Scholar]
- 11.Copley DP, Mantle JA, Rogers WJ, Russell RO, Jr, Rackley CE. Improved outcome for prehospital cardiopulmonary collapse with resuscitation by bystanders. Circulation. 1977;56:901–905. doi: 10.1161/01.cir.56.6.901. [DOI] [PubMed] [Google Scholar]
- 12.Nichol G, Stiell IG, Hebert P, Wells GA, Vandemheen K, Laupacis A. What is the quality of life for survivors of cardiac arrest? A prospective study. Acad Emerg Med. 1999;6:95–102. doi: 10.1111/j.1553-2712.1999.tb01044.x. [DOI] [PubMed] [Google Scholar]
- 13.Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group. Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 14.Wik L, Steen PA, Bircher NG. Quality of bystander cardiopulmonary resuscitation influences outcome after prehospital cardiac arrest. Resuscitation. 1994;28:195–203. doi: 10.1016/0300-9572(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 15.Ristagno G, Tang W, Chang YT, et al. The quality of chest compressions during cardiopulmonary resuscitation overrides importance of timing of defibrillation. Chest. 2007;132:70–75. doi: 10.1378/chest.06-3065. [DOI] [PubMed] [Google Scholar]
- 16.Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–2516. doi: 10.1161/hc4601.099468. [DOI] [PubMed] [Google Scholar]
- 17.Bang A, Biber B, Isaksson L, Lindqvist J, Herlitz J. Evaluation of dispatcher-assisted cardiopulmonary resuscitation. Eur J Emerg Med. 1999;6:175–183. [PubMed] [Google Scholar]
- 18.Culley LL, Clark JJ, Eisenberg MS, Larsen MP. Dispatcher-assisted telephone CPR: common delays and time standards for delivery. Ann Emerg Med. 1991;20:362–366. doi: 10.1016/s0196-0644(05)81655-5. [DOI] [PubMed] [Google Scholar]
- 19.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 20.Cheung S, Deakin CD, Hsu R, Petley GW, Clewlow F. A prospective manikin-based observational study of telephone-directed cardiopulmonary resuscitation. Resuscitation. 2007;72:425–435. doi: 10.1016/j.resuscitation.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 21.Abella BS, Aufderheide TP, Eigel B, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation. A scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008 doi: 10.1161/CIRCULATIONAHA.107.188486. Available at http://www.circ.ahajournals.org/cgi/content/abstract/CIRCULATIONAHA.107.188486v1. [DOI] [PubMed]
- 22.Dias JA, Brown TB, Saini D, et al. Simplified dispatch-assisted CPR instructions outperform standard protocol. Resuscitation. 2007;72:108–114. doi: 10.1016/j.resuscitation.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 23.Brown TB, Saini D, Pepper T, et al. Instructions to “put the phone down” do not improve the quality of bystander initiated dispatcher assisted cardiopulmonary resuscitation. Resuscitation. 2008;76:249–255. doi: 10.1016/j.resuscitation.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 24.ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV-1–IV-5. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 25.Deakin CD, Cheung S, Petley GW, Clewlow F. Assessment of the quality of cardiopulmonary resuscitation following modification of a standard telephone-directed protocol. Resuscitation. 2007;72:436–443. doi: 10.1016/j.resuscitation.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Brown TB, Dias JA, Saini D, et al. Relationship between knowledge of cardiopulmonary resuscitation guidelines and performance. Resuscitation. 2006;69:253–261. doi: 10.1016/j.resuscitation.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 28.Ødegaard S, Kramer-Johansen J, Bromley A, et al. Chest compressions by ambulance personnel on chests with variable stiffness: abilities and attitudes. Resuscitation. 2007;74:127–134. doi: 10.1016/j.resuscitation.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005;67 Suppl 1:S7–S23. doi: 10.1016/j.resuscitation.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Holmberg M, Holmberg S, Herlitz J. Swedish Cardiac Arrest Registry. Factors modifying the effect of bystander cardiopulmonary resuscitation on survival in out-of-hospital cardiac arrest patients in Sweden. Eur Heart J. 2001;22:511–519. doi: 10.1053/euhj.2000.2421. [DOI] [PubMed] [Google Scholar]
- 31.Clark JJ, Culley L, Eisenberg M, Henwood DK. Accuracy of determining cardiac arrest by emergency medical dispatchers. Ann Emerg Med. 1994;23:1022–1026. doi: 10.1016/s0196-0644(94)70097-4. [DOI] [PubMed] [Google Scholar]
- 32.Hauff SR, Rea TD, Culley LL, Kerry F, Becker L, Eisenberg MS. Factors impeding dispatcher-assisted telephone cardiopulmonary resuscitation. Ann Emerg Med. 2003;42:731–737. doi: 10.1016/s0196-0644(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 33.Odegaard S, Saether E, Steen PA, Wik L. Quality of lay person CPR performance with compression: ventilation ratios 15:2, 30:2 or continuous chest compressions without ventilations on manikins. Resuscitation. 2006 Dec;71(3):335–340. doi: 10.1016/j.resuscitation.2006.05.012. Epub 2006 Oct 27. [DOI] [PubMed] [Google Scholar]
- 34.Dorph E, Wik L, Steen PA. Dispatcher-assisted cardiopulmonary resuscitation. An evaluation of efficacy amongst elderly. Resuscitation. 2003;56:265–273. doi: 10.1016/s0300-9572(02)00374-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.