Abstract
We compared functional imaging modalities including positron emission tomography (PET) with 6-[18F]-fluorodopamine ([18F]-DA) against [123I]-metaiodobenzylguanidine ([123I]-MIBG) and somatostatin receptor scintigraphy (SRS) with [111In]-pentetreotide (Octreoscan) in non-metastatic and metastatic pheochromocytoma (PHEO). Methods: We studied 25 men and 28 women (mean age±SD: 44.2±14.2 years) with biochemically-proven non-metastatic (n: 17) or metastatic (n: 36) PHEO. Evaluation included anatomical imaging with computed tomography (CT) and/or magnetic resonance imaging (MRI) and functional imaging that included at least two nuclear medicine modalities: [18F]-DA PET, [123I]-MIBG scintigraphy, or SRS. Sensitivity of functional imaging vs. anatomical imaging was assessed on a per-patient and on a per-region basis.
Results
For this available cohort, on a per patient basis, overall sensitivity (combined for non-metastatic and metastatic PHEO) was 90.2% for [18F]-DA PET, 76.0% for [123I]-MIBG scintigraphy, and 22.0% for SRS. On a per-region basis, overall sensitivity was 75.4% for [18F]-DA PET, 63.4% for [123I]-MIBG scintigraphy, and 64.0% for SRS.
Conclusion
If available, [18F]-DA PET should be used in the evaluation of PHEO, since it is more sensitive than [123I]-MIBG scintigraphy or SRS. If [18F]-DA PET is not available, [123I]-MIBG scintigraphy (for non-metastatic/adrenal PHEO) and SRS (for metastatic PHEO) should be the first alternative imaging methods to be used.
Keywords: Radionuclide imaging, [18F]-fluorodopamine, [123I]-metaiodobenzylguanidine, [111In]-pentetreotide, pheochromocytoma
Introduction
Until recently the gold standard functional imaging method for pheochromocytoma (PHEO) was scintigraphy with [131I]-metaiodobenzylguanidine ([131I]-MIBG), with sensitivity of 77–90% and excellent specificity of 95–100% (1). However, it is scintigraphy with another radionuclide, [123I]-MIBG, that offers the option of performing single-photon emission computed tomography (SPECT) and is reported to have sensitivity of 83%–100% and specificity of 95%–100% for detecting PHEOs (2–4). Scintigraphic imaging with [123I]-MIBG is advantageous because of its optimal gamma emissions and lack of beta particles that result in a lower absorbed dose compared to [131I]-MIBG (5). Availability of [123I]-MIBG compared to [131I]-MIBG is limited, but it is expanding rapidly, especially in the United States. At present, large studies comparing various functional imaging modalities to [123I]-MIBG scintigraphy in the evaluation of pheochromocytoma are lacking.
Positron emission tomography (PET) also enables functional imaging of endocrine tumors. Although PET with [18F]-fluorodeoxyglucose (FDG), ([18F]-FDG) has been used with some success for imaging metastatic PHEO, it is nevertheless a non-specific ligand, which shows uptake in various tumors(6–8). Other ligands like [11C]-hydroxyephedrine and [11C]-epinephrine have also been used successfully for PET imaging of PHEOs (9–12). [18F]-labeled dihydroxyphenylalanine ([18F]-DOPA) has enabled PET imaging of benign PHEOs and neck neuroendocrine tumors (13, 14). Recently, we recommended the use of PET with 6-[18F]-fluorodopamine ([18F]-DA) for the detection of PHEO (15–17). Our studies have suggested that [18F]-DA is a better agent for localization of metastatic PHEO than [131I]-MIBG (with 100% sensitivity vs. 56% sensitivity, respectively) (15, 16). This is probably due to better affinity of [18F]-DA for the norepinephrine membrane transport system than MIBG, and the increased resolution of PET compared to planar gamma camera imaging.
From in vitro and in vivo studies it has been established that somatostatin receptor subtypes 3 and 4 are expressed in PHEO, including adrenal and metastatic disease (18–21). Although somatostatin receptor scintigraphy (SRS) with [111In]-pentetreotide (Octreoscan) has only moderate affinity for these subtypes compared to subtypes 2 and 5, SRS has been used with variable results to detect this tumor (18, 22–25). SRS reportedly detects neck paragangliomas with 94%–97% sensitivity (26–28), and has higher sensitivity for detecting metastatic PHEO compared to benign PHEO (29). Nevertheless, in a small study of 10 patients with malignant PHEO and 3 patients with malignant paraganglioma that compared SRS vs. [131I]-MIBG or [123I]-MIBG scintigraphy, 26 lesions were MIBG- and SRS-positive, 15 lesions were only MIBG –positive and 7 lesions were only SRS-positive (overall sensitivity for [131I]-MIBG or [123I]-MIBG scintigraphy was 85% and 92% for SRS) (18)
The aim of this study was to compare [18F]-DA PET, [123I]-MIBG, and SRS in the localization of adrenal, extra-adrenal, and metastatic or multiple PHEOs in a large study from a single institution. We also evaluated which of these radiopharmaceuticals detected the largest number of lesions in patients with metastatic PHEO. Furthermore, we aimed to give physicians new information and recommendations as to the use of various functional imaging methods when a non-metastatic or metastatic PHEO is localized.
Subjects and methods
All patients were enrolled in a National Institute of Child Health and Human Development Institutional Review Board-approved study of PHEO. Written informed consent was obtained from all patients.
Subjects were retrospectively chosen from a larger group of 178 patients originally enrolled in a study of known or suspected pheochromocytoma. Specifically, inclusion criteria for this parent protocol included positive biochemistry, suggestive biochemistry with clinical signs and/or symptoms of catecholamine excess; and a family history of pheochromocytoma with a tumor found on anatomical imaging studies even without clinical signs or symptoms. Exclusion criteria included inability to give informed consent and refusal or inability to undergo examination, including many imaging studies (claustrophobia, previous irradiation or extreme obesity). Children less than 18 years old and pregnant subjects were also excluded.
From this pool of 178 patients, 53 were retrospectively chosen for inclusion in this study based on confirmed positive biochemical evidence of PHEO [using an in-house assay, as previously described (30, 31)] and availability of certain imaging studies, including anatomical imaging (CT and/or MRI) and at least two of three of the following functional modalities ([18F]-DA PET, [123I]-MIBG scintigraphy or SRS) The imaging studies were required to have been contemporaneously performed within three months of each other.
CT scans of the neck, chest, abdomen, and pelvis were performed on a variety of equipment, including LightSpeed Ultra, LightSpeed QX/i, HiSpeed CT/i (General Electric Healthcare Technologies, Waukesha, WI) and Mx8000 IDT (Philips Medical Systems, Andover, MA) scanners. Section thickness was at the radiologists’ discretion and was set up to 3 mm in the neck, 5 mm in the chest and abdomen, and 7.5 mm in the pelvis, except for two cases where neck imaging was performed with either 3.75 or 5 mm images, and another case where chest, abdomen, and pelvis images were obtained with 10 mm thickness. All sections were contiguous. All studies were performed with a rapid infusion (130 mL injected at 2 mL/sec) of nonionic water-soluble contrast agent..
MRI scans of the neck, chest, abdomen, and pelvis were obtained with 1.5-T Signa scanners (General Electric Healthcare Technologies, Waukesha, WI), except for one study obtained at an outside institution. Phased array coils were employed for neck imaging, and either phased array torso or quadrature body coils elsewhere. T1-weighted gradient-echo and fat-suppressed fast spin-echo T2-weighted imaging parameters were adjusted so as to minimize examination time while achieving desired anatomic coverage. Images were obtained in the axial plane, with additional planes when needed. All studies included gadolinium-DTPA contrast injection, using fat-suppressed T1-weighted gradient-echo imaging in axial and coronal planes.
For [18F]-DA PET scanning, the patients were studied fasted overnight and were asked to avoid caffeine, tobacco, and alcohol for at least 12 h before the scan. [18F]-DA (1.0 mCi; 37 MBq) in 10 mL of normal saline was infused intravenously over 3 min. Attenuation-corrected images were obtained starting immediately after injection. [18F]-DA PET scanning was performed using a General Electric Advance scanner (General Electric, Milwaukee, WI) with a 15-cm field of view. The images were acquired in 2-dimensional mode from the base of the skull to the proximal thigh (in some patients with a high suspicion of lesions in the head or the lower limbs the PET studies also fully covered these areas). The duration of emission scanning was 8 to 15 minutes at each level. At least 1 transmission scan of 3 to 5 minutes duration was obtained at each level for attenuation correction.
For [123I]-MIBG scanning, patients were imaged following intravenous administration of 10.0 mCi (370 MBq) [123I]-MIBG. Patients were instructed to take 100 mg of saturated solution of potassium iodide (SSKI) by mouth twice a day for 4 days, starting the night before MIBG administration. Medications known to interfere with MIBG uptake were discontinued. Planar and SPECT images were acquired on a dual-headed gamma camera (ADAC Laboratories, Milipitas, CA or Siemens Medical Solutions USA, Malvern, PA) and triple headed gamma camera (Trionix XLT, Trionix Laboratories, Twinsburg, OH), respectively, equipped with low energy high resolution collimators. 120 sequential (40 stops per head) 40 sec images were obtained. The images were reconstructed with the manufacturers software using a standard filtered back-projection algorithm. A Butterworth filter was used for reconstruction. Twenty-four hours after injection, whole body and SPECT of the head through the pelvis was performed. SPECT studies were repeated at 48 hours as needed.
For SRS, patients were imaged approximately 4 and 24 hours following intravenous administration of 6 mCi (222 MBq) of 111In pentetreotide. Whole body scans and SPECT scans of the head through the pelvis were acquired on a dual-headed gamma camera (ADAC Laboratories, Milipitas, CA or Siemens Medical Solutions USA, Malvern, PA) and triple headed gamma camera (Trionix XLT, Trionix Laboratories, Twinsburg, OH), respectively, equipped with medium-energy general-purpose collimators. On occasion, 48–hour SPECT images were also obtained. 120 sequential 40 sec images were obtained. The images were reconstructed with the manufacturers software using a standard filtered back-projection algorithm. A Hamming filter was used for reconstruction
The radiologist (AL) who interpreted CT and MRI scan was blinded to the results of [18F]-DA PET, [123I]-MIBG scintigraphy, and SRS. Moreover, nuclear medicine studies were read independent of each other and of the anatomical studies by two physicians (CCC, JAC). Sites of uptake outside of the normal distribution were considered abnormal. [123I]-MIBG uptake in the adrenal glands was considered normal if it was mild, symmetric, and not enlarged. However, any visualized uptake of [18F]-DA in the adrenals was considered to be abnormal, based on previous experience with studies in a small number of normal volunteers which did not show any adrenal[18F]-DA uptake(please see Discussion) Abnormal foci seen in nuclear medicine studies were graded on a scale of 1–5 (1 = not PHEO 2 = probably not pheo, 3 = equivocal, 4 = probable, 5 = definite PHEO). Only lesions with scores of 4 and 5 were counted as positive findings. Discrepancies in scans from the first individual blinded reading were resolved by a joint meeting of both nuclear medicine physicians in a consensus review (with re-examination and discussion of the studies in question)
Comparison of the results of the nuclear medicine modalities was done on a per-patient basis and on a per region basis. For the former, scans were considered positive if at least one lesion with a score of 4/5 or 5/5 was seen, regardless of the number of foci (scans with no or equivocal uptake were scored as negative). Since histologic proof of metastatic lesions was largely unavailable, findings on CT and/or MRI were taken as our reference of standard (despite shortcomings of these modalities – please see Discussion section) for sensitivity calculations of imaging studies. Sensitivity by patient was calculated as follows: (number of patients positive on [18F]-DA PET or [123I]-MIBG scintigraphy or SRS)/number of patients positive on CT/MRI.
Analysis on a per-region basis was done over the following areas: left adrenal gland, right adrenal gland, liver, abdominal/pelvic compartment (excluding adrenal glands and liver), lungs, mediastinum, neck, and bone (including skull). For sensitivity calculations, studies were considered either positive or negative, regardless of the number of lesions detected in each region. CT and/or MRI were considered to be the reference standard. Sensitivity by region was calculated as follows: (number of regions positive on [18F]-DA PET or [123I]-MIBG scintigraphy or SRS)/number of regions positive on CT/MRI. Only regions that were actually covered by [18F]-DA PET or [123I]-MIBG scintigraphy or SRS as well as by either CT or MRI (CT/MRI) were included.
The McNemar test was used to compare sensitivities between different imaging modalities. A two-sided P<0.05 was considered significant.
Results
Imaging results from 25 men and 28 women (mean age±SD: 44.2±14.2 years) with biochemically-proven non-metastatic (n: 17; two patients with recurrent disease. Ten patients had T1N0M0 disease, stage I, 3 patients with T2N0Mo disease, stage II and 4 with T4N0Mo disease, stage IV) or metastatic (n: 36; all with stage IV disease: 9 with T1N0M1, 10 with T1N1M1, 1 with T2N0M1, 1 with T2N1M1, 5 with T4N0M1 and 10 with T4N1M1 disease) PHEOs were assessed. All patients were studied with CT (51 scans) and/or MRI (47 scans); Two patients had only MRI scans. Functional imaging included [18F]-DA PET and [123I]-MIBG scintigraphy in 16 patients with non-metastatic and 35 patients with metastatic PHEO and SRS in 7 patients with non-metastatic and 18 patients with metastatic PHEO. Five patients with non-metastatic and 15 with metastatic PHEO were studied with all three functional imaging modalities.
Anatomic imaging was positive in all patients. Most lesions seen on CT/MRI showed uptake with at least one functional imaging modality. In a few patients the enormous number of metastatic lesions did not permit direct one-to-one comparisons, hence the comparisons on a per-patient and on a per –region basis. In patients with non-metastatic PHEO, negative functional imaging studies were obtained in 2 patients with [18F]-DA PET, 2 patients with [123I]-MIBG scintigraphy and 5 patients with SRS. More in detail, since evaluation on a per-lesion basis was feasible only on these patients with non-metastatic PHEO: 16 lesions positive on CT/MRI were “missed” by either [18F]-DA PET or [123I]-MIBG (in 16 patients), whereas 13 lesions positive on CT/MRI were “missed” by SRS (in 7 patients). In patients with metastatic PHEO, negative functional imaging studies were obtained in 4 patients with [18F]-DA PET, 9 patients with [123I]-MIBG scintigraphy and 1 patient with SRS.
For this available cohort, on a per-patient basis, sensitivity was equal for [18F]-DA PET and [123I]-MIBG scintigraphy (87.5%) and lower for SRS (28.5%) in patients with non-metastatic PHEO (Table 1). In patients with metastatic PHEO, sensitivity was 91.4% for [18F]-DA PET, 70.6% for [123I]-MIBG, and 88.9% for SRS (Table 1). Overall sensitivity (combined for non-metastatic and metastatic PHEO) was 90.2% for [18F]-DA PET, 76.0% for [123I]-MIBG, and 22.0% for SRS. Furthermore, on a per-region basis, sensitivity for [18F]-DA PET was 67%, 75% for [123I]-MIBG, and 37.5% for SRS in patients with non-metastatic PHEO (Table 2). In patients with metastatic PHEO, sensitivity with [18F]-DA PET was 78.4%, 58.9% for [123I]-MIBG, and 68.5% for SRS (Table 2). Overall sensitivity (combined for non-metastatic and metastatic PHEO) was 75.4% for [18F]-DA PET, 63.4% for [123I]-MIBG, and 64.0% for SRS.
Table 1.
Results and comparisons of imaging modalities by patient.
| Non-metastatic PHEO
| ||
|---|---|---|
| Functional imaging modality studies | vs. CT/MRI (+) studies: | Sensitivity of functional imaging modality |
| [18F]-DA (+): 14 | 16 | 87.5% |
| [123I]-MIBG (+): 14 | 16 | 87.5% |
| SRS (+): 2 | 7 | 28.5%* |
|
| ||
| Metastatic PHEO | ||
|
| ||
| Functional imaging modality studies | vs. CT/MRI (+) studies: | Sensitivity of functional imaging modality |
|
| ||
| [18F]-DA PET (+): 32 | 35 | 91.4% |
| [123I]-MIBG (+): 24 | 34 | 70.6% |
| SRS (+): 16 | 18 | 88.9% |
p=0.0625, McNemar test; sensitivity of functional imaging studies was calculated based on the number of CT/MRI studies used as the reference standard.
Table 2.
Results and comparisons of imaging modalities by region (left adrenal gland, right adrenal gland, liver, abdominal/pelvic compartment (excluding adrenal glands and liver), lungs, mediastinum, neck and bone (including head and/or skull)).
| Non-metastatic PHEO
| ||
|---|---|---|
| Functional imaging modality – regions with foci of uptake | vs. CT/MRI (+) regions: | Sensitivity of functional imaging modality |
| [18F]-DA (+): 20 | 30 | 67.0%* |
| [123I]-MIBG (+): 21 | 28 | 75.0%** |
| SRS (+): 3 | 8 | 37.5%*** |
|
| ||
| Metastatic PHEO | ||
|
| ||
| Functional imaging modality – regions with foci of uptake | vs. CT/MRI (+) regions: | Sensitivity of functional imaging modality |
|
| ||
| [18F]-DA (+): 69 | 88 | 78.4%* |
| [123I]-MIBG (+): 56 | 95 | 58.9%* |
| SRS (+): 37 | 54 | 68.5%* |
p=0.001, McNemar test;
p=0.01, McNemar test;
p=0.0625, McNemar test; sensitivity of functional imaging studies was calculated based on the number of CT/MRI studies used as the reference standard.
In a number of patients, functional imaging modalities showed lesions in regions that were negative on CT and/or MRI. With [18F]-DA PET, this occurred in 5 more patient regions in 5 patients (in the adrenals or the abdominal/pelvic compartment), and with [123I]-MIBG scintigraphy, one additional positive region in one patient (in the right adrenal) was seen compared to the CT and/or MRI.
In patients with non-metastatic PHEO that were studied with all three functional imaging modalities, [18F]-DA PET and [123I]-MIBG scintigraphy were more positive on a per patient and on a per region basis than SRS (Table 3; Figure 1). In patients with metastatic PHEO that were studied with all three functional imaging modalities [18F]-DA PET and SRS were more positive on a per patient basis than [123I]-MIBG scintigraphy, whereas on a per region basis, SRS was more positive than [18F]-DA PET and [123I]-MIBG scintigraphy (Table 3; Figure 2).
Table 3.
Results and comparisons among functional imaging modalities by patient and by region (left adrenal gland, right adrenal gland, liver, abdominal/pelvic compartment (excluding adrenal glands and liver), lungs, mediastinum, neck and bone (including head and/or skull)) in those studied with [18F]-DA PET, [123I]-MIBG scintigraphy and SRS.
| Non-metastatic PHEO (n=5)
| ||
|---|---|---|
| Functional imaging modality | (+) patient studies: | (+) regions: |
| [18F]-DA | 5 | 6 |
| [123I]-MIBG | 5 | 5 |
| SRS | 1 | 1 |
|
| ||
| Metastatic PHEO (n=15) | ||
|
| ||
| Functional imaging modality | (+) patient studies: | (+) regions: |
|
| ||
| [18F]-DA | 14 | 31 |
| [123I]-MIBG | 10 | 31 |
| SRS | 15 | 44 |
Figure 1.
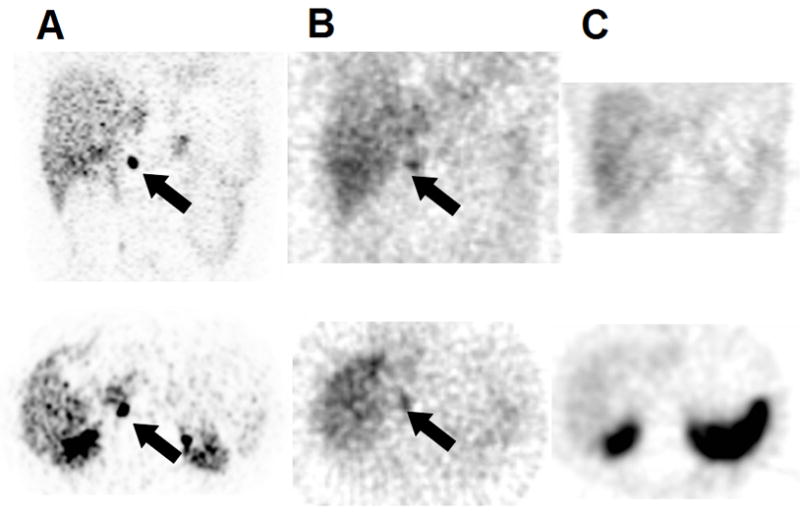
(A) Coronal (upper panels) and transverse (lower panels) [18F]-DA, (B) 24hr [123I]-MIBG and (C) 4hr SRS images of a 23 year-old male with non-metastatic recurrent right adrenal pheocromocytoma. [18F]-DA PET and [123I]-MIBG scintigraphy are both positive (arrows) whereas SRS is negative.
Figure 2.

(A) Reprojected [18F]-DA, (B) 24hr [123I]-MIBG and (C) 4hr reprojected SRS images of a 60 year-old female with left adrenal pheochromocytoma and peritoneal and retroperitoneal metastases (white arrowheads). [18F]-DA PET and SRS (black arrows) show more lesions than [123I]-MIBG scintigraphy.
Discussion
In the present -- largest to date -- comparison study of [18F]-DA PET with [123I]-MIBG scintigraphy and SRS in 17 patients with non-metastatic PHEO and 36 patients with metastatic PHEO, overall more foci of uptake were shown with [18F]-DA PET than with the other functional imaging modalities. In non-metastatic PHEO, [18F]-DA PET imaged slightly fewer foci than [123I]-MIBG scintigraphy (and both detected more foci than SRS), but in metastatic PHEO, it was [18F]-DA PET that detected more foci than [123I]-MIBG scintigraphy and SRS. There were some, mainly metastatic, lesions that were only localized by one modality, but no distinct pattern for any particular tumor size or region emerged. Overall, the scintigraphic modality with the highest sensitivity for localizing PHEO was [18F]-DA PET (75.4%), followed by [123I]-MIBG (63.4%) and SRS (64%).
In many patients with PHEO (especially those with extra-adrenal PHEO, adrenal PHEO larger than 5 cm, or in patients with mutations of genes encoding mainly subunits B and D of the mitochondrial enzyme succinate dehydrogenase; SDHB and SDHD), the possibility of metastatic disease or multiple tumors should be considered (or excluded). For this, functional imaging modalities are most useful (3, 6, 9, 16, 17, 32–34). The sensitivity of CT and MRI for detecting extra-adrenal or metastatic PHEO is approximately 90% (or lower, when postoperative changes prevent the correct localization of tumors) (35–39). Moreover, the specificities of both CT and MRI scans are disappointingly low (as low as 60%), in localizing PHEO (particularly metastatic PHEO) (3). In this study, both CT and MRI also missed lesions that were detected by functional imaging studies. While we do not have surgical confirmation that the lesions seen on functional imaging and not on anatomical imaging were PHEO, we feel confident that most of them were real based on clinical follow-up, including improvement after chemotherapy or [131I]-MIBG therapy in many cases.
PET is a physiologic method of imaging that depends on selective binding or uptake and retention of radiolabeled agents by different tissues. It has the advantages of rapid imaging and high spatial and temporal resolution. Several PET imaging agents have been used for localizing PHEO, including [18F]-FDG (6, 12, 40), [11C]-hydroxyephedrine (10, 12, 41), [11C]-epinephrine (11), [18F]-DA (15, 16), and [18F]-dihydroxyphenylalanine ([18F]-DOPA) (13, 14). A comparison study of [131I]- and [123I]-MIBG and [18F]-FDG PET scans in patients with malignant PHEO showed that [18F]-FDG PET was superior to MIBG scanning (6). Furthermore, [18F]-FDG-PET was recently shown to be superior to [18F]-DA or [123I]-MIBG in localizing metastases of highly malignant paragangliomas (in particular those with SHDB mutations) (7). However, FDG remains nonspecific for PHEO, as it also detects many other types of tumors. PET with [11C]-hydroxyephedrine and [11C]-epinephrine have yielded better results compared to [18F]-FDG in terms of the diagnostic localization of pheochromocytoma, although the short physical half-lives (T1/2 = 20 min) of these radiopharmaceuticals will likely preclude their more widespread use (10, 12, 41). Recently, PET with [18F]-DOPA, a labeled precursor of dopamine, was used in a study of 14 patients with benign adrenal PHEOs and a small number of patients (n=3) with extra-adrenal non-metastatic PHEO (14). In the former group, all tumors were localized with [18F]-DOPA PET, while in the latter group, [18F]-DOPA PET imaging was concordant with MRI results in 1 of 3 patients and imaged a tumor that was not seen with [131I]-MIBG scintigraphy (14). In another study of 10 patients with glomus jugulare tumors (which arise from the paraganglionic tissue of the head and neck and are similar to PHEOs), 11 of the 15 presumed tumors diagnosed by [18F]-DOPA PET were confirmed by MRI (13).
At the NIH, we have used [18F]-DA with excellent results in localizing both adrenal and extra-adrenal PHEOs, including metastatic lesions (15, 16, 42, 43). In a previous study of patients with metastatic PHEO, we found that [18F]-DA PET was clearly superior to [131I]-MIBG (with sensitivities of 100% and 56%, respectively) (16). The availability of [123I]-MIBG prompted us to compare it with [18F]-DA PET as well. In the present study, in patients with non-metastatic (mainly adrenal) PHEOs, [18F]-DA and [123I]-MIBG had equivalent sensitivities for tumor detection, and both were superior to SRS. In patients with metastatic disease, [18F]-DA was superior to [123I]-MIBG and detected more lesions. Interestingly, in a minority of these patients, SRS showed impressively more lesions compared to [123I]-MIBG. Additional advantages of PET compared to other functional imaging modalities include the means of immediate whole-body imaging, the possibility of quantitative assessment of uptake and the absence of artifacts from scar tissue or from the presence of metallic clips post-surgery and (44). In fact, [18F]-FDA scan artifacts appear to be quite rare, and in this study, none were noted except for mild adrenal uptake in some patients which was scored as abnormal (although with further experience, we have since found that this can be normal -see further Discussion below). Known artifacts with [18F]-FDA scanning also include uptake in adrenal hyperplasia and metabolically active brown fat.
In PHEO, [131I]-MIBG scanning offers high specificity (95%–100%) with lower sensitivity (56%–77%) (43, 45). Using [123I]-MIBG, sensitivity is elevated to 78%–91% and specificity is preserved (3, 46, 47). In the present study, [123I]-MIBG was as sensitive as [18F]-DA, and definitely superior to SRS in localizing non-metastatic PHEO. However, in the evaluation of metastatic PHEO, [123I]-MIBG was the least informative scintigraphic modality, lagging behind [18F]-DA and SRS.
SRS is used effectively for the diagnostic localization of neuroendocrine tumors (48, 49). In a small number of reports comparing the diagnostic accuracy of SRS and [123I]- or [131I]-MIBG scanning in patients with metastatic PHEO, SRS was noted to have an overall higher detection rate: SRS found up to 87% of lesions, whereas [123I]-MIBG localized only 57% (4, 18, 24, 25, 29).
We believe that SRS studies may be particularly useful as a functional imaging modality in patients with rapidly progressing and growing PHEOs. In these PHEOs changes in genetic and cellular characteristics occur, currently by unknown mechanisms, such as the expression of somatostatin receptors. In this study, SRS failed to detect the 5/7 tumors in patients with non metastatic disease. However, in metastatic PHEO, while [18F]-DA localized many lesions that SRS did not, SRS also showed a substantial number of metastatic lesions that were not detected with [18F]-DA. SRS also showed more lesions than MIBG in patients with metastatic disease ([123I]-MIBG provided the least additional information in these patients). Clinically, patients with predominantly SRS-positive lesions had rapidly progressing tumors, based on our clinical follow-up, repeated biochemistry and anatomical imaging studies.
This report has shortcomings that should be mentioned. First, only one patient with extra-adrenal non-metastatic PHEO was studied, and future studies are needed to address this subset of patients. Second, only five patients with non-metastatic PHEO were studied with all three functional imaging modalities, a deficiency that needs to be addressed as well. Third, most patients with metastatic PHEO did not undergo surgery as it could not be justified clinically, and therefore, surgical confirmation of disease is not available for most lesions in these patients. Fourth, the SRS studies were fewer than [18F]-DA and [123I]-MIBG studies; with such unequal size groups, selection bias towards doing SRS studies in patients with metastatic disease may have occurred. Fifth, we considered [18F]-DA uptake in the adrenals as being abnormal. However, with further experience and the use of PET/CT, we have since found that normal adrenal glands in some patients may demonstrate mild adrenal uptake of [18F]-DA (lean body mass SUVmax <7.3 ) (50). Finally, ascertainment bias (i.e. the tendency to produce false results and conclusions based on a distorted or nontypical sample) may have occurred, principally due to the rareness of the tumors that were studied. Nevertheless, despite negative MIBG scans before referral, in 1 patient with non-metastatic and 4 with metastatic PHEOs, all the study’s subjects had indeed biochemical proof of disease.
In conclusion, this study shows that in the diagnostic evaluation of PHEO, [18F]-DA PET and [123I]-MIBG are more sensitive than SRS in detecting non-metastatic primary adrenal PHEO. For metastatic PHEO, [18F]-DA is more sensitive than SRS, and both are superior to [123I]-MIBG. In patients with rapidly progressing and growing PHEOs, SRS may detect lesions that are negative on both [18F]-DA and [123I]-MIBG. In a study of patients with familial-SDHB-associated disease PET with [18F]-FDG was shown to be the superior functional imaging method. In those patients with PHEO where anatomical imaging modalities indicate adrenal disease, [123I]-MIBG is a valuable imaging modality to be used; this modality is comparable with other specific imaging methods such as [18F]-DA PET. For those with metastatic disease, SRS can be used. However, this approach should not exclude [18F]-DA PET scanning, which is as sensitive as [123I]-MIBG and SRS for non-metastatic and metastatic PHEO, respectively. As PET scanning becomes more available, we expect that either [18F]-DA PET or PET with another specific PET ligand will become the method of choice for functional imaging of non-metastatic and metastatic PHEO.
Acknowledgments
This work was supported in part by the Intramural Research Program of the National Institute of Child Health and Human Development. The authors have no conflict of interest to disclose.
Footnotes
This PDF receipt will only be used as the basis for generating PubMed Central (PMC) documents. PMC documents will be made available for review after conversion (approx. 2-3 weeks time). Any corrections that need to be made will be done at that time. No materials will be released to PMC without the approval of an author. Only the PMC documents will appear on PubMed Central -- this PDF Receipt will not appear on PubMed Central.
References
- 1.Sisson JC, Shulkin BL. Nuclear medicine imaging of pheochromocytoma and neuroblastoma. Q J Nucl Med. 1999;43:217–223. [PubMed] [Google Scholar]
- 2.Nielsen JT, Nielsen BV, Rehling M. Location of adrenal medullary pheochromocytoma by I-123-metaiodobenzylguanidine SPECT. Clin Nucl Med. 1996;21:695–699. doi: 10.1097/00003072-199609000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Furuta N, Kiyota H, Yoshigoe F, Hasegawa N, Ohishi Y. Diagnosis of pheochromocytoma using [123I]-compared with [131I]-metaiodobenzylguanidine scintigraphy. Int J Urol. 1999;6:119–124. doi: 10.1046/j.1442-2042.1999.06310.x. [DOI] [PubMed] [Google Scholar]
- 4.van der Harst E, de Herder WW, Bruining HA, et al. [(123)I]metaiodobenzylguanidine and [(111)In]octreotide uptake in benign and malignant pheochromocytomas. J Clin Endocrinol Metab. 2001 Feb;86(2):685–693. doi: 10.1210/jcem.86.2.7238. [DOI] [PubMed] [Google Scholar]
- 5.International Commission on Radiological Protection. Radiation dose to patients from radiopharmaceuticals. Vol. 53. Oxford, UK: Pergamon Press; 1988. pp. 329–331. Vol ICRP publication. [Google Scholar]
- 6.Shulkin BL, Thompson NW, Shapiro B, Francis IR, Sisson JC. Pheochromocytomas: imaging with 2-[fluorine-18]fluoro-2-deoxy-D-glucose PET. Radiology. 1999;212:35–41. doi: 10.1148/radiology.212.1.r99jl3035. [DOI] [PubMed] [Google Scholar]
- 7.Timmers JLM, Kozupa A, Chen CC, et al. Superiority of fluorodeoxyglucose positron emission tomography to other functional imaging techniques in the evaluation of metastatic SDHB-associated pheochromocytoma and paraganglioma. J Clin Oncol. 2007;25:2262–2269. doi: 10.1200/JCO.2006.09.6297. [DOI] [PubMed] [Google Scholar]
- 8.Mamede M, Carrasquillo JA, Chen CC, et al. Discordant localization of 2-[18F]-fluoro-2-deoxy-D-glucose in 6-[18F]-fluorodopamine- and [(123)I]-metaiodobenzylguanidine-negative metastatic pheochromocytoma sites. Nucl Med Commun. 2006;27:31–36. doi: 10.1097/01.mnm.0000189780.54658.e8. [DOI] [PubMed] [Google Scholar]
- 9.Trampal C, Engler H, Juhlin C, Bergstrom M, Langstrom B. Pheochromocytomas: detection with 11C hydroxyephedrine PET. Radiology. 2004;230:423–428. doi: 10.1148/radiol.2302021678. [DOI] [PubMed] [Google Scholar]
- 10.Shulkin BL, Wieland DM, Schwaiger M, et al. PET scanning with hydroxyephedrine: an approach to the localization of pheochromocytoma. J Nucl Med. 1992;33:1125–1131. [PubMed] [Google Scholar]
- 11.Shulkin BL, Wienland DM, Shapiro B, Sisson JC. PET epinephrine studies of pheochromocytoma. J Nucl Med. 1995;36:229P. [Google Scholar]
- 12.Mann GN, Link JM, Pham P, et al. [(11)C]metahydroxyephedrine and [(18)f]fluorodeoxyglucose positron emission tomography improve clinical decision making in suspected pheochromocytoma. Ann Surg Oncol. 2006;13:187–197. doi: 10.1245/ASO.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 13.Hoegerle S, Ghanem N, Altehoefer C, et al. 18F-DOPA positron emission tomography for the detection of glomus tumours. Eur J Nucl Med Mol Imaging. 2003 May;30(5):689–694. doi: 10.1007/s00259-003-1115-3. [DOI] [PubMed] [Google Scholar]
- 14.Hoegerle S, Nitzsche E, Altehoefer C, et al. Pheochromocytomas: Detection with 18F DOPA Whole-Body PET-Initial Results. Radiology. 2002;222:507–512. doi: 10.1148/radiol.2222010622. [DOI] [PubMed] [Google Scholar]
- 15.Pacak K, Eisenhofer G, Carrasquillo JA, Chen CC, Li ST, Goldstein DS. 6-[18F]fluorodopamine positron emission tomographic (PET) scanning for diagnostic localization of pheochromocytoma. Hypertension. 2001;38:6–8. doi: 10.1161/01.hyp.38.1.6. [DOI] [PubMed] [Google Scholar]
- 16.Ilias I, Yu J, Carrasquillo J, et al. Superiority of 6-[18F]-fluorodopamine positron emission tomography versus [131I]-metaiodobenzylguanidine scintigraphy in the localization of metastatic pheochromocytoma. J Clin Endocrinol Metab. 2003;88:4083–4087. doi: 10.1210/jc.2003-030235. [DOI] [PubMed] [Google Scholar]
- 17.Ilias I, Pacak K. Current Approaches and Recommended Algorithm for the Diagnostic Localization of Pheochromocytoma. J Clin Endocrinol Metab. 2004 February 1, 2004;89(2):479–491. doi: 10.1210/jc.2003-031091. [DOI] [PubMed] [Google Scholar]
- 18.Tenenbaum F, Lumbroso J, Schlumberger M, et al. Comparison of radiolabeled octreotide and meta-iodobenzylguanidine (MIBG) scintigraphy in malignant pheochromocytoma. J Nucl Med. 1995;36:1–6. [PubMed] [Google Scholar]
- 19.Mundschenk J, Lehnert H. Malignant pheochromocytoma. Exp Clin Endocrinol Diabetes. 1998;106(5):373–376. doi: 10.1055/s-0029-1212001. [DOI] [PubMed] [Google Scholar]
- 20.Ueberberg B, Tourne H, Redman A, et al. Differential expression of the human somatostatin receptor subtypes sst1 to sst5 in various adrenal tumors and normal adrenal gland. Horm Metab Res. 2005;37:722–728. doi: 10.1055/s-2005-921092. [DOI] [PubMed] [Google Scholar]
- 21.Unger N, Serdiuk I, Sheu SY, et al. Immunohistochemical determination of somatostatin receptor subtypes 1, 2A, 3, 4, and 5 in various adrenal tumors. Endocr Res. 2004;30:931–934. doi: 10.1081/erc-200044161. [DOI] [PubMed] [Google Scholar]
- 22.Krenning EP, Kwekkekeboom DJ, Bakker WH, et al. Somatostatin receptor scintigraphy with [111In-DTPA-D-phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med. 1993;20:716–731. doi: 10.1007/BF00181765. [DOI] [PubMed] [Google Scholar]
- 23.Lauriero F, Rubini G, D’Addabo F, Rubini D, Schettini F, D’Addabo A. I-131 MIBG scintigraphy of neuroectodermal tumors. Comparison between I-131 MIBG and In-DTPA-octreotide. Clin Nucl Med. 1995;20:243–249. doi: 10.1097/00003072-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Limouris GS, Giannakopoulos V, Stavraka A, Toubanakis N, Vlahos L. Comparison of In-111 pentetreotide, Tc-99m (V)DMSA and I-123 MIBG scintimaging in neural crest tumors. Anticancer Res. 1997;17:1589–1592. [PubMed] [Google Scholar]
- 25.Lastoria S, Maurea S, Vergara E, et al. Comparison of labeled MIBG and somatostatin analogs in imaging neuroendocrine tumors. Q J Nucl Med. 1995;39:145–149. [PubMed] [Google Scholar]
- 26.Bustillo A, Telischi F, Weed D, et al. Octreotide scintigraphy in the head and neck. Laryngoscope. 2004;114:434–440. doi: 10.1097/00005537-200403000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Duet M, Sauvaget E, Petelle B, et al. Clinical impact of somatostatin receptor scintigraphy in the management of paragangliomas of the head and neck. J Nucl Med. 2003;44:1767–1774. [PubMed] [Google Scholar]
- 28.Whiteman ML, Serafini AN, Telischi FF, Civantos FJ, Falcone S. 111In octreotide scintigraphy in the evaluation of head and neck lesions. AJNR Am J Neuroradiol. 1997;18:1073–1080. [PMC free article] [PubMed] [Google Scholar]
- 29.Kaltsas G, Korbonits M, Heintz E, et al. Comparison of somatostatin analog and meta-iodobenzylguanidine radionuclides in the diagnosis and localization of advanced neuroendocrine tumors. J Clin Endocrinol Metab. 2001;86:895–902. doi: 10.1210/jcem.86.2.7194. [DOI] [PubMed] [Google Scholar]
- 30.Eisenhofer G, Lenders JW, Linehan WM, Walther MM, Goldstein DS, Keiser HR. Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med. 1999;340:1872–1879. doi: 10.1056/NEJM199906173402404. [DOI] [PubMed] [Google Scholar]
- 31.Lenders JW, Keiser HR, Goldstein DS, et al. Plasma metanephrines in the diagnosis of pheochromocytoma. Ann Intern Med. 1995;123:101–109. doi: 10.7326/0003-4819-123-2-199507150-00004. [DOI] [PubMed] [Google Scholar]
- 32.Pacak K, Eisenhofer G, Goldstein DS. Functional imaging of endocrine tumors: role of positron emission tomography. Endocr Rev. 2004;25:568–580. doi: 10.1210/er.2003-0032. [DOI] [PubMed] [Google Scholar]
- 33.Ezuddin S, Fragkaki C. MIBG and FDG PET findings in a patient with malignant pheochromocytoma: a significant discrepancy. Clin Nucl Med. 2005;30:579–581. doi: 10.1097/01.rlu.0000170060.52675.14. [DOI] [PubMed] [Google Scholar]
- 34.Shirkare S, Kuwert T, Weckesser M, Czech N, Langen KJ, Muller-Gartner HW. Localization of a pheochromocytoma using I-123 MIBG adrenal scintigraphy. J Postgrad Med. 1994;40:85–87. [PubMed] [Google Scholar]
- 35.Bravo EL. Evolving concepts in the pathophysiology, diagnosis and treatment of pheochromocytoma. Endocr Rev. 1994;15:356–358. doi: 10.1210/edrv-15-3-356. [DOI] [PubMed] [Google Scholar]
- 36.Mannelli M, Ianni L, Cilotti A, Conti A. Pheochromocytoma in Italy: a multicentric retrospective study. Eur J Endocrinol. 1999;142:619–624. doi: 10.1530/eje.0.1410619. [DOI] [PubMed] [Google Scholar]
- 37.Maurea S, Cuocolo A, Reynolds JC, Neumann RD, Salvatore M. Diagnostic imaging in patients with paragangliomas. Computed tomography, magnetic resonance and MIBG scintigraphy comparison. Q J Nucl Med. 1996;40:365–371. [PubMed] [Google Scholar]
- 38.Shapiro B, Sisson JC, Shulkin BL, Gross MD, Zempel S. The current status of meta-iodobenzylguanidine and related agents for the diagnosis of neuro-endocrine tumors. Q J Nucl Med. 1995 Dec;39(4 Suppl 1):3–8. [PubMed] [Google Scholar]
- 39.Schmedtje JFJ, Sax S, Pool JL, Goldfarb RA, Nelson EB. Localization of ectopic pheochromocytomas by magnetic resonance imaging. Am J Med. 1987;83:770–772. doi: 10.1016/0002-9343(87)90912-0. [DOI] [PubMed] [Google Scholar]
- 40.Taniguchi K, Ishizu K, Torizuka T, et al. Metastases of predominantly dopamine-secreting phaeochromocytoma that did not accumulate meta-iodobenzylguanidine: imaging with whole body positron emission tomography using 18F-labelled deoxyglucose. Eur J Surg. 2001;167:866–870. doi: 10.1080/11024150152717733. [DOI] [PubMed] [Google Scholar]
- 41.Trampal C, Hengler H, Juhlin C, Bergstrom M, Langstrom B. Detection of pheochromocytoma using 11C-hydroxyephedrine-PET. Radiology. 2002;225(Suppl):425. doi: 10.1148/radiol.2302021678. [DOI] [PubMed] [Google Scholar]
- 42.Pacak K, Linehan WM, Eisenhofer G, Walther MM, Goldstein DS. Recent advances in genetics, diagnosis, localization and treatment of pheochromocytoma. Ann Int Med. 2001;134:315–329. doi: 10.7326/0003-4819-134-4-200102200-00016. [DOI] [PubMed] [Google Scholar]
- 43.Pacak K, Goldstein DS, Doppman JL, Shulkin BL, Udelsman R, Eisenhofer G. A “pheo” lurks: novel approaches for locating occult pheochromocytoma. J Clin Endocrinol Metab. 2001;86:3641–3646. doi: 10.1210/jcem.86.8.7714. [DOI] [PubMed] [Google Scholar]
- 44.Brink I, Hoegerle S, Klisch J, Bley TA. Imaging of pheochromocytoma and paraganglioma. Fam Cancer. 2005;4:61–68. doi: 10.1007/s10689-004-2155-y. [DOI] [PubMed] [Google Scholar]
- 45.Fujita A, Hyodoh H, Kawamura Y, Kanegae K, Furuse M, Kanazawa K. Use of fusion images of I-131 metaiodobenzylguanidine, SPECT and magnetic resonance studies to identify a malignant pheochromocytoma. Clin Nucl Med. 2000;25:440–442. doi: 10.1097/00003072-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 46.Lumachi F, Tregnaghi A, Zucchetta P, et al. Sensitivity and positive predictive value of CT, MRI and 123I-MIBG scintigraphy in localizing pheochromocytomas: a prospective study. Nucl Med Commun. 2006 Jul;27(7):583–587. doi: 10.1097/00006231-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 47.Cecchin D, Lumachi F, Marzola MC, et al. A meta-iodobenzylguanidine scintigraphic scoring system increases accuracy in the diagnostic management of pheochromocytoma. Endocr Relat Cancer. 2006 Jun;13(2):525–533. doi: 10.1677/erc.1.01066. [DOI] [PubMed] [Google Scholar]
- 48.vanderLely AJ, deHerder WW, Krenning EP, Kwekkeboom DJ. Octreoscan radioreceptor imaging. Endocrine. 2003;20:307–311. doi: 10.1385/ENDO:20:3:307. [DOI] [PubMed] [Google Scholar]
- 49.Breeman WA, De Jong M, Kwekkeboom DJ, et al. Somatostatin receptor-mediated imaging and therapy: basic science, current knowledge, limitations and future perspectives. Eur J Nucl Med. 2001;28:1412–1429. doi: 10.1007/s002590100502. [DOI] [PubMed] [Google Scholar]
- 50.Timmers HJ, Carrasquillo JA, Whatley M, et al. Usefulness of standardized uptake values for distinguishing adrenal glands with pheochromocytoma from normal adrenal glands by use of 6-18F-fluorodopamine PET. J Nucl Med. 2007;48:1940–1944. doi: 10.2967/jnumed.107.043281. [DOI] [PubMed] [Google Scholar]


