Abstract
Objective
To assess the stability of visual acuity improvement during the first year after cessation of amblyopia treatment other than spectacles in 7 to 12 year olds
Methods
At the completion of a multi-center randomized trial during which amblyopia treated with both patching and atropine improved by at least 2 lines, 80 patients 7 to 12 years old were followed off treatment (other than spectacles) for one year.
Main Outcome Measure
Ten or more letters (2 or more lines) worsening of visual acuity (measured using the electronic ETDRS method) during the year following treatment discontinuation
Results
During the year following cessation of treatment, the cumulative probability of worsening acuity (2 or more lines) was 7% (95% confidence interval 3% to 17%); 82% of patients maintained an increase in acuity of 10 or more letters compared with acuity prior to starting treatment.
Conclusion
Visual acuity improvement occurring during amblyopia treatment is sustained in most 7 to 12 year olds for at least one year after discontinuing treatment other than spectacles.
Application to Clinical Practice
The data support the treatment of 7 to 12 year olds with amblyopia by demonstrating that acuity improvement can be maintained after treatment is discontinued.
Introduction
Although amblyopia can be improved with a variety of therapies including patching2–4 and topical atropine,2, 5 there are few prospective studies on the course of visual acuity after such treatment has been discontinued. The literature consists of retrospective studies with small sample sizes, variable lengths of follow-up, and/or heterogeneous patient populations,6–9 and a prospective study of younger children.10 These studies have reported widely-varying estimates of regression risk following treatment discontinuation of 6%,6 9%,11 24%,1027%,9 33%,12 60%8 and 67%.7
We conducted a randomized trial of 507 patients age 7 to 17 years old, 67% of whom had moderate amblyopia (20/40 to 20/80) and 33% of whom had severe amblyopia (20/100 to 20/400). We had previously reported that in the 404 7 to 12 year olds, treatment with spectacles plus patching and atropine produced greater improvement than spectacle correction alone (53% versus 25% improved 2 or more lines, P< 0.001). Among the 103 patients aged 13 to 17 year old we had reported that, overall, treatment with spectacles plus patching was no better than spectacles alone (25% versus 23% improved 2 or more lines, P=0.47), although a subgroup analysis suggested a possible treatment effect in patients whose amblyopia had not been previously treated (47% vs. 20% improved 2 or more lines).1 Most patients who improved on treatment in both age groups were left with a residual visual acuity deficit. Patients whose visual acuity improved 2 or more lines during treatment with spectacles/patching/atropine continued treatment until acuity stopped improving. At that time, all treatment except for spectacles was discontinued and patients were followed for one year to determine whether visual acuity improvement was sustained. Herein, we report results from the year following treatment discontinuation. The current analysis has been limited to patients 7 to 12 years at treatment initiation because a treatment effect had been seen in 13 to 17 year olds only when analyzed using secondary outcome measures (e.g. maximum acuity improvement) or in some subgroups (e.g. previously untreated patients), and because only a very small number of patients in the 13 to 17 year old group continued follow up after treatment discontinuation.
Methods
The study, supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health, was conducted by the Pediatric Eye Disease Investigator Group at 49 clinical sites. The protocol and informed consent forms were approved by institutional review boards. The parent or guardian of each study patient gave written informed consent and each patient gave assent to participate. The details and results of the randomized trial have been published in a separate manuscript1 and are only partially described herein.
The major eligibility criteria for the randomized trial included age 7 to 17 years (as noted earlier, only the 7 to 12 year old group is included in this analysis), amblyopia due to strabismus and/or anisometropia, no amblyopia treatment other than spectacles in the prior month and no more than one month of amblyopia treatment in the prior 6 months, best-corrected amblyopic eye visual acuity between 20/40 and 20/400 inclusive and best-corrected sound eye acuity of 20/25 or better, and no ocular cause for reduced acuity.
Patients were randomly assigned to a control group that received optical correction only (if needed) or to a treatment group that received optical correction (if needed) plus additional treatment consisting of patching and atropine in patients 7 to 12 years old and patching alone in 13 to 17 year olds. Patching treatment consisted of 2–6 hours of daily patching of the sound eye with one hour of near visual activities to be performed while patching; atropine treatment consisted of daily atropine in the sound eye. Treatment was continued until there was no further improvement at two consecutive six-week interval follow-up visits. At the time of patching/atropine treatment discontinuation, patients in the treatment group whose amblyopic eye had improved 10 or more letters entered a one-year observation phase after discontinuing all treatment except for spectacles.
During the observation phase, follow-up visits were performed at three months, six months, and one year. At each visit, distance visual acuity was measured in each eye without cycloplegia and with appropriate refractive correction using the electronic ETDRS testing protocol.13 If amblyopic eye acuity had decreased 10 or more letters from the time of treatment discontinuation, the testing was repeated. If a refraction had not been performed within the prior six months, it was completed before retesting acuity.
During the one-year observation phase, no treatment was to be prescribed unless amblyopic eye acuity had worsened 10 or more letters (as described above), in which case restarting treatment was at investigator discretion. One patient restarted treatment at the 13-week visit in the absence of a documented acuity loss and did not return for subsequent follow up visits; for the analysis this patient was not considered to have worsened 10 or more letters and was censored at 13-weeks.
Statistical Methods
The primary study outcome was a worsening of amblyopic eye visual acuity by 10 or more letters. We chose a 10 letter (two line) decrease as the criterion for worsening of visual acuity based on data which demonstrated that a 10 or more letter change is unlikely to result from measurement variability.13 The one-year cumulative probability of visual acuity worsening of 10 or more letters and a 95% confidence interval (CI) were computed using the Kaplan-Meier product-limit method.
Frequency distributions and descriptive statistics for assessing change in acuity over time were calculated for the patients who completed the study, defined as completing one year of follow up or experiencing a decrease of acuity of 10 or more letters. For any patient who experienced a 10 or more letter worsening at a visit prior to one year, that acuity (prior to the reinstitution of treatment) was carried forward as the one-year acuity.
Data from the patients who completed the study were used to estimate the probability of 10 or more letter worsening among those who did not complete the study. Based on the amount of acuity change from treatment cessation which was present at the last completed visit for each patient not completing the study, a corresponding risk was assigned equal to the risk among patients completing the study who had a similar amount of change in acuity at the same timepoint. For patients with no follow-up visits, a risk was assigned equal to the risk among patients who had completed the study and who had similar baseline visual acuity.
Results
Baseline Characteristics
At the time of entry into the randomized trial, the mean age of the 80 patients was 9.3±1.5 years (range 7.1 to 12.9 years), mean visual acuity was 0.58±0.24 logMAR (approximately 20/80), and 57 (71%) of patients had acuity between 20/40 to 20/80 inclusive. Acuity improvement from the start of treatment to the time of treatment discontinuation averaged 17±8 letters (3.4±1.6 lines), ranging from 10 to 58 letters (2.0 to 11.6 lines). At the time of treatment discontinuation, 36 (45%) patients had acuity in the amblyopic eye of 20/25 or better, 27 (34%) 20/32 to 20/40, 11 (14%) 20/50 to 20/80, and 6 (8%) 20/100 or worse. Additional characteristics of the cohort are provided in Table 1.
Table 1.
Baseline Demographic and Clinical Characteristics (N=80)*
| Age at Entry into Randomized Trial N (%) | |
| 7–9 years | 56 (70) |
| 10–12 years | 24 (30) |
| Mean (SD), in years | 9.3 (1.5) |
| Gender: Female N (%) | 34 (43) |
| Race / Ethnicity N (%) | |
| White | 57 (71) |
| African-American | 8 (10) |
| Hispanic or Latino | 14 (18) |
| Asian | 1 (1) |
| Cause of Amblyopia† N (%) | |
| Strabismus | 15 (19) |
| Anisometropia | 38 (48) |
| Strabismus and anisometropia | 26 (33) |
| Spectacle Correction Prior to Entry into Randomized Trial‡ N (%) | |
| No correction worn / none needed | 3 (4) |
| Correction worn optimal | 7 (9) |
| Correction worn required change | 27 (34) |
| No correction / correction needed | 41 (51) |
| Amblyopia Treatment Prior to Entry into Randomized Trial | |
| None | 51 (64) |
| Patching | 24 (30) |
| Atropine | 1 (1) |
| Patching and atropine | 4 (5) |
| Visual Acuity at Entry into Randomized Trial N (%) | |
| 20/40 to 20/80 (>=53 letters) | 57 (71) |
| 20/100 to 20/160 (38–52 letters) | 14 (18) |
| 20/200 to 20/400 (<=37 letters) | 9 (11) |
| Mean (SD) logMAR | 0.58 (0.24) |
| Length of Treatment in Randomized Trial Prior to Discontinuation N (%) | |
| Less than 3 months | 8 (10) |
| 3 months – <6 months | 25 (31) |
| 6 months – <9 months | 36 (45) |
| 9 months or more | 11 (14) |
| Mean (SD), in months | 6.4 (2.5) |
| Acuity Improvement During Randomized Trial N (%) | |
| 10–14 letters | 31 (39) |
| 15–19 letters | 30 (38) |
| >=20 letters | 19 (24) |
| Mean (SD) letters | 17.5 (8.1) |
| Visual Acuity at Treatment Discontinuation N (%) | |
| 20/25 or better (>=78 letters) | 36 (45) |
| 20/32 to 20/40 (68–77 letters) | 27 (34) |
| 20/50 to 20/80 (53–67 letters) | 11 (14) |
| 20/100 or worse (<=52 letters) | 6 (8) |
| Mean (SD) logMAR | 0.23 (0.23) |
Values are expressed as number (percentage) unless otherwise indicated.
One patient had indeterminate cause of amblyopia.
Spectacle correction history data are missing for two patients.
Visit Completion
Sixty-seven (84%) patients completed the study, defined as completing one year of follow up or experiencing a decrease of acuity of 10 or more letters during follow up. The 3-month visit was completed by 69 (86%) patients and the 6-month visit by 71 (89%).
Change in Amblyopic Eye Visual Acuity During Follow Up
For the 67 patients completing the study, the mean change in amblyopic eye visual acuity from treatment discontinuation to 3 months was 0.0±4.1 letters, to 6 months was −1.0±3.9 letters, and to one year was −1.3±5.1 letters. One-year visual acuity was within 4 letters (less than one line) of the acuity at the time of treatment discontinuation for 46 (69%) patients (Table 2, Figure 1). Two patients (3%) had an increase in acuity of 10 letters or more and 6 (9%) had an increase of 5 to 9 letters, while 5 (7%) patients had an acuity decrease of 10 or more letters and 8 (12%) had a decrease of 5 to 9 letters (Table 3). The cumulative probability of a 10 or more letter worsening during the one-year follow-up period was 7% (95% confidence interval 3% to 17%) overall, 4% in the 47 patients 7 to 9 years old and 15% in the 20 patients 10 to 12 years old at the time of entry into the randomized trial (Table 2).
Table 2.
Change in Visual Acuity On Treatment and Following Treatment Discontinuation According to Age (N=67)*
| Age at Randomization | |||
|---|---|---|---|
| Total N=67 | 7–9 Years N=47 | 10–12 Years N=20 | |
| Acuity Improvement on Treatment | |||
| Mean (SD) letters | 17.4 (7.8) | 18.3 (8.9) | 15.2 (3.7) |
| Change In Acuity From Treatment Discontinuation to One-Year | |||
| Mean (SD) letters | −1.3 (5.1) | −0.7 (4.9) | −2.7 (5.5) |
| Increased >=10 Letters | 2 (3) | 1 (2) | 1 (5) |
| Increased 5–9 Letters | 6 (9) | 5 (11) | 1 (5) |
| Within 0–4 Letters | 46 (69) | 33 (70) | 13 (65) |
| Decreased 5–9 Letters | 8 (12) | 6 (13) | 2 (10) |
| Decreased >=10 Letters | 5 (7) | 2 (4) | 3 (15) |
| Cumulative probability of decreasing >=10 letters†, percent | 7% | 4% | 15% |
Includes all patients who completed the observation phase, defined as completing one year of follow up or experiencing a decrease of acuity of 10 or more letters during followup. For the 1 patient who experienced an acuity decrease of 10 or more letters prior to the one-year visit, the one-year acuity is the acuity at the time of the decrease.
Cumulative probability obtained from Kaplan-Meier product-limit method.
Figure 1. Visual Acuity At Treatment Discontinuation Versus One-Year Post-Treatment Discontinuation Visual Acuity (N=67).
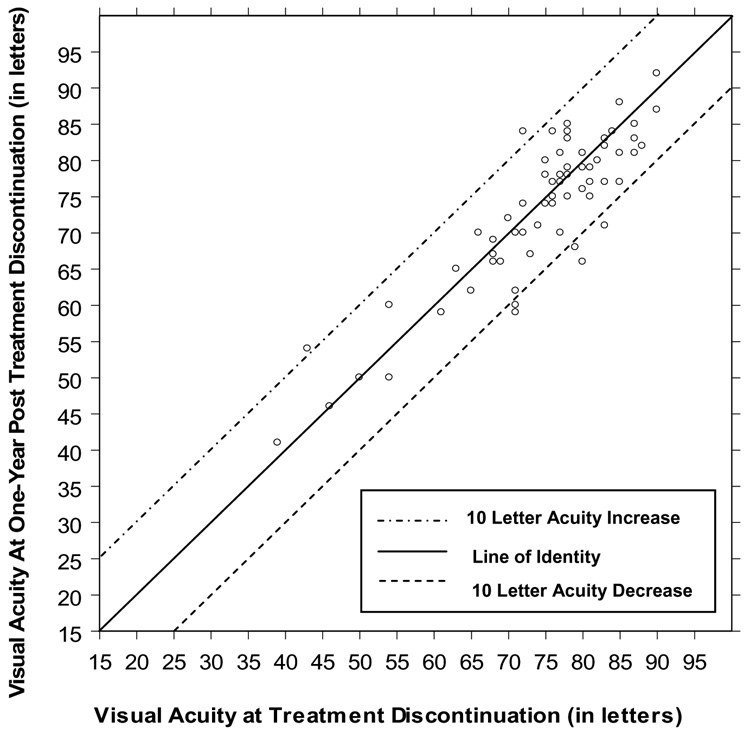
Plot includes all patients who completed the observation phase, defined as completing one year of follow up or experiencing a decrease of acuity of 10 or more letters during follow up. For the 1 patient who experienced an acuity decrease of 10 or more letters prior to the one-year visit, the one-year acuity is the acuity at the time of the decrease. A letter score of 85 corresponds to 20/20, with 5 letters representing one line. Lower letter scores indicate worse visual acuity.
Among the 61 patients who had improved 10 to 19 letters on treatment, 4 patients (cumulative probability = 8%) experienced a decrease of 10 or more letters off treatment: an 7.8 year old who dropped from 20/25 to 20/50 at 6 months, an 7.8 year old who dropped from 20/25 to 20/40 at one year, an 11.2 year old who dropped from 20/20 to 20/40 at one year, and an 11.3 year old who dropped from 20/40 to 20/63 at one year. Among the 19 patients who had improved 20 letters or more on treatment, one patient (cumulative probability = 6%) experienced a decrease of 10 or more letters off treatment, a 12.9 year old whose acuity dropped from 20/40 to 20/63 at the one-year visit. A supplemental table shows the baseline characteristics of the 5 patients who experienced a 10 or more letter worsening and the course of their visual acuity after stopping treatment.
In most patients (82%) one-year amblyopic eye visual acuity remained 10 or more letters better than the pretreatment acuity, and no patient had a one-year visual acuity that was worse than the pretreatment acuity (Figure 2). Mean one-year visual acuity was 16 ± 9 letters (3.2±1.8 lines) better than the pre-treatment acuity, with 3 patients (4%) having a one-year acuity 30 or more letters better than the pretreatment acuity, 16 (24%), 20 to 29 letters better, 36 (54%) 10 to 19 letters better, 9 (13%) 5 to 9 letters better, and 3 (4%) 0 to 4 letters better. Comparing the one-year acuity with the improvement in acuity gained on treatment, the percentage of acuity improvement retained for each patient ranged from 13% to 100% with a median of 91%. Twenty-nine patients (43%) maintained 100% of their acuity improvement.
Figure 2. Visual Acuity At Pre-treatment Versus One-Year Post-Treatment Discontinuation Visual Acuity (N=67).
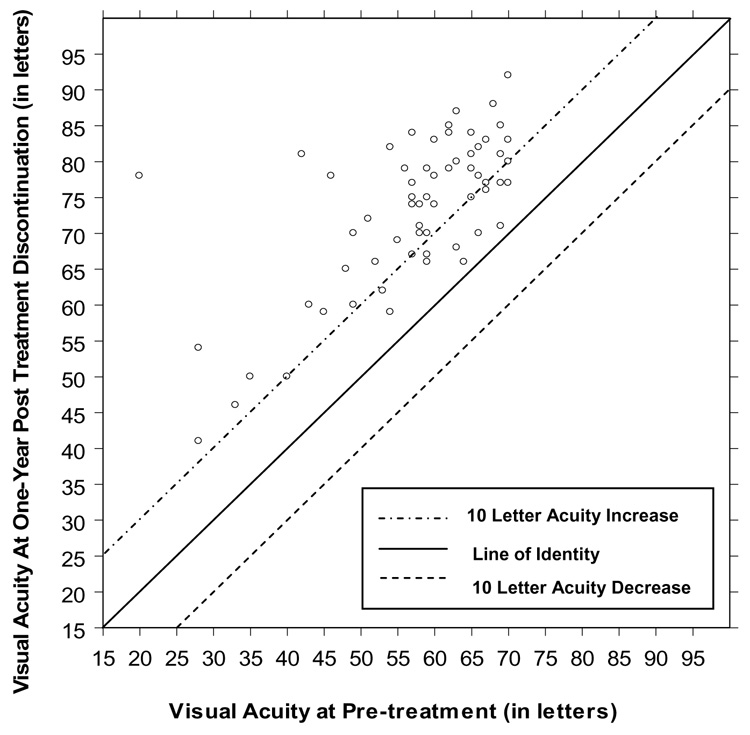
Plot includes all patients who completed the observation phase, defined as completing one year of follow up or experiencing a decrease of acuity of 10 or more letters during follow up. For the 1 patient who experienced an acuity decrease of 10 or more letters prior to the one-year visit, the one-year acuity is the acuity at the time of the decrease. A letter score of 85 corresponds to 20/20, with 5 letters representing one line. Lower letter scores indicate worse visual acuity.
Characteristics of Patients Not Completing the Study
Of the 13 patients not completing the study, 5 had no protocol follow-up visits, 3 dropped out after the 3-month visit and 5 after the 6-month visit. The mean age of patients not completing the study was 9.6 years compared with 9.2 years for patients who completed the study; 69% of the patients not completing the study were female compared with 37% of patients who completed the study. Mean amblyopic eye acuity at the time of treatment discontinuation on average was 8 letters (1.6 lines) worse in the patients who did not complete the study than in those who did (P=0.03).
The 3 patients who dropped out following the 3-month visit had a change in acuity from the time of treatment discontinuation to the 3-month visit of −5, −4, and −2 letters, and the 5 patients who dropped out following the 6-month visit had a change in acuity from the time of treatment discontinuation to the 6-month visit of −9, −5, −5, −4, and +3 letters. Utilizing the data of the patients who completed the study to impute the one-year risk of worsening 10 or more letters for the patients who did not provided an estimate that 7% of the 13 noncompleters would have had a 10 or more letter worsening of acuity if follow up had been complete.
Discussion
In this prospective study of 80 amblyopic children between 7 and 12 years of age, visual acuity improvement of 10 or more letters (≥2 lines) that occurred with patching/atropine treatment was generally sustained during one year of observation after treatment other than refractive correction was discontinued. The one-year probability of a worsening of acuity of 10 or more letters (2 or more lines) was 7%. This low risk cannot be compared with the risk reported in previous studies because those studies either involved children of different ages or were retrospective studies with heterogeneous patient populations, small sample sizes, high drop-out rates, variable lengths of follow up, and either unspecified or varying criteria for successful treatment and for significant loss of acuity off treatment.6–10 11, 12
One possible explanation for the notably low incidence of acuity worsening after treatment discontinuation relates to the role of spectacle correction in our study. Concurrent with the initiation of patching/atropine treatments at the time of entry into the randomized trial, 51% of the patients were prescribed new spectacles and an additional 34% required a change in spectacles. We assume that in many of these patients, a portion of the improvement that occurred on treatment was due to spectacle wear and not solely due to the effect of atropine/patching. In the randomized trial, control group patients aged 7–12 years received spectacle correction alone and improved an average of 7 letters.1 At the time of discontinuation of patching/atropine, spectacle wear was continued. Because improvement as a result of spectacle wear would not be expected to be lost when spectacle wear was continued, some patients might not have been capable of losing 10 or more letters when patching/atropine was discontinued. If this were an explanation for the low incidence of worsening, we might expect to have found that worsening 10 or more letters occurred in the study principally in patients who had improved substantially more than 10 letters on treatment, but this was not found to be the case as the risk of worsening 10 or more letters was 8% among patients who improved 10 to 19 letters on treatment and 6% among those who improved 20 or more letters.
Although we had planned to assess whether the risk of acuity worsening off treatment was related to factors such as age at treatment initiation, pre-treatment acuity and amount of improvement on treatment, the small number of patients who experienced a 10 or more letter worsening (only 5 patients out of 80) precluded such analyses. Given this small number of observed events, statistical power would be low for detecting associations if they truly did exist.
The study completion percentage of 84% is somewhat lower than we had hoped but is not unexpected given that we anticipated more retention issues with the older population (7–12 years) in the current study than with the younger populations (under 7 years) in our other amblyopia studies. However, utilizing the follow-up visual acuity data of the patients who completed the study to estimate the one-year acuity of those who did not complete the study suggested that the losses to follow up were not appreciably biasing the results.
In conclusion, we have determined the risk of a significant acuity worsening (10 letters or more) is low after cessation of amblyopia treatment other than spectacles children 7 to 12 years old. Our data are encouraging and demonstrate that when older children continue to wear their refractive correction after cessation of patching/atropine treatment, visual acuity improvement is generally sustained. These data are important because the results address one of the major arguments against the treatment of amblyopia in older children. Some clinicians who do not treat older children with amblyopia have suggested that even if treatment is effective in this age group, regression is likely to be common, thereby nullifying the treatment’s value. The data from this study combined with our previously published results1 support the treatment of amblyopia in children 7 to 12 years old.
Supplementary Material
Acknowledgments
Writing Committee: Lead authors: Richard W. Hertle, M.D.; Mitchell M. Scheiman, O.D.; Roy W. Beck, M.D., Ph.D.; Danielle L. Chandler, M.S.P.H.; Additional writing committee members (alphabetical): Darron A. Bacal, M.D.; Eileen Birch, Ph.D.; Raymond H. Chu, O.D.; Jonathan M. Holmes B.M., B.Ch.; Deborah L. Klimek, M.D.; Katherine A. Lee M.D.; Ph.D., Michael X. Repka, M.D.; David R. Weakley Jr. M.D.
A complete listing of the Pediatric Eye Disease Investigator Group members who participated in this study has been published.1
Supported through a cooperative agreement from the National Eye Institute EY11751
References
- 1.Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–447. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 2.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 3.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 4.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–2087. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076–2085. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 6.Kushner BJ. Ophthalmology Annual. New York: Raven Press; 1988. Functional amblyopia: a purely practical pediatric patching protocol; pp. 173–198. [Google Scholar]
- 7.Rutstein RP, Fuhr PS. Efficacy and stability of amblyopia therapy. Optom & Vis Sci. 1992;69(10):747–754. doi: 10.1097/00006324-199210000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Levartovsky S, Gottesman N, Shimshoni M, Oliver M. Factors affecting long-term results of successfully treated amblyopia: age at beginning of treatment and age at cessation of monitoring. J Pediatr Ophthalmol Strabismus. 1992;29:219–223. doi: 10.3928/0191-3913-19920701-08. [DOI] [PubMed] [Google Scholar]
- 9.Flynn JT, Woodruff G, Thompson JR, et al. The therapy of amblyopia: an analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc. 1999;97:373–390. [PMC free article] [PubMed] [Google Scholar]
- 10.Pediatric Eye Disease Investigator Group. Risk of amblyopia recurrence after cessation of treatment. J AAPOS. 2004;8:420–428. doi: 10.1016/S1091853104001612. [DOI] [PubMed] [Google Scholar]
- 11.Mohan K, Saroha V, Sharma A. Successful occlusion therapy for amblyopia in 11- to 15-year-old children. J Pediatr Ophthalmol Strabismus. 2004;41(2):89–95. doi: 10.3928/0191-3913-20040301-08. [DOI] [PubMed] [Google Scholar]
- 12.Leiba H, Shimshoni M, Oliver M, Gottesmann N, Levartovsky S. Long-term follow-up of occlusion therapy in amblyopia. Ophthalmology. 2001;108(9):1552–1555. doi: 10.1016/s0161-6420(01)00697-2. [DOI] [PubMed] [Google Scholar]
- 13.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the Electronic Early Treatment Diabetic Retinopathy Study testing protocol in children 7 to <13 years old. Am J Ophthalmol. 2003;136(4):655–661. doi: 10.1016/s0002-9394(03)00388-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


