Abstract
This is a clinical radiographic study, spanning over three decades, analyzing the three-dimensional (3-D) changes in spine geometry after corrective surgery for adolescent idiopathic scoliosis (AIS) using four generations of instrumentation systems. The objective of this study was to retrospectively evaluate the evolution of spinal instrumentation over time by measuring the 3-D changes of spinal shape before and after surgical correction of subjects with AIS using Harrington/Harrington-Luque (H/HL) instrumentation, original and recent generations of Cotrel-Dubousset Instrumentation (CDI) with rod rotation maneuvers, as well as third generation systems using thoracic pedicle screws and direct vertebral derotation (DVD) manoeuver in order to determine if the claims for improved 3-D correction from generation to next generation could be substantiated. The 3-D shape of the thoracic and lumbar spine was recorded from a pair of standing radiographs using a novel 3-D reconstruction technique from uncalibrated radiographs in 128 adolescents with AIS undergoing surgery by a posterior approach. Changes in coronal Cobb angles, kyphosis, lordosis, as well as in a series of 3-D parameters computed from the spine reconstructions before and after surgery were used to compare the four groups. Results demonstrate statistically significant differences (P = 0.05) between generations with regards to the correction of the coronal Cobb angle, and different loss of physiological lordosis. More importantly, significant differences in the 3-D correction of the spine based on the orientation of the planes of maximal curvature were observed (20/−6% H/HL vs. 39/39% CDI vs. 42/18% DVD for the thoracic/lumbar regions, respectively), confirming that recent CDI and third generation instrumentations coupled with DVD can bring the deformity significantly closer to the sagittal plane. An increased correction in apical vertebra axial rotation was observed with the DVD manoeuver (74%), while fewer notable differences were found between DVD and recent CDI systems in terms of 3-D correction. This is the first quantitative study to clearly demonstrate that the rod derotation and DVD maneuvers can significantly improve 3-D correction of scoliotic deformities, thereby supporting the transition towards these more elaborate and costly instrumentation technologies in terms of 3-D assessment.
Keywords: Adolescent idiopathic scoliosis, Spinal instrumentation, Three-dimensional reconstruction, 3-D correction, Retrospective analysis
Introduction
Significant changes have occurred over the past three decades in the field of spinal instrumentation for the correction of adolescent idiopathic scoliosis (AIS). In early years, spinal surgical instrumentations were designed primarily to apply distraction forces to the spine. Such was the case with the Harrington instrumentation which was the standard for surgical correction of AIS for almost 25 years since its introduction in 1962. The Harrington-Luque instrumentation included segmental sublaminar wiring to increase construct rigidity and to counteract its tendency to decrease the sagittal profile, effectively correct the coronal Cobb angle [5, 6, 25], improve balance and decrease the number of fusion levels [19]. However, as interest towards three-dimensional (3-D) correction grew in the surgical field, the Harrington technique was shown to achieve inadequate rib cage correction [14], and this did not correlate with vertebral derotation. Aaro [1] used Computerized Tomography (CT) to demonstrate that the Harrington technique did not produce significant derotation of the apical vertebra and thus could not achieve a 3-D correction of the spine.
In the mid 1980s, the introduction of the Cotrel-Dubousset instrumentation (CDI) [11] provided the first attempt to achieve true 3-D correction of the spine with the concept of the rod rotation manoeuver, by offering a complex combination of forces to correct the spinal deformity and provide increased rigidity of the corrected spine. The technique was intended to “derotate” the spine and is performed in two stages: first globally, and then locally. Globally the spine is rotated from its predominant plane of curvature in the coronal plane into the sagittal plane, thus producing normal kyphosis and lordosis. Therefore, the plane of maximum curvature of the spine is rotated in the same direction as the rod rotation. But scoliosis also involves transverse plane rotation of the vertebrae in the opposite direction for a curve in a kyphotic thoracic region [30]. In order to derotate the vertebrae (vertebral derotation), moments in the opposite sense should also be applied to the vertebrae.
The 3-D effect of CDI has been extensively documented in previous studies and has demonstrated satisfactory 3-D correction of the scoliotic curve [9, 21, 23], but various generations were introduced in the past decade in response to reported problems thought to be linked with the derotation maneuvers of the technique. These new CD instrumentation techniques (e.g., CD Legacy, CD Horizon) were also designed for more versatile and user-friendly spinal implants, as well as aiming to achieve better 3-D correction by substantially increasing the number of pedicle screws used during the procedure. The pedicle screw, which is used as an adjunct to spinal fusion surgery, provides a better means of gripping a spinal segment. Pedicle screws are thought to enhance patient recovery because they provide more rigid fixation for the spine and early mobilization for the patient, with improved fusion rates. However, the ability of achieving adequate rotational correction with pedicle screws remained unclear. A new correction technique, known as direct vertebral rotation (DVR), was introduced by Suk to offer a system which would apply rotational forces to the apical vertebrae in the opposite direction to the rod derotation. This technique was shown to achieve significant correction of the apical vertebral rotation, thus demonstrating that segmental pedicle screw fixation with “direct vertebral rotation” showed better rotational and coronal correction when compared to the simple rod derotation [22]. While DVR only applies a derotation manoeuver on the apical vertebra, a similar technique performs vertebral derotation maneuvers on each vertebral level in the instrumented segment and is known as direct vertebral derotation (DVD). This is the current technique used at our institution.
Clinical studies with cohorts of patients have compared the relative correction of the Harrington and Cotrel-Dubousset procedures [12, 15, 16], but these were limited to the Cobb angles in the coronal or sagittal planes. Although the effect of the Harrington instrumentation on the coronal plane shape of the spine has been well documented [6, 24, 25, 33], its effect on the 3-D geometry of the spine after surgery has never been portrayed because 3-D reconstruction techniques with calibrated devices were unavailable. Furthermore, no thorough 3-D evaluation of the evolution of spinal instrumentation throughout the decades, going back from the Harrington technique to more recent procedures such as the DVR technique using pedicle screws, has been presented in the literature. A preliminary study of a small number of cases was presented by Stokes et al. [31], but was limited to the axial view and thus did not measure the global 3-D correction of the spine since the axial rotation is measured locally similar to the standard rotation measurement computed from CT scan.
Recent clinical studies have also compared direct vertebral rotation instrumentations to previous systems based on simple rod derotation maneuvers, but were limited to evaluating coronal curves and apical rotation [13, 22, 27], therefore lacking in a true 3-D evaluation of this new technology. The standard clinical radiographs do not demonstrate the 3-D spinal shape, but a new self-calibration method recently proposed by Kadoury et al. [18], enables 3-D reconstruction from uncalibrated frontal and lateral X-rays, making it now possible to perform retrospective 3-D analysis. The basis of this new self-calibration employs identified anatomical landmarks on the patient’s spine, in order to calibrate and subsequently reconstruct the spine in 3-D without the need of a calibration apparatus. This method was clinically validated in a previous study and showed insignificant differences with previous reconstruction methods used for the 3-D assessment of scoliotic deformities [18]. This purely radiographic study used available clinical documentation of pre- and postoperative spinal shape together with these new calibration methods to show how correction in 3-D spinal shape concentrated in the thoracic and lumbar regions have evolved over time with the development of new instrumentation techniques.
The aim was to establish the relative contributions of various mechanisms such as distraction, compression, global and local derotation maneuvers based on the hypothesis that more recent instrumentation systems are more effective at gaining global 3-D correction compared to earlier techniques such as Harrington instrumentation or preliminary versions of the Cotrel-Dubousset instrumentation.
This study evaluated changes between pre- and postoperative 3-D shape of the thoracic and lumbar spine between the T1 and L5 vertebrae in four cohorts of adolescents with idiopathic scoliosis undergoing posterior surgery: Harrington or Harrington-Luque instrumentation (Group A), original Cotrel-Dubousset instrumentation (Group B) with a majority of vertebral hooks, recent CDI (Group C) with a majority of pedicle screws or direct vertebral derotation techniques (Group D). The four instrumentation generations selected for this study were determined in order to reflect the evolution of spinal instrumentation at our institutions and establish an historical documentation of the major instrumentation types proposed throughout decades.
Materials and methods
Subjects
This study concerns 128 patients who underwent posterior spinal surgery in their adolescence for idiopathic scoliosis correction between 1982 and 2008. Inclusion criteria consisted of: (1) presence of adolescent idiopathic scoliosis, (2) indication for surgical correction by a posterior approach as determined by an experienced orthopedic surgeon, (3) a thoracic or lumbar curve, and (4) 10–18 years old at time of surgery. Exclusion criteria were: (1) any other significant musculoskeletal disease, (2) non idiopathic scoliosis, (3) previous spine surgery, (4) thoracoplasty or anterior surgery done previously or in combination with the posterior approach, (5) incomplete radiological record, (6) poor X-rays quality or missing anatomical landmarks, (7) uncertainty about surgical approach/type of instrumentation used, or (8) Cobb angle of main curve greater than 80°. Four equally distributed instrumentations groups of randomly selected patients were created, with the patient size determined by the number of eligible patients with Harrington/Harrington-Luque (H/HL) instrumentation due to the limited amount of radiographic data available. The characteristics of the four groups of patients are provided in Table 1.
Table 1.
Patient characteristics for the four study groups
| Group | A | B | C | D | Probability of groupwise difference |
|---|---|---|---|---|---|
| Instrumentation | H/HL (82–87) | Original CDI (90–95) | Recent CDI (97–06) | DVD (07–08) | |
| Number of patients | 32 | 32 | 32 | 32 | |
| Average age at time of surgery (year) | 15.3 ± 2.3 | 15.0 ± 1.9 | 15.2 ± 1.7 | 15.6 ± 1.7 | NS (0.655) |
| Number of thoracic (T) curves | 31 | 30 | 31 | 31 | |
| Number of lumbar (L) curves | 18 | 23 | 19 | 22 | |
| Average Cobb angle preop (°) | |||||
| PT | 22 ± 11 | 27 ± 14 | 24 ± 11 | 29 ± 15 | NS (0.115) |
| MT | 50 ± 14 | 52 ± 15 | 50 ± 11 | 53 ± 11 | NS (0.672) |
| TL/L | 45 ± 11 | 45 ± 14 | 47 ± 13 | 44 ± 15 | NS (0.786) |
| Average flexibility of the main curve (bending test) (%) | 49 ± 20a | 45 ± 19 | 49 ± 17 | 42 ± 17 | NS (0.286) |
| Risser sign (% of mature) | 80a | 69b | 80 | 72 | NS (0.163) |
SD Significant difference, NS non-significant difference
a 11 cases missing, b 3 cases missing
There were four groups of patients: Patients in Group A (30 females, 2 males) underwent surgery with Harrington/Harrington-Luque H/HL instrumentation (14 H and 18 H/HL). Patients in Group B (29 females, 3 males) received the original Cotrel-Dubousset Instrumentation (CDI) as introduced in the late 1980s using vertebral hooks (60% or more) and rod rotation. Patients in Group C (28 females, 4 males) were treated with more subsequent generations of CDI (CD Horizon or CD Legacy) using mostly mono-axial or poly-axial pedicle screw constructs (70% or more) and rod rotation Patients in Group D (25 females, 7 males) were treated with mono-axial pedicle screw constructs only with DVD [Monarch, Expedium (Depuy Spine) or PLUS (SpineVision)]. The average age at the time of surgery was 15.3 ± 1.9 years and was similar in all groups. In all, there were 77 patients with doubles curves (King type I and King type II) and 51 with single curves (King type III, King type IV and lumbar curves), making a total of 123 thoracic and 82 lumbar curves. Differences in patients preoperative characteristics were assessed using ANOVA for continuous variables and no statistically significant differences (P < 0.05) were found for the curve’s severity in terms of Cobb angle measurement in all groups (Table 1). The flexibility of the curves or the percentage of curve reduction measured from supine bending tests (normalized difference between main coronal Cobb angle in standing and supine lateral bending positions) was not statistically different between groups. A χ2 test was performed on the Risser sign and showed no statistical difference between groups.
3-D reconstruction of the spine geometry
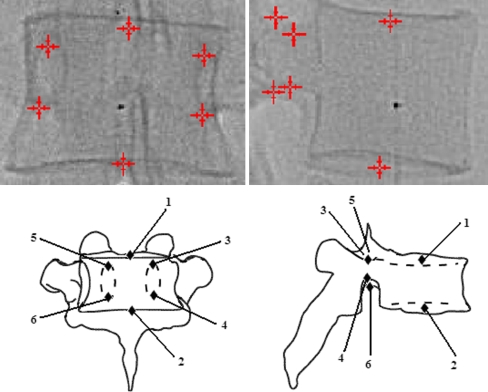
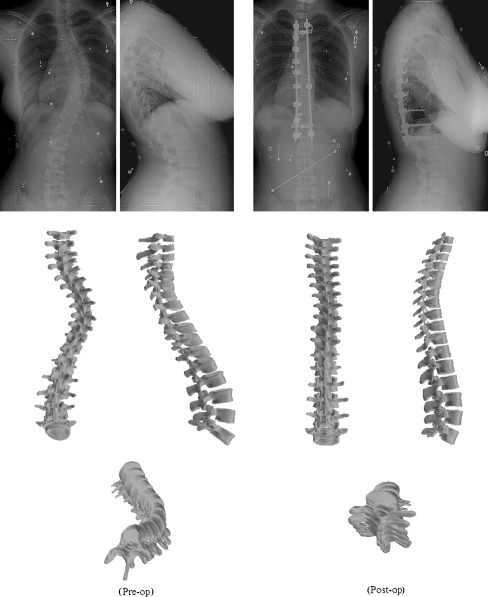
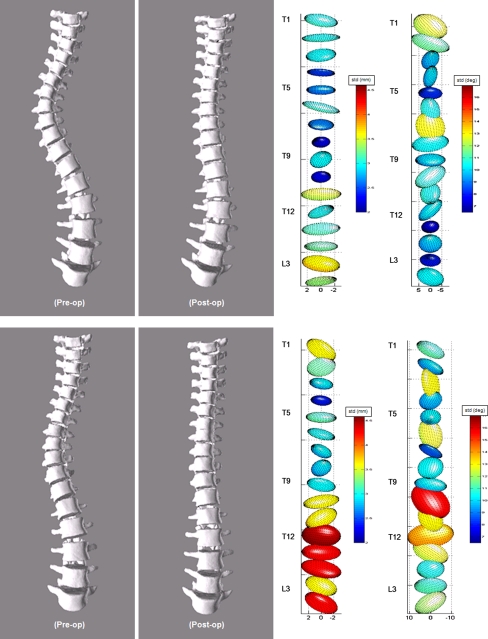
For each patient, 3-D reconstructions of the spinal shape were obtained before admission to the hospital (Stage I) and after surgery (Stage II; 1.3 ± 0.7 months on average after surgery) with pairs of radiographs (posterior and lateral) taken at both stages. A biplanar self-calibration radiographic technique based on identified anatomical landmarks was used [8, 18], thus allowing to retrospectively perform 3-D reconstructions of the spine. This method requires the identification and marking of 6 anatomical landmarks (tips of both pedicles and the superior and inferior center of each plate) from T1 to L5 on the biplane standing radiographs of the spine (Fig. 1) to self-calibrate the radiographic setup by optimization. The 3-D coordinates of each landmark are computed using a stereo-triangulation method, and can be visualized in any desired projection (Fig. 2), while anthropometric data can be added to the reconstructions to improve visual representation (Figs. 3, 4). The spine geometry was limited between T1 and L5 since lower limbs such as the pelvis or femoral heads were not routinely captured for past instrumentation systems. The accuracy of 3-D reconstruction with biplanar radiographs has been measured and reported of being 1.6 mm when compared to a CT-like “gold-standard” models [4, 10], which is quite acceptable for clinical evaluation of spinal deformities.
Fig. 1.
Identified anatomical landmarks (pedicle tips and endplate centers) used by the self-calibration algorithm
Fig. 2.
Example of a 3-D reconstruction of the spine with corresponding radiographs for an adolescent with scoliosis before surgery (Pre-op) and after surgery using Harrington/Harrington-Luque instrumentation (Post-op). The model can be viewed in the coronal plane, sagittal plane, apical view (along Z axis), or planes of maximum curvature
Fig. 3.
Example of a 3-D parameteric representation of the spine with corresponding radiographs for an adolescent with scoliosis before surgery (Pre-op) and after surgery using original Cotrel-Dubousset instrumentation (Post-op)
Fig. 4.
Example of a 3-D parameteric representation of the spine with corresponding radiographs for an adolescent with scoliosis before surgery (Pre-op) and after surgery using recent Cotrel-Dubousset instrumentation (Post-op)
3-D geometrical measurements
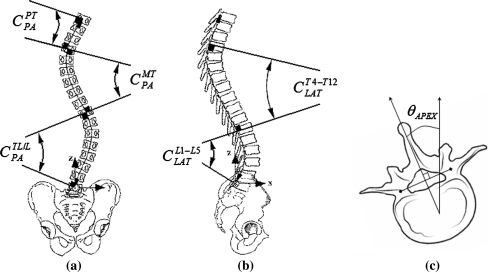
The following 3-D geometric indices were computed from the 3-D reconstructed spine models:
Computed Cobb angle of the proximal thoracic (PT), main thoracic (MT) and thoracolumbar/lumbar (TL/L) curves in the coronal plane, which are similar to the standard radiographic Cobb angles, but computed from the coronal view of the 3-D model by calculating the angle between the intersection of two lines perpendicular to the spinal curve at its inflexion points and passing through the pedicle centroids (Fig. 5a). These measurements average 11% greater than the conventional Cobb angle measured from endplate inclinations [17, 32].
Computed kyphosis constrained to the T4–T12 segment and calculated in a similar fashion to the computed 3-D Cobb angle described above. The lordosis angle was computed between L1 and L5 (Fig. 5b). Both angles were reported in signed value (positive value = kyphosis; negative value = lordosis).
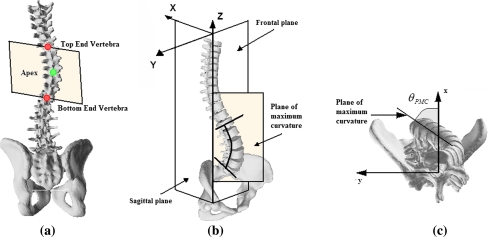
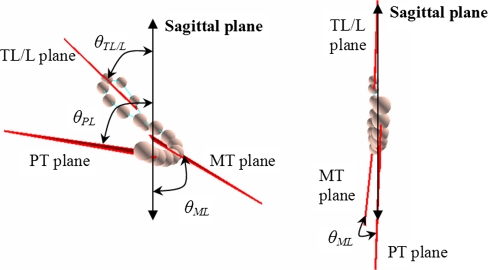
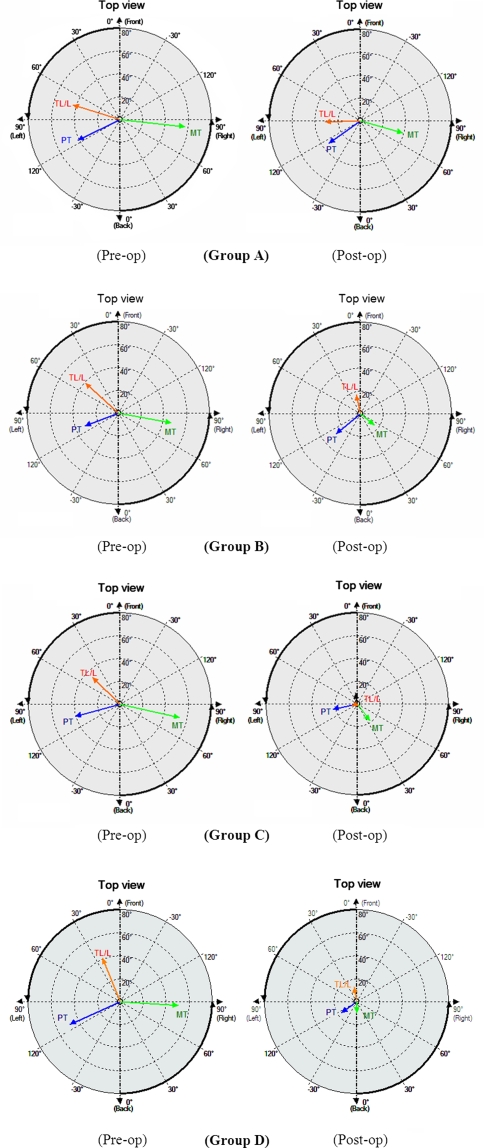
Orientation of the plane of maximum curvature (PMC) of in the proximal thoracic (PT), main thoracic (MT) and thoracolumbar/lumbar (TL/L) regions, measured by the angle between the plane of maximum curvature and the sagittal plane as presented in [3]. To calculate this measure for a given curve, a 3-D plane passing through both end vertebrae and the apex was identified on the coronal plane (Fig. 6a). The plane is then rotated around the vertical axis of the spine, and at each 1° increment, the Cobb angles are projected on the plane (Fig. 6b). The orientation of the plane of maximum curvature is the plane rotation where the projected Cobb angle is maximum (Fig. 6c). The orientation of planes is reported in absolute value relative to the sagittal plane (0°). Figure 7 illustrates two cases with one exhibiting severe scoliosis deformity and another with no deformity showing the planes of maximum deformity close to the sagittal plane. Because the PMC does not fit exactly to the spine, this measure can be considered as a simplification of the 3-D deformity, however, it was shown to effectively represent and assess the true 3-D nature of the deformity of AIS in previous studies [9, 28, 34].
Computed Cobb angle of the PT, MT and TL/L curves in the plane of maximum curvature, obtained by the same method described above which rotates the spine around the vertical axis and measures the computed Cobb angle on the two-dimensional projection of the pedicle centroid line of that plane until the highest computed Cobb angle is obtained.
Axial orientation of the apical vertebra, measured by the Stokes method [29] (Fig. 5c).
Fig. 5.
Graphical representation of 3-D clinical indices used for the evaluation of spinal deformities. a Computer Cobb angle in the coronal plane, b Kyphosis and lordosis in the sagittal plane, c axial rotation of the apical vertebra
Fig. 6.
a Determining the contrained plane passing through the end vertebrae. b Projection of the maximal curvature plane in 3-D view. c Plane of maximal curvature in the top view
Fig. 7.
Top view of the spine (view along spinal axis) illustrating orientation of planes of maximum deformity (θ) for a case exhibiting severe scoliosis (left) and a case exhibiting no scoliosis (right). In the normal case, the orientation of the planes of maximum curvature is close to 0° from the sagittal plane
Data analysis
In each group, differences between Stages I and II of each geometric parameter described above was compared using paired two-sided Student’s t tests, P = 0.05. The correction (difference between Stages I and II) of these same geometric parameters was also compared between groups using ANOVA followed by Tukey multiple comparison procedure, P′ = 0.05 (Table 5). In order to evaluate the statistical power, a 20% or more difference between the groups was set as the minimum difference to be observed in order to consider the changes clinically significant and relevant. This was based on the limit considered by Delorme et al. [9], who justified this level by the order of the accuracy of the 3-D reconstructions and variability of the geometric parameters.
Table 5.
Means, standard deviations, and levels of significance (P) for geometric parameters in Group D (Direct vertebral derotation instrumentation) at stages I and II (before and after surgery)
| Parameter | Stage I (pre) | Stage II (post) | P (I vs. II) (paired t-test) |
|---|---|---|---|
| Coronal Cobb angle (°) | |||
| PT | 29 ± 15 | 11 ± 9 | SD (<0.001) |
| MT | 53 ± 11 | 16 ± 7 | SD (<0.001) |
| TL/L | 44 ± 15 | 21 ± 11 | SD (<0.001) |
| Kyphosis (°) | 30 ± 15 | 30 ± 13 | NS (0.808) |
| Lordosis (°) | −34 ± 11 | −23 ± 10 | SD (<0.001) |
| Maximum Cobb angle (°) | |||
| PT | 38 ± 15 | 27 ± 11 | SD (<0.001) |
| MT | 57 ± 10 | 28 ± 13 | SD (<0.001) |
| TL/L | 50 ± 13 | 31 ± 12 | SD (<0.001) |
| Orientation of the plane of maximum curvature (°) | |||
| PT | 58 ± 16 | 37 ± 19 | SD (0.014) |
| MT | 70 ± 14 | 41 ± 22 | SD (<0.001) |
| TL/L | 61 ± 15 | 50 ± 23 | SD (0.005) |
| Apical vertebral axial rotation (°) | 19 ± 7 | 5 ± 4 | SD (<0.001) |
SD Significant difference, NS non-significant difference
Results
Differences in pre- and postoperative measurements
Group A patients (H/HL) had significant correction of their proximal thoracic, main thoracic and lumbar curves in the coronal plane (Table 2) with an average correction of 24, 38 and 29%, respectively. While there was no significant change of kyphosis in the sagittal plane, thus preserving the preoperative thoracic kyphosis between T4 and T12, the lumbar lordosis had a significant change, diminishing the lordosis angle by 35%. The Cobb angle in the plane of maximum curvature in all curves was significantly decreased, however, the orientation of these planes were not all significantly derotated, i.e., both the proximal thoracic and lumbar planes did not come significantly closer to the sagittal plane. In fact in both cases, the orientation went further away from the sagittal plane. With regards to the derotation of the apical vertebra, the rotation towards the normal axial orientation was significantly decreased by 4° on average; however, this change of the axial orientation is within the variability of the measuring technique used for this parameter [20].
Table 2.
Means, standard deviations, and levels of significance (P) for geometric parameters in Group A (Harrington/Harrington-Luque instrumentation) at stages I and II (before and after surgery)
| Parameter | Stage I (pre) | Stage II (post) | P (I vs. II) (paired t-test) |
|---|---|---|---|
| Coronal Cobb angle (°) | |||
| PT | 22 ± 11 | 17 ± 10 | SD (0.001) |
| MT | 50 ± 14 | 31 ± 11 | SD (<0.001) |
| TL/L | 45 ± 11 | 32 ± 12 | SD (<0.001) |
| Kyphosis (°) | 29 ± 12 | 27 ± 10 | NS (0.190) |
| Lordosis (°) | −31 ± 14 | −20 ± 13 | SD (0.002) |
| Maximum Cobb angle (°) | |||
| PT | 29 ± 11 | 23 ± 10 | SD (<0.001) |
| MT | 54 ± 14 | 38 ± 10 | SD (<0.001) |
| TL/L | 51 ± 11 | 36 ± 12 | SD (<0.001) |
| Orientation of the plane of maximum curvature (°) | |||
| PT | 54 ± 16 | 60 ± 20 | NS (0.245) |
| MT | 71 ± 12 | 57 ± 18 | SD (<0.001) |
| TL/L | 60 ± 17 | 66 ± 19 | NS (0.071) |
| Apical vertebral axial rotation (°) | 19 ± 8 | 15 ± 5 | SD (0.003) |
SD Significant difference, NS non-significant difference
Group B patients (original CDI) also had significant correction of their proximal thoracic, main thoracic and lumbar curves in the coronal plane (Table 3) with an average correction of 23, 52 and 49%, respectively. No significant change was measured in the sagittal plane with the preservation of the preoperative kyphosis curve (between T4 and T12), and slight decrease in lumbar lordosis (between L1 and L5). The Cobb angle in the plane of maximum curvature was significantly corrected in all curves. The results are similar for the orientation of these planes, where the main thoracic and lumbar planes were brought significantly closer to the sagittal plane (from 70° to 51° and from 61° to 43°, respectively), while the orientation of the PT plane was decreased but not significantly. Finally, significant corrections were observed for the derotation of the apical vertebra towards the normal axial orientation, with a decrease of 8°, representing an average correction of 33%.
Table 3.
Means, standard deviations, and levels of significance (P) for geometric parameters in Group B (original Cotrel-Dubousset instrumentation) at stages I and II (before and after surgery)
| Parameter | Stage I (pre) | Stage II (post) | P (I vs. II) (paired t-test) |
|---|---|---|---|
| Coronal Cobb angle (°) | |||
| PT | 27 ± 14 | 21 ± 10 | SD (<0.001) |
| MT | 52 ± 15 | 25 ± 11 | SD (<0.001) |
| TL/L | 45 ± 14 | 23 ± 12 | SD (<0.001) |
| Kyphosis (°) | 28 ± 13 | 29 ± 11 | NS (0.321) |
| Lordosis (°) | −31 ± 18 | −26 ± 16 | NS (0.101) |
| Maximum Cobb angle (°) | |||
| PT | 34 ± 12 | 29 ± 11 | SD (0.009) |
| MT | 55 ± 14 | 32 ± 11 | SD (<0.001) |
| TL/L | 51 ± 13 | 36 ± 11 | SD (<0.001) |
| Orientation of the plane of maximum curvature (°) | |||
| PT | 59 ± 22 | 55 ± 19 | NS (0.359) |
| MT | 70 ± 12 | 51 ± 16 | SD (<0.001) |
| TL/L | 61 ± 17 | 43 ± 24 | SD (<0.001) |
| Apical vertebral axial rotation (°) | 21 ± 9 | 14 ± 8 | SD (<0.001) |
SD Significant difference, NS non-significant difference
Group C patients more recent generations of CDI had significant correction of all three curves in both the coronal plane and planes of maximal curvature (Table 4), but most notably in the coronal plane with a correction of 25, 62 and 61% in the PT, MT and TL/L regions, respectively. The preoperative kyphosis was preserved in the sagittal plane while there was a significant decrease in the lumbar lordosis curve (23%). The orientation of all three planes of maximum curvature was brought significantly closer to the sagittal plane (from 56° to 50° in the PT, from 70° to 43° in the MT and from 60° to 37° in the TL/L). Finally, in the case of the apical vertebra axial rotation, a significant derotation towards the normal axial position was obtained with a 64% average correction.
Table 4.
Means, standard deviations, and levels of significance (P) for geometric parameters in Group C (recent generations of CDI) at stages I and II (before and after surgery)
| Parameter | Stage I (pre) | Stage II (post) | P (I vs. II) (paired t-test) |
|---|---|---|---|
| Coronal Cobb angle (°) | |||
| PT | 24 ± 11 | 18 ± 10 | SD (<0.001) |
| MT | 50 ± 11 | 19 ± 10 | SD (<0.001) |
| TL/L | 47 ± 13 | 19 ± 10 | SD (<0.001) |
| Kyphosis (°) | 28 ± 13 | 27 ± 10 | NS (0.515) |
| Lordosis (°) | −37 ± 11 | −28 ± 11 | SD (<0.001) |
| Maximum Cobb angle (°) | |||
| PT | 31 ± 11 | 24 ± 13 | SD (0.010) |
| MT | 53 ± 10 | 28 ± 11 | SD (<0.001) |
| TL/L | 54 ± 12 | 33 ± 11 | SD (<0.001) |
| Orientation of the plane of maximum curvature (°) | |||
| PT | 56 ± 19 | 50 ± 20 | SD (0.041) |
| MT | 70 ± 11 | 43 ± 19 | SD (<0.001) |
| TL/L | 60 ± 17 | 37 ± 20 | SD (<0.001) |
| Apical vertebral axial rotation (°) | 19 ± 10 | 7 ± 4 | SD (<0.001) |
SD Significant difference, NS non-significant difference
Group D patients (third generation instrumentation systems and DVD) also had significant correction of all three curves with regards to the Cobb angle in the coronal plane and in the planes of maximal curvature (Table 5). The preoperative kyphosis was preserved in the sagittal plane, while a 34% significant decrease was observed for lumbar lordosis. The orientation of the plane of maximum curvature was significantly sagittalized in all three curves, with an average correction of 36, 42 and 18% in the PT, MT and TL/L curves, respectively. Significant correction of Cobb angles in all three maximal planes was observed as well. The vertebra axial rotation was significantly derotated with a 74% average correction.
Differences between groups
Comparing the important changes of the spinal shape in terms of 3-D measurements between the four groups (Tables 6, 7), a significant correction in both the orientation of the MT and TL/L planes of maximal curvature and the axial rotation of the apical vertebral was detected between the Harrington, and CDI or DVD techniques. Fewer differences were detected between both CDI generations or between recent CDI and DVD with regards to 3-D measurements, besides a significant correction of the PT curve and a slight decrease in the correction of the lumbar curve with Group D (DVD). In the case of the Cobb angles in the planes of maximal curvature, there was no differences observed between the Harrington and original generation of CDI; however, a significant change was found in the MT curve and a tendency in the TL/L curve between the Harrington and recent CDI.
Table 6.
Means, standard deviations, and levels of significance (P) for differences of geometric parameters between stages I and II (correction) in Groups A, B, C and D
| Parameter | Group A (H/HL) | Group B (1st CD) | Group C (2nd CD) | Group D (DVD) | P-value (Anova) |
|---|---|---|---|---|---|
| Coronal Cobb angle (°) | |||||
| PT | −5 ± 8 | −6 ± 7 | −7 ± 9 | −18 ± 14 | SD (<0.001) |
| MT | −19 ± 11 | −27 ± 11 | −31 ± 11 | −37 ± 11 | SD (<0.001) |
| TL/L | −13 ± 8 | −22 ± 10 | −28 ± 10 | −23 ± 14 | SD (<0.001) |
| Kyphosis (°) | −2 ± 9 | 2 ± 9 | −1 ± 7 | −1 ± 12 | NS (0.466) |
| Lordosis (°) | −11 ± 19 | −5 ± 17 | −8 ± 11 | −10 ± 11 | NS (0.473) |
| Maximum Cobb angle (°) | |||||
| PT | −7 ± 10 | −6 ± 11 | −6 ± 13 | −12 ± 12 | NS (0.107) |
| MT | −15 ± 12 | −22 ± 11 | −25 ± 13 | −29 ± 15 | SD (0.001) |
| TL/L | −15 ± 11 | −15 ± 13 | −21 ± 11 | −20 ± 14 | NS (0.075) |
| Orientation of the plane of maximum curvature (°) | |||||
| PT | 5 ± 22 | −4 ± 22 | −8 ± 19 | −21 ± 20 | SD (<0.001) |
| MT | −14 ± 14 | −20 ± 17 | −27 ± 19 | −29 ± 17 | SD (0.001) |
| TL/L | 6 ± 16 | −18 ± 21 | −24 ± 19 | −11 ± 21 | SD (<0.001) |
| Apical vertebral axial rotation (°) | −4 ± 6 | −8 ± 9 | −13 ± 9 | −14 ± 7 | SD (<0.001) |
SD Significant difference, NS non-significant difference
Table 7.
Levels of significance (P) for pairwise differences of geometric parameters between stages I and II (correction) between Groups A, B, C and D
| Parameter | P (A vs. B) | P (A vs. C) | P (B vs. C) | P (A vs. D) | P (B vs. D) | P (C vs. D) |
|---|---|---|---|---|---|---|
| Coronal Cobb angle (°) | ||||||
| PT | NS (0.995) | NS (0.863) | NS (0.947) | SD (<0.001) | SD (<0.001) | SD (<0.001) |
| MT | SD (0.033) | SD (<0.001) | NS (0.483) | SD (<0.001) | SD (0.003) | NS (0.153) |
| TL/L | SD (0.009) | SD (<0.001) | NS (0.058) | SD (0.002) | NS (0.964) | NS (0.168) |
| Kyphosis (º) | NS (0.387) | NS (0.917) | NS (0.786) | NS (0.902) | NS (0.802) | NS (0.999) |
| Lordosis (º) | NS (0.467) | NS (0.945) | NS (0.811) | NS (0.998) | NS (0.578) | NS (0.981) |
| Maximum Cobb angle (°) | ||||||
| PT | NS (0.980) | NS (0.995) | NS (0.999) | NS (0.278) | NS (0.125) | NS (0.169) |
| MT | NS (0.162) | SD (0.017) | NS (0.789) | SD (< 0.001) | NS (0.186) | NS (0.706) |
| TL/L | NS (0.999) | NS (0.154) | NS (0.157) | NS (0.392) | NS (0.400) | NS (0.947) |
| Orientation of the plane of maximum curvature (°) | ||||||
| PT | NS (0.377) | NS (0.098) | NS (0.886) | SD (<0.001) | SD (0.010) | SD (0.048) |
| MT | NS (0.491) | SD (0.017) | NS (0.376) | SD (0.002) | NS (0.098) | NS (0.898) |
| TL/L | SD (<0.001) | SD (<0.001) | NS (0.750) | SD (0.006) | NS (0.488) | NS (0.080) |
| Apical vertebral axial rotation (°) | NS (0.224) | SD (<0.001) | SD (0.028) | SD (<0.001) | SD (0.021) | NS (0.999) |
SD Significant difference, NS non-significant difference
In the coronal plane, significant differences in the lumbar and main thoracic curves were found between the original generation of CDI and Harrington. The difference is even greater with the more recent generations of CDI with significant changes in both MT and TL/L curves. A significant difference was found between both original and recent CDI generations in the TL/L curve, as well as between DVD and all other groups in the PT curve. In the sagittal plane, no measurable differences were found in the kyphosis and lumbar lordosis between the groups. The computed statistical power (1-β) was higher than 80% in all statistical comparison tests performed in these comparisons. This indicates that there is very little possibility of a Type II error, meaning that a 20% or more difference between the four groups would not be detected because of insufficient sample size.
Discussion
In general, significantly better 3-D corrections were achieved with CDI or DVD technique, with the most notable and important differences observed with the Harrington/Harrington-Luque instrumentation. When analyzing more current 3-D oriented surgical techniques, less important but continuous improvements in 3-D correction nonetheless were found between original, recent CDI and DVD generations with significant differences in apical rotation. A definite corrective trend can be substantiated between DVD and recent CDI systems with significant differences found in terms of global 3-D correction and apical derotation, while requiring fewer levels of fusion. A clear tendency with regards to loss of lumbar lordosis can be observed in all instrumentation groups. To our knowledge there was no literature on this subject and it was our belief that this observational comparative study would be of interest to raise the level of evidence concerning 3-D effects of these surgical approaches.
Correction in the coronal and sagittal plane
Results indicate that the correction of the spine in the coronal plane follows the same tendency for all groups with a postoperative improvement; however, a significantly better correction was achieved in the lumbar region of the spine by using the CD technique compared to Harrington. This phenomenon is confirmed when analyzing the postoperative lordosis angle with the Harrington technique. In contrast, DVD does not compare as well to recent CDI systems with regards to the lumbar curve, but this effect can most probably be explained by the fewer lumbar curves being instrumented in the DVD group. In contrast, it achieves significantly better correction in the main and proximal thoracic curve. A higher level of instrumented vertebrae with a higher number of pedicle screws used in the PT region with Group D probably explain this increased correction, with 85% of patients being instrumented with pedicle screws higher than T4 compared to 15% in Group C (recent CDI).
With regards to changes in the sagittal profile, all four groups seem to preserve the preoperative thoracic kyphosis as observed by Helenius [15] and Mikhailovsky [26]. Mikhailovsky et al. documented 3-D correction with the Harrington technique, using computer-optical topography rather than 3-D radiographic reconstructions. The effect on lumbar lordosis was quite different, with a loss of physiological lumbar lordosis in Group A, confirming the well-known flat back effect [2] commonly seen with this technique and explained by the distraction mechanism of the procedure. A decrease of lumbar lordosis was also observed in Groups C and D, however, contrary to the Harrington technique, the more recent CDI and DVD generations brought above average lumbar lordosis angular values back to physiological lumbar lordosis (23 and 33% correction, respectively).
There is a definite tendency which can be observed in each generation with regards to reduction in lumbar lordosis at the postoperative stage, which was also found by Mikhailovsky et al. [26] when comparing Harrington and CDI. Although this loss of lordosis is not ideal for achieving spinal balance, this effect still remains to be explained and understood. This point still needs to be addressed in the future, and maybe linked to the effect of the pelvic and femoral head alignment in order to maintain harmony of the thoraco-lumbar segment. Variability and means shape models portraying inter-vertebral transformations within the various Groups as demonstrated in Fig. 8, may help to elucidate this observed phenomenon by analysing the effective 3-D corrective parameters [7].
Fig. 8.
Statistical model of spine shape deformations of cases in Group D (Direct Vertebral Derotation) instrumented up to L2 (Top), and lower than L2 (Bottom). From left to right: mean shapes, 3-D rotation and 3-D translation covariance
Results seem to confirm a significant improvement of coronal correction when using CDI and DVD in the main thoracic and lumbar regions, and in the proximal thoracic region with DVD, as shown in Fig. 9a. By comparison, Mikhailovsky et al. found great reduction in coronal plane Cobb angles both in the CDI and Harrington groups.
Fig. 9.
Evolution of spinal instrumentation. a Percentage (%) of correction for coronal Cobb angles; b Percentage (%) of decrease in kyphosis and lordosis; c Percentage (%) of correction in 3-D measurements including plane of maximum curvature (PMC)
Global and local 3-D correction
Orientation of the planes of maximal deformity indicates if a true 3-D correction of the spine has been achieved, and both CDI and DVD techniques significantly corrected these planes, which was not the case for the Harrington technique. In fact, a deterioration of orientation of PT and TL/L planes of maximal deformity was observed with Group A (the orientation of the planes of maximal deformity did not move towards the sagittal plane) as illustrated in Fig. 9c. This effect can also be observed in Fig. 10 showing the top views of planes of maximum curvature for similar preoperative cases taken from each group, and compared to the post-op model. Once again, the deterioration in the lumbar segment of the spine correlates with the observed flat back effect in the lordosis measurement. This may be explained by the fact that the inherent distraction phenomenon was concentrated on the main thoracic curve while distorting the lumbar curve. The introduction of the derotation manoeuver with CDI seems to counter this effect by applying forces directly on this region. In fact, Stokes et al. [31] observed a similar effect with CDI instrumentation achieving a better derotation of the maximum curvature plane when compared to the Harrington, although the improvement was of lesser amplitude. For curve measurements in the planes of maximal deformity, the results follow the same pattern as in the coronal plane, with most significant differences found between the DVD using pedicle screws and Harrington instrumentations.
Fig. 10.
Top views of planes of maximal curvature for typical pre- and post-op cases in Group A (Harrington/Harrington-Luque), Group B (original Cotrel-Dubousset Instrumentation), Group C (recent generations of Cotrel-Dubousset Instrumentation), Group D (Direct Vertebral Derotation)
Surprisingly, even though the DVD manoeuver is based on vertebral derotation, results indicate it did not achieve the same level of 3-D correction in the lumbar curve as both CDI groups. This can be linked to fewer instrumented levels in the lumbar region in the DVD group, with 72% of patients having pedicle screw insertion no lower than L2, compared to 40% with recent generations of CDI (Legacy, Horizon). In fact, a statistical difference can be found between patients instrumented higher or lower to L2 with DVD for shifting the lumbar curve towards the sagittal plane (19° vs. 8°).
With regards to the axial rotation of the apical vertebra, adequate correction was achieved in all four groups with a progressive improvement as the instrumentation type became more and more recent, especially with DVD. Stokes et al. [31] reported this phenomenon with CDI in the analysis of the apical vertebra axial rotation. This can be substantiated by the increasing number of pedicle screws used for the local derotation manoeuver in the CDI technique, and explains the very high percentage of correction in apical rotation for DVD (74%).
Methodological issues
This was a retrospective study using randomly selected patients within each Group, but no differences in patient characteristics were detected, and there did not appear to be differences associated with the fact that different surgeons were involved. Because of its retrospective nature and the use of comparison groups, this is a study of moderate strength that may benefit from additional data and replication in other populations. However, any selection bias was avoided since patients were selected on availability of data without regard to preoperative deformity or clinical characteristics.
This study reports changes in spinal geometry focused in the thoracic and lumbar regions. Inclusion of the pelvis, femoral heads and lower limbs is a crucial and important factor for understanding and analyzing the harmony of the thoraco-lumbar alignment in postoperative assessment of the spine. Because acquisition of the lower limbs and cervical spine was not mandatory at the time of the Harrington or original CDI era, the 3-D reconstruction of these structures was not included in this study. Therefore a correct and adequate comparison with recent films could not be done for this study. However, routine radiographic acquisition from head to feet is now possible with newer technologies (low-dose EOS system), making it feasible to adequately analyze the effect of the global axis of gravity of the body with regards to the effective loss of lordosis observed in the study groups.
Conclusion
With these results, we can confirm the hypothesis that an increased 3-D correction was achieved as spinal instrumentation evolved towards derotation maneuvers when comparing Harrington, CDI and DVD techniques. We can therefore state that significant progress in 3-D correction of adolescent idiopathic scoliosis has been achieved with continuous improvements in surgical techniques and instrumentations, by assessing simplified global 3-D descriptors such as the plane of maximum deformity, which measures the overall 3-D shift of the spine, or local 3-D measurements such as axial rotation.
Results obtained in this study show recent Cotrel-Dubousset Instrumentations (CDI) or direct vertebral derotation (DVD) techniques achieve important and significantly better 3-D correction of thoracic and lumbar curves of scoliotic deformities in AIS compared to previous systems such as the Harrington/Harrington-Luque techniques or the original generation of the Cotrel-Dubousset system. Recent generations of CDI achieve slightly better correction compared to original versions of CDI, while DVD techniques offer a better correction of apical vertebra rotation and of the proximal thoracic curve. Differences were also found between DVD and recent CDI systems in terms of true 3-D correction with fewer vertebral levels being fused together.
This is the first quantitative study to clearly demonstrate that the derotation manoeuvre (e.g., CDI, DVD) can produce better 3-D correction of scoliosis deformities than techniques based on distraction alone (H/HL) which only achieves correction in the 2-D plane, thereby supporting the higher costs of the CDI technique and subsequent versions of this technology.
Acknowledgments
This paper was supported in part by the Fonds Québecois de la Recherche sur la Nature et les Technologies (FQRNT) and MENTOR, a strategic training program of the Canadian Institutes of Health Research. Special thanks to Julie Joncas, Philippe Labelle and Xavier Glorot for their assistance.
Contributor Information
Samuel Kadoury, Email: samuel.kadoury@polymtl.ca.
Hubert Labelle, Phone: +1-514-3454931, FAX: +1-514-3454755, Email: hubert.labelle@recherche-ste-justine.qc.ca.
References
- 1.Aaro S, Dahlborn M (1982) The effect of Harrington instrumentation on the longitudinal axis rotation of the apical vertebra and on the spinal and rib-cage deformity in idiopathic scoliosis studied by computer tomography. Spine 7:456–462. doi:10.1097/00007632-198209000-00009 [DOI] [PubMed]
- 2.Aaro S, Ohlen G (1983) The effect of Harrington instrumentation on the sagittal configuration and mobility of the spine in scoliosis. Spine 8:570–575. doi:10.1097/00007632-198309000-00002 [DOI] [PubMed]
- 3.Aubin C-E, Lobeau D, Labelle H, Maquinghen-Godillon AP, LeBlanc R, Dansereau J (1999) Planes of Maximum Deformity in the Scoliotic Spine. In: IAF Stokes (ed) Research into spinal deformities 2. IOS Press, Amsterdam, pp 45–48
- 4.Aubin CE, Dansereau J, Parent F, Labelle H, de Guise JA (1997) Morphometric evaluations of personalised 3D reconstructions and geometric models of the human spine. Med Biol Eng Comput 35:611–618. doi:10.1007/BF02510968 [DOI] [PubMed]
- 5.Bassett GS, Hensinger MC, Keiper MD (1989) Effect of posterior spinal fusion on spinal balance in idiopathic scoliosis. J Pediatr Orthop 9:672–674 [DOI] [PubMed]
- 6.Benson DR, DeWald RL, Schultz AB (1977) Harrington rod distraction instrumentation: its effect on vertebral rotation and thoracic compensation. Clin Orthop Relat Res 125:40–44 [PubMed]
- 7.Boisvert J, Pennec X, Ayache N, Labelle H, Cheriet F (2006) 3D anatomical variability assessment of the scoliotic spine using statistics on Lie groups. In: 2006 3rd IEEE international symposium on biomedical imaging: macro to nano. IEEE, Arlington, pp 750–753
- 8.Cheriet F, Dansereau J, Petit Y, Aubin CE, Labelle H, De Guise JA (1999) Towards the self-calibration of a multiview radiographic imaging system for the 3D reconstruction of the human spine and rib cage. Int J Pattern Recogn Artif Intell 13:761–779. doi:10.1142/S0218001499000434 [DOI]
- 9.Delorme S, Labelle H, Aubin CE, de Guise JA, Rivard CH, Poitras B et al (2000) A three-dimensional radiographic comparison of Cotrel-Dubousset and Colorado instrumentations for the correction of idiopathic scoliosis. Spine 25:205–210. doi:10.1097/00007632-200001150-00010 [DOI] [PubMed]
- 10.Delorme S, Petit Y, de Guise JA, Labelle H, Aubin CE, Dansereau J (2003) Assessment of the 3-D reconstruction and high-resolution geometrical modeling of the human skeletal trunk from 2-D radiographic images. IEEE Trans Biomed Eng USA 50:989–998. doi:10.1109/TBME.2003.814525 [DOI] [PubMed]
- 11.Dubousset J, Cotrel Y (1991) Application technique of Cotrel-Dubousset instrumentation for scoliosis deformities. Clin Orthop Relat Res 264:103–110 [PubMed]
- 12.Fitch RD, Turi M, Bowman BE, Hardaker WT (1990) Comparison of Cotrel-Dubousset and Harrington rod instrumentations in idiopathic scoliosis. J Pediatr Orthop 10:44–47 [PubMed]
- 13.Friend L, Czerwein J Jr, Sharan A, Amaral T, Sarwahi V (2007) P79. Segmental direct vertebral rotational technique for scoliosis correction. Spine J 7:119S. doi:10.1016/j.spinee.2007.07.286 [DOI]
- 14.Gaines RW, McKinley LM, Leatherman KD (1981) Effect of the Harrington compression system on the correction of the rib hump in spinal instrumentation for idiopathic scoliosis. Spine 6:489–493 [DOI] [PubMed]
- 15.Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenzka D, Helenius M et al (2003) Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am 85-A:2303–2309 [DOI] [PubMed]
- 16.Humke T, Grob D, Scheier H, Siegrist H (1995) Cotrel-Dubousset and Harrington Instrumentation in idiopathic scoliosis: a comparison of long-term results. Eur Spine J 4:280–283. doi:10.1007/BF00301034 [DOI] [PubMed]
- 17.Jeffries BF, Tarlton M, De Smet AA, Dwyer SJ 3rd, Brower AC (1980) Computerized measurement and analysis of scoliosis: a more accurate representation of the shape of the curve. Radiology 134:381–385 [DOI] [PubMed]
- 18.Kadoury S, Cheriet F, Dansereau J, Labelle H (2007) Three-dimensional reconstruction of the scoliotic spine and pelvis from uncalibrated biplanar X-ray images. Spinal Disorders Techniques 20:160–168 [DOI] [PubMed]
- 19.King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65:1302–1313 [PubMed]
- 20.Labelle H, Dansereau J, Bellefleur C, Jequier JC (1995) Variability of geometric measurements from three-dimensional reconstructions of scoliotic spines and rib cages. Eur Spine J 4:88–94. doi:10.1007/BF00278918 [DOI] [PubMed]
- 21.Labelle H, Dansereau J, Bellefleur C, Poitras B, Rivard CH, Stokes IA et al (1995) Comparison between preoperative and postoperative three-dimensional reconstructions of idiopathic scoliosis with the Cotrel-Dubousset procedure. Spine 20:2487–2492 [DOI] [PubMed]
- 22.Lee SM, Suk SI, Chung ER (2004) Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine 29:343–349. doi:10.1097/01.BRS.0000109991.88149.19 [DOI] [PubMed]
- 23.Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL (1992) Cotrel-Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Joint Surg Am 74:1056–1067 [PubMed]
- 24.Luk KD, Leong JC, Reyes L, Hsu LC (1989) The comparative results of treatment in idiopathic thoracolumbar and lumbar scoliosis using the Harrington, Dwyer, and Zielke instrumentations. Spine 14:275–280. doi:10.1097/00007632-198903000-00006 [DOI] [PubMed]
- 25.Mielke CH, Lonstein JE, Denis F, Vandenbrink K, Winter RB (1989) Surgical treatment of adolescent idiopathic scoliosis. A comparative analysis. J Bone Joint Surg Am 71:1170–1177 [PubMed]
- 26.Mikhailovsky MV, Novikov VV, Sarnadsky VV (2002) Three-dimensional correction with CD instrumentation and Harrington rod in the treatment of idiopathic scoliosis. Stud Health Technol Inform 91:216–221 [PubMed]
- 27.Shah SA (2007) Derotation of the Spine. Neurosurg Clin N Am 18:339–345. doi:10.1016/j.nec.2007.02.003 [DOI] [PubMed]
- 28.Stokes IA (1994) Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine 19:236–248 [PubMed]
- 29.Stokes IA, Bigalow LC, Moreland MS (1986) Measurement of axial rotation of vertebrae in scoliosis. Spine 11:213–218. doi:10.1097/00007632-198604000-00006 [DOI] [PubMed]
- 30.Stokes IA, Bigalow LC, Moreland MS (1987) Three-dimensional spinal curvature in idiopathic scoliosis. J Orthop Res 5:102–113. doi:10.1002/jor.1100050113 [DOI] [PubMed]
- 31.Stokes IA, Labelle H, Aronsson DD (1993) Spinal shape changes in idiopathic scoliosis after Harrington or C-D instrumentation: the axial view. In: Scoliosis Research Society Annual Meeting
- 32.Stokes IA, Shuma-Hartswick D, Moreland MS (1988) Spine and back-shape changes in scoliosis. Acta Orthop Scand 59:128–133 [PubMed]
- 33.Thometz JG, Emans JB (1988) A comparison between spinous process and sublaminar wiring combined with Harrington distraction instrumentation in the management of adolescent idiopathic scoliosis. J Pediatr Orthop 8:129–132 [PubMed]
- 34.Villemure I, Aubin CE, Grimard G, Dansereau J, Labelle H (2001) Progression of vertebral and spinal three-dimensional deformities in adolescent idiopathic scoliosis: a longitudinal study. Spine 26:2244–2250. doi:10.1097/00007632-200110150-00016 [DOI] [PubMed]