Abstract
It is a measurement of Cobb’s angles between adolescent (AIS) and juvenile (JIS) idiopathic scoliosis who had stable curves (variation <5 degrees) in more than three visits. Main objective of this paper is to measure inter- and intra-observer reliability of measurements between AIS and JIS who had stable curves in regular follow-up. Twenty-nine JIS and 44 AIS patients who had stable curves without bracing were identified using PACS system. Two observers independently measured Cobb’s angle twice on first, during follow-up and final radiogram using computer-based digital radiogram. Both observers were given pre-decided level of upper and lower end plates. Inter- and intra-observer reliability of the measurement was calculated using Pearson correlation-coefficient test between JIS and AIS group. There was no significant difference in Cobb’s angle in all measurements by both observers either in JIS (p = 0.756, range 0.706–0.815; ANOVA) or AIS (p = 0.871, range 0.795–0.929; ANOVA) group which suggested that there is no significant difference in Cobb’s angle in repeated measurements. Intra-observer reliability for JIS (r = 0.600, range 0.521–0.751; Pearson test) was less than AIS (r = 0.969, range 0.943–0.984; Pearson test); and similarly, inter-observer reliability for JIS (r = 0.547, Pearson test) was also less than AIS (r = 0.961, Pearson test) which indicates that Cobb’s angle measurement is less reliable in patients who have juvenile idiopathic scoliosis. Using the identical condition for measurements in both the groups, we could find only one reason for less reliability in JIS group and that is poor demarcation of the vertebral end-plates in this group. This poor inter- and intra-observer reliability in JIS due to ill-defined endplates can be reduced by measuring all previous curves along with latest curves at the same time during the follow-up of patients with JIS to decide about the progression of curves and treatment options.
Keywords: Juvenile and adolescent idiopathic scoliosis, Stable curves, Cobb’s angle, Computerized digital radiogram, Inter- and intra-observer reliability
Introduction
The Cobb’s method is the standard method of quantitating scoliosis measurement [7]. Although it is originally intended for evaluation of the adolescent idiopathic scoliosis (AIS), the use of the Cobb’s angle has expanded to be used in other forms of scoliosis, including congenital and juvenile form [10, 16, 17]. Although the Cobb’s angle is recognized as being a measure of the amount of tilt of the end-vertebrae rather than as objective measure of all aspects of the deformity, it is used to make decisions about the progression of a curve, the need for treatment, and the effectiveness of treatment. Surgical planning, including the levels to be fused, also proceeds in part from determination of the upper and lower vertebrae of the major curve [12]. However, we have observed that even in a same radiogram or different radiograms with a stable curve, measurement of Cobb’s angle shows different values. Most investigators have considered 5 degrees of change or more between two successive radiograms to be clinically important, even though there is no firm evidence to support the use of this figure [3, 19]. Lonstein and Carlson [18], in their study of the natural progression of scoliosis, used a 5-degree difference between the Cobb’s angles on two successive radiographs as the criterion of progression. Brooks et al. [2] and Rogala et al. [24] also used 5 degree as the criterion of progression in their epidemiological studies.
In most scientific endeavors, including medicine, there is need of accurate measurement that decides the guideline for the further treatment. Measuring accuracy of Cobb’s angle, it varies between 2 and 11 degrees in the literature [4, 5, 27] for adolescent idiopathic scoliosis. This difference could be more in congenital or non-congenital scoliosis ≤10 years of group [17]. Literature showed inter- and intra-observer variability in measurement of Cobb’s angle if measured for many times. A few reports also noted different reliability in adolescent idiopathic scoliosis [8, 20, 29]. Reliability denotes the repeatability of measurements by assessing the agreement of different rates viewing the same material. More reliability simply means less variation among the different measurements. Advancement in technology like computerized digital radiogram has shown good reliability and less variation in measurement than manual method in various articles [6, 15, 21, 23, 27]. However, if identical conditions applied to two groups adolescent idiopathic (AIS) and juvenile idiopathic (JIS) scoliosis, reliability has not been described; especially if measured in more than one radiogram with stable curves.
In present paper, we have measured Cobb’s angle in patients who had stable curves (less than 5 degrees variation between successive follow-up and between first and last follow-up) and tried to find out inter- and intra-observer reliability. Our aim was to compare this reliability between stable AIS and JIS groups and find out if there is any difference.
Material and methods
We have identified 29 curves with JIS and 44 curves with AIS from our record of 3,466 patients who had stable curves and visited more than three times to our outpatient clinic. Criteria for selection of patient were: (1) more than three visits; (2) difference between two successive radiogram was <5 degrees and between first and last radiogram was also <5 degrees; (3) curve should be >10 degrees on database; (4) age for JIS patients were between 5 and 10 years for all radiograms and for AIS between 10 and 16 years for all visits; and (5) none of patient received bracing or any kind of manipulation treatment. In our computerized recorded database system (PACS), all curves were measured by the senior author (SWS) and it was used to find out our required database for this study. All radiograms were taken with digitalized radiogram with patients in standing position keeping the tube 72 inches from the body. All patients had undergone anteroposterior radiogram of whole spine and stored in our PACS system. The average age at last radiogram for JIS group was 8.3 ± 1.7 years (range 5–10 years) and for AIS were 13 ± 1.32 years (range 11–16 years). All curves were having King types II or III scoliosis and so angles were measured at thoracic level using Cobb’s method. To reduce the error related with decision of level of the curves, upper and lower endplates for the curves were predicated by senior author (SWS) who also has chosen three radiograms (initial visit, during follow-up and last visit) for all patients in present study.
Two spine fellows (HNM and CT) who are well aware of all measurement techniques measured the Cobb’s angle for all the curves (i.e., three stable curves for each patient) using computer-based digital radiogram on picture achieving computer system (PACS) independently. Two weeks later same procedure was repeated by both the observers and that is how measurements were done two times. Both observers utilized the same endplates for measurement of Cobb’s angle in all curves both the times.
Statistical analysis
To find out any difference in the Cobb’s angle among three curves, ANOVA test was applied for both JIS and AIS group. Intra-observer reliability of measurement among all three curves and among the curves between first and second measurements was calculated using Pearson’s correlation coefficient test for both observers independently and r value was compared between JIS and AIS group. Similarly, inter-observer reliability for all repeated measurements of stable curves between two observers was calculated using Pearson’s correlation coefficient test and r value was compared between JIS and AIS groups.
Results
There were 29 patients in juvenile idiopathic scoliosis (JIS) and 44 patients in adolescent idiopathic scoliosis (AIS) group with an average age of 8.3 ± 1.7 years (range 5–10 years) and 13 ± 1.32 years (range 11–16 years), respectively. There were 7 males and 22 females in JIS group, and 13 males and 31 females in AIS group suggesting no difference (p = 0.612, Chi-square test) between both the groups. The average Cobb’s angle was 13.64 ± 2.64 degrees (range 10–23 degrees) for JIS and 27.27 ± 9.76 degrees (range 10–45 degrees). None of the patient had treatment with bracing; all patients were being observed during outpatient clinic. Measuring the Cobb’s angle in JIS group, there was no significant difference among all three curves (p = 0.756; range 0.706–0.816, ANOVA test) for both the measurements by two observers. Similarly Cobb’s angle measurement in AIS group, we could not find out any significant difference (p = 0.871; range 0.795–929, ANOVA test) for both the measurements by two observers (Tables 1, 2).
Table 1.
Average Cobb’s angle with their standard deviation for both observers in all radiograms in Juvenile idiopathic scoliosis (JIS) group
| Observer A | Observer B | All | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First observation | Second observation | First observation | Second observation | ||||||||||
| X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | Average | |
| Cobb’s (degree) | 13.6 | 13.2 | 13.8 | 13.5 | 13.7 | 13.2 | 13.4 | 13.4 | 13.9 | 13.8 | 13.6 | 14.1 | 13.6 |
| SD (degree) | 2.8 | 2.8 | 3.0 | 2.9 | 2.7 | 2.6 | 2.8 | 2.6 | 3.3 | 2.6 | 2.1 | 3.5 | 2.8 |
| ANOVA (p value) | 0.706 | 0.815 | 0.753 | 0.749 | 0.756 | ||||||||
SD standard deviation, X-1 initial radiogram, X-2 follow-up radiogram, X-3 final radiogram
Table 2.
Average Cobb’s angle with their standard deviation for both observers in all radiograms in adolescent idiopathic scoliosis (AIS) group
| Observer A | Observer B | All | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First observation | Second observation | First observation | Second observation | ||||||||||
| X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | X-1 | X-2 | X-3 | Average | |
| Cobb’s (degree) | 26.2 | 26.5 | 27.2 | 26.6 | 27.3 | 27.6 | 27.0 | 27.5 | 28.4 | 27.2 | 28.0 | 27.3 | 27.2 |
| SD (degree) | 10.0 | 9.8 | 9.4 | 10.0 | 9.7 | 9.2 | 9.9 | 10.1 | 9.6 | 9.7 | 9.8 | 10.4 | 9.7 |
| ANOVA (p value) | 0.881 | 0.881 | 0.795 | 0.929 | 0.871 | ||||||||
SD standard deviation, X-1 initial radiogram, X-2 follow-up radiogram, X-3 final radiogram
Intra-observer reliability
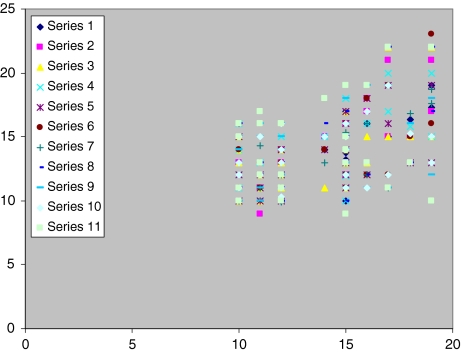
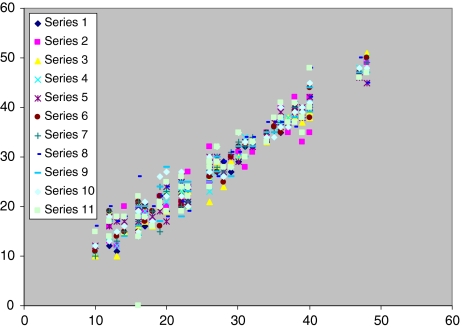
For JIS group, average intra-observer reliability was 0.600 (range 0.473–0.752) for first and second observer, which indicates poor intra-observer reliability in measuring Cobb’s angle in JIS patients (Table 3). However, for AIS group, average intra-observer reliability was 0.969 (range 0.943–0.984) for first and second observer, which indicates high intra-observer reliability in measuring Cobb’s angle in AIS patients (Table 3; Figs. 1, 2).
Table 3.
Intra-observer reliability values among all radiograms for both observers individually in both groups
| Observer A | Observer B | |||||||
|---|---|---|---|---|---|---|---|---|
| X-1 | X-2 | X-3 | All | X-1 | X-2 | X-3 | All | |
| JIS group | 0.521 | 0.578 | 0.752 | 0.605 | 0.558 | 0.473 | 0.715 | 0.611 |
| Average | 0.600 | |||||||
| AIS group | 0.975 | 0.984 | 0.952 | 0.971 | 0.977 | 0.982 | 0.943 | 0.964 |
| Average | 0.969 | |||||||
Values ‘r’ is calculated using Pearson correlation test. Value 0.80–1.00 denotes high reliability; 0.60–0.79 denotes good reliability and <0.60 denote poor reliability
Fig. 1.
Measurement of Cobb’s angle in Juvenile idiopathic scoliosis is scattered and less reliable
Fig. 2.
Measurement of Cobb’s angle in adolescent idiopathic scoliosis is uniform and more reliable
Inter-observer reliability
For JIS group, inter-observer reliability was 0.527 (range 0.412–0.604), which indicates again poor inter-observer reliability in JIS patients (Table 4). While for AIS group, inter1 observer reliability was 0.963 (range 0.957–973), which indicates high inter-observer reliability in AIS patients (Table 4; Figs. 1, 2).
Table 4.
Inter-observer reliability values among different measurements in both observers in both groups
| A1 versus B1 | A1 versus B2 | A2 versus B1 | A2 versus B2 | Average | |
|---|---|---|---|---|---|
| JIS group | 0.603 | 0.412 | 0.492 | 0.604 | 0.527 |
| AIS group | 0.968 | 0.957 | 0.953 | 0.973 | 0.963 |
A1 versus B1 means first observation of observer A is compared with first measurement of observer B; A1 versus B2 means first observation of observer A is compared with second measurement of observer B; A2 versus B1 means second observation of observer A is compared with first measurement of observer B; and A2 versus B2 means second observation of observer A is compared with second measurement of observer B
Identifiable cause of reliability
Statistical test indicates that there is no significant difference among the different observation in both the groups suggesting all curves are stable. However, using identical situations for measuring Cobb’s angle JIS had poor inter- and intra-observer reliability than AIS group. Comparing the end-plates we could find out poorly demarcated end-plates in JIS group compared to AIS group (Fig. 3), which was the only identifiable factor for the difference.
Fig. 3.
a Poorly demarcated end plates in juvenile idiopathic scoliosis which causes inter- and intra-observer reliability less than (b) adolescent idiopathic scoliosis which has well-demarcated end plates
Discussion
As reported by several authors, we have considered stable curve that has less than 5 degrees variation in successive radiograms as well as first and final radiograms. In the most of reports reliability was measured for AIS group; while in present study we have measured and compared reliability in JIS and AIS both groups. And, we found that inter- or intra-observer reliability is less in JIS group. In addition, all previous studies have used only one radiogram for measurement variability or reliability; however, none of the report has measured the same in stable scoliosis using repeated radiograms. In present paper, we have identified 29 stable curves in JIS group and 44 stable curves in AIS group from our computerized database of 3,464 patients; and therefore, this is the first study using stable curves on three radiograms and measuring intra- and inter-observer reliability for both groups.
There are various reports suggesting intra- and inter-observer reliability for measuring Cobb’s angle using conventional radiogram; however, there are a few studies using digital radiograms also [1, 4, 11, 13–15, 21–23, 27]. The use of digital radiography offers several advantages, including easy storage, accessibility, long-term cost savings, portability, and ability to adjust contrast and brightness using specialized software. It can be rapidly transmitted among facilities and examined by different practitioners. It is quickly becoming the standard medium [27]. In present paper, we have calculated Cobb’s angle using digital radiogram for all the curves.
Cheung [5] also reported high inter-observer reliability for computer based measurements of the coronal Cobb’s angle. Shea [27] compared Cobb’s angle measurements of curves with preselected end-vertebrae and found reliability value of 0.96 for the manual set and 0.97 for the computer set. Mok et al. [20] measured inter-observer reliability of Cobb’s angle measurements made using conventional radiographs and three commonly used forms of digital radiography representing different outputs of the identical image captured on a digital radiography system. They found excellent inter-observer reliability (0.93–0.98) for conventional radiographs, computer-based images, and digital fitted print-outs. Kuklo [15] compared intra-observer reliability for manual versus computer-based measurements and found similar intra-observer variability and good to excellent correlation of manual and digital measurements. These studies comparing digital and conventional radiograms relied on images obtained by conventional radiography and subsequently scanned into a computer. However, in our study, digital images were produced by a digital radiographic system. Stokes and Aronsson [28] also noted that computer-assisted algorithms improve reliability of Cobb angle measurement of scoliosis. We have measured the Cobb’s angle on digital radiogram using computer-based system which is very fast and can be calculated with magnification too.
Wills et al. [29] compared Cobb’s angle measurement of scoliosis radiographs with preselected end vertebrae and noted 0.994 reliability for traditional and digital, 0.987 for traditional and computer, and 0.993 for digital and computer radiograms. They also noted that with preselected end vertebrae in AIS, Cobb’s angle measurement is a reliable method for traditional, digital or computer method. Morrissy et al. [21] noted that selection of end-vertebrae is the single most error in different variability or poor reliability in measuring Cobb’s angle; however, our results deny this as we have preselected end-vertebrae levels. Senior author pre-selected the upper and lower end plates for all the curves before the study which was given to both the observers; and they measured the Cobb’s angle independently twice at an interval of 2 weeks on computer. We have major difference in intra- and inter-observer reliability between JIS and AIS group, which we think only due to indistinct demarcation of end-plates in JIS group. After obtaining the results we again tried to find out the cause for less reliability in JIS group even though we have used identical situations for measuring the Cobb’s angle in both groups. And we observed less demarcated one of either or both the end plates in JIS group than AIS group [23]. We think even using identical situations and due to the obvious difference in appearance in end plates, inter- and intra-observer reliability is going to be less in JIS patients. Previously reports mentioned that in children less than 10 years with congenital scoliosis or noncongenital scoliosis (includes neuromuscular and infantile also) the inter- and intra-observer variation is higher than AIS patients to determine curve progression. However, in stable curves (difference was less than 5 degrees between two consecutive radiograms, and between first and final radiograms) with preselected end vertebrae, there should be high reliability in measuring the Cobb’s angle in either group. But we did not find high reliability in JIS group which suggested us to measure all radiograms once again during the follow-up of a patient at the same time; and based on repeated measurement we should conclude about the progression of curve.
Sapkas et al. [25] have showed significant correlation among thoracic, thoracolumbar and lumbar Cobb’s angle in their study on prediction of Cobb’s angle in adolescent idiopathic scoliosis. However, in present study, we found out only those stable curves that had primarily thoracic curves to avoid variations among the other curve patterns. We think that this is the positive aspect of our study. Authors have also reported that there may be some extrinsic errors [9, 26, 30] in measuring the Cobb’s angle like technique of radiograph. Distance of X-ray tube from the body, timing of the radiogram, technician and position of patients are described as extrinsic errors which can cause less reliability or high variations in Cobb’s angle and which could be limiting factors for our study. However, we have taken all radiograms using a single radiogram machine with a single X-ray technician. Timing while taking radiogram is also described as important factor; however, in our institute we have outpatient clinic for the scoliosis patients on a fixed single day in a week only for 3 h (every Thursday evening 5–8 pm is our scoliosis clinic for all new and old scoliosis patients) and; we think this would not make errors in measuring the angles. Regarding the positions and distance, all radiographs were taken in standing positions with a distance of 72 inches from patients as standard. Second thing, all radiograms were antero-posterior view of whole spine so universally for all patients and so we think that could not be added to the measurement errors.
In conclusion, we could say that there is less inter- and intra-observer reliability in measurement of Cobb’s angle in juvenile idiopathic scoliosis than adolescent idiopathic scoliosis mainly due to indistinct end plates in JIS. This can be reduced by measuring all previous curves along with latest curves at a same time during the follow-up of patients with JIS to decide about the progression of curves and treatment options. We think our study of measuring inter- and intra-observer reliability of Cobb’s angle in different radiograms with stable curves and comparing them between two different groups would further add focus regarding the progression and treatment strategies especially in JIS group.
Conflict of interest statement
Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interests, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Contributor Information
Hitesh N. Modi, Email: modispine@yahoo.co.in
Seung Woo Suh, Phone: +82-2-6261992, FAX: +82-2-8671145, Email: spine@korea.ac.kr.
References
- 1.Bansal GJ (2006) Digital radiography. A comparison with modern conventional imaging. Postgrad Med J 82:425–428. doi:10.1136/pgmj.2005.038448 [DOI] [PMC free article] [PubMed]
- 2.Brooks HL, Azen SP, Gerberg E, Brooks R, Chan L (1975) Scoliosis: a prospective epidemiological study. J Bone Joint Surg Am 57:968–972 [PubMed]
- 3.Brown JC, Axelgaard J, Howson DC (1984) Multicenter trial of a noninvasive stimulation method for idiopathic scoliosis: a summary of early treatment results. Spine 9:382–387. doi:10.1097/00007632-198405000-00010 [DOI] [PubMed]
- 4.Carman DL, Browne RH, Birch JG (1990) Measurement of scoliosis and kyphosis radiographs: intraobserver and interobserver variation. J Bone Joint Surg Am 72:328–333 [PubMed]
- 5.Cheung J, Wever DJ, Veldhuizen AG et al (2002) The reliability of quantitative analysis on digital images of the scoliotic spine. Eur Spine J 11:535–542. doi:10.1007/s00586-001-0381-7 [DOI] [PubMed]
- 6.Chockalingam N, Dangerfield PH, Giakas G, Cochrane T, Dorgan JC (2002) Computer-assisted Cobb measurement of scoliosis. Eur Spine J 11:353–357. doi:10.1007/s00586-002-0386-x [DOI] [PMC free article] [PubMed]
- 7.Cobb JR (1948) Outline for the study of scoliosis. In: Instructional course lectures, vol. 5. American Academy of Orthopedic Surgeons, Ann Arbor, pp 61–75
- 8.Dang NR, Moreau MJ, Hill DL, Mahood JK, Raso J (2005) Inter-observer reproducibility and intra-observer reliability of the radiographic parameters in the spinal deformity study group’s AIS radiographic measurement manual. Spine 30(9):1064–1069. doi:10.1097/01.brs.0000160840.51621.6b [DOI] [PubMed]
- 9.Dawson EG, Smith RK, McNiece GM (1978) Radiographic evaluation of scoliosis. A reassessment and introduction of the scoliosis chariot. Clin Orthop Relat Res 131:151–155 [PubMed]
- 10.Facanha-Filho FA, Winter RB, Lonstein JE et al (2001) Measurement accuracy in congenital scoliosis. J Bone Joint Surg Am 83:42–45 [DOI] [PubMed]
- 11.Goldberg MS, Poitras B, Mayo NE et al (1988) Observer variation in assessing spinal curvature and skeletal development in adolescent idiopathic scoliosis. Spine 13:1371–1377. doi:10.1097/00007632-198812000-00008 [DOI] [PubMed]
- 12.James JIP (1976) Scoliosis, 2nd ed edn. Churchill Livingstone, Edinburg, pp 10–11
- 13.Kuklo TR, Potter BK, O’Brien MF et al (2005) Reliability analysis for digital adolescent idiopathic scoliosis measurement. J Spinal Disord Tech 18:152–159. doi:10.1097/01.bsd.0000148094.75219.b0 [DOI] [PubMed]
- 14.Kuklo TR, Potter BK, Polly DW Jr et al (2005) Reliability analysis for manual adolescent idiopathic scoliosis measurements. Spine 30:444–454. doi:10.1097/01.brs.0000153702.99342.9c [DOI] [PubMed]
- 15.Kuklo TR, Potter BK, Schroeder TM, O’Brien MF (2006) Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine 11(31):1240–1246. doi:10.1097/01.brs.0000217774.13433.a7 [DOI] [PubMed]
- 16.Loder RT, Urquhart A, Steen H et al (1995) Variability in Cobb’s angle measurement in children with congenital scoliosis. J Bone Joint Surg Br 77:768–770 [PubMed]
- 17.Loder RT, Spiegel D, Gutknecht S, Kleist K, Ly T, Mehbod A (2004) The assessment of intraobserver and interobserver error in the measurement of noncongenital scoliosis in children ≤10 years of age. Spine 22(29):2548–2553. doi:10.1097/01.brs.0000144828.72721.d8 [DOI] [PubMed]
- 18.Lonstein JE, Carlson JM (1984) The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 66:1061–1071 [PubMed]
- 19.McCollough NCIII (1986) Nonoperative treatment of idiopathic scoliosis using surface electrical stimulation. Spine 11:802–804. doi:10.1097/00007632-198610000-00010 [DOI] [PubMed]
- 20.Mok JM, Berven SH, Diab M, Hackbarth M, Hu SS, Devieren V (2008) Comparison of observer variation in conventional and three digital radiographic methods used in the evaluation of patients with adolescent idiopathic scoliosis. Spine 6(33):681–686 [DOI] [PubMed]
- 21.Morrissy RT, Goldsmith GS, Hall EC et al (1990) Measurement of the Cobb angle on radiographs of patients who have scoliosis: evaluation of intrinsic error. J Bone Joint Surg Am 72:320–327 [PubMed]
- 22.Munro BH (1997) Correlation. In: Munro BH (ed) Statistical methods for health care research, 3rd edn. Lippincott-Raven, Philadelphia, pp 224–245
- 23.Oda M, Rauh S, Gregory PB et al (1982) The significance of roentgenographic measurement in scoliosis. J Pediatr Orthop 2:378–382 [DOI] [PubMed]
- 24.Rogala EJ, Drummond DS, Gurr J (1978) Scoliosis: incidence and natural history. A prospective epidemiological study. J Bone Joint Surg Am 60:173–176 [PubMed]
- 25.Sapkas G, Papagelopoulos PJ, Kateros K, Koundis GL, Boscainos PJ, Koukou UI, Katonis P (2003) Prediction of Cobb angle in idiopathic adolescent scoliosis. Clin Orthop Relat Res 411:32–39. doi:10.1097/01.blo.0000068360.47147.30 [DOI] [PubMed]
- 26.Sevastikoglou JA, Bergquist E (1969) Evaluation of the reliability if radiological methods for registration of scoliosis. Acta Orthop Scand 40:608–613 [DOI] [PubMed]
- 27.Shea KG, Stevens PM, Nelson M et al (1998) A comparison of manual versus computer-assisted radiographic measurement intraobserver measurement variability for Cobb angles. Spine 23:551–555. doi:10.1097/00007632-199803010-00007 [DOI] [PubMed]
- 28.Stokes IAF, Aronsson DD (2006) Computer-assisted algorithms improve reliability of King classification and Cobb angle measurement of scoliosis. Spine 6(31):665–670. doi:10.1097/01.brs.0000203708.49972.ab [DOI] [PubMed]
- 29.Wills BPD, Auerbach JD, Zhu X, Caird MS, Horn BD, Flynn JM, Drummond DS, Dormans JP, Ecker ML (2007) Comparison of Cobb angle measurement of scoliosis radiographs with preselected end vertebrae. Traditional versus digital acquisition. Spine 1(32):98–105. doi:10.1097/01.brs.0000251086.84420.d1 [DOI] [PubMed]
- 30.Zetterberg C, Hansson T, Lidstrom J, Irstram L, Andersson G (1983) Daytine postural changes of the scoliosis spine. Orthop Trans 7:7–8