Abstract
Objective
Aim of study was to find a proper method for assessing subsidence using a radiologic measurement following anterior cervical discectomy and fusion (ACDF) with stand-alone polyetheretherketone (PEEK), Solis™ cage.
Methods
Forty-two patients who underwent ACDF with Solis™ cage were selected. With a minimum follow-up of 6 months, the retrospective investigation was conducted for 37 levels in 32 patients. Mean follow-up period was 18.9 months. Total intervertebral height (TIH) of two fused vertebral bodies was measured on digital radiographs with built-in software. Degree of subsidence (ΔTIH) was reflected by the difference between the immediate postoperative and follow-up TIH. Change of postoperative disc space height (CT-MRΔTIH) was reflected by the difference between TIH of the preoperative mid-sagittal 2D CT and that of the preoperative mid-sagittal T1-weighted MRI.
Results
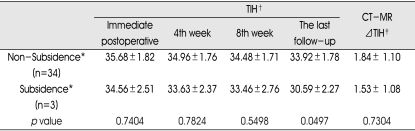
Compared to preoperative findings, postoperative disc height was increased in all cases and subsidence was observed only in 3 cases. For comparison of subsidence and non-subsidence group, TIH and CT-MRΔTIH of each group were analyzed. There was no statistically significant difference in TIH and CT-MRΔTIH between each group at 4 and 8 weeks, but a difference was observed at the last follow-up TIH (p=0.0497).
Conclusion
ACDF with Solis™ cage was associated with relatively good radiologic long-term results. Fusion was achieved in 94.5% and subsidence occurred in 8.1% by the radiologic assessment. Statistical analysis reveals that the subsidence seen later than 8 weeks after surgery and the development of subsidence does not correlate statistically with the change of the postoperative disc space height.
Keywords: Cervical PEEK cage, Radiologic assessment, subsidence, Fusion rate, Anterior cervical discectomy and fusion
INTRODUCTION
After the first description of anterior cervical discectomy and fusion (ACDF)7,19), the surgical techniques and cages have been modified to minimize the complications associated with interbody fusion5,14). There has been an advent of various types of cages to avoid the problems associated with tricortical iliac crest graft, particularly donor site morbidity2,18). Recently, this operation has undergone changes involving synthetic interbody cages with materials such as titanium, carbon fiber, and polyetheretherketone (PEEK)4,12,16). However, a study of Bartels et al.3) has raised concerns in regard to subsidence failure of stand-alone cages. They investigated the subsidence of a carbon fiber reinforced polymer cage and reported a high rate of subsidence of approximately 30%. This prompted us to review our own cases of ACDF in which a PEEK cage (Solis™ cage, Stryker Spine, Allendale, NJ) was utilized as a stand-alone device. We evaluated the radiologic outcomes and an attempt was made to reflect exact subsidence rate measured by a proper radiologic method.
MATERIALS AND METHODS
Forty-two patients who underwent the ACDF using the Solis™ cage from July 2004 to November 2006 were included. Surgical indications were limited to degenerative cervical disc disease and cervical spondylotic radiculopathy or myelopathy. The retrospective investigation was conducted in May 2007.
Surgical technique
Surgical procedure was performed using a standard anterior cervical approach. Microscope-assisted discectomy and decompression were performed. The cartilaginous end plate was removed with curettage and the posterior longitudinal ligament was opened and removed. The bony end plates were protected from drilling or curetting procedure. After the dura was decompressed, an appropriate-sized cage for disc space height was selected with trial cages in the operative field. The cage was filled with allograft bone chip or the demineralized bone matrix (DBM) and gently impacted into the prepared disc space. The Solis™ cage is a hollow frame with retentive teeth on the top and bottom, which improve the fixation of the cage to the bone. The two associated titanium pins are placed vertically in the medial plane and inserted 1 mm into adjacent vertebral bodies. After surgery, all patients were instructed to use a soft cervical collar for comfort during the first 8 weeks.
Radiological outcome assessment
Plain lateral radiographs were taken after surgery and at 4 and 8 weeks after operation. At least 6 months after surgery, the last follow-up neutral lateral, flexion and extension radiographs and two-dimensional computed tomography (2D CT) were taken. In this study, a proper method of disc space height measurement was applied to each case. Total intervertebral height (TIH) of two fused vertebral bodies was measured as distance between the mid-point of upper end plate of cranial vertebral body and the mid-point of lower end plate of caudal vertebral body on digital radiographs with built-in software (Marosis 5.0 PACS viewer, Marotech, Korea) (Fig. 1). Degree of subsidence (ΔTIH) was reflected by difference between the immediate postoperative TIH and the follow-up TIH. ΔTIH was calculated as a difference between TIH at the immediate postoperative and TIH at the 4 weeks, 8 weeks and the last follow-up lateral radiographs (Fig. 2A). With the same method, change of postoperative disc space height (CT-MR ΔTIH) was reflected by the difference between TIH of the postoperative mid-sagittal 2D CT and that of the preoperative mid-sagittal T1-weighted MRI. CT-MR ΔTIH was calculated between TIH of the postoperative CT and that of the preoperative T1-weighted MRI (Fig. 2B). ΔTIH greater than 3 mm was considered as relevant subsidence9,20) (Fig. 3). A negative CT-MR ΔTIH represents that the postoperative disc space height was decreased compared with preoperative disc space height. Fusion was assessed with the 2D CT by observation of bony bridge formation around or inside the cage or increase of bone density inside the cage (Fig. 4).
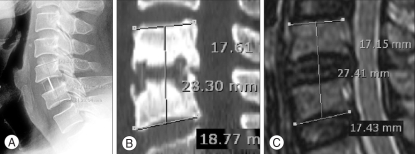
Fig. 1.
Digital radiologic images on which total inter-vertebral height (TIH) of the two fused vertebral bodies. The distance between the mid-point of upper end plate of cranial vertebral body and the mid-point of lower end plate of caudal vertebral body was measured with in-built software (Marosis 5.0 PACS viewer, Marotech, Korea). TIH are measured on the postoperative lateral plain radiograph (A), postoperative mid-sagittal 2D computed tomography (B), preoperative mid-sagittal T1-weighted magnetic resonance image (C).
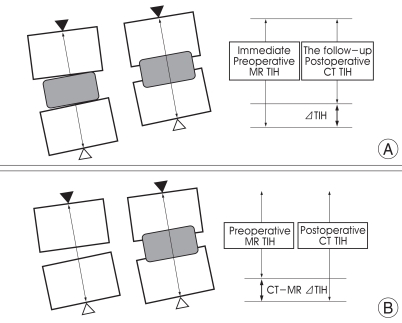
Fig. 2.
Diagram showing measurement of total inter-vertebral height (TIH) of the two fused vertebral bodies, the black arrow head is the mid-point of upper end plate of cranial vertebral body, the white arrow head is the mid-point of lower end plate of caudal vertebral body and the arrow line indicates TIH. A showing measurement of ΔTIH (difference between the immediate postoperative TIH and the follow-up TIH in the lateral radiographs). B showing measurement of computed tomography (CT)-magnetic resonance (MR) ΔTIH (difference between TIH of the postoperative mid-sagittal 2D CT and that of the preoperative mid-sagittal T1-weighted MR). The degree of subsidence was reflected by ΔTIH and the change of postoperative disc space height was reflected by CT-MR ΔTIH.
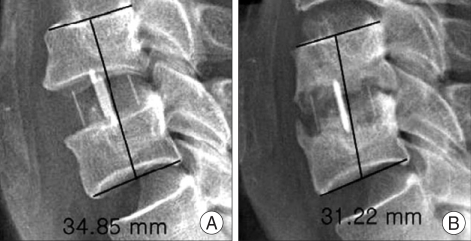
Fig. 3.
Radiographs demonstrating the cage subsidence in the immediate postoperative (A) and the last follow-up (B). Δtotal inter-vertebral height greater than 3 mm was considered relevant subsidence (ΔTIH : 34.85-31.22 = 3.63mm > 3mm).
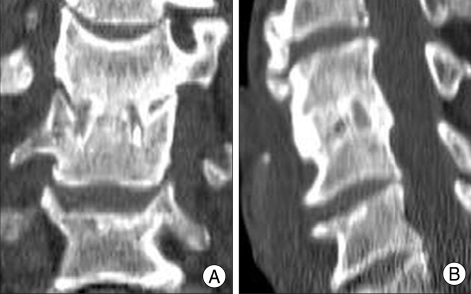
Fig. 4.
The two-dimensional computed tomography findings of fusion state. There is bony bridge formation around or inside the cage and increasing bone density inside the cage. Coronal reconstruction view (A), sagittal reconstruction view (B).
Statistical analysis
Descriptive data are represented as mean±standard deviation (mm). For comparison of nonparametric data, Wilcoxon rank-sum test and Wilcoxon Two-Sample test were used. The level of significance was a probability value of less than 0.05. All analyses were performed using a commercial software package (Statistical Analysis System, SAS institute, Cary, NC).
RESULTS
Demographic results
Among the 42 patients who underwent ACDF with Solis™ cage for cervical disease, 7 patients were lost to follow-up and in 3 patients, the measurement of TIH was not possible because of the obscuration by shoulder on the lateral radiograph. In the total 32 patients (27 patients had a single level fusion and 5 patients two-level fusion), 37 fusion levels were assessed. The mean follow-up period was 18.9 months (range, 6-34 months). All patients were male. The mean age was 57.4 years (range 43-68 years).
Radiological outcome
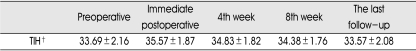
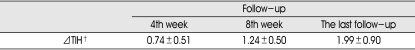
The mean±standard deviation of TIH measured at the preoperative, immediate postoperative, 4 weeks, 8 weeks and the last follow-up radiographs were given in Table 1. ΔTIH of 4 weeks, 8 weeks and the last follow-up were listed in Table 2. None of ΔTIH at 4 weeks and 8 weeks were greater than 3 mm and there were 3 cages where ΔTIH at the last follow-up were more than 3 mm. That is, subsidence greater than 3 mm was observed in 3 cages at the last follow-up (8.1%, 3 of 37 cages).
Table 1.
Total inter-vertebral height (TIH) of the two fused vertebral bodies*
*descriptive data represents mean±standard deviation (mm),†TIH indicates the distance between the mid-point of upper end plate of cranial vertebral body and the mid-point of lower end plate of caudal vertebral body
Table 2.
ΔTIH at 4 weeks, 8 weeks and the last follow-up*
*descriptive data represents mean±standard deviation (mm),†ΔTIH=difference between the immediate postoperative TIH and the follow-up TIH (4th, 8th week and the last follow-up)
The mean±standard deviation of CT-MR ΔTIH was 1.73±1.08 mm and there was no negative CT-MR ΔTIH, indicating that the postoperative disc space height was increased in all cages, compared with the preoperative height.
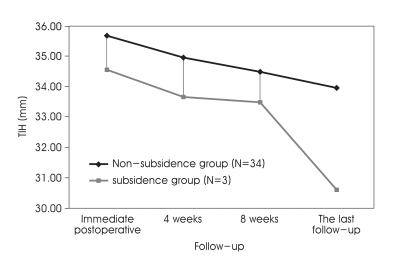
For comparison of subsidence and non-subsidence cage, each cage was grouped into subsidence cage group (n=3) and non-subsidence cage group (n=34). TIH and CT-MR ΔTIH of each group were analyzed statistically (Table 3) and TIH of each group was graphed in Fig. 5. Until the 8th week, there were no statistically significant difference in TIH between non-subs idence group and subsidence group. Statistically significant difference was observed at the last follow-up between the two groups (p=0.0497), indicating that the subsidence was seen after than 8 weeks after surgery. There was no statistically significant difference in CT-MR ΔTIH between the two groups, which means that the development of subsidence did not correlate statistically with the change of the postoperative disc space height.
Table 3.
TIH and CT-MR ΔTIH of non-subsidence cage group and subsidence cage group
The level of significance was a probability value of less than 0.05. *descriptive data represents mean±standard deviation (mm), †Statistic analysis between TIH of non-subsidence and subsidence groups was performed with the Wilcoxon rank-sum test, ‡Statistic analysis between CT-MR ΔTIH of non-subsidence and subsidence group was performed with the Wilcoxon Two-sample test
Fig. 5.
The graph illustrating total inter-vertebral height (TIH) of non-subsidence group and subsidence group at each follow-up. Until the 8 week follow-up, there was no statistically significant difference in TIH between non-subsidence group and subsidence group. Statistically significant difference is observed at the last follow-up(p=0.0497), indicating that the subsidence has occurred at later than 8 weeks after surgery.
At the last follow-up 2D CT, fusion was demonstrated in 30 patients (93.7%, 30 of 32 patients). Among the patients who did not present fusion, one patient had only one-level fusion failure in the two levels operated. Therefore, overall fusion was noticed in 35 cages (94.5%, 35 of 37 cages).
DISCUSSION
Importance of subsidence assessment
Cage stand-alone technology, as presented by Bagby1), was found on the principle of distraction compression. A sufficiently distracted intervertebral space after discectomy could be stabilized for multidirectional movement by tension forces of residual annulus and ligaments. Cages filled-up with autologous material, allograft or bone substitute would resist disc space collapse and should not migrate until fusion occurred, allowing biological bone healing in an incompressible spacer. In clinical practice6,8,13), distraction with restoration of disc height in degenerative spine increased intervertebral foraminal volume and contributed to nerve root decompression as measured experimentally. But, in vitro study10,21), simulated repeated neck movements caused not only an increase of the flexibility but also subsidence of the implants into the adjacent vertebrae. The relation between flexibility increase and subsidence seemed to depend on the implant design : subsiding threaded cages partially supported spinal stability whereas subsiding impacted cage did not. In the threaded cage group, a large subsidence depth was associated with a small increase in flexibility and a small subsidence depth with a large flexibility increase. But, the impacted cage group showed the inverse behavior. In conclusion, subsidence that occurred in ACDF with impacted cage would be the cause of reduction of intervertebral foraminal volume and instability of cervical spine, which would result in foraminal root compression symptoms, pseudoarthrodesis and failure of stand-alone cage. Therefore, subsidence following ACDF has been a foremost concern ever since development of the surgical procedure.
Why measure the total intervertebral height of the two fused vertebral bodies?
Many reports have described risk factors of subsidence, clinical correlation with subsidence, fusion rate and subsidence rate for the different cages3,9,11,15,20). Although there were many factors known to influence the subsidence, the results of these reports would have deviation and an obser-vational error because of different methods and inaccurate measurement. Several authors3,9,15) decided the degrees of subsidence as the direct measurement of change of the intervertebral disc space height with a reported subsidence rate 29.2% to 55.6%. But, we believe that direct measurement of changes of the intervertebral disc space height does not accurately reflect the degree of subsidence. Because the intervertebral disc space height was reduced not only by subsidence but also by bone growth of upper and lower end plate, subsidence was thought to be overestimated by bone growth in the intervertebral disc space after operation. It is also difficult to obtain accurate measurement of the intervertebral disc space height in case of radio-opaque cages like titanium material. In this regard, others11,20) have measured the subsidence with different methods. They decided the degree of subsidence as the change of the total vertical height of two fused bodies. The measurement of the total vertical height of two fused bodies was more reasonable. But, because of intra-individual variations of the magnification factor in the radiographs, this method was modified for magnification differences by using the anteroposterior diameter of the upper vertebral body on the lateral cervical radiograph17). This method was expressed not in a numerical data but in a ratio data without calculating the quantity of subsidence. Because of these reasons, we aimed to find a proper method for the assessment of subsidence. In this study, proper radiologic assessment was applied to measure the subsidence of the cage. Because our radiographs were made by digital data, we have attempted various methods to find an accurate and relevant method for measurement of subsidence. Among the various attempts, the measurement of TIH and calculation of ΔTIH and CT-MR ΔTIH were chosen for the assessment of subsidence. The method applied in this study was not directed to measure intervertebral disc space height changes. As a result, subsidence was not overestimated by bone growth, and accurate measurement was possible in case of radio-opaque cages. Moreover, TIH was measured on digital radiographs with built-in software, capable of measuring the length to 1/100 mm, this method offers a very accurate numerical data and the process of correction for magnification differences was unnecessary. For this reason, the measurement of TIH was thought to be the most proper method and will avert the pitfall. However, the disadvantage of this method is that the TIH cannot be measured in invisible cases (3 cases) at the lower end-plate of C7 or T1 obscured by the shoulder on the radiograph.
Subsidence of Solis™ cages
In this study, the radiological outcome of 37 Solis™ cages in 32 patients was evaluated with this method after mean follow-up period of 18.9 months. Fusion was achieved in 94.5% at the last follow-up, and subsidence greater than 3 mm was observed in 8.1% of cages. Although clinical analysis for the patients was performed simultaneously with radiologic follow up, only radiological outcome was reviewed in this study in terms of cage subsidence, and the clinical results and assessment will be followed in a separate report. Statistical analysis of subsidence revealed that the subsidence was seen later than 8 weeks after surgery. This is somewhat different from the other results3), which reported that subsidence was seen at 6 weeks postoperatively and progression was not noticed afterward. The authors, however, believe that long term follow-up greater than 8 weeks may be clinically necessary for ACDF with Solis™ cages. Colpan et al.8) reported that cervical intervertebral height and cervical foraminal area significantly increased after cervical ring cage placement but subsidence during the follow-up period negatively affected foraminal area. However, in overall, there was a relative increase of foraminal area and intervertebral height when compared with preoperative values. In this study, as the same result of Colpan et al., there was no negative CT-MR ΔTIH, which represents the postoperative disc space height was more increased than the preoperative disc space height. Moreover, the development of subsidence did not correlate statistically with the change of the postoperative disc space height.
CONCLUSION
ACDF with Solis™ cages was associated with relatively good radiologic long-term results. Fusion was achieved in 94.5% at the last follow-up, and subsidence greater than 3 mm occurred in 8.1% of cages by the new radiologic assessment. Statistic analysis of subsidence reveals that the subsidence seen later than 8 weeks after surgery and the development of this subsidence does not correlate statistically with the change of the postoperative disc space height.
References
- 1.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11:931–934. doi: 10.3928/0147-7447-19880601-13. [DOI] [PubMed] [Google Scholar]
- 2.Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine. 1995;20:1055–1060. doi: 10.1097/00007632-199505000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58:502–508. doi: 10.1227/01.NEU.0000197258.30821.50. discussion 502-508. [DOI] [PubMed] [Google Scholar]
- 4.Brooke NS, Rorke AW, King AT, Gullan RW. Preliminary experience of carbon fibre cage prostheses for treatment of cervical spine disorders. Br J Neurosurg. 1997;11:221–227. doi: 10.1080/02688699746285. [DOI] [PubMed] [Google Scholar]
- 5.Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491–502. doi: 10.1097/00006123-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Chen D, Fay LA, Lok J, Yuan P, Edwards WT, Yuan HA. Increasing neuroforaminal volume by anterior interbody distraction in degenerative lumbar spine. Spine. 1995;20:74–79. doi: 10.1097/00007632-199501000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 8.Colpan ME, Attar A, Sekerci Z, Tuna H, Egemen N. Cervical foraminal area and intervertebral height changes after titanium ring cage placement : preliminary results. J Clin Neurosci. 2006;13:228–232. doi: 10.1016/j.jocn.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 9.Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion : warning. Eur Spine J. 2003;12:513–516. doi: 10.1007/s00586-003-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kettler A, Wilke HJ, Claes L. Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg. 2001;94(1 Suppl):97–107. doi: 10.3171/spi.2001.94.1.0097. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion : preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007;7:205–209. doi: 10.1016/j.spinee.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine. 1999;24:1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 13.Murphy MA, Trimble MB, Piedmonte MR, Kalfas IH. Changes in the cervical foraminal area after anterior discectomy with and without a graft. Neurosurgery. 1994;34:93–96. [PubMed] [Google Scholar]
- 14.Rosenorn J, Hansen EB, Rosenorn MA. Anterior cervical discectomy with and without fusion. A prospective study. J Neurosurg. 1983;59:252–255. doi: 10.3171/jns.1983.59.2.0252. [DOI] [PubMed] [Google Scholar]
- 15.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion : 2-year follow-up study. J Neurosurg Spine. 2006;4:447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 16.Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA. Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion : early technical experience. J Neurosurg Spine. 2005;2:116–122. doi: 10.3171/spi.2005.2.2.0116. [DOI] [PubMed] [Google Scholar]
- 17.Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. J Bone Joint Surg Br. 2003;85:1019–1025. doi: 10.1302/0301-620x.85b7.13398. [DOI] [PubMed] [Google Scholar]
- 18.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003;28:134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 20.van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage : early radiological assessment of fusion and subsidence. Spine J. 2005;5:645–649. doi: 10.1016/j.spinee.2005.07.007. discussion 649. [DOI] [PubMed] [Google Scholar]
- 21.Wilke HJ, Kettler A, Goetz C, Claes L. Subsidence resulting from simulated postoperative neck movements : an in vitro investigation with a new cervical fusion cage. Spine. 2000;25:2762–2770. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]