Abstract
Congenital absence of a cervical spine pedicle is a rare clinical entity, and it is usually found incidentally on radiological studies performed after trauma in patients with cervical pain. We report two cases of congenital absence of a cervical spine pedicle and present a review of the literature.
Keywords: Congenital defects, Cervical vertebrae, Radiography
INTRODUCTION
Absence of a cervical spine pedicle is an unusual congenital anomaly frequently associated with other osseous anomalies and potentially confusing radiologic manifestations, especially in cases of acute trauma5,9,12,14). Thus, it is important to distinguish the absence of a cervical spine pedicle from other clinical entities that require different diagnostic and therapeutic procedures. Approximately 70 cases of this congenital anomaly have been reported in the literature2-5,7-14) since it was first described by Hadley 60 years ago4). Although many cases can be diagnosed by plain radiography, other imaging studies, especially three-dimensional computed tomography (CT), should be performed in order to accurately evaluate the radiological findings.
In the present study, we report two cases of congenital absence of a cervical spine pedicle and present a review of the literature.
CASE REPORT
Case 1
A 47-year-old woman presented with posterior neck pain and right arm pain following a traffic accident. She had no motor deficit and no history of posterior neck pain prior to the accident. Cervical spine X-ray showed an enlarged neural foramen extending from C4 to C5 on the right side, suggesting a traumatic facet fracture-dislocation or spinal tumor (Fig. 1A). However, a three-dimensional CT scan of the cervical spine revealed the absence of the right pedicle and much of the posterior arch of C4 (Fig. 1B, C). The patient was treated conservatively, and her symptoms resolved completely.
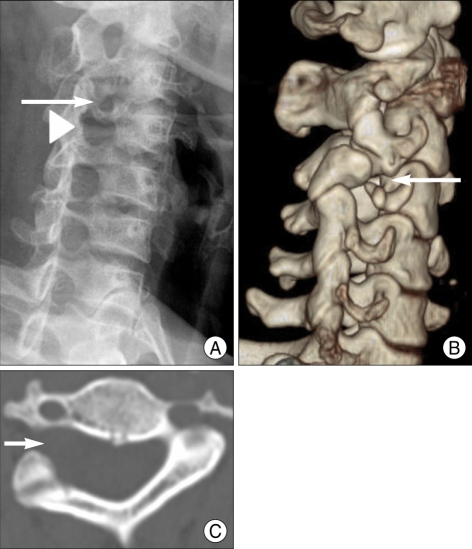
Fig. 1.
Right anterior oblique view (A) showing an enlarged neural foramen at C4/5 (arrowhead) and a relatively small neural foramen at C3/4 (arrow). In addition, cervical spine 3-dimensional computed tomography (B and C) shows the absence of the right C4 pedicle (arrow).
Case 2
A 49-year-old woman presented with neck pain following trauma. Neurological examination revealed normal findings. Cervical spine X-ray suggested a C3 rotational injury (Fig. 2A). A three-dimensional CT scan of the cervical spine showed no evidence of traumatic injury, but the images did reveal the absence of the left pedicle, lateral mass, and lamina of C3 (Fig. 2B). The patient was treated conservatively and eventually became asymptomatic.
Fig. 2.
Simple anterior-posterior radiographs (A) suggesting a C3 rotational injury; however, cervical spine 3-dimensional computed tomography (B) reveals the absence of the left pedicle, lateral mass and lamina of C3 (arrow) and consequently large lateral mass at C4 (arrowhead).
DISCUSSION
Absence of a cervical spine pedicle is an unusual congenital anomaly with potentially confusing clinical and radiological manifestations. Seventy cases of congenital absence of cervical spine pedicles have been reported in the literature to date. The most commonly affected level of the cervical spine is C6 (39%), and this anomaly is almost always unilateral5,11,14). Although neck pain is the most common symptom of congenital absence of a cervical spine pedicle, the finding of an absent cervical spine pedicle is usually incidental and often occurs after trauma9).
Radiographic evaluation of these patients typically begins with conventional radiography but frequently includes CT, myelography, and magnetic resonance imaging (MRI)10). According to Wiener et al.14), this congenital anomaly has several radiographic features including : 1) the false appearance of an enlarged ipsilateral neural foramen owing to the absent pedicle; 2) a dysplastic, dorsally displaced ipsilateral articular pillar and lamina; and 3) a dysplastic ipsilateral transverse process. The spectrum of this anomaly also has included absence of the ipsilateral pillar, absence of the entire ipsilateral neural arch, and other osseous anomalies in more than half of the cases.
In a previous study, Archer et al.1) discussed the embryogenesis of this anomaly, and reported that elements of multiple organs are formed by four weeks of gestation and that organogenesis is completed in eight weeks. The processes involved in the development of the cervical spine, including migration, segmentation and chondrification, take place during this period. Each vertebra has six chondrification centers : two forming the vertebral bodies; two forming the pedicles, lateral masses, and transverse processes; and two forming the lamina and spinous processes. Chondrification centers form by seven weeks, and ossification of the centrum and lamina begins at nine weeks of gestation. Failure of the development of a vertebral chondrification center for the posterior arch of a particular sclerotome or failure of appropriate ossification could lead to the absence of a pedicle. Absent pedicle syndrome results from the failure to develop ventral chondrification centers at seven to eight weeks of gestation1).
The differential diagnosis of an enlarged neural foramen includes dumbbell-shaped spinal tumors, bone tumors, bone erosion by a tortuous or aneurysmal vertebral artery, meningocele, and fracture9). The dysplastic reversed facet may be mistaken for a facet fracture-dislocation in traumatized patients3). Thus, traction reduction therapy has been reported in a significant number of patients before the correct diagnosis is made10). However, careful inspection of cervical spine radiographs with knowledge of the radiologic triads of findings in patients with an absent cervical spine pedicle should allow proper diagnosis in all cases. Fortunately, in our patient, we did not use any traction. If the diagnosis is uncertain, especially in traumatized patients, a three-dimensional CT scan would be useful for evaluating the anomaly8). In our patient, three-dimensional CT scan reconstruction very clearly showed the anatomical structures of an absent cervical spine pedicle, as well as the associated bony anomalies, as previously illustrated in the literature1-2). Since three-dimensional CT scan reconstruction can provide comprehensive images of bony structures, it should be performed in situations in which the diagnosis is uncertain, when possible. It is needless to say that a definite diagnosis of absent cervical pedicle cannot be obtained from MR images alone, though they offer certain information about the content of the enlarged neural foramen.
Conservative nonoperative therapy is recommended for patients with congenital absence of a cervical spine pedicle, as it was successful in most cases.
CONCLUSION
Congenital absence of a cervical spine pedicle is a rare clinical entity. Recognition of this anomaly is important so as not to confuse it with more clinically significant anomalies, such as facet fracture-dislocation, which could result in inappropriate surgical intervention. Initial evaluation with conventional radiography frequently led to misinterpretation, thus three-dimensional computed tomography can help confirm the diagnosis in equivocal cases. Appropriate knowledge and awareness of such an anomaly can prevent inappropriate management.
References
- 1.Archer E, Batnitzky S, Franken EA, Muller J, Hale B. Congenital dysplasia of C2-6. Pediatr Radiol. 1977;6:121–122. doi: 10.1007/BF00973536. [DOI] [PubMed] [Google Scholar]
- 2.Brugman E, Palmers Y, Staelens B. Congenital absence of a pedicle in the cervical spine : a new approach with CT scan. Neuroradiology. 1979;17:121–125. doi: 10.1007/BF00556029. [DOI] [PubMed] [Google Scholar]
- 3.Dimitrov DF, Bronec PR, Friedman AH. Congenitally absent C-7 pedicle presenting as a jumped locked facet. J Neurosurg. 2003;99(2 Suppl):239. doi: 10.3171/spi.2003.99.2.0239. [DOI] [PubMed] [Google Scholar]
- 4.Hadley LA. Congenital absence of pedicle from the cervical vertebra. AJR Am J Roentgenol. 1946;55:193–197. [PubMed] [Google Scholar]
- 5.Hanson EC, Shook JE, Wiesseman GJ, Wood VE. Congenital pedicle defects of the axis vertebra. Report of a case. Spine. 1990;15:236–238. doi: 10.1097/00007632-199003000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Kong DS, Park K, Cho BM, Kim JH. Congenital spondylolisthesis of the sixth cervical vertebra. J Korean Neurosurg Soc. 1999;28:1639–1643. [Google Scholar]
- 7.Mays S. Absent cervical spine pedicle : report of a case in a mediaeval skeleton. Skeletal Radiol. 2007;36:773–777. doi: 10.1007/s00256-007-0276-8. [DOI] [PubMed] [Google Scholar]
- 8.Morales-Cano MD, Vázquez-Saez V, Reus-Pintado M, Climent-Oltra V, Martinez Pérez M. [Congenital absence of a cervical spine pedicle. Incidental finding in patient with cervical pain. Diagnostic approach by helical CT.] Neurocirugia (Astur) 2004;15:476–479. [PubMed] [Google Scholar]
- 9.Rodriguez-Romero R, Vargas-Serrano B, Carro-Mrtinez A. Congenital absence of the neural arch in the cervical spine : an extreme form of pedicle absence. Eur J Radiol. 1995;20:100–104. doi: 10.1016/0720-048x(95)00638-7. [DOI] [PubMed] [Google Scholar]
- 10.Sheehan J, Kaptain G, Sheehan J, Jane J., Sr Cengenital absence of a cervical pedicle : report of two cases and review of the literature. Neurosurgery. 2000;47:1439–1442. [PubMed] [Google Scholar]
- 11.Taguchi Y, Matsuzawa M, Ye JM, Uzura M, Watanabe H, Hayakawa M. Posttraumatic cervical epidural hematoma associated with congenital absence of a cervical spine pedicle : case report and literature review. J Trauma. 2001;51:579–582. doi: 10.1097/00005373-200109000-00030. [DOI] [PubMed] [Google Scholar]
- 12.Tebbal MR, Ben Romdhane MH, Montagne JP, Ducou le Pointe H, Lipszyc H. [What is it? Congenital absence of the left pedicle of C7 vertebra.] J Radiol. 1998;79:1509–1512. [PubMed] [Google Scholar]
- 13.van Dijk Azn R, Thijssen HO, Merx JL, Lemmens JA, Wackenheim A. The absent pedicle syndrome. Neuroradiology. 1987;29:69–72. doi: 10.1007/BF00341041. [DOI] [PubMed] [Google Scholar]
- 14.Wiener MD, Martinez S, Forsberg DA. Congenital absence of a cervical spine pedicle : clinical and radiologic findings. AJR Am J Roentgenol. 1990;155:1037–1041. doi: 10.2214/ajr.155.5.2120932. [DOI] [PubMed] [Google Scholar]