Abstract
Lateral femoral cutaneous neuropathy occurring during spinal surgery is frequently related to iliac bone graft harvesting, but meralgia paresthetica (MP) can result from the patient being in the prone position. Prone position-related MP is not an uncommon complication after posterior spine surgery but there are only few reports in the literature on this subject. It is usually overlooked because of its mild symptoms and self-limiting course, or patients and physicians may misunderstand the persistence of lower extremity symptoms in the early postoperative period to be a reflection of poor surgical outcome. The authors report a case of prone position-related MP after posterior lumbar interbody fusion at the L3-4 and reviewed the literature with discussion on the incidence, pathogenesis, and possible risk factors related to this entity.
Keywords: Meralgia paresthetica (MP), Lateral femoral cutaneous nerve (LFCN), Prone position, Posterior spinal surgery
INTRODUCTION
Meralgia paresthetica (MP) is a neuropathy resulting from compression of the lateral femoral cutaneous nerve (LFCN) as it crosses between the anterior superior iliac spine (ASIS) and the inguinal ligament, while entering the thigh4,9).
LFCN neuropathy occurring during spinal surgery is frequently related to iliac bone graft harvesting, but MP can occur de novo as a transient compression neuropathy resulting from placing the patient in a prone position for spinal surgery5,7,9,13). Prone position-related MP is not an uncommon occurrence in patients who have undergone posterior spine surgery, but there are only few reports in the literature on this subject5,7,13).
We report a case of prone position-related MP after posterior lumbar interbody fusion (PLIF) at the L3-L4 level with review of the literature and discussion on the incidence, pathogenesis, and possible risk factors related to this entity.
CASE REPORT
A 51-year-old female presented with several months history of low back pain and referred pain to her buttock and thigh. She was treated with various non-operative measures, but her pain became more intense over the course of the treatment period. Her height was 160 cm, and her body weight was 61 kg. Radiographs of the lumbar spine demonstrated spondylolisthesis with dynamic instability at the L3-L4 level. Magnetic resonance images demonstrated lumbar stenosis at that level. Instrumented PLIF was performed, with pedicle screws and two intervertebral cages filled with artificial bone chips. Intraoperative blood loss was 500 cc, and operative time was recorded as 270 min.
Postoperatively, the patient complained of unpleasant paresthesia and burning sensation over the anterior aspect of the right thigh. Neurological examination revealed hypesthesia of the right anterior thigh, with no motor weakness. We initially considered the possibility of right L3 nerve root injury caused by pedicle screw misplacement, but postoperative plain radiography and computed tomography of the lumbar spine demonstrated proper positioning of the pedicle screws and the right-sided intervertebral cage (Fig. 1). The day after surgery, the patient noted increased sensitivity to clothing. She was able to partially alleviate the burning sensation by rubbing or massaging her right thigh. She was not able to sit for a few minutes because of aggravation of the burning sensation in the right thigh. She had to alternate between sitting and standing multiple times during meals. She also noted a tender point near the right ASIS, where pressure reproduced the burning sensation. We considered the possibility of MP secondary to compression of the LFCN near the ASIS, possibly caused by the pelvic bolster placed under the ASIS during surgery in the prone position. Oral nonsteroidal anti-inflammatory drug (NSAID) and gabapentin were administered, but the patient's symptom persisted.
Fig. 1.
Postoperative simple lateral radiograph of lumbar spine (A), axial computed tomography scans of the L3 pedicle (B), intervertebral cages (C), and L4 pedicle (D) reveal no violation of the medial wall of pedicle by the pedicle screws and proper position of the right-sided intervertebral cage.
Two weeks after surgery, an electrodiagnostic study was conducted to determine if there was nerve injury. No waves were found on nerve conduction study or sensory evoked potential studies of the right LFCN. Needle electromyography studies revealed no definite evidence of denervation in the vastus lateralis, vastus medialis, iliopsoas, or adductor magnus muscles. We diagnosed the patient with the right LFCN entrapment neuropathy at the level of the ASIS, without lumbar radiculopathy, on the basis of the electrodiagnostic study results.
The patient's symptoms were partially relieved after injection of a local anesthetic and steroid at the point of tenderness. With continued NSAID and gabapentin, her symptoms almost completely subsided by 6 months after surgery.
DISCUSSION
The LFCN is formed from the L2 and L3 spinal nerve roots and travel along the posterolateral aspect of the psoas major muscle, crossing the ilium toward the ASIS8). Compression of the LFCN may occur at the level of the L2 and L3 roots as a result of upper lumbar disk herniation, or tumor in the second lumbar vertebra10,11). The LFCN may also be compressed along its retroperitoneal course by space-occupying lesions, such as tumors, or by retraction of the psoas muscle during a retroperitoneal procedure1,7). Abnormal posture, persistent regional muscle spasm, tight-fitting braces or corsets, and thigh injuries are other sources of impingement on the LFCN6). LFCN neuropathy occurring during spinal surgery is frequently related to iliac bone graft harvesting but MP can occur de novo as a transient compression neuropathy resulting from prone positioning of the patient during spinal surgery5,7,9,13).
Variability exists in the course of the LFCN, its relation to the ASIS, and its exit point. Aszmann et al. observed that in 5 of the 9 dissected cadaver, the exit of the nerve was more than 1 cm away from the ASIS, and Murata et al. found that LFCN may cross over the iliac crest more than 2 cm away from the ASIS2,8). De Ridder et al. found abnormal anatomy in 26% of cadavers3). The nerve is most vulnerable and susceptible to compression and entrapment at its exit point2). Prone position-related MP is not an uncommon occurrence in patients who have undergone posterior spine surgery, but there are few reports in the literature on this subject (Table 1).
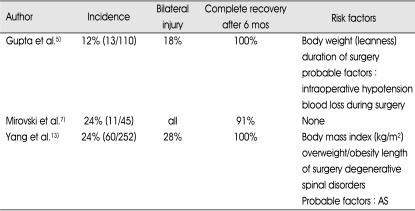
Table 1.
Prone position-related meralgia paresthetica after posterior lumbar surgery in the literature
mos : months, AS : ankylosing spondylitis
The reported incidence of prone position-related MP after posterior spinal surgery was as high as 24%. Unilateral MP was more frequent, although Mirovski et al. reported MP in 11 of 45 patients who underwent posterior spinal procedures, mainly fusions without iliac bone graft harvesting, on four-post Hall-Relton frame and all the 11 patients showed bilateral MP5,7,13). Asymmetric positioning may cause excessive compression near one ASIS and may cause unilateral involvement of the LFCN. If the distance between two pelvic posts, supports, or bolsters is not wide enough, excessive compression will be generated near both ASIS and may cause bilateral MP13). Statistically significant risk factors related to the development of prone position-related MP are surgery longer than 3.5 hours and degenerative spinal disorders related to mild preexisting damage to the second or third lumbar roots caused by degenerative intervertebral disks or hypertrophic facet joint13). Probable risk factors are ankylosing spondylitis, intraoperative hypotension and significant blood loss during surgery5,13). There are conflicting opinions about patient body weight as it relates to prone position-related MP risk. Yang et al. reported that overweight/obese patients and those with greater body mass index (BMI) [calculated by the formula : body weight (kg)/height (m)2] had a significantly higher incidence of prone position-related MP. In the prone position, the abdominal wall distends downward because of the weight of the viscera and an abundance of subcutaneous fat. As the LFCN courses between the two laminae of the iliac fascia, the downward distension of the abdominal wall can stretch the anterior lamina, which is firmly attached to the muscles of the anterior abdominal wall, and increase compression of the LFCN. This compression effect is more significant in overweight and obese patients13). However, Gupta et al. reported a higher incidence of prone position-related MP in thinner individuals, supporting the theory of direct compression of the LFCN in the prone position5).
In our patient, operative time was 4 hours. She had spondylolisthesis and stenosis at the L3-L4 level, which was probably related to chronic damage to the L3 nerve root. Intraoperative blood loss was not insignificant (500 cc). Her BMI was 23.8 kg/m2, which was within normal limit according to the report by WHO expert consultation12). Longer surgical time, probably chronic damage to the L3 root, significant intraoperative blood loss and asymmetric positioning might have led to the unilateral prone position-related MP in our patient.
Although prone position-related MP is not uncommon occurrence after posterior spine surgery, it is usually overlooked because the sensory impairment is not always severe and recovery is usually rapid and complete as in the literature reviewed5,7,13). The condition is usually self-limiting and does not require any specific treatment. Nevertheless, it is sometimes associated with severe pain, paresthesias, burning sensation, and restriction of daily living, as was seen in our patient. Patients and physicians may misunderstand the persistence of lower extremity symptoms in the early postoperative period to be a reflection of poor surgical outcome. MP is frequently misdiagnosed and may be mistakenly attributed to surgical sequelae, as in our case. As soon as MP is suspected, it can be diagnosed or excluded through electrophysiological studies of the LFCN and can be treated with medication, physiotherapy, local steroid/anesthetic injection, or nerve decompression surgery9).
CONCLUSION
Although prone position-related MP is not an uncommon complication after posterior spine surgery, it is usually overlooked because of its mild symptoms and self-limiting course. Nevertheless, it is sometimes associated with severe burning sensation and restriction of daily living, and may be mistakenly attributed to surgical sequelae or poor surgical outcome, as in our patient. To decrease the incidence of prone position-related MP, certain preoperative cautions should be observed. The patient should be positioned symmetrically, with smaller bolsters under the ASIS and adequate distance between the two pelvic posts, supports, or bolsters. Every effort should be made to reduce the length of surgery, minimize intraoperative blood loss, and avoid hypotension during surgery.
References
- 1.Amoiridis G, Wöhrle J, Grunwald I, Przuntek H. Malignant tumour of the psoas : another cause of meralgia paraesthetica. Electromyogr Clin Neurophysiol. 1993;33:109–112. [PubMed] [Google Scholar]
- 2.Aszmann OC, Ebmer JM, Dellon AL. The anatomic basis for the innervated mylohyoid/digastric flap in facial reanimation. Plast Reconstr Surg. 1998;102:369–372. doi: 10.1097/00006534-199808000-00010. [DOI] [PubMed] [Google Scholar]
- 3.de Ridder VA, de Lange S, Popta JV. Anatomical variations of the lateral femoral cutaneous nerve and the consequences for surgery. J Orthop Trauma. 1999;13:207–211. doi: 10.1097/00005131-199903000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Dias Filho LC, Valença MM, Guimaräes Filho FA, Medeiros RC, Silva RA, Morais MG, et al. Lateral femoral cutaneous neuralgia : an anatomical insight. Clin Anat. 2003;16:309–316. doi: 10.1002/ca.10106. [DOI] [PubMed] [Google Scholar]
- 5.Gupta A, Muzumdar D, Ramani PS. Meralgia paraesthetica following lumbar spine surgery : a study in 110 consecutive surgically treated cases. Neurol India. 2004;52:64–66. [PubMed] [Google Scholar]
- 6.Lorei MP, Hershman EB. Peripheral nerve injuries in athletes. Treatment and prevention. Sports Med. 1993;16:130–147. doi: 10.2165/00007256-199316020-00005. [DOI] [PubMed] [Google Scholar]
- 7.Mirovsky Y, Neuwirth M. Injuries to the lateral femoral cutaneous nerve during spine surgery. Spine. 2000;25:1266–1269. doi: 10.1097/00007632-200005150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000;82:746–747. doi: 10.2106/00004623-200005000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Nouraei SA, Anand B, Spink G, O'Neill KS. A novel approach to the diagnosis and management of meralgia paresthetica. Neurosurgery. 2007;60:696–700. doi: 10.1227/01.NEU.0000255392.69914.F7. discussion 700. [DOI] [PubMed] [Google Scholar]
- 10.Rinkel GJ, Wokke JH. Meralgia paraesthetica as the first symptom of a metastatic tumor in the lumbar spine. Clin Neurol Neurosurg. 1990;92:365–367. doi: 10.1016/0303-8467(90)90067-f. [DOI] [PubMed] [Google Scholar]
- 11.Trummer M, Flaschka G, Unger F, Eustacchio S. Lumbar disc herniation mimicking meralgia paresthetica : case report. Surg Neurol. 2000;54:80–81. doi: 10.1016/s0090-3019(00)00264-0. [DOI] [PubMed] [Google Scholar]
- 12.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 13.Yang SH, Wu CC, Chen PQ. Postoperative meralgia paresthetica after posterior spine surgery : incidence, risk factors, and clinical outcomes. Spine. 2005;30:E547–E550. doi: 10.1097/01.brs.0000178821.14102.9d. [DOI] [PubMed] [Google Scholar]