Abstract
Primary intracranial squamous cell carcinoma is extremely rare, with most cases arising from a preexisting benign epidermoid cyst. We report a rare case of primary intracranial squamous cell carcinoma in the brain stem with a cerebellopontine angle (CPA) epidermoid cyst. A 72-year-old female suffered from progressive left hemiparesis, difficulty in swallowing, and right hemifacial numbness. Diffusion-weighted magnetic resonance imaging revealed a high signal intensity (SI) lesion in the CPA region and an intra-axially ring-enhanced cystic mass in the right brain stem with low SI. Whole-body positron emission tomography showed no evidence of metastatic disease. The histological findings revealed a typical epidermoid cyst in the CPA region and a squamous cell carcinoma in the brain stem. We speculate that the squamous cell carcinoma may have been developed due to a chronic inflammatory response by the adjacent epidermoid cyst. The patient underwent a surgical resection and radiotherapy. After 12 months, she had no evidence of recurrence.
Keywords: Squamous cell carcinoma, Epidermoid cyst, Brain stem, Cerebellopontine angle
INTRODUCTION
Intracranial epidermoid cysts are histologically benign and slow growing congenital neoplasms. They account for only 0.2 to 1.8% of all intracranial tumors5,13,15). Primary intracranial squamous cell carcinomas are extremely rare and usually arise from malignant transformation of benign intracranial epidermoid and dermoid cysts6,7,9,12,16). They are most commonly found in close proximity to the precursor lesions, with most reported cases involving the cerebellopontine angle (CPA). The CPA is also the preferential site for epidermoid cysts7,16). This report describes a rare case of primary intracranial squamous cell carcinoma in the brain stem with a CPA epidermoid cyst. We describe its clinical, radiological, operative, and pathological features.
CASE REPORT
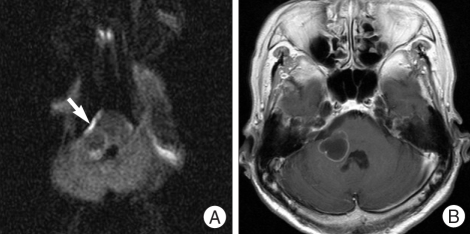
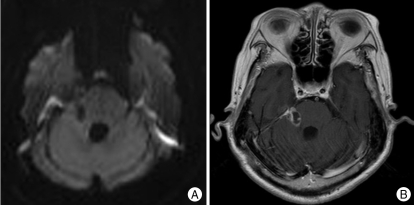
A 72-year-old female presented with progressive right hemifacial sensory loss. Diffusion-weighted magnetic resonance imaging (MRI) revealed a high signal intensity (SI) lesion in the right CPA region, and a low SI lesion in the adjacent brain stem. A T1-weighted gadolinium-enhanced MRI showed an intra-axial ring-enhanced mass in the brain stem. After 2 months, a left hemiparesis was developed and a follow-up MRI revealed that the brain stem lesion was larger than before. The lesion was compressing both the brain stem and cerebellum (Fig. 1A, B).
Fig. 1.
A: Preoperative axial diffusion-weighted magnetic resonance image showing high signal intensity at the right cerebellopontine angle lesion (white arrow). B: Axial T1-weighted MR gadolinium-enhanced image showing an intra-axial ring-enhanced mass on the right brain stem.
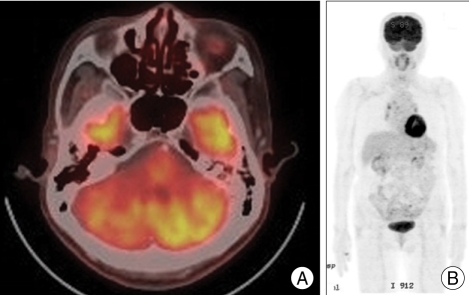
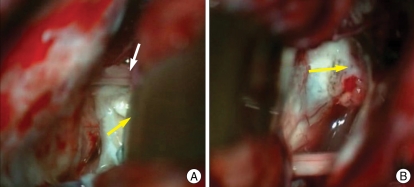
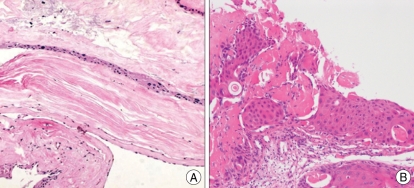
After a whole-body positron emission tomography scan confirmed the absence of metastasis, a surgical resection was performed (Fig. 2). Intraoperatively, the CPA mass appeared to be a typical epidermoid cyst. It connected to the intra-axial mass of the brain stem. The CPA epidermoid cyst was completely and easily removed. However, the cystic wall of intra-axial tumor was relatively firm and could not be completely resected due to its adhesion with the cerebellum and brain stem (Fig. 3). Thus, the cystic wall was partially removed, and a yellowish clear fluid was drained. Histological findings of the CPA epidermoid cyst showed multiple layers of squamous epithelial lining and keratinization, entirely consistent with a benign epidermoid cyst (Fig. 4A). Meanwhile, the histological findings of the brain stem tumor showed an atypical cyst with a squamous epithelial lining and pleomorphic nuclei (Fig. 4B). After surgical resection, the left hemiparesis and difficulty in swallowing were improved. The patient received intensity-modulated radiotherapy (IMRT) with a total dose of 5,400 cGy in 30 fractions. After 12 months, the tumor has remained stable according to follow-up MRI. This leads us to believe that local tumor control has been working (Fig. 5).
Fig. 2.
Preoperative positron emission tomograpy images showing a hypometabolic state at the cerebellar peduncle and no definite hypermetabolic lesion that suspects the metastatic lesion in the whole body.
Fig. 3.
(A) Intraoperative findings showing a typical epidermoid cyst (yellow arrow) and VII and VIII cranial nerve complex (white arrow), and (B) an adhesive and infiltrative malignant cyst on the brain stem (yellow arrow) after the rupture of the cyst.
Fig. 4.
A: Histopathological finding showing multiple layers of squamous epithelium lining and keratinization consistent with a benign epidermoid cyst (H&E, × 100). B: The cyst contains high cellular area with enlarged pleomorphic and hyperchromatic nuclei, which is a component of poorly differentiated squamous cell carcinoma (H&E, × 100).
Fig. 5.
A: Axial diffusion-weighted magnetic resonance (MR) image obtained one year after operation and radiotherapy reveals that the right cerebellopontine angle epidermoid cyst has been totally removed. B: Axial T1-weighted MR gadolinium-enhanced image reveals that the remaining tumor is stable.
DISCUSSION
Intracranial epidermoid cysts are well-differentiated cystic lesions along the cistern. These tumors are thought to arise between the third and fifth week of embryonic development if squamous epithelial remnants are included in the neural tube when the neural tube separates from the ectoderm2). Intracranial squamous cell carcinoma can develop from metastasis, direct extension from the cranial base and malignant transformation of a benign cyst. However, most cases of primary intracranial squamous cell carcinoma derive from an epidermoid cyst. Hamlat et al.8) have reviewed the mechanisms of malignant transformation of benign epidermoid cysts. In general, these mechanisms of this transformation remain unclear. Some potential mechanisms include a chronic inflammatory response due to repeated cystic rupture, or a subtotal resection of the cystic wall1).
Primary intracranial squamous cell carcinomas have been classified into five groups9). These five groups include an initial malignant transformation of an epidermoid cyst, malignant transformation from a remnant epidermoid cyst, malignant transformation with leptomeningeal carcinomatosis, squamous cell carcinoma from other benign cysts, and other malignancies arising from the benign cysts6). According to these classifications and mechanisms, we postulate that our case can be classified as the initial malignant transformation of an epidermoid cyst due to a chronic inflammatory stimulation caused by repeated cystic rupture. On MRI, the SI of the benign epidermoid cyst is generally similar to that of cerebrospinal fluid, which shows a very low signal on T1-weighted images and a very high signal on T2-weighted images4). Usually, diffusion-weighted imaging (DWI) enables one to distinguish epidermoid cysts from the brain parenchyma and surrounding cerebrospinal fluid spaces10,17). Nawashiro et al.14) have reported the differences between a benign epidermoid cyst and malignant transformation on DWI. According to this report, benign epidermoid cysts have a very high SI on DWI, while a highly malignant transformation has a low SI on DWI and a ring-like enhancement on T1-weighted gadolinium-enhanced MRI. Similarly, our patient had shown a low SI and ring-enhanced lesion in the brain stem and a high SI lesion in the CPA simulatneouly. Based on this finding, we speculate that primary intracranial squamous cell carcinoma originates from malignant transformation of the epidermoid cyst. Primary intracranial squamous cell carcinoma arising from malignant transformation of the benign epidermoid cyst is shown by enhancement on MRI after administering contrast medium and by rapid growth13,15,16). In our case, MRI revealed a rapidly growing lesion with the capsular enhance ment at the cerebellum and pons. These findings suggest a malignant tumor.
Pathologic findings of malignant epidermoid cysts include cytological atypia and stromal invasion. Many reports describe a benign epidermoid cyst as having multiple keratin debris, squamous epithelium and lacking malignant cells3,16). Meanwhile, primary intracranial squamous cell carcinomas have poorly differentiated abnormal cells with pleomorphic nuclei10,12). Our case involved an atypical cyst lined by squamous epithelial cells. This squamous cell epithelium could not be seen on the neoplasm of the central nervous system.
The complete surgical removal of the squamous cell carcinoma of the brain stem is limited because the tumor adheres strongly to the brain parenchyma, cerebral vessels, and particularly the brain stem. Thus, aggressive removal of the tumor may cause severe neurological deficit16). Radiotherapy is recommended as a palliative treatment for residual squamous cell carcinoma after surgical resection. The survival rate is increased in those receiving radiotherapy compared to those who have no further palliative treatment following the surgery9,15). In our case, subtotal removal of the tumor was performed along with the postoperative IMRT for the residual mass in the brain stem. After adjuvant therapy, disease has not progressed for 12 months.
The modalities of adequate chemotherapy have been examined in various studies, but the effectiveness remains uncertain9). Recently, stereotactic radiosurgery has also been used in some cases with good survival benefits11,16). We have reported a rare case of primary intracranial squamous cell carcinoma in the brain stem with a CPA epidermoid cyst. We speculate that this squamous cell carcinoma may have developed due to a chronic inflammatory response by the adjacent epidermoid cyst. The combination of subtotal resection and radiotherapy may be useful for local tumor control. However, longer follow-up periods with more patients are needed to fully validate the efficacy of these treatments.
CONCLUSION
Primary intracranial squamous cell carcinomas should be considered in the differential diagnosis of a cystic lesion in the brain stem with a CPA epidermoid cyst. Aggressive attempts to remove squamous cell carcinoma in the brain stem can result in significant morbidity and mortality. In our case, IMRT after subtotal resection appears to have provided good tumor control. Therefore, radiotherapy for residual squamous cell carcinoma is likely to be a good adjuvant treatment.
References
- 1.Abramson RC, Morawetz RB, Schlitt M. Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery. 1989;24:574–578. doi: 10.1227/00006123-198904000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Acciarri N, Padovani R, Foschini MP, Giulioni M, Finizio FS. Intracranial squamous cell carcinoma arising in an epidermoid cyst. Br J Neurosurg. 1993;7:565–569. doi: 10.3109/02688699308995081. [DOI] [PubMed] [Google Scholar]
- 3.Fiume D, Gazzeri G, Spallone A, Santucci N. Epidermoid cysts of the fourth ventricle. Surg Neurol. 1988;29:178–182. doi: 10.1016/0090-3019(88)90002-x. [DOI] [PubMed] [Google Scholar]
- 4.Fujita N, Hirabuki N, Kashiwagi N, Watanabe Y, Nakamura H. Epidermoid tumor of the cerebellopontine angle: signal loss in the contralateral cistern. AJNR Am J Neuroradiol. 1998;19:333–335. [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia CA, McGarry PA, Rodriguez F. Primary intracranial squamous cell carcinoma of the right cerebellopontine angle. J Neurosurg. 1981;54:824–828. doi: 10.3171/jns.1981.54.6.0824. [DOI] [PubMed] [Google Scholar]
- 6.Goldman SA, Gandy SE. Squamous cell carcinoma as a late complication of intracerebroventricular epidermoid cyst. Case report. J Neurosurg. 1987;66:618–620. doi: 10.3171/jns.1987.66.4.0618. [DOI] [PubMed] [Google Scholar]
- 7.Guan LM, Qi XX, Zhang JR, Xu K, Cui LJ, Zhang Q. Intracranial squamous cell carcinoma developing in remnant of an epidermoid cyst: case report and literature review. Chin Med J (Engl) 2004;117:1880–1883. [PubMed] [Google Scholar]
- 8.Hamlat A, Hua ZF, Saikali S, Egreteau J, Guegan Y. Malignant transformation of intracranial epidermoid cyst with leptomeningeal carcinomatosis: case report. Acta Neurol Belg. 2003;103:221–224. [PubMed] [Google Scholar]
- 9.Hamlat A, Hua ZF, Saikali S, Laurent JF, Gedouin D, Ben-Hassel M, et al. Malignant transformation of intra-cranial epithelial cysts: systematic article review. J Neurooncol. 2005;74:187–194. doi: 10.1007/s11060-004-5175-4. [DOI] [PubMed] [Google Scholar]
- 10.Kodama H, Maeda M, Hirokawa Y, Suzuki H, Hori K, Taki W, et al. MRI findings of malignant transformation of epidermoid cyst: case report. J Neurooncol. 2007;82:171–174. doi: 10.1007/s11060-006-9255-5. [DOI] [PubMed] [Google Scholar]
- 11.Link MJ, Cohen PL, Breneman JC, Tew JM., Jr Malignant squamous degeneration of a cerebellopontine angle epidermoid tumor. Case report. J Neurosurg. 2002;97:1237–1243. doi: 10.3171/jns.2002.97.5.1237. [DOI] [PubMed] [Google Scholar]
- 12.Michael LM, 2nd, Moss T, Madhu T, Coakham HB. Malignant transformation of posterior fossa epidermoid cyst. Br J Neurosurg. 2005;19:505–510. doi: 10.1080/02688690500495356. [DOI] [PubMed] [Google Scholar]
- 13.Mori Y, Suzuki Y, Tanasawa T, Yoshida J, Wakabayashi T, Kobayashi T. [A case report of epidermoid carcinoma in the cerebellopontine angle] No Shinkei Geka. 1995;23:905–909. [PubMed] [Google Scholar]
- 14.Nawashiro H, Higo R, Tokumaru AM, Tsuzuki N, Shima K. Diffusion-weighted MRI of an intracranial epidermoid with malignant transformation. Neuroradiology. 2001;43:891. doi: 10.1007/s002340100612. [DOI] [PubMed] [Google Scholar]
- 15.Nishio S, Takeshita I, Morioka T, Fukui M. Primary intracranial squamous cell carcinomas: report of two cases. Neurosurgery. 1995;37:329–332. doi: 10.1227/00006123-199508000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Tamura K, Aoyagi M, Wakimoto H, Tamaki M, Yamamoto K, Yamamoto M, et al. Malignant transformation eight years after removal of a benign epidermoid cyst: a case report. J Neurooncol. 2006;79:67–72. doi: 10.1007/s11060-005-9117-6. [DOI] [PubMed] [Google Scholar]
- 17.Uchino A, Hasuo K, Matsumoto S, Uda K, Moriguchi M, Nishio T, et al. Intracranial epidermoid carcinoma: CT and MRI. Neuroradiology. 1995;37:155–158. doi: 10.1007/BF00588635. [DOI] [PubMed] [Google Scholar]