Abstract
The filoviruses Ebola and Marburg are zoonotic agents that are classified as both biosafety level 4 and category A list pathogens. These viruses are pathogenic in humans and cause isolated infections or epidemics of viral hemorrhagic fever, mainly in Central Africa. Their natural reservoir has not been definitely identified, but certain species of African bat have been associated with Ebola and Marburg infections. Currently, there are no licensed options available for either treatment or prophylaxis. Different animal models have been developed for filoviruses including mouse, guinea pig and nonhuman primates. The ‘gold standard’ animal models for pathogenesis, treatment and vaccine studies are rhesus and cynomolgus macaques. This article provides a brief overview of the clinical picture and the pathology/pathogenesis of human filovirus infections. The current animal model options are discussed and compared with regard to their value in different applications. In general, the small animal models, in particular the mouse, are the most feasible for high biocontainment facilities and they offer the most options for research owing to the greater availability of immunologic and genetic tools. However, their mimicry of the human diseases as well as their predictive value for therapeutic efficacy in primates is limited, thereby making them, at best, valuable initial screening tools for pathophysiology, treatment and vaccine studies.
Research problem
Ebola virus (EBOV) and Marburg virus (MARV) infections cause a severe form of viral hemorrhagic fever (VHF) with lethality in humans ranging from 23–90% depending on the virus species and strain (Sanchez et al., 2007). Given the high virulence in humans and the classification of these viruses as biosafety level 4 and category A list pathogens, animal models are crucial for understanding the underlying mechanisms of disease, as well as for the development of therapeutics and vaccines. Furthermore, for biothreat agents, where studies of clinical effectiveness in humans are impossible, the new FDA animal rule comes into place when demonstrating efficacy in animal models that resemble human cases and for which the natural history of the particular disease is fully understood [http:www.fda.gov/cder/guidance/8324concept.pdf].
The ‘gold standard’ animal model for EBOV and MARV is the nonhuman primate (NHP) because these are the only animals that are lethally infected with nonadapted human isolates and the resulting pathology is close to that described in humans (Sanchez et al., 2007). However, owing to ethical, practical and expense issues in dealing with NHPs, small animal models have had to be created. Small animal models have been developed for Zaire ebolavirus (ZEBOV) and Lake Victoria marburgvirus (LVMARV) through serial passaging in both mice and guinea pigs. This adaptation process is necessary because wild-type virus induces no discernible pathology in these small animals. The pathogenesis of the adapted rodent strains differs in many aspects but similarities to the disease in primates have also been demonstrated (Table 1). Nevertheless, the rodent models are the first choice for in vivo, efficacy screening studies for therapeutics and vaccines. However, their predictive value for efficacy in primates is limited (Geisbert et al., 2002). There are currently no adequate small animal models for the remaining EBOV species [Sudan ebolavirus (SEBOV), Cote d’Ivoire ebolavirus (CIEBOV) and Reston ebolavirus (REBOV)] (Feldmann et al., 2005a).
Table 1.
Infection in animal models and humans
| Mouse (wt) | Mouse (ad)* | Guinea pig (wt) | Guinea pig (ad) | NHP (wt) | Human (wt) | |
|---|---|---|---|---|---|---|
| Viremia | Low | High | Low | High | High | High |
| Virulence | Low | High | Low | High | High | High |
| Primary cell tropism | Unknown | MPC | Unknown | MPC | MPC | MPC |
| Macular rush | No | No | No | No | Yes | Yes |
| Coagulation abnormalities | No | Not profound | No | Some | Yes | Yes |
| Liver enzymes | Unknown | Elevated | Unknown | Elevated | Elevated | Elevated |
| Thrombocytopenia | Unknown | Yes | Unknown | Yes | Yes | Yes |
| Lymphocyte apoptosis | Unknown | Yes | Unknown | Limited | Yes | Yes |
| Proinflammatory cytokine response | Unknown | Yes | Unknown | Yes | Yes | Yes |
MPC= mononuclear phagocytic cell; ad=adapted strain; wt=wild-type strain;
Ebola virus only. [Table altered from Stroeher and Feldmann (Stroeher and Feldmann, 2006).]
Filoviral hemorrhagic fever
Clinical presentation
Following an incubation period of 2–21 days, human EBOV and MARV infections normally show an abrupt disease onset that is characterized by flu-like symptoms (fever, chills, malaise and myalgia). The subsequent signs and symptoms indicate multi-system involvement, including systemic (prostration, lethargy), gastrointestinal (anorexia, nausea, vomiting, abdominal pain, diarrhea), respiratory (chest pain, shortness of breath, cough), vascular (conjunctival injection, postural hypotension, edema) and neurologic (headache, confusion, seizure, coma) manifestations. Hemorrhagic manifestations may develop during the peak of the illness and include petechiae, ecchymoses, uncontrolled bleeding from venipuncture sites, epistaxis and other mucosal hemorrhages, and postmortem evidence of visceral hemorrhagic effusions. In addition, there is often a maculopapular rash associated with varying degrees of erythema and desquamation. In late stages of the disease, shock, convulsions, severe metabolic disturbances and diffuse coagulopathy occur. Fatal cases develop clinical signs early during infection and demise typically occurs in the second week, mainly as a result of the consequences of hypovolemic shock. Fever is present in nonfatal cases for about 5–9 days and improvement typically coincides with when the antibody response is noted (days 7–11). Convalescence is prolonged and sometimes associated with myelitis, recurrent hepatitis, psychosis or uveitis (for reviews, see Martini and Siegert, 1971; Pattyn, 1978; Peters and LeDuc, 1999; Feldmann et al., 2003; Sanchez et al., 2007).
Pathogenesis
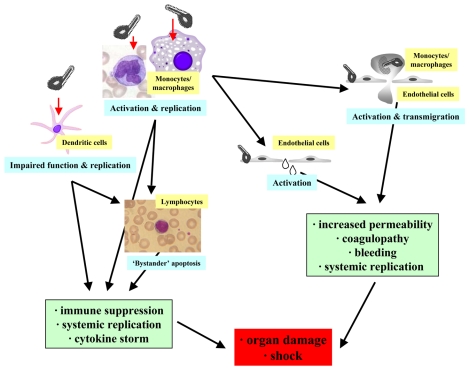
In general terms, human VHF resulting from EBOV and MARV infections is associated with fluid distribution problems, hypotension and coagulation disorders, and often leads to fulminant shock and subsequent multiorgan system failure (Fig. 1). Viral replication, in conjunction with immune and vascular dysregulation, is thought to play a role in disease development. Specific organ involvement includes extensive disruption of the parafollicular regions in the spleen and lymph nodes, and proliferation of the virus in mononuclear phagocytic cells has been demonstrated. A dramatic lymphopenia is thought to be the result of ‘bystander apoptosis’, most likely triggered through either mediators released from virus-activated primary target cells or by as yet unidentified interactions between host and viral products. In contrast to the activation of monocytes/macrophages, infected dendritic cells were impaired in the secretion of pro-inflammatory cytokines, the production of co-stimulatory molecules and the stimulation of T cells. The ability of filoviruses to interfere with the host innate immune system, especially the interferon (IFN) response, has been attributed to the virion proteins (VP) 35 and VP24. Overall, EBOV and MARV infections clearly affect the innate immune response but with obvious varying outcomes. In particular, the presence of IL-1β and elevated levels of IL-6 during the early symptomatic phase of the disease have been suggested as blood markers for survival, whereas the release of IL-10 and high levels of neopterin and IL-1 receptor antagonist (IL-1RA) during the early stage of disease are more indicative of fatal outcomes (for reviews, see Feldmann et al., 2003; Sullivan et al., 2003; Geisbert and Hensley, 2004; Geisbert and Jahrling, 2004; Mohamadzadeh et al., 2007; Sanchez et al., 2007).
Fig. 1.
Ebola virus pathogenesis. The final event in severe/lethal cases of Ebola infection is shock, which is caused by several processes that influence each other: systemic viral replication, immune suppression, an increase in vascular permeability and coagulopathy. Infection of primary target cells such as monocytes/macrophages and dendritic cells results in the systemic spread of the virus and differential activation. Monocytes/macrophages are activated to produce pro-inflammatory cytokines and tissue factor, whereas dendritic cell activation is impaired, leading to poor protective immune responses. Although the virus does not infect lymphocytes and natural killer (NK) cells, there is extensive apoptosis in subsets of these cell types. Endothelial cells are activated by pro-inflammatory cytokines and virus particles, leading to increased permeability. Tissue factor expression in monocytes/macrophages induces coagulopathy, which is also able to increase inflammation.
The disturbance of the blood-tissue barrier, which is controlled primarily by endothelial cells, is another important factor in pathogenesis (Fig. 1). The endothelium seems to be affected directly by virus activation and lytic replication, as well as indirectly by an inflammatory response through mediators derived from primary target cells or viral expression products. These processes might explain the imbalance of fluid between the intravascular and extravascular tissue space that is observed in patients. Clinical and laboratory data also indicate disturbances in hemostasis during infection. Although thrombocytopenia is observed with severe infections in primates, studies on the role of disseminated intravascular coagulation (DIC) and consumption coagulopathy, as well as platelet and endothelial dysfunctions, are still incomplete. DIC can be observed regularly in primates and seems to be triggered by widespread endothelial cell injury as well as the release of tissue factor or thromboplastic substances (for reviews, see Feldmann et al., 2003; Sanchez et al., 2007; Aleksandrowicz et al., 2008).
Case study.
Marburg hemorrhagic fever: a 42-year-old man fell ill with fever, headache and conjunctivitis which lasted 10, 5 and 4 days, respectively. Beginning on day 4, mild diarrhea occurred and he started to develop a slightly clouded awareness. The patient was admitted to hospital on day 7 post onset of symptoms, when he showed the beginning of a scarlatinoid rash, hepatitis (elevated transaminases), bloody diarrhea and encephalitis. His condition deteriorated over the next 4 days with increasingly severe bloody diarrhea, hematemesis, hematuria and cutaneous hemorrhages. The initial leucopenia converted into a leucocytosis. The fever remained throughout the disease course and ranged from 39–40.8°C. Finally the patient developed kidney failure and congestive heart failure. He succumbed to the infection on day 10 post onset of symptoms (summarized from Stille and Boehle, 1971).
Animal models
Mouse models
Immunocompetent adult mice are resistant to infection with wild-type filoviruses, which is thought to be the result of their strong innate immune response, particularly the type I IFN response (Bray et al., 2001) (Tables 1 and 2). Newborn mice, however, succumb to lethal infection following intraperitoneal or intracerebral infection (van der Groen et al., 1979), which might be explained by an incompletely developed type I IFN response in these mice (Pfeifer et al., 1993). Filovirus infection is also lethal for adult immunodeficient mice such as the severe combined immunodeficient (SCID) mouse, which lacks functional B- and T-cell responses (Table 2). Unlike humans or other animal models, SCID mice remain healthy for several weeks, then develop gradual, progressive weight loss and slowing of activity, and then die 20–25 or 50–70 days after ZEBOV or MARV challenge, respectively (Bray, 2001; Warfield et al., 2007). Mice lacking a complete type I IFN response (innate immune response), such as knockout mice that do not express STAT or the IFN receptor α/β, uniformly die within a week of subcutaneous challenge with a variety of filovirus strains (Bray, 2001) (Table 2).
Table 2.
Ebola virus infection in mice
| Deficiency | Mouse strain | ZEBOV (ad)(i.p.) | ZEBOV (ad)(s.c.) | ZEBOV (wt)(i.p.) | ZEBOV (wt)(s.c.) |
|---|---|---|---|---|---|
| None | BALB/c, C57BL/6 | + | − | − | − |
| Adaptive immune response | SCID | + | + | + | + |
| Rag-2 | + | + | + | + | |
| Nude | + | + | − | − | |
| Beige | + | − | − | − | |
| IFN-γ knockout | + | − | − | − | |
| TNF-α knockout | + | − | − | − | |
| Innate immune response | IFN-α/β-receptor knockout | + | + | + | + |
| STAT1 knockout | + | + | + | + | |
| Other | Lymphotoxin-α knockout | + | + | − | − |
+=lethal infection; −=no apparent disease; ad=adapted strain; i.p.=intraperitoneal; s.c.=subcutaneous; wt =wild-type strain [summarized from Bray (Bray, 2001)].
An immunocompetent murine model was developed by passaging ZEBOV nine times in progressively older suckling mice (Bray et al., 1998) (Tables 1 and 2). In mice infected with this mouse-adapted strain, the onset of illness was 3 days after inoculation and death occurred after 5–7 days. High virus titers [up to 109 plaque-forming units (PFU)/gram] could be detected in the liver and spleen (Bray et al., 1998). The pathological changes in the liver and spleen, as well as the levels of serum transaminases (aspartate transaminase, AST; alanine transaminase, ALT), in infected mice resembled those in ZEBOV-infected primates (Bray et al., 2001). However, in contrast to primate infections, only a few fibrin deposits were found in mouse tissues and infection was only lethal when the virus was inoculated intraperitoneally. Furthermore, mice were resistant to large doses of the same virus when inoculated by other routes.
At this time, no immunocompetent mouse model for MARV has been reported (Table 1). A recent report has described a SCID mouse model, which uses liver homogenates from MARV-infected SCID mice that have been serially passaged ten times, that reduces the time to death from between 50–70 days to 7–10 days (Warfield et al., 2007). At 3–4 days post-inoculation, infected mice showed weight loss, a hunched appearance and exhibited decreased grooming; some mice appeared to have hemorrhages and some developed hind-leg paralysis. The viremia peaked at around 106 PFU/ml in serum at days 6–8. MARV was present at high titers in the blood, liver, spleen, kidney and other organs. After infection, profound thrombocytopenia, as well as notable alterations in serum chemistry levels (especially liver enzymes), occurred with progressively increasing severity (Warfield et al., 2007).
Guinea pig models
Guinea pigs inoculated with wild-type EBOV develop only a short-lived, nonlethal febrile illness (Bowen et al., 1978; Bowen et al., 1980; Ryabchikova et al., 1996). A lethal guinea pig model for EBOV infection was developed eventually by infecting inbred and outbred guinea pig strains with ZEBOV, followed by sequential passages (4–8 times) of virus in naïve guinea pigs (Bowen et al., 1978; Bowen et al., 1980; Conolly et al., 1999; Ryabchikova et al., 1996) (Table 1). The resulting guinea-pig-adapted strains of virus were uniformly lethal, typically resulting in death after 8–11 days. Infected guinea pigs exhibit few clinical signs of infection until around day 5 when they cease eating and become febrile and dehydrated. In these guinea pigs, death was not accompanied by visible signs of hemorrhage (Ryabchikova et al., 1996). The virus was first detected in the spleen and liver on day 2, and by day 3 it could also be detected in the kidney, adrenal gland, lung and pancreas. Mean organ titers rose progressively and reached their highest levels (4.8–6.4 log10 PFU/g) on day 9, and viremia peaked on day 7 with ~105 PFU/ml (Connolly et al., 1999). Infected guinea pigs also showed progressive prolongation of the prothrombin time (PT) and the partial thromboplastin time (aPTT).
As seen in ZEBOV infection, guinea pigs that were experimentally infected with wild-type MARV developed only a mild febrile disease and most of them survived the infection (Table 1). The virulence of the virus was increased by serial passage in guinea pigs. Four to eight passages were sufficient to produce a virus that was lethal for all animals by 7–17 days after infection (Simpson et al., 1968). Infected animals showed weight loss, elevated temperature and edematous faces, and the blood from some animals failed to clot. As seen in NHPs, a sudden decrease in temperature occurred shortly before death.
Nonhuman primates
Filovirus infections have been intensively investigated in various species of NHP, but mainly in cynomolgus (Macaca fascicularis) and rhesus macaques (Macaca mulatta). African green monkeys (Chlorocebus aethiops) are resistant to REBOV and baboons (Papio hamadryas) appear to be somewhat more resistant to all EBOV species (Fisher-Hoch et al., 1992; Fisher-Hoch and McCormick, 1999; Gonchar et al., 1991; Ryabchikova et al., 1999a; Ryabchikova et al., 1999b). The viral dose and strain, the route of infection and the species of NHP used all appear to influence the onset, duration and severity of the clinical signs.
Several NHP species have been used as models to study ZEBOV infection, namely the African green monkey (Bowen et al., 1978; Fisher-Hoch et al., 1992; Davis et al., 1997; Ryabchikova et al., 1999a; Ryabchikova et al., 1999b), hamadryad baboon (Jones, 1980; Mikhailov et al., 1994; Borisevich et al., 1995; Ryabchikova et al., 1996; Kudoyarova-Zubavichene et al., 1999; Ryabchikova et al., 1999a; Ryabchikova et al., 1999b), rhesus macaque (Bowen et al., 1978; Fisher-Hoch et al., 1985; P’iankov et al., 1995; Jaax et al., 1996; Johnson et al., 1996; Geisbert et al., 2002) and cynomolgus macaque (Jones, 1980; Fisher-Hoch et al., 1992; Geisbert et al., 2003). For cynomolgus macaques infected with ZEBOV, the onset of clinical signs is fairly rapid, occurring within 4–5 days. In other NHP models, the onset of symptoms is slower and thus more similar to that observed in humans. Usually macaques become febrile and lethargic between 2–3 days after infection and fever persists throughout the course of the disease. A drop in body temperature usually precedes death. Animals also show weight loss of up to 10% of their body weight, which is probably primarily related to dehydration rather than mobilization of fat reserves and catabolism – although all of these factors probably contribute. In addition, some animals develop diarrhea and intermittent melena. As soon as day 4 after infection, NHPs generally develop a maculopapular rash that remains prominent until death. Lymphadenopathy of peripheral lymph nodes develops early in the disease course and an enlarged liver with rounded capsular borders is seen at mid- to late-stages of the disease (Geisbert and Hensley, 2004). Virus can normally be detected in the blood on day 2 after infection and usually peaks 2–3 days later. Throughout the course of the disease, a rise in both absolute and relative neutrophil counts develops, coinciding with severe lymphopenia in which neutrophils account for over 90% of all leukocytes. In addition, a marked thrombocytopenia is uniformly seen in these infected animals. Prolongation of the aPTT has been reported as early as day 6 after infection and by day 10–12 blood samples often lose their ability to clot (Fisher-Hoch et al., 1983). Plasma levels of sodium, potassium and calcium all fall during disease progression, whereas urea and creatinine levels increase. Further, the levels of the liver transaminases (AST, ALT) start to increase, usually at around day 5, and remain high until death (Fisher-Hoch et al., 1983; Fisher-Hoch et al., 1985).
Only a few studies have evaluated the pathogenesis of SEBOV in NHPs. In rhesus and cynomolgus macaques, the SEBOV disease course appears to be several days slower than that seen following ZEBOV infection and rates of survival appear to be higher (Ellis et al., 1978; Fisher-Hoch et al., 1992; Geisbert et al., 2008).
Different species of NHP, namely African green monkeys, rhesus macaques and squirrel monkeys (Saimiri sciureus), have been experimentally infected with MARV (Simpson et al., 1968; Simpson, 1969; Lub et al., 1995). Wild-type MARV is uniformly lethal for all species. After an incubation period of 2–6 days, all NHPs develop a febrile illness that is independent of both the inoculum dose and the route of infection. The clinical presentation is more or less identical in all three species, showing fever (40–40.5°C), anorexia, weight loss and unresponsiveness. Hemorrhaging from the rectum or injection site and diarrhea can be found occasionally (Simpson et al., 1968). Rhesus macaques in particular develop petechial skin rashes, resembling human cases where rashes have been described on the arms and thighs, and to a lesser extend on the thorax, face and neck. Rashes were not typically seen in African green monkeys (Simpson, 1969). A rapid deterioration in the condition of these animals was followed by hypothermia, shock and finally death, which occurred at 6–13 days post-infection. Marked thrombocytopenia, lymphopenia and blood coagulation abnormalities can also be found in infected animals. Both the levels of liver transaminases and the neutrophil count increase during the course of disease (Simpson et al., 1968; Simpson, 1969; Gonchar et al., 1991; Johnson et al., 1996). Virus can be detected in the blood as early as 3 days after infection and peak viremia titers reach 107–108 PFU/ml.
Clinical terms.
Ecchymoses – bruise-like black-and-blue or purple skin lesions caused by ruptured blood vessels
Epistaxis – nosebleed
Viral hemorrhagic fevers (VHFs) – a diverse group of animal and human illnesses that are caused by RNA viruses, characterized by fever and bleeding disorders and can progress to high fever, shock and death in extreme cases
Hypovolemic shock – decreased blood volume causing insufficient blood circulation, also known as hypovolemia
Lymphadenopathy – abnormal swelling and enlargement of the lymph nodes, indicative of disease
Maculopapular rash – a flat, red skin rash covered with bumps, thus containing characteristics of both macules (flat, discolored regions) and papules (raised bumps)
Melena – black, tar-like stools associated with gastrointestinal bleeding
Myalgia – muscle pain
Petechiae – small reddish or purplish spots resulting from a localized hemorrhage in skin or mucous membrane
Thrombocytopenia – a persistent low blood platelet count
Viremia – presence of viruses in the blood
Discussion of animal models
Although rodent models have some similarities to the human disease, they are of limited value for clinical disease presentation of human filovirus infection because the disease course in rodents differs from that reported in humans and NHPs (Gibb et al., 2001; Geisbert et al., 2002; Feldmann et al., 2003). In addition, important clinical signs such as maculopapular rash and an elevated temperature throughout the course of the disease are missing. Mice do not display all of the characteristics of DIC, which is a hallmark of filovirus infection in primates that includes prolongation of PT and aPTT, circulating fibrin degradation products, decreased plasma fibrinogen and decreased fibrin deposition (Bray et al., 2001; Geisbert and Hensley, 2004; Sanchez et al., 2007). Compared with mice, infected guinea pigs develop more severe coagulation defects, including a drop in platelet counts and an increase in coagulation time, but the level of fibrin deposition and coagulopathy are not as high as the levels seen in NHPs (Connolly et al., 1999; Reed and Mohamadzadeh, 2007). Further, lymphocyte bystander apoptosis, an important feature in primates and mice, is not as prominent in guinea pigs (Bray et al., 1998; Connolly et al., 1999; Bradfute et al., 2007). Mice differ from guinea pigs and monkeys in that they display a decrease in blood urea nitrogen (BUN), rather than an increase (Bray, 2001). Additionally, the histopathologic features of filovirus disease in humans are more closely mirrored by NHPs than rodent models (Zaki and Goldsmith, 1999).
Clinical and basic research opportunities.
Creating small animal models of Sudan ebolavirus (SEBOV), Cote d’Ivoire ebolavirus (CIEBOV) and Reston ebolavirus (REBOV)
Development of an immunocompetent mouse model for MARV
Development of EBOV and MARV models in smaller non-human primate species
In vivo screening studies for new EBOV and MARV therapeutics and vaccines
Using animal models for clinical effectiveness studies in accordance with new guidelines set by the Food & Drug Administration (FDA) and Center for Biologics Evaluation and Research (CBER)
NHPs are excellent models with which to study filovirus pathogenesis because they closely resemble the clinical disease and pathology described in humans. When selecting a suitable NHP model, the species, sex and age of the NHPs, together with the route of infection and the administration dose, must all be taken into consideration because all of these factors will have an influence on the study (Geisbert et al., 2004). Cynomolgus and rhesus macaques are considered the ‘gold standard’ models for filovirus infections, and studies using rhesus macaques have additional advantages in that this species is widely used in the pharmaceutical industry and its genome sequence has been published (Geisbert et al., 2004; Rhesus Macaque Genome Sequencing and Analysis Consortium, 2007). Nevertheless, the increase demand for NHPs for biodefense and infectious disease research has contributed to a current shortage of macaques (Cohen, 2000; Patterson and Carrion, 2005; Satkoski et al., 2008). In the future, the development of a model that uses a smaller species of NHP, such as certain species of new world monkeys, might help to ease the burden.
Despite the differences in clinical presentation and pathogenesis, rodents can serve an important role for the initial in vivo evaluation of filovirus vaccines and treatment schemes (Huggins et al., 1995; Wilson et al., 2000). In particular, mice offer certain advantages including the ease with which large numbers of animals can be obtained and the availability of numerous strains, including genetically engineered strains, as well as a wide range of well-characterized reagents. However, one must use caution when interpreting data from rodents, because a number of antiviral therapies and vaccines have been shown to be effective in rodents but then failed in NHP models (Bray and Paragas, 2002; Geisbert et al., 2002; Feldmann et al., 2005b; Reed and Mohamadzadeh, 2007). This might be the result of considerable differences between rodent and primate immunology (Mestas and Hughes, 2004), particularly the strong innate immune response in rodents (Bray, 2001).
Footnotes
COMPETING INTERESTS
The authors declare no competing financial interest.
REFERENCES
- Aleksandrowicz P., Wolf K., Falzarano D., Feldmann H., Seebach J., Schnittler H. (2008). Viral haemorrhagic fever and vascular alterations. Hamostaseologie 28, 77–84 [PubMed] [Google Scholar]
- Borisevich I. V., Mikhailov V. V., Krasnianskii V. P., Gradoboev V. N., Lebedinskaia E. V., Potryvaeva N. V., Timan’kova G. D. (1995). Development and study of the properties of immunoglobulin against Ebola fever. Vopr. Virusol. 40, 270–273 [PubMed] [Google Scholar]
- Bowen E. T., Platt G. S., Simpson D. I., McArdell L. B., Raymond R. T. (1978). Ebola haemorrhagic fever: experimental infection of monkeys. Trans. R. Soc. Trop. Med. Hyg. 72, 188–191 [DOI] [PubMed] [Google Scholar]
- Bowen E. T., Platt G. S., Lloyd G., Raymond R. T., Simpson D. I. (1980). A comparative study of strains of Ebola virus isolated from southern Sudan and northern Zaire in 1976. J. Med. Virol. 6, 129–138 [DOI] [PubMed] [Google Scholar]
- Bradfute S. B., Braun D. R., Shamblin J. D., Geisbert J. B., Paragas J., Garrison A., Hensley L. E., Geisbert T. W. (2007). Lymphocyte death in a mouse model of Ebola virus infection. J. Infect. Dis. 196 Suppl. 2, S296–S304 [DOI] [PubMed] [Google Scholar]
- Bray M. (2001). The role of the Type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 82, 1365–1373 [DOI] [PubMed] [Google Scholar]
- Bray M., Paragas J. (2002). Experimental therapy of filovirus infections. Antiviral Res. 54, 1–17 [DOI] [PubMed] [Google Scholar]
- Bray M., Davis K., Geisbert T., Schmaljohn C., Huggins J. (1998). A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178, 651–661 [DOI] [PubMed] [Google Scholar]
- Bray M., Hatfill S., Hensley L., Huggins J. W. (2001). Haematological, biochemical and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J. Comp. Pathol. 125, 243–253 [DOI] [PubMed] [Google Scholar]
- Cohen J. (2000). AIDS research: vaccine studies stymied by shortage of animals. Science 287, 959–960 [DOI] [PubMed] [Google Scholar]
- Connolly B. M., Steele K. E., Davis K. J., Geisbert T. W., Kell W. M., Jaax N. K., Jahrling P. B. (1999). Pathogenesis of experimental Ebola virus infection in guinea pigs. J. Infect. Dis. 179 Suppl. 1, S203–S217 [DOI] [PubMed] [Google Scholar]
- Davis K. J., Anderson A. O., Geisbert T. W., Steele K. E., Geisbert J. B., Vogel P., Connolly B. M., Huggins J. W., Jahrling P. B., Jaax N. K. (1997). Pathology of experimental Ebola virus infection in African green monkeys: involvement of fibroblastic reticular cells. Arch. Pathol. Lab. Med. 121, 805–819 [PubMed] [Google Scholar]
- Ellis D. S., Simpson I. H., Francis D. P., Knobloch J., Bowen E. T., Lolik P., Deng I. M. (1978). Ultrastructure of Ebola virus particles in human liver. J. Clin. Pathol. 31, 201–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H., Jones S., Klenk H. D., Schnittler H. J. (2003). Ebola virus: from discovery to vaccine. Nat. Rev. Immunol. 3, 677–685 [DOI] [PubMed] [Google Scholar]
- Feldmann H., Geisbert T. W., Jahrling P. B., Klenk H. D., Netesov S. V., Peters C. J., Sanchez A., Swanepoel R., Volchkov V. E. (2005a). Filoviridae. In Virus Taxonomy, VIIIth Report of the ICTV (ed. Fauquet C. M., Mayo M. A., Maniloff J., Desselberger U., Ball L. A.), pp. 645–653 London: Elsevier [Google Scholar]
- Feldmann H., Jones S. M., Schnittler H. J., Geisbert T. (2005b). Therapy and prophylaxis of Ebola virus infections. Curr. Opin. Investig. Drugs 6, 823–830 [PubMed] [Google Scholar]
- Fisher-Hoch S. P., McCormick J. B. (1999). Experimental filovirus infections. Curr. Top. Microbiol. Immunol. 235, 117–143 [DOI] [PubMed] [Google Scholar]
- Fisher-Hoch S. P., Platt G. S., Lloyd G., Simpson D. I., Neild G. H., Barrett A. J. (1983). Haematological and biochemical monitoring of Ebola infection in rhesus monkeys: implications for patient management. Lancet 2, 1055–1058 [DOI] [PubMed] [Google Scholar]
- Fisher-Hoch S. P., Platt G. S., Neild G. H., Southee T., Baskerville A., Raymond R. T., Lloyd G., Simpson D. I. (1985). Pathophysiology of shock and hemorrhage in a fulminating viral infection (Ebola). J. Infect. Dis. 152, 887–894 [DOI] [PubMed] [Google Scholar]
- Fisher-Hoch S. P., Brammer T. L., Trappier S. G., Hutwagner L. C., Farrar B. B., Ruo S. L., Brown B. G., Hermann L. M., Perez-Oronoz G. I., Goldsmith C. S. (1992). Pathogenic potential of filoviruses: role of geographic origin of primate host and virus strain. J. Infect. Dis. 166, 753–763 [DOI] [PubMed] [Google Scholar]
- Geisbert T. W., Hensley L. E. (2004). Ebola virus: new insights into disease aetiopathology and possible therapeutic interventions. Expert Rev. Mol. Med. 6, 1–24 [DOI] [PubMed] [Google Scholar]
- Geisbert T. W., Jahrling P. B. (2004). Exotic emerging viral diseases: progress and challenges. Nat. Med. 10, 110–121 [DOI] [PubMed] [Google Scholar]
- Geisbert T. W., Pushko P., Anderson K., Smith J., Davis K. J., Jahrling P. B. (2002). Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 8, 503–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert T. W., Hensley L. E., Larsen T., Young H. A., Reed D. S., Geisbert J. B., Scott D. P., Kagan E., Jahrling P. B., Davis K. J. (2003). Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol. 163, 2347–2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert T. W., Jahrling P. B., Larsen T., Davis K., Hensley L. (2004). Filovirus pathogenesis in nonhuman primates. In Ebola and Marburg Viruses (ed. Klenk H. D., Feldmann H.), vol. 1, pp. 203–237 London: Taylor and Francis [Google Scholar]
- Geisbert T. W., Daddario-DiCaprio K. M., Williams K. J., Geisbert J. B., Leung A., Feldmann F., Hensley L. E., Feldmann H., Jones S. M. (2008). Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J. Virol. 82, 5664–5668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb T. R., Bray M., Geisbert T. W., Steele K. E., Kell W. M., Davis K. J., Jaax N. K. (2001). Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J. Comp. Pathol. 125, 233–242 [DOI] [PubMed] [Google Scholar]
- Gonchar N. I., Pshenichnov V. A., Pokhodiaev V. A., Lopatov K. L., Firsova I. V. (1991). The sensitivity of different experimental animals to the Marburg virus. Vopr. Virusol. 36, 435–437 [PubMed] [Google Scholar]
- Huggins J., Zhang Z., Monath T. I. (1995). Inhibition of Ebola virus replication in vitro and in a SCID mouse model by S-adenosylhomocysteine hydrolase inhibitors. Antiviral Res. Suppl, 122 [Google Scholar]
- Jaax N. K., Davis K. J., Geisbert T. J., Vogel P., Jaax G. P., Topper M., Jahrling P. B. (1996). Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch. Pathol. Lab. Med. 120, 140–155 [PubMed] [Google Scholar]
- Johnson E. D., Johnson B. K., Silverstein D., Tukei P., Geisbert T. W., Sanchez A. N., Jahrling P. B. (1996). Characterization of a new Marburg virus isolated from a 1987 fatal case in Kenya. Arch. Virol. Suppl. 11, 101–114 [DOI] [PubMed] [Google Scholar]
- Jones T. C. (1980). The value of animal models. Am. J. Pathol. 101, S3–S9 [PMC free article] [PubMed] [Google Scholar]
- Kudoyarova-Zubavichene N. M., Sergeyev N. N., Chepurnov A. A., Netesov S. V. (1999). Preparation and use of hyperimmune serum for prophylaxis and therapy of Ebola virus infections. J. Infect. Dis. 179 Suppl. 1, S218–S223 [DOI] [PubMed] [Google Scholar]
- Lub M. I., Sergeev A. N., P’iankov O. V., P’iankova O. G., Petrishchenko V. A., Kotliarov L. A. (1995). Certain pathogenetic characteristics of a disease in monkeys in infected with the Marburg virus by an airborne route. Vopr. Virusol. 40, 158–161 [PubMed] [Google Scholar]
- Martini G. A., Siegert R. (1971). Marburg Virus Disease, pp. 1–230 New York: Springer [Google Scholar]
- Mestas J., Hughes C. C. (2004). Of mice and not men: differences between mouse and human immunology. J. Immunol. 172, 2731–2738 [DOI] [PubMed] [Google Scholar]
- Mikhailov V. V., Borisevich I. V., Chernikova N. K., Potryvaeva N. V., Krasnianskii V. P. (1994). The evaluation in hamadryas baboons of the possibility for the specific prevention of Ebola fever. Vopr. Virusol. 39, 82–84 [PubMed] [Google Scholar]
- Mohamadzadeh M., Chen L., Schmaljohn A. L. (2007). How Ebola and Marburg viruses battle the immune system. Nat. Rev. Immunol. 7, 556–567 [DOI] [PubMed] [Google Scholar]
- Patterson J. L., Carrion R., Jr (2005). Demand for nonhuman primate resources in the age of biodefense. ILAR J. 46, 15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattyn S. R. (1978). Ebola Virus Haemorrhagic Fever, pp. 1–436 Amsterdam: Elsevier [Google Scholar]
- Peters C. J., LeDuc J. W. (1999). Ebola: the virus and the disease. J. Infect. Dis. 179 Suppl. 1, S1–S288 [DOI] [PubMed] [Google Scholar]
- Pfeifer K., Ushijima H., Lorenz B., Muller W. E., Schroder H. C. (1993). Evidence for age-dependent impairment of antiviral 2′,5′-oligoadenylate synthetase/ribonuclease L-system in tissues of rat. Mech. Ageing Dev. 67, 101–114 [DOI] [PubMed] [Google Scholar]
- P’iankov O. V., Sergeev A. N., P’iankova O. G., Chepurnov A. A. (1995). Experimental Ebola fever in Macaca mulatta. Vopr. Virusol. 40, 113–115 [PubMed] [Google Scholar]
- Reed D. S., Mohamadzadeh M. (2007). Status and challenges of filovirus vaccines. Vaccine 25, 1923–1934 [DOI] [PubMed] [Google Scholar]
- Rhesus Macaque Genome Sequencing and Analysis Consortium. Gibbs R. A., Rogers J., Katze M. G., Bumgarner R., Weinstock G. M., Mardis E. R., Remington K. A., Strausberg R. L., Venter J. C., et al. . (2007). The rhesus macaque genome sequence informs biomedical and evolutionary analyses. Science 31, 222–234 [DOI] [PubMed] [Google Scholar]
- Ryabchikova E., Kolesnikova L., Smolina M., Tkachev V., Pereboeva L., Baranova S., Grazhdantseva A., Rassadkin Y. (1996). Ebola virus infection in guinea pigs: presumable role of granulomatous inflammation in pathogenesis. Arch. Virol. 141, 909–921 [DOI] [PubMed] [Google Scholar]
- Ryabchikova E. I., Kolesnikova L. V., Luchko S. V. (1999a). An analysis of features of pathogenesis in two animal models of Ebola virus infection. J. Infect. Dis. 179 Suppl. 1, S199–S202 [DOI] [PubMed] [Google Scholar]
- Ryabchikova E. I., Kolesnikova L. V., Netesov S. V. (1999b). Animal pathology of filoviral infections. Curr. Top. Microbiol. Immunol. 235, 145–173 [DOI] [PubMed] [Google Scholar]
- Sanchez A., Geisbert T. W., Feldmann H. (2007). Marburg and Ebola viruses. In Fields Virology 5th edn, vol. 1, (ed. Knipe D. M., Howley P. M.), pp. 1409–1448 Philadelphia: Lippincott Williams and Wilkins [Google Scholar]
- Satkoski J. A., Malhi R., Kanthaswamy S., Tito R., Malladi V., Smith D. (2008). Pyrosequencing as a method for SNP identification in the rhesus macaque (Macaca mulatta). BMC Genomics 9, 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson D. I. (1969). Marburg agent disease: in monkeys. Trans. R. Soc. Trop. Med. Hyg. 63, 303–309 [DOI] [PubMed] [Google Scholar]
- Simpson D. I., Zlotnik I., Rutter D. A. (1968). Vervet monkey disease: experiment infection of guinea pigs and monkeys with the causative agent. Br. J. Exp. Pathol. 49, 458–464 [PMC free article] [PubMed] [Google Scholar]
- Stille W., Boehle E. (1971). Clinical course and prognosis of Marburg virus (“Green-Monkey”) disease. In Marburg Virus Disease (ed. Martini G. A., Siegert R.), pp. 10–18 New York, Heidelberg, Berlin: Springer Verlag [Google Scholar]
- Stroeher U., Feldmann H. (2006). Progress towards the treatment of Ebola Haemorrhagic fever. Expert Opin. Investig. Drugs 15, 1523–1535 [DOI] [PubMed] [Google Scholar]
- Sullivan N., Yang Z. Y., Nabel G. J. (2003). Ebola virus pathogenesis: implications for vaccines and therapies. J. Virol. 77, 9733–9777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Groen G., Jacob W., Pattyn S. R. (1979). Ebola virus virulence for newborn mice. J. Med. Virol. 4, 239–240 [DOI] [PubMed] [Google Scholar]
- Warfield K. L., Alves D. A., Bradfute S. B., Reed D. K., van Tongeren S., Kalina W. V., Olinger G. G., Bavari S. (2007). Development of a model for marburgvirus based on severe-combined immunodeficiency mice. Virol. J. 4, 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J. A., Hevey M., Bakken R., Guest S., Bray M., Schmaljohn A. L., Hart M. K. (2000). Epitopes involved in antibody-mediated protection from Ebola virus. Science 287, 1664–1666 [DOI] [PubMed] [Google Scholar]
- Zaki S. R., Goldsmith C. S. (1999). Pathologic features of filovirus infections in humans. Curr. Top. Microbiol. Immunol. 235, 97–116 [DOI] [PubMed] [Google Scholar]