Abstract
Background & Aims
The effect of GI endoscopy nursing experience on polyp detection is unknown. The aim of this study was to determine whether nurse experience is associated with odds of polyp detection.
Methods
Retrospective analysis of screening colonoscopies performed by attendings at University of North Carolina Hospitals between August 2003 and 2005. Nurse experience was dichotomized at 6 months. The primary outcome was polyp detection, with secondary analysis by histologic type. Descriptive statistics, bivariate analysis, and multivariable logistic regression were performed.
Results
Any polyp was detected in 44% of the eligible 3,631 colonoscopies. Multiple polyps were detected in 23%, adenomas in 25%, advanced lesions in 5%, and hyperplastic polyps in 11%. Twenty-nine nurses were employed during the study period, 19 of whom were new to endoscopy nursing. For nurses with 6 months of experience or less, any polyp was detected in 40.3% of procedures compared with 46.0% of procedures for nurses with more than 6 months of experience (OR 1.26, 95% CI: 1.09, 1.46). Similar results were seen for multiple polyps (OR 1.54, 95% CI: 1.29, 1.84) and hyperplastic polyps (OR 1.47, 95% CI 1.22, 1.76) but not for adenomas (OR 1.10 95% CI: 0.93, 1.30) or advanced lesions (OR 0.99, 95% CI: 0.71, 1.36). These relationships were unchanged after adjusting for potential confounding patient and procedure variables.
Conclusions
Procedures staffed by less experienced GI endoscopy nurses have increased odds of not detecting polyps. Sub-analysis suggests that detection of hyperplastic polyps explains much of this relationship.
Colonoscopy is recommended as a screening option for the prevention of colorectal cancer by a number of national organizations.1, 2 The success of this procedure rests in part with the reliable detection and removal of benign polyps that are precursors to malignant lesions.3, 4 Current quality-of-care guidelines recommend that endoscopists should detect polyps in approximately 25% of men and 15% of women based on multiple cross-sectional studies of the prevalence of polyps in the general population.5
In addition, there has been extensive recent investigation into factors that predict polyp detection. Polyp prevalence is greater in males than females, and increases with age in both genders.5–8 It may also increase in obese patients or those with elevated BMI or visceral fat levels.9–11 For optimal polyp detection, physicians must have appropriate training and experience in colonoscopy and polypectomy and must maintain their endoscopy skills.12–15 During the procedure, adequate bowel preparation with complete mucosal visualization is ideal, the cecum must be reached, and recent literature has highlighted the importance of a colonoscope withdrawal time sufficient to carefully examine the colon.16–19 It is not known, however, whether the experience level of the GI endoscopy nurse staffing the procedure is associated with polyp detection, but it has been our clinical experience that all aspects of the procedure may be facilitated by an experienced nurse.
Because the GI procedures unit at our center has had a high rate of nurse turnover in recent years, we recognized that there were a set of nurses with low levels of GI endoscopy nursing experience in whom this question could be addressed. Therefore, the aim this study was to determine whether the experience level of GI endoscopy nurses is associated with the odds of polyp detection during screening colonoscopy after controlling for other factors known to influence polyp detection.
Methods
We performed a retrospective analysis of outpatient screening colonoscopies performed by attending physicians in adult patients at University of North Carolina (UNC) Hospitals. All procedures from August 2003 through August 2005 at our hospital-based and off-site outpatient unit were included, with the exception of any procedure in which a fellow was involved to minimize any trainee-effect on polyp detection rates.
We defined our main exposure variable, nursing experience, in a previous study examining the relationship between nurse experience and other screening colonoscopy outcomes.20, 21 In brief, for each individual nurse staffing each procedure, experience was measured in weeks from the initial start date in any GI procedures unit (either at UNC or elsewhere) to the date of that procedure. For the purposes of this analysis, experience was dichotomized a priori at 6 months based on the results of our past work showing that this tended to be a threshold level for a number of performance parameters such as time to cecum, cecal intubation rate, and total procedure time.21 Over the time course of the study, an individual nurse may have participated in cases initially as an inexperienced nurse and in later procedures as an experienced nurse. When two nurses were present during a procedure for training purposes (with a more experienced nurse acting as a mentor), the case was assigned the experience level of the less experienced nurse. At our center, GI endoscopy nurses do not perform endoscopy, but do monitor the patient, administer sedation under physician supervision, and assist with polypectomy and other technical aspects of the procedure. Additionally, nurses are not assigned to a specific physician, and physicians rotate between cases and rooms in no set order.
The primary outcome of our study was any polyp detection. We used UNC Hospitals’ electronic medical record system, as well as our electronic endoscopy databases (ProvationMD and ProvationRN, Provation Medical, Minneapolis, MN), to extract data about polyp detection. We recorded procedures in which any polyp was detected as well as procedures where multiple (>1) polyps were detected. In essentially all cases when a polyp was detected, polypectomy was also performed. We performed a secondary analysis of polyp detection per procedure by histologic type, including adenomas, advanced lesions (defined as size ≥ 1cm, villous architecture, or high grade dysplasia)22, 23, and hyperplastic polyps.
Covariates of interest and potential confounding factors were obtained from the same electronic records and included: patient age; patient gender; patient body mass index (BMI; calculated as body weight in kilograms divided by height in meters squared) and physician-assessed bowel preparation quality. Data on patient family history of colorectal polyps or cancer was not available. We also measured the cecal intubation rate (which we defined as the proportion of procedures where the cecum was reaching given that bowel preparation was adequate and that the recto-sigmoid junction was passed, in order to eliminate cases where visualization was precluded or cases which were immediate technical failures) and colonoscope withdrawal time (defined as the total procedure time minus the cecal intubation time). Finally, to capture attending physician colonoscopy volume, we recorded the total number of screening colonoscopies that were performed (without GI fellow involvement) over the study time frame. The attending physicians in this study were all experienced colonoscopists with > 1000 colonoscopies performed in their careers-to-date.
Statistical analysis included routine descriptive and bivariate statistics using chi-square for comparisons between two categorical variables and t-tests for comparisons including one continuous variable. Logistic regression with an analysis of covariance strategy was used for multivariable analysis. Initially, a full model consisting of all potential confounding factors was used to estimate the effect of nursing experience on polyp detection. Then, we used likelihood ratio testing to evaluate interactions between the exposure and potential confounders. There were no significant interactions by this test (at an a priori α level of 0.20), so interactions terms were not included in the model. Finally, we used a backwards elimination approach to remove covariates and assess for confounding. If a covariates’ exclusion from the model resulted in an a priori change in estimate of less than 10% compared with the fully adjusted model, then it was not considered to be a confounder and was left out of the final model.
There were missing data only for 4 covariates: BMI (3.2% missing); bowel preparation quatlity and reaching the cecum (7.4% missing for each); and withdrawal time (11.5% missing). There was no differential pattern for the missing data between less experienced and more experienced nurses, and missing data were excluded from bivariate and multivariate analysis.
This study was approved by the UNC School of Nursing Institutional Review Board.
Results
Patient, nurse, and procedure characteristics
A total of 3,631 screening colonoscopies were included in this study (Table 1). A full description of the study characteristics has been previously reported.20, 21 In brief, the mean patient age was 58 years, 58% of subjects were female, and a good or excellent bowel preparation was reported in 78%.
Table 1.
Selected patient, nurse, and colonoscopy characteristics
| Patient characteristics | Number (%) or mean |
|---|---|
| Mean age (years ± SD, range) | 58.4 ± 9.5 (21–90) |
| Males | 1,533 (42.2) |
| BMI | |
| < 25 (normal) | 1,279 (35.2) |
| ≥ 25 and < 30 (overweight) | 1,265 (34.9) |
| ≥ 30 (obese) | 971 (26.7) |
| Not reported | 116 (3.2) |
|
| |
| Nurse characteristics
| |
| Total number of nurses during study period | 29 |
| Number of nurses at the beginning | 10 |
| Number of nurses at the end | 15 |
| GI endoscopy nurse experience | |
| 0 – 6 months | 1,069 (29.4) |
| > 6 months | 2,562 (70.6) |
| Procedures with two nurses present | 347 (9.6) |
|
| |
| Colonoscopy characteristics
| |
| Total number of screening colonoscopies during study period | 3,631 |
| Location of procedure | |
| Hospital-based unit | 2,383 (65.6) |
| Off-site unit | 1,248 (34.4) |
| Mean physician procedure volume (± SD, range) | 329 ± 176 (11–554) |
| Bowel preparation quality | |
| Excellent | 1,449 (39.9) |
| Good | 1,372 (37.8) |
| Fair | 428 (11.8) |
| Poor | 84 (2.3) |
| Unsatisfactory | 31 (0.9) |
| Not reported | 267 (7.4) |
| Cecal intubation rate (%)* | 93.5 |
| Mean withdrawal time (minutes ± SD, range) | 11.8 ± 7.7 (1.8 – 99.1) |
| Polyp detection by procedures | |
| Any polyp detected | 1,609 (44.3) |
| Multiple polyps (any type) detected | 846 (23.3) |
| Adenomas detected | 896 (24.8) |
| Advanced lesions detected† | 185 (5.1) |
| Hyperplastic polyps detected | 792 (21.9) |
| Other lesions detected‡ | 397 (11.0) |
Defined as the rate for cases with adequate bowel preparation in which the rectosigmoid junction was passed; this excludes 74 cases where the cecum was intubated with a poor or unsatisfactory bowel preparation where the examination was deemed to not adequately evaluate the colonic mucosa.
Defined as defined as size ≥ 1cm, villous architecture, or high grade dysplasia.
Other lesions included inflammatory polyps, lymphoid nodules, carcinoid tumors, and normal colonic mucosa.
Twenty-nine nurses were employed during the study period, 19 of whom were newly hired and had not worked in a GI procedures unit previously. Overall, 1,069 of the procedures (29.4%) were staffed by nurses with 6 months or less of GI nursing experience. Of note, during the course of the study, a given nurse may have participated in some cases as an inexperienced nurse and later as an experienced nurse.
Screening colonoscopies were performed by 20 different attending physicians, and the mean physician procedure volume over the course of the study time frame was 329 ± 176 colonoscopies. The cecal intubation rate was 93.5% and the mean withdrawal time was 11.8 ± 7.7 minutes, including time taken for biopsies, polypectomies, or other maneuvers. There was no difference in withdrawal time based on the level of nurse experience.
Polyp characteristics
At least one polyp of any histologic type was detected in 1,609 procedures (44%), and multiple polyps were found in 23% of cases (Table 1). Of these polyps, histopathologic data were available for 1,597 (99.3%). Adenomas were detected in 896 procedures (25%), of which 185 (5%) were advanced lesions, and hyperplastic polyps were detected in 792 procedures (22%) (Table 1). A total of 3,666 polypoid lesions were removed (mean 2.3 polyps ± 2.0 per procedure; range 1–25) with a mean size of 5.8 mm ± 4.8 mm (range 1–50 mm).
Bivariate analysis showed that the presence of any polyp was associated with increased age, male sex, increased BMI, increased physician procedure volume, better quality bowel preparation, reaching the cecum, and increased coloscopy withdrawal time (Table 2). The same associations were seen for the detection of multiple polyps as well as for adenomas, advanced lesions, and hyperplastic polyps (data not shown).
Table 2.
Bivariate associations between polyp detection and selected study characteristics
| Characteristic | Procedures with any polyp detected
|
||
|---|---|---|---|
| n | % or mean (± SD) | p value* | |
| Mean age | |||
| No polyp detected | 2,022 | 58.0 ± 9.45 | 0.02 |
| Any polyp detected | 1,609 | 58.8 ± 9.46 | |
| Sex | |||
| Male | 1,533 | 50.4 | < 0.001 |
| Female | 2,098 | 39.9 | |
| Body mass index (mg/kg2) | |||
| < 25 (normal) | 475 | 37.1 | < 0.001 |
| ≥ 25 and < 30 (overweight) | 601 | 47.5 | |
| ≥ 30 (obese) | 490 | 50.5 | |
| Location of procedure | |||
| Hospital-based unit | 2,383 | 38.9 | < 0.001 |
| Off-site unit | 1,248 | 54.7 | |
| Mean physician procedure volume | |||
| No polyp detected | 2,022 | 307 ± 174 | < 0.001 |
| Any polyp detected | 1,609 | 357 ± 174 | |
| Bowel preparation quality | |||
| Excellent | 1,449 | 50.4 | < 0.001 |
| Good | 1,372 | 43.0 | |
| Fair | 428 | 41.4 | |
| Poor | 84 | 32.1 | |
| Unsatisfactory | 31 | 16.1 | |
| Cecal intubation rate† | |||
| Cecum not reached | 219 | 37.9 | 0.02 |
| Cecum reached | 3,145 | 46.0 | |
| Mean withdrawal time | |||
| No polyp detected | 1,774 | 9.1 ± 4.8 | < 0.001 |
| Any polyp detected | 1,439 | 15.0 ± 9.2 | |
| GI endoscopy nurse experience | |||
| 0 – 6 months | 1,069 | 40.3 | 0.002 |
| > 6 months | 2,562 | 46.0 | |
Tests based on chi-square for categorical variables and t-test for continuous variables.
Defined as the rate for cases with adequate bowel preparation in which the rectosigmoid junction was passed.
Polyp detection
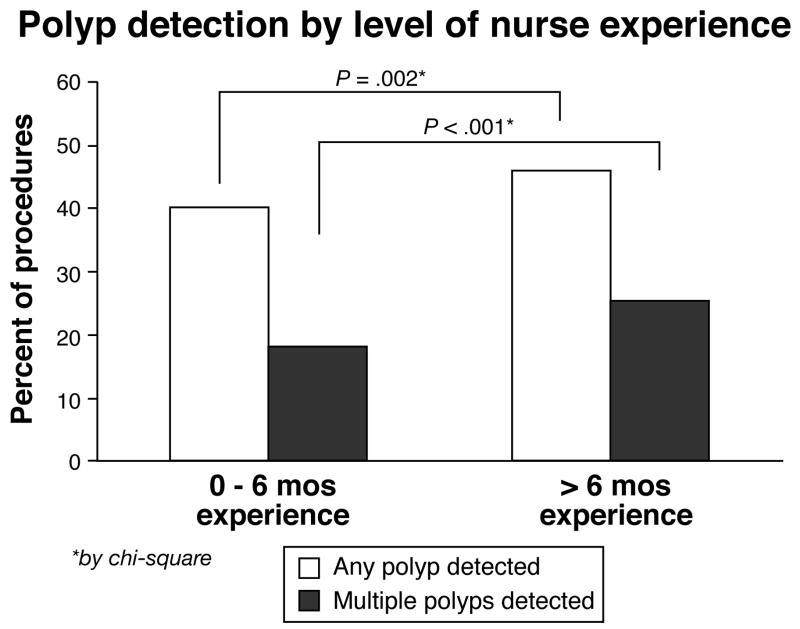
Polyps of any histologic type were detected in 40.6% of procedures (n = 1,069) staffed by nurses with 0–6 months of experience, but in 46.0% of procedures (n = 2,562) staffed by more experienced nurses (p = 0.002; Figure 1). This yields an unadjusted odds ratio (OR) of 1.26 (95% CI: 1.06, 1.46). Specifically, procedures staffed by nurses with 6 months or less of GI nursing experience had 1.26 times the odds of not detecting a polyp compared to nurses with more experience. Similarly, multiple polyps were detected in 18.2 % of procedures staffed by less experienced nurses and in 25.5% of procedures staffed by more experienced nurses (p < 0.001; OR 1.54; 95% CI: 1.29, 1.84; Figure 1).
Figure 1.
Polyp detection be level of nurse experience. Light gray bars indicate the proportion of screening colonoscopies in which any polyp is detected. Black bars indicate the proportion of procedures in which multiple (>1) polyps are detected. Analysis is show by level of GI endoscopy nurse experience (0–6 months vs > 6 months) for 3,631 screening colonoscopies performed by attendings at UNC Hospitals. Statistical testing performed with Chi-square.
On sub-analysis by histologic type, we found adenomas were detected in 23.5% of procedures (n = 250) staffed by less experienced nurses compared with 25.3 % of procedures (n = 646) staffed by more experienced nurses (p = 0.24). Similarly, advanced lesions were detected in 5.2% of procedures (n = 55) staffed by less experienced nurses compared with 5.1 % (n = 130) with more experienced nurses (p = 0.93). In contrast, hyperplastic polyps were detected in 17.5% of procedures (n = 186) with less experienced nurses and in 23.7% (n = 606) with more experienced nurses (p < 0.001). Odds ratios are presented in Table 3.
Table 3.
Multivariate analysis of nursing experience and polyp detection*
| OR (95% CI)
|
|
|---|---|
| Primary outcomes: | |
| For any polyp detected | |
| Crude estimate | 1.26 (1.09, 1.46) |
| Fully adjusted model† | 1.15 (0.95, 1.40) |
| Minimally adjusted model‡ | 1.16 (1.00, 1.35) |
| For multiple polyps detected | |
| Crude estimate | 1.54 (1.29, 1.84) |
| Fully adjusted model† | 1.56 (1.23, 1.97) |
| Minimally adjusted model‡ | 1.39 (1.16, 1.67) |
| Secondary outcomes: | |
| For adenomas | |
| Crude estimate | 1.10 (0.93, 1.30) |
| Fully adjusted model† | 1.03 (0.87, 1.23) |
| For advance lesions | |
| Crude estimate | 0.99 (0.71, 1.39) |
| Fully adjusted model† | 1.20 (0.77, 1.85) |
| For hyperplastic polyps | |
| Crude estimate | 1.47 (1.22, 1.76) |
| Fully adjusted model† | 1.35 (1.12, 1.62) |
Multivariate analysis performed using logistic regression with an analysis of covariance strategy; ORs represent the odds of not detected polyp(s) in procedures staffed by nurses with 0–6 months of GI endoscopy nursing experience compared with nurses with > 6 months of experience.
Adjusted for age, gender, bowel preparation, body mass index, reaching the cecum, colonoscopy withdrawal time, and physician procedure volume during the study time frame.
Adjusted for physician procedure volume only.
For both the primary and secondary outcomes, the multivariate analysis did not substantially change these results (Table 3). For detecting any polyp, the OR for a model adjusted for only physician procedure volume was 1.16 (95% CI 1.00, 1.35), essentially identical to the OR for the model adjusted for all potential confounders including patient age, gender, BMI, bowel preparation quality, reaching the cecum, withdrawal time, and physician procedure volume. This indicates that the majority of confounding was due to physician procedure volume alone. For detecting multiple polyps, the OR for the fully adjusted model was very similar to the crude (1.56 vs 1.54), indicating little confounding. On sub-analysis by histology type, this overall effect seemed to be explained by detecting hyperplastic lesions (ORadjusted = 1.35, 95% CI: 1.12, 1.62) as opposed to adenomas (ORadjusted = 1.03, 95% CI: 0.87, 1.23) or advanced lesions (ORadjusted = 1.20, 95% CI: 0.77, 1.85).
Discussion
This study found that during screening colonoscopies performed by experienced attending physicians, the odds of not detecting polyps were mildly increased in procedures staffed by less experienced nurses compared to procedures staffed by more experienced nurses. Further, this effect persisted after controlling for patient, endoscopist, and procedural factors known to be associated with polyp detection. On sub-analysis by histologic polyp type, however, this effect seemed to be explained by increased detection of hyperplastic, rather than adenomatous, lesions.
To our knowledge, the effect of nurse experience on colorectal polyp detection has not been previously reported in the literature, so we are unable to compare our results directly to any other study. Analogous studies in other procedural fields such as cardiology, interventional radiology, or surgery have not been performed either. Our group has previously shown, however, that GI endoscopy nurse inexperience is associated with selected colonoscopy outcomes, including immediate procedural complications, prolonged cecal intubation times, decreased cecal intubation rates, and prolonged total procedure times,20, 21 and these findings would be consistent with those observed here.
How important is this finding? The absolute difference in any polyp detection between experienced and inexperienced nurses was modest, at about 6% for any polyp and 7% for multiple polyps. However, this does represent a 14% increase in polyp yield. More importantly, given the large numbers of screening colonoscopies performed every day, even modest increases in polyp yield result in very large absolute numbers of subjects in whom a polyp is (or is not) detected. Taken from a public health context, a 6% increase in yield may result in hundreds of thousands of subjects. Even though our increased yield was largely due to detection of hyperplastic lesions in this study, given the recent data on the importance of detecting flat polyps,24 there may be clinical importance to finding an increased yield of small polyps. During our study time frame, however, it had not yet become standard to describe whether polyps were flat or not, so we were unable to analyze this factor.
A strength of this study was the careful characterization of nurse experience. The amount of experience nurses had in a GI procedures unit was definitively known for the newly hired nurses during the study period (none had prior experience elsewhere). For the established nurses, start dates were determined from employment records, and because these nurses had more than 6 months of experience and we used a binary exposure, the chance that they were classified correctly was high. Additionally, based on previous work we considered 6 months to be the a priori cut point for nurse experience.21 We did perform a post-hoc sensitivity analysis, however, looking at a number of cut-points for nurse experience, and the 6 month point appeared to be a threshold level above which detection rates remain relatively constant (data not shown).
Misclassification of polyp detection was unlikely. Every screening colonoscopy over the study period was reviewed, and there were no missing data for the outcome. While the information in electronic/clinical endoscopy databases is subject to the quality of physician entry, it is unlikely that there were polyps that were detected but not documented; the entire goal of screening colonoscopy is polyp detection. Another check on the quality of the data was that polypectomy was performed for essentially every polyp detected; there were no polypectomies documented for procedures without polyps also documented. Our primary outcome was to focus on real-time detection of all polyps, regardless of pathologic type and size; with the current technology and equipment in our unit, it is not yet standard practice to attempt to make a pathologic diagnosis on optical/endoscopic appearance alone. Because this could be considered a limitation of the study, we also were able to obtain histologic characterization of nearly every polyp removed and to perform a sub-analysis by histology type. Overall however, we would argue that the key clinical issue is not the size and type of polyps that were detected, but the size and type of polyps that were missed. By definition though, because a polyp is missed, there is no way to know the details about that polyp.
Even though this was a single center study, findings on bivariate analysis in our data were consistent with findings reported in the literature.6–11, 16–19 First, we found that polyp detection was associated with male sex, increased age, higher BMI, better bowel preparation, higher cecal intubation rates, and increased withdrawal times. Our overall polyp detection rate of 44% is high, but certainly within the realm of clinical practice and rates reported in the literature,25, 26 and our adenoma detection rate of 25% meets the goal set by the U.S Multi-Society Task Force on Colorectal Cancer.5
An additional limitation of this study results from using logistic regression used to estimate the odds ratio (OR). When the outcome of interest is common, as it is here, the OR tends overestimate the risk ratio (RR).27 To assess this, we performed a sensitivity analysis using alternative methods (ie binomial regression) to estimate the RR and our results were not substantially changed. This is likely because the overall magnitude of effect, particularly after controlling for confounding factors, is relatively modest. A final limitation was this study’s retrospective design; definitive evidence to support our findings would require a prospective trial.
Our results confirm the common sense expression that “two pairs of eyes are better than one,” which is probably the most straightforward way to interpret our results. Nurses who are new to a GI procedures unit may not initially know how to recognize the endoscopic appearance of polyps or may not feel confident in pointing out a possible finding that the colonoscopist may not have seen. They may also be more focused on performing their responsibilities during the procedure such as sedation, monitoring, and assisting with biopsies or polypectomies than on watching for findings on the monitor. Conversely, more experienced nurses may be more comfortable in pointing out possible findings, and are also better at multi-tasking during the procedure. They may also be better at more effective sedation, patient positioning, or application of abdominal pressure, all of which might help with ease of colonoscopy, cecal intubation, and more efficient detection of polyps. These hypotheses could be evaluated in future studies aimed at further explaining the effect observed here.
In conclusion, this study has shown that GI endoscopy nurse inexperience is associated with increased odds of not detected polyps during screening colonoscopy compared with more experienced nurses, and that this relationship holds even after adjusting for patient, procedural, and physician factors associated with polyp detection. However, on sub-analysis by histologic polyp type, this effect seemed to be explained by increased detection of hyperplastic, rather than adenomatous, lesions. These findings may have resonance with the current trend toward “pay-for-performance” in endoscopy reimbursement, and suggest a novel way to improve the quality of colorectal cancer screening programs that utilize colonoscopy. Further work will be needed to confirm our results, but if this effect is seen in other endoscopy units, GI endoscopy nurses training paradigms may need to be altered to help maximize rates of polyp detection. For example, perhaps multimedia visual aids, similar to those already available for endoscopists, could be part GI endoscopy nurse training as well. Additionally, focusing on procedures staffed by less experienced nurses, perhaps by alerting physicians, slowing down withdrawal times, or adding additional nurse support, may increase polyp detection rates and further improve the quality of screening colonoscopy.
Acknowledgments
This work is funded in part by grants from the National Institutes of Health training grant T32 DK007634 and P30 DK3497.
Abreviations
- BMI
body mass index
- GI
gastrointestinal
- OR
odds ratio
- RR
risk ratio
- UNC
University of North Carolina
Footnotes
Disclosures: No conflicts of interest pertaining to this study exist for any of the authors.
Data from this study were presented, in part, as an oral presentation at DDW, Washington D.C., May, 2007, and as a poster at the American College of Gastroenterology National Meeting, Philadelphia, PA, October, 2007.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Winawer S, Fletcher R, Rex D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology. 2003;124(2):544–60. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 2.Davila RE, Rajan E, Baron TH, et al. ASGE guideline: colorectal cancer screening and surveillance. Gastrointest Endosc. 2006;63(4):546–57. doi: 10.1016/j.gie.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med. 1992;326(10):658–62. doi: 10.1056/NEJM199203053261002. [DOI] [PubMed] [Google Scholar]
- 4.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977–81. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 5.Rex DK, Bond JH, Winawer S, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97(6):1296–308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman DA, Prindiville S, Weiss DG, Willett W. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. Jama. 2003;290(22):2959–67. doi: 10.1001/jama.290.22.2959. [DOI] [PubMed] [Google Scholar]
- 7.Terry MB, Neugut AI, Bostick RM, et al. Risk factors for advanced colorectal adenomas: a pooled analysis. Cancer Epidemiol Biomarkers Prev. 2002;11(7):622–9. [PubMed] [Google Scholar]
- 8.Almendingen K, Hofstad B, Vatn MH. Lifestyle-related factors and colorectal polyps: preliminary results from a Norwegian follow-up and intervention study. Eur J Cancer Prev. 2002;11(2):153–8. doi: 10.1097/00008469-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Wallace K, Baron JA, Karagas MR, et al. The association of physical activity and body mass index with the risk of large bowel polyps. Cancer Epidemiol Biomarkers Prev. 2005;14(9):2082–6. doi: 10.1158/1055-9965.EPI-04-0757. [DOI] [PubMed] [Google Scholar]
- 10.Kim SE, Shim KN, Jung SA, Yoo K, Moon IH. An association between obesity and the prevalence of colonic adenoma according to age and gender. J Gastroenterol. 2007;42(8):616–23. doi: 10.1007/s00535-007-2074-4. [DOI] [PubMed] [Google Scholar]
- 11.Almendingen K, Hofstad B, Vatn MH. Does high body fatness increase the risk of presence and growth of colorectal adenomas followed up in situ for 3 years? Am J Gastroenterol. 2001;96(7):2238–46. doi: 10.1111/j.1572-0241.2001.03942.x. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein C, Thorn M, Monsees K, Spell R, O'Connor JB. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61(1):72–5. doi: 10.1016/s0016-5107(04)02461-7. [DOI] [PubMed] [Google Scholar]
- 13.Harewood GC. Relationship of colonoscopy completion rates and endoscopist features. Dig Dis Sci. 2005;50(1):47–51. doi: 10.1007/s10620-005-1276-y. [DOI] [PubMed] [Google Scholar]
- 14.Marshall JB. Technical proficiency of trainees performing colonoscopy: a learning curve. Gastrointest Endosc. 1995;42(4):287–91. doi: 10.1016/s0016-5107(95)70123-0. [DOI] [PubMed] [Google Scholar]
- 15.Rex DK, Chadalawada V, Helper DJ. Wide angle colonoscopy with a prototype instrument: impact on miss rates and efficiency as determined by back-to-back colonoscopies. Am J Gastroenterol. 2003;98(9):2000–5. doi: 10.1111/j.1572-0241.2003.07662.x. [DOI] [PubMed] [Google Scholar]
- 16.Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355(24):2533–41. doi: 10.1056/NEJMoa055498. [DOI] [PubMed] [Google Scholar]
- 17.Rex DK. Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc. 2000;51(1):33–6. doi: 10.1016/s0016-5107(00)70383-x. [DOI] [PubMed] [Google Scholar]
- 18.Sanchez W, Harewood GC, Petersen BT. Evaluation of polyp detection in relation to procedure time of screening or surveillance colonoscopy. Am J Gastroenterol. 2004;99(10):1941–5. doi: 10.1111/j.1572-0241.2004.40569.x. [DOI] [PubMed] [Google Scholar]
- 19.Simmons DT, Harewood GC, Baron TH, et al. Impact of endoscopist withdrawal speed on polyp yield: implications for optimal colonoscopy withdrawal time. Aliment Pharmacol Ther. 2006;24(6):965–71. doi: 10.1111/j.1365-2036.2006.03080.x. [DOI] [PubMed] [Google Scholar]
- 20.Dellon ES, Lippmann QK, Galanko JA, Shaheen NJ. Nurse experience: A strong and previously unidentified predictor of screening colonoscopy complications. Gastroenterology. 2007;132 (Suppl 2):A129. [Google Scholar]
- 21.Dellon ES, Lippmann QK, Galanko JA, Shaheen NJ. Endoscopy nurse experience predicts screening colonoscopy procedure times and cecal intubation rates. Gastroenterology. 2007;132 (Suppl 2):A128. [Google Scholar]
- 22.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130(6):1872–85. doi: 10.1053/j.gastro.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Soetikno RM, Kaltenbach T, Rouse RV, et al. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008;299(9):1027–35. doi: 10.1001/jama.299.9.1027. [DOI] [PubMed] [Google Scholar]
- 25.Atkin W, Rogers P, Cardwell C, et al. Wide variation in adenoma detection rates at screening flexible sigmoidoscopy. Gastroenterology. 2004;126(5):1247–56. doi: 10.1053/j.gastro.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 26.Pinsky PF, Schoen RE, Weissfeld JL, Kramer B, Hayes RB, Yokochi L. Variability in flexible sigmoidoscopy performance among examiners in a screening trial. Clin Gastroenterol Hepatol. 2005;3(8):792–7. doi: 10.1016/s1542-3565(05)00286-7. [DOI] [PubMed] [Google Scholar]
- 27.Rothman KJ, Greenland S. Modern Epidemiology. 2. Philadelphia, PA: Lippincott Williams & Wilkins; 1998. [Google Scholar]