Abstract
Colchicine-induced leukopenia usually occurrs in intentional or accidental overdoses or inappropriate use in combination with intravenous and oral colchine; however, there have been several reports of hematologic toxicity in short-term and small-dose colchicine medication courses. We present two cases of leukopenia induced by colchicine use concurrent with immunosuppressants in Behçet's disease. We postulate that the mechanism of colchicine-induced leukopenia might be the destruction of circulating leukocytes and an inhibition of leukocyte production by the immediate and direct toxic effect of colchicine on idiosyncrasies unique to each patient. The concurrently administered immunosuppressant might decrease the threshold for hematologic toxicity of colchicine in the leukocytes and their precursor cells.
Keywords: Behçet's disease, colchicine, leukopenia
Sir, Behçet's disease (BD) is recurrent and long standing inflammatory disease which is hard to control in some patients. Colchicine appears to be a promising and safe drug for BD with infrequent or minor side effects.1 Common side effects of colchicine including diarrhea and gastrointestinal upset are mild and self-limited, however, severe reactions like leukopenia, aplastic anemia, confusion, azoospermia, alopecia, myopathy and chorea-like syndrome may occur.2 We present two cases of acute leukopenia after short-term use of colchicine in BD patients who were concurrently taking immunosuppresants.
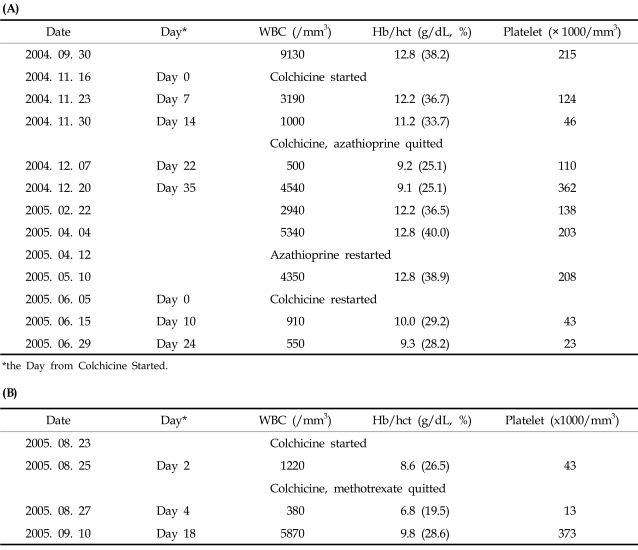
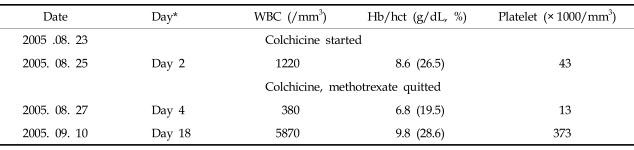
A 58-year-old Korean woman (case 1) who had been taking prednisolone and azathioprine for two years and a 71-year-old Korean woman (case 2) who had been taking methotrexate for three years. Both of them were diagnosed as incomplete type BD according to RCJ Criteria.3 Oral colchicine (1.2mg per day) was added to alleviate mucocutaneous symptoms, and leukopenia was discovered after adding oral colchicine, on 14th days in the first patient and 3rd days in the second patient. However, blood cell counts of both patients were recovered after cessation of colchine and immunosuppresants with conservative treatment with G-CSF (Table 1). In case 2, neither colchicine nor immunosuppresant administered afterward and her symptoms are well controlled only with sulfasalazine, aceclofenac and topical dexaltin currently. On the other hand, in case 1, prednisolone, analgesics and azathioprine were restarted 5 months later due to intractable BD, and regular laboratory studies showed no abnormalities. Uveitis and aphthous ulcer of the patient were not well controlled at that time, so oral colchicine (1.2mg per day) was added to her regimen again. Ten days after adding colchicine, the patient was readmitted due to septic shock and leukopenia and she was died despite intensive care.
Table 1.
Blood Cell Count in the Patient of Case 1 (A) and Case 2 (B)
*the Day from Colchicine Started.
It is assumed that colchicines was closely related in leukopenia of both patients even though the dose was small and the duration of colchicine use was short. Our patients had received immunosuppressant drugs for a few years without complications before taking colchicine, and the prompt discontinuation of colchicine resulted in recovery of the leukocyte count in both patients. In addition, the leukopenic event was repeated after the re-initiation of colchicine therapy in case 1. It is hard to conclude that leucopenia was caused by inhibiting microtubule assembly in mitosis by colchicine because the dose of colchicine was too small and leukopenia developed very rapidly after the administration.2 Bone marrow cellularities and leukocyte counts were decreased and leukocytes with abnormal morphology appeared in peripheral blood in both of our patients. So the immediate destruction of leukocytes with an accompanying inhibition of leukocyte production might have been caused by the direct toxic effect of colchicines and it could be the mechanism of colchicine-induced acute leukopenia superimposed on idiosyncrasies. Proposed mechanisms of acute colchicine-induced leukopenia were decreased clearance of the drug in the patients with underlying hepatic or renal dysfunction, drug interaction of colchicine with some drugs which inhibit P-glycoprotein, and concurrent viral infection.4,5 However, our patients did not have any evidence of hepatic dysfunction, renal dysfunction or usage of drugs which inhibit P-glycoprotein. And serologic tests for cytomegalovirus, rubella virus, measles virus, Ebstein-Barr virus, human immunodeficiency virus and varicella zoster virus were negative. We propose that immunosuppresants might decrease the threshold for the idiosyncratic reaction of colchicine in leukocytes and precursor cells. In fact, it is well known that those cells which are chronically exposed to immunosuppressant are vulnerable to the toxicity of other drugs and infections, and also the concentration of colchicine and immunosuppresants of the leukocytes and precursor cells are higher than the concentration of serum due to much slower clearance of the compound.6,7
We share our case to highlight colchicines use in the patients taking immunosuppressant can induce acute leukopenia which is acute, unpredictable and may be irreversible and life-threatening. We propose that any patient who is treated with colchicine may be at risk of hematologic toxicity and should be monitored frequently, especially in case of concurrently using immunosuppressants as well as other drugs known to have interactions with colchicine. In addition, prompt administration of G-CSF must be considered in the patient with colchicine-induced leukopenia, because the administration of G-CSF is known to be very useful and effective treatment regardless of whether colchicine-induced leukopenia is caused by overdose or long-term treatment or an idiosyncratic reaction.8,9
Table 2.
Blood Cell Count in the Patient of Case 2
*the day from Colchicine started.
References
- 1.Andrews J, Haskard DO. Current management options in Behçet's disease. Minerva Med. 2002;93:335–345. [PubMed] [Google Scholar]
- 2.Neuss MN, McCallum RM, Brenckman WD, Silberman HR. Long-term colchicine administration leading to colchicine toxicity and death. Arthritis Rheum. 1986;29:448–449. doi: 10.1002/art.1780290324. [DOI] [PubMed] [Google Scholar]
- 3.Bello YM, Phillips TJ. Management of venous ulcers. J Cutan Med Surg. 1998;3(Suppl 1):6–12. [PubMed] [Google Scholar]
- 4.Ben-Chetrit E, Navon P. Colchicine-induced leukopenia in a patient with familial Mediterranean fever: the cause and a possible approach. Clin Exp Rheumatol. 2003;21(4 Suppl 30):S38–S40. [PubMed] [Google Scholar]
- 5.Rollot F, Pajot O, Chauvelot-Moachon L, Nazal EM, Kélaïdi C, Blanche P. Acute colchicine intoxication during clarithromycin administration. Ann Pharmacother. 2004;38:2074–2077. doi: 10.1345/aph.1E197. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph SA, Greengard P, Malawista SE. Effects of colchicine on cyclic AMP levels in human leukocytes. Proc Natl Acad Sci U S A. 1977;74:3404–3408. doi: 10.1073/pnas.74.8.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace SL, Ertel NH. Occupancy approach to colchicine dosage. Lancet. 1970;2:1250–1251. doi: 10.1016/s0140-6736(70)92206-3. [DOI] [PubMed] [Google Scholar]
- 8.Folpini A, Furfori P. Colchicine toxicity clinical features and treatment. Massive overdose case report. Clin Toxicol. 1995;33:71–77. doi: 10.3109/15563659509020219. [DOI] [PubMed] [Google Scholar]
- 9.Critchley JA, Critchely LA, Yeung EA, Young RP, Young RJ, Chan TY, et al. Granulocyte-colony stimulating factor in the treatment of colchicine poisoning. Hum Exp Toxicol. 1997;16:229–232. doi: 10.1177/096032719701600413. [DOI] [PubMed] [Google Scholar]