Abstract
Purpose
To examine the efficacy of cognitive-behavioral therapy (CBT) for the prevention of postpartum depression (PPD) in "at risk" women.
Materials and Methods
We recruited 927 pregnant women in 6 obstetric and gynecology clinics and screened them using Beck Depression Inventory (BDI). Ninety-nine of the screened women who had significantly high scores in BDI (a score above 16) were selected for the study. They were contacted through by telephone, and 27 who had consented to participate in the study were interviewed via SCID-IV-I. Twenty-seven eligible women were randomly assigned to the CBT intervention (n = 15) and control condition (n = 12). All participants were required to complete written questionnaires, assessing demographic characteristics, depressive symptoms, negative thoughts, dyadic communication satisfaction, and global marital satisfaction prior to treatment and approximately 1 month postpartum. The 15 women in the CBT condition received 9 bi-weekly 1-hour individual CBT sessions, targeting and modifying negative patterns of thinking and behaviors occurring in the context of the dyadic relationship.
Results
The analysis of covariance (ANCOVA) showed that there were significant differences in all postpartum measures between the 2 groups, indicating that our antenatal intervention with CBT was effective in reducing depressive symptoms and improving marital satisfaction, which lasted until the postpartum period.
Conclusion
Our pilot study has provided preliminary empirical evidence that antenatal CBT intervention can be an effective preventive treatment for PPD. Further study in this direction was suggested.
Keywords: Cognitive behavioral therapy, postpartum depression, prevention
INTRODUCTION
Women with PPD complain of depressive mood, insomnia, frequent crying, lack of appetite and motivation, fatigue, and multiple somatic symptoms, inability to cope, low self-esteem, and suicidal ideation. The reported prevalence of PPD is variable, with rates ranging from 5 to 25%, depending on the measures used. According to a meta-analysis of 59 studies, the prevalence rate of depression was 14% by diagnostic interview, which is similar to the value of 12% obtained by self-reporting measurements.1 Although the majority of PPD are spontaneously recovered within the first few months after birth,2 more than half of women with PPD continue to experience episodes of depression beyond the first postpartum year. Women with prolonged PPD are likely to have insecurely attached to their infants, and reported more negative perceptions of their infants.3 Observational research shows that infants and children of depressed mothers compared to children of non-depressed mothers are fussier, receive lower scores on measures of intellectual and motor development, and have more difficult temperaments and less secure attachments to their mothers. Infants and children of depressed mothers also react more negatively to stress show delayed development of self-regulatory strategies, and exhibit poorer academic performance, fewer social competencies, lower levels of self-esteem, and higher levels of behavioral problems.4 Consequently, point prevalence rates of psychiatric disorders among children of depressed parents have been estimated to be 2 - 5 times above normal at 41 - 77%.5,6 In addition, PPD has been linked to elevated rates of depression in spouses,7 and 50 - 70% of depressed women report that they experience marital problems and conflict. Therefore, left untreated, PPD causes not only considerable distress to women inflicted with this disorder but also yields more serious consequences of marital relationships and child-caring capacity. After birth relapse, the occurrence of depression and its recurrence are common.8 Although it is widely known that a substantial number of women are suffering from PPD, most of them seldom seek professional help.
The most common risk factors cited for PPD include depressed mood during pregnancy, lack of partner support, and low self-esteem.9,10 Especially, more than half of the women previously depressed in the postpartum period are at risk of developing depression again. Given the recurrent nature of depression, the antenatal period offers a window of opportunity during which a preventative approach to this serious condition can be instituted to high risk women during routine visits to the obstetric clinics. There have been 6 randomized controlled trials examining the effectiveness of antenatal group intervention aimed at preventing PPD in high risk women. The majority of the studies used psycho-educational group intervention delivered by non-specialist mental health professionals and found the intervention to be overall ineffective.11,12 The lack of positive effects suggests that presenting psycho-educational intervention in a group format by non-specialist mental health professionals may not be an optimal preventive strategy. It is of interest to note that positive outcomes were reported by 1 study using a validated structural intervention (IPT) delivered by a clinical psychologist in contrast to psycho-educational group intervention.13 In a recently published study, the CBT group intervention delivered by a clinical psychologist was found to be effective in reducing depressive symptoms in a perinatal period, however they failed to produce superior outcomes compared to "non-specific" booklet control condition.10 Given that CBT in a standard form is administered by clinical psychologists over 16 sessions, the poor outcome in this study might be attributable to the fact that they used a briefer CBT, focusing more on the behavioral rather than cognitive components of CBT.13 These findings suggest that specific intervention at a full dosage delivered by a specialist is necessary to bring about changes in depressive symptoms and behaviors to achieve the prevention of PPD.
Currently, 50 - 70% of depressed pregnant women reported that they had experienced marital problems and conflicts.1 These studies suggest that marital therapy or therapy dealing with marital conflict would be effective in preventing PPD. Some studies have reported that the level of depressive symptoms predicts later marital distress of depressed people as well as their partners, and depressive episodes prior to marriage may bring about increased risk of subsequent marital discord.14,15 Therefore, intervention seems to be desperately needed for improving marital relationships. For buffering negative events related to marital discord and alleviating depression, 5 types of positive and supportive behaviors of the partner are potentially important: spending quality time together, listening positively, acquiring support and boosting self-esteem and building intimacy. Once depressed women perceive the positive and supportive behavior from their spouse, the level of depression seems to decrease over time. Accordingly, marital intervention for depressive women has a strong foundation upon which to build. Until recently, studies have shown that preventive intervention is not sufficiently effective for reducing PPD. However, it would be possible that a full dosage intervention with specific dyadic component added to traditional CBT and delivered by a specialist can bring changes in depressive symptoms and behaviors to prevent PPD.
In this study, we maintained the basic tenet of cognitive-behavioral treatment and used the techniques of CBT for depression but focused on marital conflicts when dealing with negative thought and used behavioral techniques to improve marital relationships.16-18 The aim of this study was to investigate whether our CBT intervention was effective in improving depressive symptoms and marital relationships of pregnant depressive women and also in preventing PPD.
MATERIALS AND METHODS
Sample and sampling technique
Pregnant women receiving prenatal care at 3 Departments of Obstetrics and Gynecology at the University Medical Center and 2 private obstetric clinics were recruited. In the late second or early third trimester, an obstetrician/gynecologist introduced a paper sheet with our CBT program to the pregnant women to measure the risk of PPD. Pregnant women who perceived themselves in depressive state voluntarily filled out the BDI. Although BDI was originally developed as a general depression instrument to measure clinical depression, it has widely been used in PPD research for the past 4 decades.19,20 Moreover, because we needed to measure depression symptom levels not only during the pregnant period but also after birth, BDI seemed to be of the most appropriate inventories for the purpose of our study. Among 927 women, 99 who scored more than 16 points in BDI were asked to participate in a clinical phone call interview and only those wanted to participate in the study were interviewed by the first author(HJC) via SCID-I (Structured Clinical Interview for DSM-IV-I). Women who participated in the study were diagnosed as depressive disorder (major depressive disorder, dysthymic disorder, depressive disorder NOS) through the clinical interview. Depressive disorders due to alcohol abuse, bipolar disorder, organic brain disorder, and obstetric complications were excluded from our study.
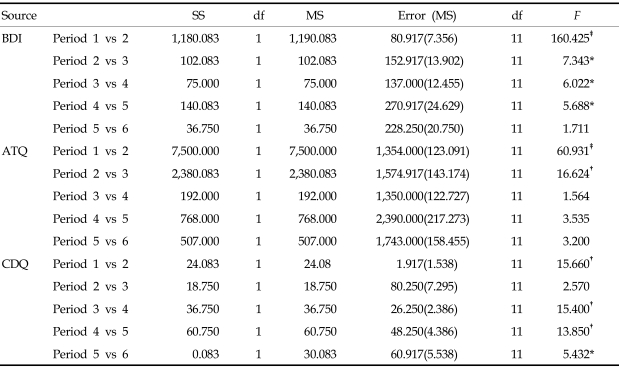
Finally, 27 eligible women were randomly assigned to either the CBT intervention (n = 15) or control condition (n = 12). A pre-post treatment design was used to collect data to pilot testing the effect of CBT intervention for preventing PPD. Prior to treatment and at 1 month after child birth that questionnaires were administered to all participants. Twelve of 15 women in the CBT group attended all therapy sessions and completed all assessments. Among 3 participants who dropped out of the treatment, 1 dropped out after the first 2 sessions due to premature delivery, 1 withdrew because she no longer felt depressed after 3 sessions, and 1 ultimately quit after frequent absences. Ten of 12 women in the control group completed the postpartum assessment and the other 2 participants did not return the survey sheet by mail. Participants were on average 29 years (SD : 3.4) and in their 29th week of pregnancy (SD : 5.9). All participants had more than 12 years of educational background and most of them were housewives (63.6%). There were 8 participants with major depression disorder, 3 with for dysthymic disorder, and 11 with depression disorder NOS (Fig. 1).
Fig. 1.
Participant rates at each stage of the trial.
Procedure
The preventive intervention consisted of 1-hour bi-weekly sessions of cognitive behavioral therapy, focusing on improving depressing mood and dysfunctional marital relationships in the context of pregnancy. Since all participants were pregnant women, therapy could not be carried on longer than 1-hour bi-weekly sessions, because of the mother's condition and convenience. To ensure program consistency, CBT intervention was developed into a manual format. The intervention was administered individually to 15 women by the first author, a licensed clinical psychologist in Korea. All contents of the 9 intervention sessions were audio-taped and supervised weekly using face-to-face by the second author, a licensed international supervisor for CBT. She reviewed the audiotape to ensure consistent adherence according to the manual and discussed the intervention with the first author. The components of CBT included educating participants about depression, scheduling pleasant events, and changing negative automatic thoughts to positive ones. Components of marital intervention consisted of promoting acceptance through better understanding of the personalities of their spouses through MBTI, improving communication skills of I-message training by the professional, and making and exchanging a list of rewarding positive behaviors from their spouses.
Sessions 1, 2, and 3 focused on education about depression, goal-setting, and increasing pleasurable activities. In sessions 4 - 6, participants were individually taught cognitive restructuring techniques in order to help them identify and challenge irrational or overly negative thoughts, with a special focus on thoughts related to marital interaction. Sessions 7 - 9 focused on helping participants improve marital relationships. Communication skills training and behavioral exchange exercises were taught, and acceptance of their spouses was promoted. In the final session, plans for follow up were discussed. On the other hand, the control group was educated about depression and strategies to control symptoms of depression in 1 session during the pretest period, and they assessed only questionnaires related to depression 1 month after child birth by mail.
Questionnaires
Depressive symptoms
A 21-item version of the Korean version of BDI21 was utilized as a self-reporting measure of depressive symptoms. BDI has a 21-item self-reporting scale that assesses the severity of depressive symptoms over the past week. Its reliability and validity as a depressive symptom measure have been documented. In our samples, Cronbach's α was 0.82.
Automatic thoughts
The Automatic Thought Questionnaire (ATQ) developed by Hollen and Kendall22 and translated by Ha18 was used in this study. The ATQ consisted of 30 statements reflecting negative cognitions (e.g. "I feel like I'm up against the world"). Respondents are asked to rate the frequency at which each self-statement or a similar self-statement occurred over the course of the past week. Each item is scored from 0 to 4 in order to determine the severity of symptoms. High scores represent large numbers of negative thoughts. In our sample, Cronbach's α was 0.93.
Dyadic communication dissatisfaction
The emotional communication dissatisfaction scale and the problem-solving communication dissatisfaction scale of the Korean version of Snyder's Marital Satisfaction Inventory-R23 were used to assess subjective dissatisfaction in dyadic communication.24 The emotion and problem-solving communication dissatisfaction subscale are composed of 13 and 19 items, respectively. Altogether, these 2 scales consisted of 32 items in a yes-or-no answer format. In our sample, the value of Cronbach's α used for these 2 subscales were 0.85, and 0.87 respectively.
Global marital dissatisfaction
The global marital dissatisfaction scale of the Korean version of Snyder's Marital Satisfaction Inventory-R was used.24 The MSI-R consisted of a broad range of dimensions in marriage since they relate to global marital satisfaction. The GDS of the MSI-R consisted of 22 items in a yes-or-no answer format that measured global marital dissatisfaction. In our sample, Cronbach's α was 0.87.
Data analysis
We compared the CBT intervention group to the control group in regards to depression, automatic thoughts, communication satisfaction, and general marital satisfaction before the treatment and 1 month after their parturition. In order to control pretreatment differences, we performed ANCOVA, in which the pretreatment score was used as the covariate. Finally, within-subjects contrast analyses were used to examine how depressive symptoms, automatic thoughts, and communication satisfaction changed in each phase of treatment.
RESULTS
Demographic variables
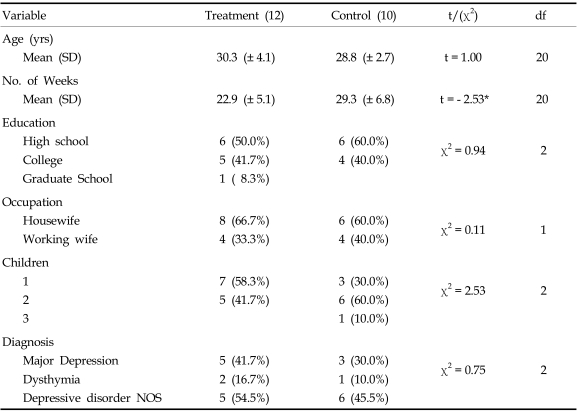
The demographics of the CBT intervention and control groups are shown in Table 1. The CBT and control group did not show any significant differences in diagnosis, average age, education level, employment, or number of children. With regard to the diagnosis based on SCID-I, the treatment group was composed of 5 participants with major depressive disorder (41.7%), 2 with dysthymic disorder (16.7%), and 5 with depressive disorder NOS (54.5%). The control group had 3 individuals with major depression (30%), 1 with dysthymic disorder (10%) and 6 with depressive disorder NOS (45.5%). There was a significant difference only in the length of gestation; 22.9 weeks for women in the treatment group and 29.3 weeks in the control group, t (12, 10) = - 2.53, p < 0.05.
Table 1.
Characteristics of Subjects in the Treatment and Control Groups
SD, standard deviation; NOS, not otherwise specified; df, degree of freedom.
*p < 0.020.
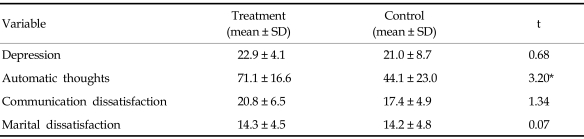
Pretreatment comparison between the CBT and control groups
We compared the data obtained in the pretreatment assessment to examine the homogeneity of the 2 groups (Table 2). According to the t-tests, the 2 groups did not exhibit any significant differences in terms of depression, communication dissatisfaction, or general marital dissatisfaction. However, a significant difference was found in automatic thoughts with the treatment group scoring higher [71.1(SD : 16.6)] than the control group [44.1(SD : 23)] ; t (12, 10) = 3.20, p < 0.01 (Table 3).
Table 2.
Pretreatment Comparison between the 2 Groups
*p < 0.004.
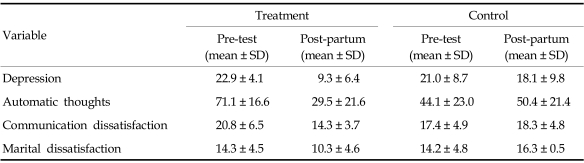
Table 3.
Pre-Treatment and Postpartum Comparison between the 2 Groups
Rates of depression in the postpartum period
Participants who received CBT intervention had a lower rate of PPD when estimated by a self-report measure (score of 16 or higher in BDI; 18.3%) than women with depression in the control group (score of 16 or higher in BDI; 30%).
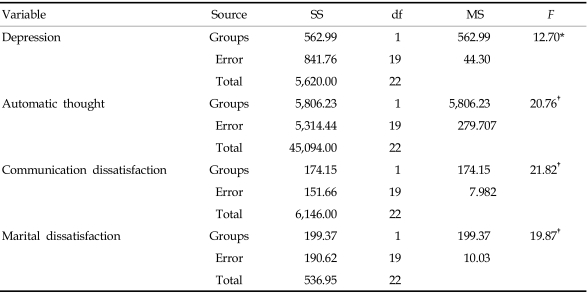
Outcome analyses: efficacy of CBT
Taking the pre-treatment depression score as the covariate, we performed ANCOVA on the PPD score (Table 4). The result, showed a significant difference between the treatment and control groups [F (1, 19) = 12.71, p < 0.01], indicating that the treatment was effective in reducing PPD. The results of separate ANCOVAs indicated that there were significant differences between the 2 groups in automatic thoughts [F (1, 19) = 20.76, p < 0.001], communication dissatisfaction [F (1, 19) = 21.82, p < 0.001], and marital dissatisfaction [F (1, 19) = 19.7, p < 0.001]. These results demonstrated that our intervention with CBT for pre-partum depressive women was effective in reducing depressive symptoms and had an enduring effect that lasted until the postpartum period.
Table 4.
ANCOVA on Dependent Measures between the 2 Groups
ANCOVA, analysis of covariance; SS, sum of square; df, degree of freedom; MS, mean squared.
*p < 0.006, †p < 0.001.
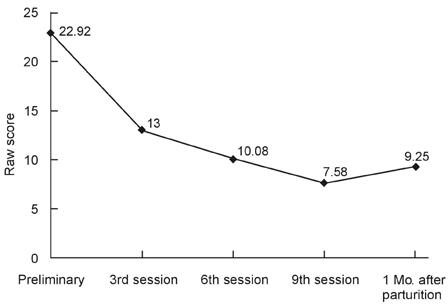
Contrast analyses by treatment phase in the treatment group
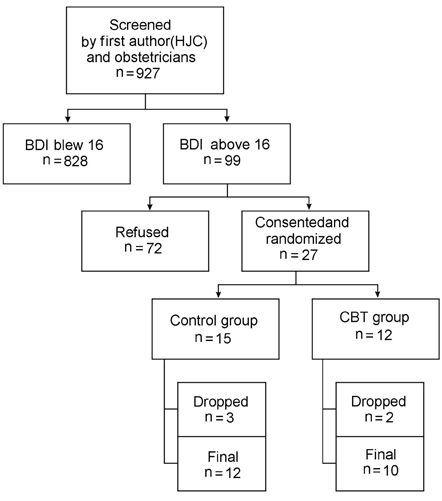
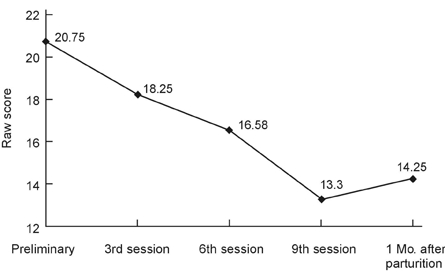
We performed within-subjects contrast tests in order to examine the progress of change as a function of the treatment phase, and found significant differences in BDI scores between the pre-treatment and 3rd sessions (1st phase), between the 3rd (1st phase) and 6th sessions (2nd phase), between the 6th (2nd phase) and 9th sessions (post-treatment), and between the 9th (post-treatment) and postpartum period, indicating that depressive symptoms decreased continuously until the postpartum period. Automatic thoughts decreased between the pre-treatment and 3rd sessions, and between the 3rd and 6th sessions. This finding indicated that negative automatic thoughts decreased significantly during the first 2 phases of therapy in which negative automatic thoughts were extensively dealt with. Finally, we found significant differences in communication and marital dissatisfaction score between the preliminary and 3rd sessions, between the 6th and 9th sessions, and between the 9th session and postpartum period, indicating that communication and marital dissatisfaction decreased continuously until the postpartum period (Table 5), (Figs. 2, 3, 4, and 5).
Table 5.
Contrasts Test by Evaluation Period of the Treatment Group
SS, sum of square; df, degree of freedom; MS, mean squared; BDI, beck depression inventory; ATQ, automatic thought questionnaire; CDQ, communication dissatisfaction.
*p < 0.045, †p < 0.002, ‡p < 0.001.
Fig. 2.
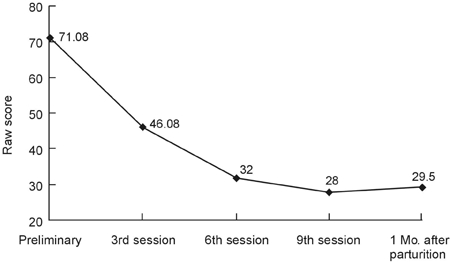
Changes in depression by evaluation period.
Fig. 3.
Changes in automatic thought by evaluation period.
Fig. 4.
Changes in communication dissatisfaction by evaluation period.
Fig. 5.
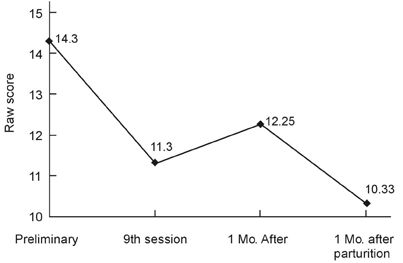
Changes in marital dissatisfaction by evaluation period.
DISCUSSION
In this study, we examined whether brief individual CBT intervention tailored to meet the needs of depressive pregnant women could prevent PPD. This CBT intervention consisted of standard CBT components for depression and components of enhancing marital relationships. It was found that CBT intervention resulted in a significant improvement in depressive symptoms compared to the control group as measured by BDI. We also found that CBT intervention was effective in reducing negative automatic thoughts, dyadic communication dissatisfaction, and global marital dissatisfaction. For the majority of the outcome measures, the control group did not exhibit any significant differences compared to the treatment group either before or after parturition.
This finding is in contrast with a previous finding in which brief CBT intervention did not produce superior outcomes compared to the control condition. Although some of studies failed to find any beneficial effects of such interventions,25,26 the present study demonstrated that providing prenatal intervention can be effective in reducing depressive symptoms not only during the perinatal period but also after birth. More successful outcome in our study might have been due to the fact that the CBT was administered individually and at full dosage. Thus, tailored individual intervention with CBT appears to be more effective to pregnant women than group CBT.27 In group CBT sessions, personal states such as pregnancy fatigue, condition of an unborn child, and dissatisfaction from their partner should not be talked. This course was especially tailored to accommodate the needs of pregnant women and new mothers by teaching strategies of the cognitive and behavioral mood regulation and correcting negative thoughts during depressive periods. In addition, we provided depressive women with effective communication skills to enhance marital relationships. Participants who received CBT intervention exhibited an improvement in marital relationship, even after childbirth, whereas control group participants showed increased dissatisfaction in their marriages. It is likely that the therapeutic intervention designed to improve the quality of the participant's marital relationship played an important role in preventing PPD. This improvement of marital satisfaction was achieved through therapeutic intervention, which involved the review and modification of dysfunctional cognition in the marital relationship by promoting acceptance of the spouse's characteristics and exchanging positive reinforcement techniques.
The limitations of this study are as follows; First, the small number of participants in this study limits the generalization of the positive outcome of CBT intervention. Second, we could not administer post-treatment assessment to the control group in order to maximize the response rate of postpartum assessment, and therefore, post-treatment differences were not examined between the 2 groups. Since the majority of outcome measures in the control group did show high level of pre-treatment scores postpartum, it is likely that their depressive symptoms were maintained at post-treatment. However, the possibility remains that depressive symptoms of the control participants disappeared at post-treatment and then increased again postpartum. Third, only the self-report measure was administered as postpartum assessment. Although BDI is widely being used in PPD, BDI and EPDS (Edinburgh Postnatal Depression Scale) are positively correlated,28 Furthermore, BDI is not a specific instrument for measuring PPD. High BDI scores might not necessarily mean that PPD is clinically diagnosed. Thus, in future research, not only self-report measures but also structured clinical interviews need to be used for postpartum assessment to check for the presence of major depressive disorder at postpartum.
Despite these limitations, our results demonstrated the efficacy of brief individual CBT intervention in preventing PPD. Although PPD poses serious mental health problems to mothers and infants, no attempts have been made to develop an effective preventive approach in Korea. We developed an appropriate treatment for depressed pregnant women who are likely to develop PPD and examined its efficacy on a small scale. The results obtained so far are encouraging. A shorter duration of preventive approach can be more effective than treatment that is administered after the onset of depression, and this may in turn exert a positive carry-on effect on households or social economy. Moreover, preventing depression for nursing mothers helps not only the psychological well-being of the mothers but also the entire family. It has been documented that many children who are reared by a depressed mother display psychological and behavioral disorders in middle childhood.29,30 If the findings of this pilot study would be replicated in a larger trial, it would greatly contribute to promotion of women's public health.
References
- 1.O'Hara M, Swain AM. Rates and risks of postpartum depression: A meta-analysis. Int Rev Psychiatry. 1996;8:37–54. [Google Scholar]
- 2.Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression. Br J Psychiatry. 2003;182:412–419. [PubMed] [Google Scholar]
- 3.Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kowalenko N, Tennant C. Postnatal depression and infant cognitive and motor development in the second postnatal year: The impact of depression chronicity and infant gender. Infant Behav Dev. 2005;28:407–417. [Google Scholar]
- 4.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 5.Beardslee WR, Keller MB, Lavori PW, Staley J, Sacks N. The impact of parental affective disorder on depression in offspring: a longitudinal follow-up in a nonreferred sample. J Am Acad Child Adolesc Psychiatry. 1993;32:723–730. doi: 10.1097/00004583-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Beardslee WR, Versage EM, Gladston TR. Children of affectively ill parents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Cutrona CE. Social support and stress in the transition to parentghood. J Abnorm Psychol. 1984;93:378–390. doi: 10.1037//0021-843x.93.4.378. [DOI] [PubMed] [Google Scholar]
- 8.Phillipps LHC, O'Hara MW. Prospective study of postpartum depression: 4 1/2 year follow up of women and children. J Abnorm Psychol. 1991;100:151–155. doi: 10.1037//0021-843x.100.2.151. [DOI] [PubMed] [Google Scholar]
- 9.Zelkowitz P, Milet TH. Postpartum psychiatric disorders: their relationship to psychological adjustment and marital satisfaction in the spouses. J Abnorm Psychol. 1996;105:281–285. doi: 10.1037//0021-843x.105.2.281. [DOI] [PubMed] [Google Scholar]
- 10.Brown GW, Bifulco A, Andrew B. Self-esteem and depression III. Aetiological issues. Soc Psychiatry Psychiatr Epidemiol. 1990;25:235–243. doi: 10.1007/BF00788644. [DOI] [PubMed] [Google Scholar]
- 11.Spinelli MG. Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry. 1997;154:1028–1030. doi: 10.1176/ajp.154.7.1028. [DOI] [PubMed] [Google Scholar]
- 12.Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med. 2000;30:1273–1281. doi: 10.1017/s0033291799002937. [DOI] [PubMed] [Google Scholar]
- 13.Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal therapy-oriented group intervention. Am J Psychiatry. 2001;15:638–640. doi: 10.1176/appi.ajp.158.4.638. [DOI] [PubMed] [Google Scholar]
- 14.Cascardi M, O'Leary KD, Lawrence EE, Schlee KA. Characteristics of women physically abused by their spouses and who seek treatment regarding marital conflict. J Consult Clin Psychol. 1995;63:616–623. doi: 10.1037//0022-006x.63.4.616. [DOI] [PubMed] [Google Scholar]
- 15.Beach SRH, Sandeen EE, O'Leary KD. Depession in marriage: A model for etiology and treatment. New York: Guilford; 1990. pp. 53–83. [Google Scholar]
- 16.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Epstein N, Baucom DH, Rankin LA. Treatment of marital conflict: a cognitive-behavioral approach. Clin Psychol Rev. 1993;13:45–57. [Google Scholar]
- 18.Beach SR, Sandeen EE, O'leary KD. Depression in marriage: a model for etiology and treatment. New York: The Guilfrord Press; [Google Scholar]
- 19.Horowitz JA, Damato E, Solon L, Von Metzsch G, Gill V. Postpartum depression: issues in clinical assessment. J Perinatol. 1995;15:268–278. quiz 279-80. [PubMed] [Google Scholar]
- 20.Posner NA, Unterman RR, Williams KN, Williams GH. Screening for postpartum depression. An antepartum questionnaire. J Reprod Med. 1997;42:207–215. [PubMed] [Google Scholar]
- 21.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press; 1979. [Google Scholar]
- 22.Hollen SD, Kendall PC. Cognitive self-statements in depression: Development of an automatic thoughts questionnaire. Cognit Ther Res. 1980;4:383–395. [Google Scholar]
- 23.Snyder DK. Marital satisfaction inventory (MSI) Manual. Los Angeles: Western Psychological Service; 1997. [Google Scholar]
- 24.Kwon JH, Chae PK. A validation study of Korean marital satisfaction inventory. Korean J Clin Psychol. 1999;18:123–139. [Google Scholar]
- 25.Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med. 2000;30:1273–1281. doi: 10.1017/s0033291799002937. [DOI] [PubMed] [Google Scholar]
- 26.Hayes BA, Muller R, Bradley BS. Perinatal depression: a randomized controlled trial of an antenatal education intervention for primiparas. Birth. 2001;28:28–35. doi: 10.1046/j.1523-536x.2001.00028.x. [DOI] [PubMed] [Google Scholar]
- 27.Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ. 2005;331:1–8. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Affonso DD, De AK, Horowitz JA, Mayberry LJ. An international study exploring levels of postpartum depressive symptomatology. J Psychosom Res. 2000;49:207–216. doi: 10.1016/s0022-3999(00)00176-8. [DOI] [PubMed] [Google Scholar]
- 29.Beck CT. Maternal depression and child behaviour problems: a meta-analysis. J Adv Nurs. 1999;29:623–629. doi: 10.1046/j.1365-2648.1999.00943.x. [DOI] [PubMed] [Google Scholar]
- 30.Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]