Abstract
Purpose
Endobronchial tuberculosis (EBTB) presenting as right middle lobe syndrome (RMLS) is an uncommon clinical condition. We investigated the clinical characteristics in patients with EBTB presenting as RMLS.
Patients and Methods
We retrospectively reviewed the records of 22 patients with EBTB presenting as RMLS who were diagnosed at our hospital from 2003 to 2006.
Results
Its occurrence was more common in females than males (F, 18; M, 4). The mean age was 70.3 ± 8.5 years, and 17 patients were above the age of 65 years. Cough with sputum was the most common manifestation and 2 patients were asymptomatic. In bronchoscopic analysis, the most common finding was edematous-type EBTB, which was found in 15 patients, followed by actively caseating type in 6 and tumorous type in 1. Acid-fast bacilli (AFB) staining for bronchial washing fluid was positive in only 5 patients: 1 with edematous type and 4 with actively caseating type. Bronchoscopic biopsy showed chronic granulomatous inflammation in 16 patients. Follow-up chest X-ray after treatment showed complete disappearance of the lesion in 2 patients, more than 50% improvement in 5, less than 50% improvement in 5, and no change of lesion in 4.
Conclusion
Edematous-type EBTB was the most common type of EBTB presenting as RMLS, and it usually occurred in elderly patients. Culturing for mycobacterium and histologic examination by bronchoscopy are necessary for proper diagnosis in these patients.
Keywords: Endobronchial tuberculosis, right middle lobe syndrome
INTRODUCTION
Endobronchial tuberculosis (EBTB) is defined as a tuberculous infection of the tracheobronchial tree.1 It can affect any part of the tracheobronchial tree, however, it usually results in right middle lobe collapse,2 when EBTB involves the right middle lobe. When the right middle lobe is chronically or recurrently collapsed by certain pathologic conditions, it is called right middle lobe syndrome (RMLS).3 Because the right middle lobe has an anatomically narrowed orifice, it is easily obliterated by certain pathologic conditions, such as cancer or inflammatory conditions. RMLS is a relatively uncommon condition, and clinicians should perform diagnostic procedures to identify a cause. The literature dealing with causes of RMLS show that benign inflammatory diseases such as bronchiectasis or pneumonia are the most common causes while RMLS due to malignant diseases is relatively infrequent.3,4 There has been a recent report in Korea that showed that pulmonary tuberculosis, including EBTB is the most common cause of RMLS.5 The proportion of endobronchial involvement in active pulmonary tuberculosis is variable according to the literature.6 Recently, a prospective analysis of endobronchial involvement in patients with pulmonary tuberculosis has been reported. An et al. studied bronchoscopic findings in 458 patients showing active pulmonary tuberculosis. Among these patients, about 50% also showed EBTB, and the most common finding was edema-hyperemia type EBTB.7
EBTB is still a common disease in Korea. Nevertheless, EBTB presenting as RMLS is infrequently seen in clinical situations and it has been reported only as clinical cases,2 which are considered to have no distinctive clinical characteristics. Therefore, we herein report 22 cases of EBTB presenting as RMLS.
PATIENTS AND METHODS
Among patients with chest radiographs of RMLS who underwent bronchoscopy at Gyeongsang University Hospital from 2003 to 2006, we reviewed the medical records of those diagnosed with EBTB. One chest radiologist had confirmed the diagnosis of RMLS by chest radiography and CT scan, which showed a wedge-shaped density that extended anteriorly and inferiorly from the hilum.3,4 The diagnosis of EBTB was made primarily based on a mucosal change of bronchial lumen by bronchoscopy as well as identification of mycobacterium tuberculosis (MTB) in bronchial washing or expectorated sputum or chronic granulomatous inflammation with or without caseation necrosis in a biopsy specimen.8,9 In case of negative bacteriologic findings, we diagnosed it as EBTB when patients had a gross mucosal change with bronchoscopic findings and chronic granulomatous inflammation in a biopsy specimen.
We reviewed the clinical features and radiologic and bronchoscopic findings of these patients. Bronchoscopic findings of EBTB were rated according to Jung's classification.9 To evaluate change of a chest X-ray lesion with treatment, we compared a chest X-ray that was taken at the time of initial diagnosis to one taken after complete treatment. We also classified the change of a chest X-ray into complete disappearance of the lesion, more than 50% improvement, less than 50% improvement, and no lesion changed.
RESULTS
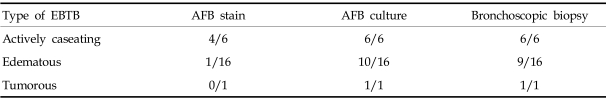
Eighteen women and 4 men were identified, and the age of the patients ranged from 48 to 81 years (mean age, 70.3 ± 8.5 years). Seventeen patients were older than 65 years of age. The chief complaints were cough, sputum, hemoptysis, dyspnea on exertion, and general weakness. Two patients were asymptomatic. Cough with sputum was the most common manifestation of the condition. Bronchoscopic findings showed actively caseating type in 6 patients, edematous type in 15, and tumorous type in 1. Acid-fast bacilli (AFB) staining for bronchial washing fluid was positive in only 5 patients: 1 with edematous type and 4 with actively caseating type. Bronchial washing fluid culture revealed growth of MTB in 16 patients, 10 with edematous type and 6 with actively caseating type. Chronic granulomatous inflammation in bronchoscopic specimens was seen in 16 patients; 9 with edematous type, 6 with actively caseating type, and 1 with tumorous type (Table 1). All patients were diagnosed by bronchial biopsy and/or MTB culture of bronchial washing fluid.
Table 1.
Diagnostic Yield of Microbiologic and Histologic Examination according to Type of Endobronchial Tuberculosis
EBTB, endobronchial tuberculosis; AFB, acid-fast bacilli.
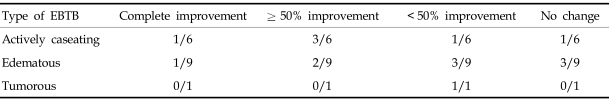
Radiographic findings showed the loss of right middle lobe volume in 9 patients, only consolidation in 10, consolidation with additional volume loss in 2, and mass-like density in 1. Follow-up chest radiographs were done in 16 patients after complete treatment. It showed complete disappearance of the lesion in 2 patients, more than 50% improvement in 5, less than 50% improvement in 5, and no lesion changed in 4. Actively caseating-type EBTB usually showed marked improvement of the lesion on a follow up chest X-ray, 4 out of 6 patients showed more than 50% improvement of the lesion. However, edematous-type EBTB usually showed persistent abnormality on chest X-ray; 6 out of 9 patients showed less than 50% improvement after treatment (Table 2).
Table 2.
Change of Middle Lobe Lesion on Chest X-ray after Treatment according to Type of Endobronchial Tuberculosis
EBTB, endobronchial tuberculosis.
Eighteen patients were treated with standard anti-tuberculous medication. It included INH, RFP, EMB, and PZA. Four patients were transferred to private clinics. Two patients developed severe drug eruption during treatment. The medication was changed to tarivid, EMB, prothionamide, cycloserine and INH, RFP, tarivid in each patient. The mean duration of treatment was 6.5 ± 1.8 months.
Follow-up bronchoscopy was done in 2 patients because chest X-ray did not improve despite 3 months of anti-tuberculous treatment. It showed fibrotic change of the middle lobe, edematous change, and some secretion in the middle lobe. Parenchymal pulmonary tuberculosis combined was found in 5 patients, and no patient had extrapulmonary tuberculosis. Oral prednisolone was taken with anti-tuberculous medication by 1 patient for the first 2 months of treatment.
DISCUSSION
In this study, we found that edematous EBTB was the most common type of EBTB presenting as RMLS, and bronchial washing alone had a low diagnostic yield in the confirmation of edematous-type EBTB.
Bronchoscopic findings in retrospective analysis revealed that actively caseating-type EBTB was the most common form of EBTB in 280 EBTB patients.10 Recent studies have shown that the most common bronchoscopic finding of EBTB is edematous and hyperemic change of the bronchial mucosa.6,7 We found in the present study that edematous-type EBTB was much more common than actively caseating-type EBTB presenting as RMLS. Since the RML bronchus has a normally narrowed orifice, even a mild edematous change can make it obstruct the bronchial lumen. Due to the anatomical character of the right middle lobe, edematous-type EBTB is the most common type of EBTB presenting as RMLS.
Bronchoscopic evaluation is necessary to ensure proper diagnosis of EBTB. If bronchoscopy shows typical gross finding of EBTB, the condition is relatively easily diagnosed by bronchoscopy alone, especially in the case of actively caseating type. Additionally, actively caseating-type EBTB can easily be diagnosed by microbiologic examination because bronchial washing and/or sputum are usually positive for AFB staining. However, in the case of edematous-type EBTB, it is difficult to differentiate an active lesion from an inactive lesion by gross findings alone, and AFB staining of sputum and even in bronchial washing usually shows a negative response. In the present study, only 1 patient out of 15 total patients with edematous-type EBTB was positive for AFB staining. Because of the low-positive yield for AFB staining, a culture for MTB and histologic examination should be performed to diagnose edematous-type EBTB.
It has been shown that EBTB is usually more commonly observed in women than men, especially young women.10,11 However, a recent report demonstrated that there was a 2-peak incidence of EBTB, and it is also common in elderly patients.7 In our present study, most patients were over the age of 65 years, and the mean age was about 70 years. It is highly likely that the reason for such high occurrence in elderly patients is due to advanced diagnostic procedures such as bronchoscopy, which is usually performed in an out patient setting at a tertiary hospital. Furthermore, involvement of the tracheobronchial tree in EBTB might be different between young and elderly patients.12 EBTB in elderly patients is more frequently involved in the lobar and segmental bronchus than in younger patients. However, EBTB in younger patients is usually prevalent in the trachea or main bronchus. Because of this difference in tracheobronchial involvement characteristic of EBTB between ages, we suggest that EBTB presenting as RMLS is more common in elderly patients.
Although adequate treatment was given, persistent abnormality on chest X-ray was found in more than 50% of patients after complete treatment. Edematous EBTB has a tendency to show a persistent abnormality on chest X-ray after treatment. We suggest that edematous-type EBTB may be changed to fibrotic-type EBTB during the healing process. In contrast, actively caseating-type EBTB can completely be cleared with minimal fibrotic change by treatment if it is not combined with edematous change. If it is combined with edematous change, it might be able to evolute to fibrotic-type EBTB, thus showing a persistent abnormality on chest X-ray. Actively caseating-type EBTB is frequently combined with edematous change of mucosa. The study with serial bronchoscopy showed that more than 60% of actively caseating- and edematous-type EBTB changed to fibrostenotic type.13 We performed follow-up bronchoscopy in 2 patients at 3 months after starting medication, and observed a fibrotic stenosis of the middle lobe bronchus by serial bronchoscopy in 1 patient. Fibrotic scarring during healing of EBTB makes it a permanent obliteration of the bronchial lumen.
Systemic corticosteroid administration with anti-tuberculosis treatment has been shown to more rapidly reduce tuberculosis symptoms, but its effect in preventing bronchial stenosis in EBTB remains doubtful.14,15 A prospective study with 34 EBTB revealed that systemic steroid had no significant effect on preventing bronchial stenosis.16 Therefore, we used oral steroid in only 1 patient in the present study. Since we suspected that she had concomitant bronchial asthma.
In the present study, edematous-type EBTB was the most common type of EBTB presenting as RMLS, and it usually occurred in elderly patients. Culturing for mycobacterium and histologic examination by bronchoscopy are necessary for proper diagnosis of edematous-type EBTB. Persistent abnormality was frequently shown on chest X-ray despite adequate anti-tuberculosis treatment.
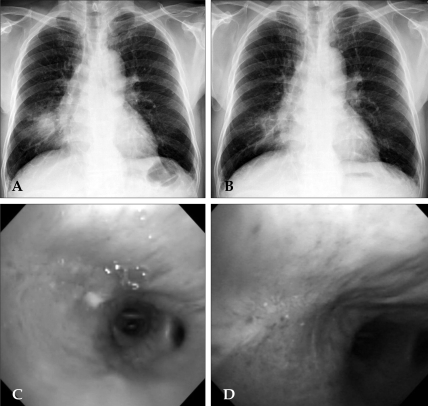
Fig. 1.
Chest X-ray of a 72-year-old man with chronic cough. It shows persistent right middle lobe collapse in serial chest X-ray after 6 months of anti-tuberculous treatment (A) before treatment, (B) after treatment. Bronchoscopic findings showed a mass-like lesion with some necrotic tissue in the middle lobe that completely occluded the bronchial lumen; initial diagnosis (C) and fibrotic scarring in serial bronchoscopy after 3 months of treatment (D).
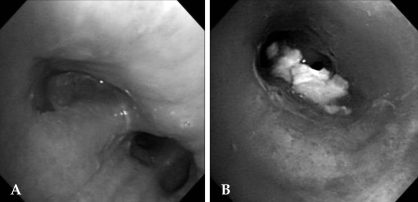
Fig. 2.
(A) Bronchoscopic findings of a 69-year-old woman with chronic cough. Bronchoscopic findings showed an inflammatory change with mucosal edema and some secretion. The middle lobe was narrowed by an edematous change of the mucosa, indicating edematous-type EBTB. (B) Bronchoscopic findings of a 52-year-old woman with chronic cough. Bronchoscopic findings showed whitish necrotic material in the middle lobe, indicating actively caseating-type EBTB. Upon biopsy specimen, numerous bacilli were observed on AFB staining. EBTB, endobronchial tuberculosis.
References
- 1.Chung HS. Endobronchial tuberculosis. J Korean Med Assoc. 2006;49:799–805. [Google Scholar]
- 2.Gupta PP, Gupta KB, Agarwal D. Middle lobe syndrome due to tuberculous etiology: a series of 12 cases. Indian J Tuberc. 2006;53:104–108. [Google Scholar]
- 3.Gudmundsson G, Gross TJ. Middle lobe syndrome. Am Fam Physician. 1996;53:2547–2550. [PubMed] [Google Scholar]
- 4.Kwon KY, Myers JL, Swensen SJ, Colby TV. Middle lobe syndrome: a clinicopathological study of 21 patients. Hum Pathol. 1995;26:302–307. doi: 10.1016/0046-8177(95)90062-4. [DOI] [PubMed] [Google Scholar]
- 5.Kim HO, Ma JE, Lee SJ, Cho YJ, Jeong YY, Jeon KN, et al. Causes of Right Middle Lobe Syndrome: Recent Experience in Local Tertiary Hospital for Several Years. Tuberc Respir Dis. 2007;62:192–196. [Google Scholar]
- 6.Morrone N, Abe NS. Bronchoscopic finding in patients with pulmonary tuberculosis. J Bronchol. 2007;14:15–18. [Google Scholar]
- 7.An JY, Lee JE, Park HW, Lee JH, Yang SA, Jung SS, et al. Clinical and bronchoscopic features in endobronchial tuberculosis. Tuberc Respir Dis. 2006;60:532–539. [Google Scholar]
- 8.Lee JH, Park SS, Lee DH, Shin DH, Yang SC, Yoo BM. Endobronchial tuberculosis: clinical and bronchoscopic features in 121 cases. Chest. 1992;102:990–994. doi: 10.1378/chest.102.4.990. [DOI] [PubMed] [Google Scholar]
- 9.Chung HS, Lee JH, Han SK, Shim YS, Kim KY, Han YC, et al. Classification of endobronchial tuberculosis by the bronchoscopic fratures. Tuberc Respir Dis. 1991;38:108–115. [Google Scholar]
- 10.Park EJ, Kim MO, Yang SC, Sohn JW, Yoon HJ, Shin DH, et al. Clinical and bronchoscopic features of 280 patients with endobronchial tuberculosis (1990-2001) Korean J Med. 2003;64:284–292. [Google Scholar]
- 11.Lee JY, Kim CM, Moon DS, Lee CW, Lee KS, Yang SC, et al. The clinical features of endobronchial tuberculosis - A retrospective study on 201 patients for 6 years. Tuberc Respir Dis. 1996;43:671–682. [Google Scholar]
- 12.Kim HJ, Kim HS, Ma JE, Lee SJ, Ham HS, Cho YJ, et al. Clinical characteristics of endobronchial tuberculosis that develops in patients over 70 years of age. Tuberc Respir Dis. 2007;63:412–416. [Google Scholar]
- 13.Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000;117:385–392. doi: 10.1378/chest.117.2.385. [DOI] [PubMed] [Google Scholar]
- 14.Cisneros JR, Murray KM. Corticosteroids in tuberculosis. Ann Pharmacother. 1996;30:1298–1303. doi: 10.1177/106002809603001115. [DOI] [PubMed] [Google Scholar]
- 15.Rikimaru T. Therapeutic management of endobronchial tuberculosis. Expert Opin Pharmacother. 2004;5:1463–1470. doi: 10.1517/14656566.5.7.1463. [DOI] [PubMed] [Google Scholar]
- 16.Park IW, Choi BW, Hue SH. Prospective study of corticosteroid as an adjunct in the treatment of endobronchial tuberculosis in adults. Respirology. 1997;2:275–281. doi: 10.1111/j.1440-1843.1997.tb00089.x. [DOI] [PubMed] [Google Scholar]