Abstract
Purpose
The surgical robotic system is superior to traditional laparoscopy in regards to 3-dimensional images and better instrumentations. Robotic surgery for hepatic resection has not yet been extensively reported.
Patients and Methods
Between March and May 2007, we performed 3 robot-assisted left lateral sectionectomies of the liver. Case 1 had a hepatocellular carcinoma (HCC), case 2 had colon cancer with liver metastasis, and case 3 had intrahepatic duct stones.
Results
All patients had successful operation and recovered without complications. Shorter length of hospital stays, earlier start of oral feeding and less amount of ascites were found. However, case 1 had recurrent HCC at 3 months after operation.
Conclusion
Robotic-assisted liver surgery is still a new field in its developing stage. In patients with small malignant tumors and benign liver diseases, robotic-assisted laparoscopic resection is feasible and safe. Through experience, the use of robotics is expected to increase in the treatment of benign diseases and malignant neoplsms. However, careful patient selection is important and long-term outcomes need to be evaluated.
Keywords: Hepatocellular carcinoma, robotic liver resection, minimally invasive surgery
INTRODUCTION
The development of minimally invasive surgery has led to an increase in laparoscopic hepatic resection. Particularly for hepatocellular carcinoma (HCC), in which the possibility of repetitive operation for tumor recurrence or liver transplantation is high, laparoscopic approach results in less postoperative adhesion than open abdominal surgery, decreasing the difficulty of dissection in future operation.
However, laparoscopy is limited by 2-dimensional imaging and restricted instrument motion. Advanced computer-enhanced technology has been developed to overcome these limitations. The surgical robotic system provides 3-dimensional images, allowing surgeons to operate with advanced vision. Moreover, the robotic system utilizes EndoWrist, an instrument with a 360-degree range of motion.
The da Vinci Surgical System (Intuitive Surgical, Mountain View, CA, USA) and Zeus system (Computer Motion, Santa Barbara, CA, USA) have been the only 2 commercially available robotic systems. In 2003 Computer Motion was purchased by Intuitive Surgical, thus leaving only the daVinci in production.1
There have been few reports discussing the indications of robotic surgery in hepatobiliary surgery, and robotic surgery for hepatic resection has not been extensively reported. We present herein 3 cases of da Vinci robotic-assisted left lateral sectionectomy of the liver.
PATIENTS AND METHODS
Between March and May 2007, we performed 3 robot-assisted left lateral sectionectomies of the liver at the Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
Case 1
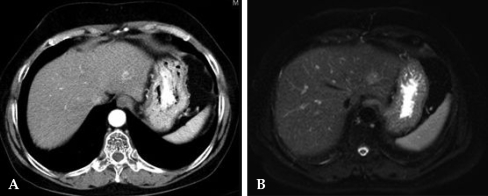
A 63-year-old female with a 20-year history of HBV carrier status was admitted for HCC in liver segment II. Serum alpha-fetoprotein (AFP) level was 559.3 IU/mL. The patient had liver cirrhosis corresponding to Child-Pugh class A, and the Indocyanine Green retention rate at 15 minutes (ICG-R 15) was 1.4%. Imaging included CT and MRI, and hepatic angiography revealed a 2 cm single mass in Segment II consistent with HCC (Fig. 1). We performed left lateral sectionectomy using the da Vinci robotic system.
Fig. 1.
CT (A) and MRI (B) show a 2 cm mass consistent with HCC in segment II. HCC, hepatocellular carcinoma.
Case 2
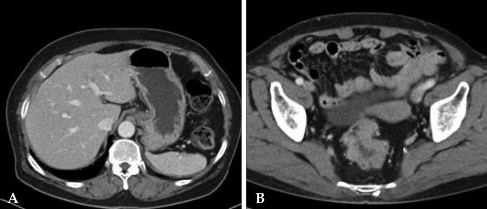
A 70-year-old female presented with a 10-month history of anal bleeding and tenesmus. Colonoscopy revealed an ulcerofungating mass in the rectosigmoid colon, 10 - 15 cm from the anal verge and adenocarcinoma was confirmed from biopsy. CT showed an ulcerofungating mass at the rectosigmoid junction with pericolic fat infiltration and a 1.5 cm hypodense mass on liver segment III, which was compatible with metastasis (Fig. 2). Serum carcinoembryonic antigen (CEA) level was 12.7 ng/mL, and carbohydrate antigen 19 - 9 (CA 19 - 9) level 66.5 U/mL. Simultaneous operation on the colon and metastatic hepatic lesion was planned using the da Vinci robotic system.
Fig. 2.
CT shows a hypodense, 1.5 cm mass (A) in segment III consistent with metastasis and an ulcerofungating mass (B) with minimal pericolic fat infiltration at the rectosigmoid junction.
Case 3
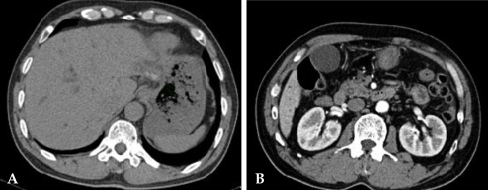
A 59-year-old male with a history of removal of common bile duct (CBD) stone by endoscopic retrograde cholangiopancreatography (ERCP) in 2004 presented acute abdominal pain for 3 days. On admission, total and direct bilirubin was 4.3 and 3.9 mg/dL, respectively, and alkaline phosphatase was 267 IU/L. The other laboratory findings were within the normal limits. Precontrast CT revealed several radiopaque stones noted in liver segment II and a 6 mm calcified stone in the distal CBD. Mild intrahepatic duct dilatation was noted with moderate CBD dilatation (Fig. 3). Robot-assisted left lateral sectionectomy following ERCP removal of CBD stone was planned.
Fig. 3.
Precontrast CT shows IHD and CBD dilatation with several radiopaque stones in liver segment II (A) and a 6 mm calcified stone in the distal CBD (B). IHD, intrahepatic duct; CBD, common bile duct.
Surgical technique
Under general anesthesia, the patient was placed in a supine position, and 5 trocars were used. Pneumoperitoneum to 12 mmHg was established. A 12-mm trocar for the robotic camera was placed above or below the umbilicus by the Hassen method. Three additional 8-mm trocars were placed at the left upper quadrant (LUQ), epigastric, and right upper quadrant (RUQ) areas under the laparoscopic guidance, respectively. A 12-mm trocar for an assistant was also placed at the LUQ area. Insertion sites of trocars were slightly different for each case because of additional procedures. The 4-arm da Vinci surgical robot system was brought into position and docked following port placement. The operator moved to the console to control the robotic arms. The assistant remained at the patient's left side to change robotic instruments and perform clipping, stapling, intraoperative ultrasonography, and choledochoscope through the 12-mm LUQ trocar site.
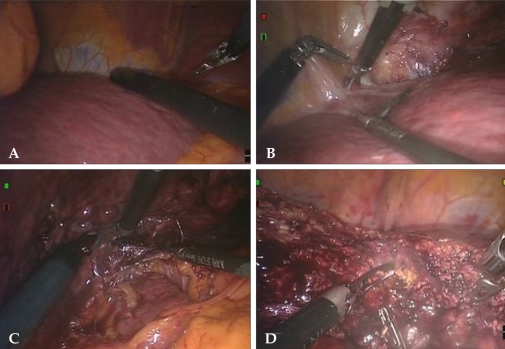
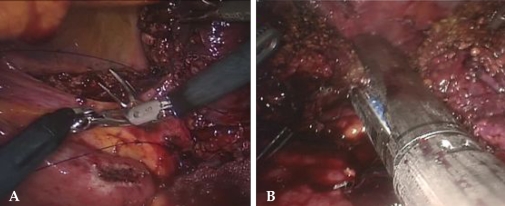
A 30° robotic camera was used. After exploration of the abdominal cavity, intraoperative ultrasonography was used to examine the remaining liver to search for undetectable lesions and obtain adequate surgical resection margins. The undissected round ligament was used as grips to effectively retract the liver. The liver was mobilized by dividing the left triangular ligament and lesser omentum. Parenchymal division proceeded from the anterior edge of the liver by harmonic scalpel and electrocautery (Fig. 4). The small vessels and bile ducts exposed during parenchymal dissection were ligated and divided by clipping. The Glisson's pedicles of segments II and III were clamped and divided by endo-GIA or suture technique (Fig. 5). Dissection proceeded posteriorly to the left hepatic vein trunk, which was also clamped and divided by endo-GIA. Pringle's maneuver was not applied.
Fig. 4.
Operative procedures. Intraoperative ultrasonography for detecting other lesions and determining resection margins (A). Dissection of falciform ligament and ligamentum venosum after detaching the left triangular ligament using a harmonic scalpel (B and C). Parenchymal dissection using a harmonic scalpel and electrocautery (D).
Fig. 5.
Suture for Glissonian pedicle (A) and endo-GIA for division of hepatic vein (B).
A closed suction drain catheter was placed in the subhepatic space. The specimen was placed in an endoscopic retrieval bag and removed through a left subcostal mini-laparotomy incision extending from the port site.
Especially for case 2, we also performed da Vinci-assisted low anterior resection following hepatic resection. However, additional port placement was not required. For case 3, we performed an intraoperative choledochoscopic exam, lithotripsy of the CBD stone, and cholangiography following lateral sectionectomy of the liver and cholecystectomy. The choledochoscopic exam through the left intrahepatic duct showed a 7 mm stone. The stone was removed by Forgathy catheter. We confirmed by cholangiography that there was no stone in the biliary tree. The left intrahepatic duct was closed with several interrupted sutures.
RESULTS
Postoperative course and outcomes
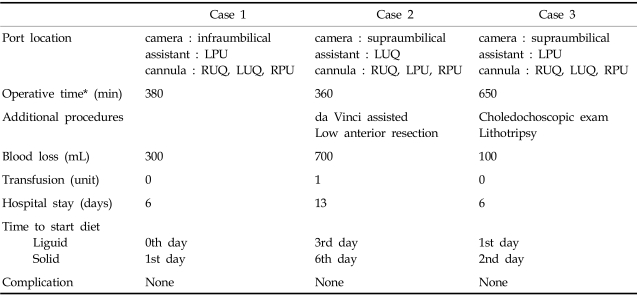
Three consecutive patients successfully underwent laparoscopic robot-assisted left lateral sectionectomy. Short-term outcomes including operative factors are shown in Table 1. After hepatic resection (cases 1 and 3), hospitalization lasted for 6 days although recovery was observed at postoperative day 4. A clear liquid diet was started on postoperative day 1. For case 2, hospital stay was longer (total 13 days), and the diet was started later because of combined colon surgery. During the Postoperative course, all patients recovered without complication.
Table 1.
Operative and Postoperative Outcomes
RUQ, Rt. Upper Quadrant; LUQ, Lt. Upper Quadrant; RPU, Rt. Paraumblical; LPU, Lt. Paraumbilical.
*Operative time for liver surgery.
Pathological examination of case 1 demonstrated a 2.2-cm HCC with capsular invasion and focal microvessel invasion. The resection margin was free of carcinoma and the distance was 0.8 cm. Pathological examination of case 2 showed a metastatic adenocarcinoma of the liver with free resection margins. Pathological examination of case 3 showed intrahepatic duct stones with chronic proliferative cholangitis and ductal dilatation.
Follow-up outcome
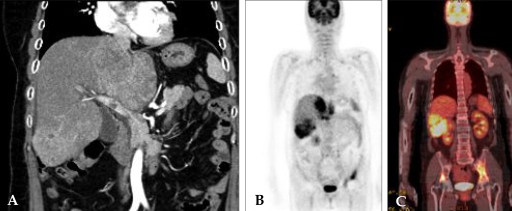
The patient with HCC (case 1) visited the outpatient clinic 3 months postoperatively with left hip pain that had persisted for several days. On evaluation, AFP level was 65151.8 IU/mL, an increase from 132.09 IU/mL measured on postoperative day 7. Follow-up CT showed multiple intrahepatic masses, compatible with recurrent HCC and tumor thrombi, in the main portal trunk. Positron Emission Tomography (PET) showed multiple strong uptake of F-18 FDG in the liver and pelvic bone mainly on the left side. There was no evidence of peritoneal seeding (Fig. 6). The patient was referred to a radiation oncologist.
Fig. 6.
A 3-month follow-up CT showed multiple intrahepatic masses compatible with HCC with tumor thrombi in the main portal trunk (A). PET scan shows multiple strong F-18 FDG uptakes at the liver and pelvic bone (B and C). HCC, hepatocellular carcinoma; PET, positron emission tomography.
DISCUSSION
Robotic surgery enables the operator to control the robotic system alone and to perform more precise and complex operations. The da Vinci Surgical System provides surgeons with 1) intuitive translation of the instrument handle to the tip movement, thus eliminating the mirror-image effect, 2) visualization with high-quality 3-dimensional images and stable camera platform, 3) scaling, 4) tremor filtering, 5) coaxial alignment of eyes, hand, and tooltip images, 6) EndoWrist with a 360-degree range of motion, 7) comfortable, ergonomically ideal operating position, and 8) possibility of remote site surgery.2-4 These benefits are most evident when used for precise surgeries in limited spaces. Robotic liver surgery provides access to fine structures of the liver and allows surgeons to see delicate blood vessels and ducts. Three-dimensional vision offers the advantage of improved depth-perception and accuracy.5 Furthermore, the robotic system involves minimal intraoperative manipulation of the tumor mass, resulting in less trauma.
Robotic surgery has several limitations: 1) high cost, 2) inadequate coverage by medical insurance, 3) lack of tactile sense, that can impair surgeons' capacity to make intuitive decisions, 4) lack of training systems, 5) heavy robotic arms and equipments, 6) time-consuming set up, and 7) difficulty in converting to open surgery.2,3,6 Furthermore, the da Vinci system is not attached to the operating table, requiring undocking to change table position. When perilous circumstances such as massive bleeding occur, the assistant can compress bleeding focus with laparoscopic instruments until conversion to open surgery. Although conversion time can be longer than in laparoscopic surgery, the difference was quite small in our simulations. Problems will most likely be resolved as computer-enhanced technology continues to develop and surgeons accumulate experience.
Currently, the da Vinci robotic system is applied to almost every surgical procedure. Evaluation of robotic-assisted surgery in other fields such as prostate cancer or colorectal disease was proven to be safe and feasible. Oncological and functional outcomes are promising.4,7-10 In the laparoscopic era, no randomized clinical trials have been performed comparing laparoscopy to open hepatic resection in terms of safety, feasibility and efficacy. Simillis et al. investigated laparoscopic versus open hepatic resection for hepatic neoplasms through a meta-analysis and concluded that operative blood loss and duration of hospital stay were significantly reduced after laparoscopic surgery and that there was no difference in postoperative adverse events or the extent of oncological clearance.11 Vibert et al. concluded after 10 years of experience in performing laparoscopic liver surgery that the results of laparoscopy are similar to those of laparotomy, suggesting that laparoscopy approach could be used for most hepatic surgeries, including major hepatectomy, for malignancy.12 Moreover, Chang et al. advocate that laparoscopic left lateral sectionectomy for benign or malignant neoplasm is safe and feasible and can be considered as a routine approach in selected patients.13 However, there have been few reports about robotic-assisted hepatic resection.
In our experience, operative time was longer due to unfamiliarity with robotic instruments and set-up time. However, the length of time required will continue to decrease as surgeons become more familiar with the procedure. In patients with small malignant tumors and benign diseases, robotic-assisted laparoscopic resection is feasible. Furthermore, we expect that accumulating experience will make it possible to safely perform other major hepatectomies. We found shorter length of hospital stays, earlier start of oral feeding and less amount of ascites after robotic surgery compared to open surgery for liver resection.
From the oncologic point of view, the potential benefits of a minimally invasive approach in terms of curability, recurrence, and long-term survival are inconclusive. Nevertheless to perform anatomical resection with safe resection margins, intraoperative laparoscopic ultrasonography is indispensable and guarantees precise segmental tumor location and adjacent vascular or biliary involvement excluding adjunctive lesions.14 Therefore, we performed laparoscopic ultrasonography on all patients.
In spite of this effort, case 1 had fulminant intrahepatic recurrent tumors and bone metastasis. Preoperative CT, MRI, and angiography did not show any signs for early recurrence. The possibility that robotic surgery contributed to early recurrence cannot be excluded. However, the tumor mass was less manipulated compared to conventional open surgery.
Another concern is that carbon dioxide insufflation might promote cancer dissemination, port site metastases, and peritoneal seeding.15,16 However, there is no definite evidence in the literature to show that the spread of cancer is increased.15,17 In spite of the massive intrahepatic disseminated masses and bony metastasis in case 1, there was no evidence of peritoneal seeding. Therefore, we believe that the route of recurrence was hematogenous with portal vein tumor thrombi. Intrahepatic metastasis by the portal venous system is probably an important mechanism for intrahepatic recurrence either from micrometastasis or dissemination with manipulation of tumor during hepatectomy.18,19 For patients with poor prognostic factors after resection for HCC, a number of adjuvant therapies, such as systemic chemotherapy and radiation therapy, are available.
In conclusion, da Vinci robotic-assisted hepatic resection can open a new horizon of treatment strategies and overcome the limitations of laparoscopic surgery. In the near future, the use of robotics is expected to increase in the treatment of benign disease and malignant neoplasm of the liver as a minimally invasive surgery. Experience and judicious application of this new technology are important.
References
- 1.Hanly EJ, Talamini MA. Robotic abdominal surgery. Am J Surg. 2004;188(4A Suppl):19S–26S. doi: 10.1016/j.amjsurg.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 2.Vidovszky TJ, Smith W, Ghosh J, Ali MR. Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res. 2006;136:172–178. doi: 10.1016/j.jss.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Hashizume M, Tsugawa K. Robotic surgery and cancer: the present state, problems and future vision. Jpn J Clin Oncol. 2004;34:227–237. doi: 10.1093/jjco/hyh053. [DOI] [PubMed] [Google Scholar]
- 4.D'Annibale A, Morpurgo E, Fiscon V, Trevisan P, Sovernigo G, Orsini C, et al. Robotic and laparoscopic surgery for treatment of colorectal disease. Dis Colon Rectum. 2004;47:2162–2168. doi: 10.1007/s10350-004-0711-z. [DOI] [PubMed] [Google Scholar]
- 5.Camarillo DB, Krummel TM, Salisbury JK., Jr Robotic technology in surgery: past, present, and future. Am J Surg. 2004;188(4A Suppl):2S–15S. doi: 10.1016/j.amjsurg.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen MM, Das S. The evolution of robotic urologic surgery. Urol Clin North Am. 2004;31:653–658. doi: 10.1016/j.ucl.2004.06.002. vii. [DOI] [PubMed] [Google Scholar]
- 7.Lee YS, Han WK, Oh YT, Choi YD, Yang SC, Rha KH. Robot-assisted laparoscopic radical prostatectomy: four cases. Yonsei Med J. 2007;48:341–346. doi: 10.3349/ymj.2007.48.2.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anvari M, Birch DW, Bamehriz F, Gryfe R, Chapman T. Robotic-assisted laparoscopic colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2004;14:311–315. doi: 10.1097/01.sle.0000148473.05042.8f. [DOI] [PubMed] [Google Scholar]
- 9.Talamini MA, Chapman S, Horgan S, Melvin WS. The Academic Robotics Group. A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc. 2003;17:1521–1524. doi: 10.1007/s00464-002-8853-3. [DOI] [PubMed] [Google Scholar]
- 10.Patel VR, Chammas MF, Jr, Shah S. Robotic assisted laparoscopic radical prostatectomy: a review of the current state of affairs. Int J Clin Pract. 2007;61:309–314. doi: 10.1111/j.1742-1241.2006.01235.x. [DOI] [PubMed] [Google Scholar]
- 11.Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms-a meta-analysis. Surgery. 2007;141:203–211. doi: 10.1016/j.surg.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 12.Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B. Laparoscopic liver resection. Br J Surg. 2006;93:67–72. doi: 10.1002/bjs.5150. [DOI] [PubMed] [Google Scholar]
- 13.Chang S, Laurent A, Tayar C, Karoui M, Cherqui D. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg. 2007;94:58–63. doi: 10.1002/bjs.5562. [DOI] [PubMed] [Google Scholar]
- 14.Santambrogio R, Opocher E, Ceretti AP, Barabino M, Costa M, Leone S, et al. Impact of intraoperative ultrasonography in laparoscopic liver surgery. Surg Endosc. 2007;21:181–188. doi: 10.1007/s00464-005-0738-9. [DOI] [PubMed] [Google Scholar]
- 15.Allardyce RA. Is the port site really at risk? Biology, mechanisms and prevention: a critical view. Aust N Z J Surg. 1999;69:479–485. doi: 10.1046/j.1440-1622.1999.01606.x. [DOI] [PubMed] [Google Scholar]
- 16.Gutt CN, Kim ZG, Hollander D, Bruttel T, Lorenz M. CO2 environment influences the growth of cultured human cancer cells dependent on insufflation pressure. Surg Endosc. 2001;15:314–318. doi: 10.1007/s004640000321. [DOI] [PubMed] [Google Scholar]
- 17.Takiguchi S, Matsuura N, Hamada Y, Taniguchi E, Sekimoto M, Tsujinaka M, et al. Influence of CO2 pneumoperitoneum during laparoscopic surgery on cancer cell growth. Surg Endosc. 2000;14:41–44. doi: 10.1007/s004649900008. [DOI] [PubMed] [Google Scholar]
- 18.Nagasue N, Uchida M, Makino Y, Takemoto Y, Yamanoi A, Hayashi T, et al. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology. 1993;105:488–494. doi: 10.1016/0016-5085(93)90724-q. [DOI] [PubMed] [Google Scholar]
- 19.Poon RT, Fan ST, Ng IO, Lo CM, Liu CL, Wong J. Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma. Cancer. 2000;89:500–507. [PubMed] [Google Scholar]