Abstract
Purpose
Numerous methods have been utilized to repair nasal septal perforation with varying degrees of success; however, no consensus has been reached on nasoseptal perforation repair. Here, the authors describe a surgical method based on human dermal allograft (Surederm™, Hans Biomed Corp. Korea) for the repair of nasal septal perforations.
Materials and Methods
Eleven patients with a nasal septal perforation were included in this study. The causes of these septal perforations included previous nasal surgery, trauma, foreign body (button battery), and idiopathy. There were several sites of perforation: 9 in the central area, 1 in the posterior-central area, and 1 in the anterior area. An interpositional graft incorporating Surederm™ was positioned between bilateral mucoperichondrial flaps using an intranasal approach. A silastic sheet was then left in the nasal septum bilaterally until complete healing had occurred through new nasal mucosa, which took a mean duration of 6 weeks.
Results
Outcomes in ten of the eleven patients were successful, with complete septal perforation closure. The remaining perforation, which was caused by a button battery, closed incompletely; however, its initial size of 2 cm was reduced to 5 mm.
Conclusion
The described technique has a high success rate and can be performed under local anesthesia without external scarring. In the absence of donor site morbidity, this technique can also be utilized to repair posterior or multiple septal perforations without difficulty.
Keywords: Allograft, nasal septum
INTRODUCTION
The majority of nasal septal perforations are asymptomatic, but some patients seek treatment for a variety of symptoms, e.g., nasal obstruction, nasal crust, or epistaxis, that turn out to be nasal septal perforations. Asymptomatic perforations rarely require any treatment, and some symptomatic patients can be managed conservatively. However, surgery is an option when medical treatment fails to alleviate symptoms.
Currently available surgical procedures for nasal septal perforations include advancement mucosal flaps,1 lateral nasal wall flaps,2 and autografts using temporal fascia3 or allograft dermal matrix.4 Surgical approaches include the endonasal approach and the open external approach.5 However, nasal septal perforation closure remains a surgical challenge and is frequently unsuccessful.
Surederm™ is an allograft dermal matrix composed of collagen, elastin, and proteoglycan and does not elicit an immune response. Moreover, surgery can be performed in the absence of donor site morbidity. We describe an endonasal surgical repair technique using an allograft dermal matrix to close septal perforations.
MATERIALS AND METHODS
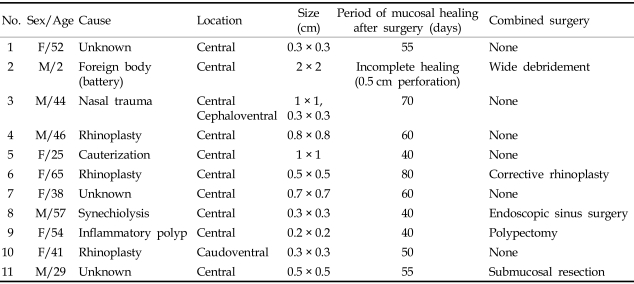
Eleven symptomatic patients with septal perforations were treated surgically using an allograft dermal matrix at our ENT department from April 2004 and May 2006. Five patients were male and six were female, and they had a mean age of 41 (age range 2 - 65). Perforations were surgically induced in 5, iatrogenic in 3, post-traumatic in 2, and caused by a foreign body (button battery) in 1. Preoperative symptoms and perforation sizes and locations were evaluated, with a mean perforation diameter of approximately 5 mm. Perforation locations were defined about imaginary lines that divided the septum into halves, i.e., ventral/dorsal and caudal/cephalic, respectively. Perforation sites were located as follows; 9 centrally, 1 caudoventrally, and two perforations in one septum (1 centrally and 1 centroventrally). Symptoms, improvement in perforation size, duration of treatment, and complications were evaluated postoperatively (Table 1).
Table 1.
Clinical Data of Patients with Septal Perforation
F, female; M, male.
Surgical technique
Septal repair using an endonasal approach with an allograft dermal matrix was performed under local anesthesia with the exception of one case, with a 2-year-old male, which was performed under general anesthesia. Preoperative nasal packing was performed for 15 minutes with a cotton pledget soaked in 1:100,000 epinephrine and 2% lidocaine to achieve nasal decongestion and local anesthesia. A Killian incision (mainly left) was then made 1 - 2 mm posterior to the caudal septum, and both sides of the mucoperichondrial flaps were then raised around the perforation. Sufficient dissection of the mucoperichondrial flaps from the septal cartilage, perpendicular plate, and vomer was performed to create a space for an allograft dermal matrix insertion. Septoplasty was performed with septal repair simultaneously in cases with a deviated septum, and debridement around the perforation site was performed when scar or granulation tissue was present at the perforation site. The allograft dermal matrix was soaked in normal saline for over 10 minutes and cut 1 cm wider than the perforation. It was then interposed between both mucoperichondrial flaps to overlap the perforation site (there is no need to differentiate between dermal and epidermal sides of Surederm). The allograft dermal matrix was then placed on one side between the remaining cartilage and the mucoperichondrial flap, and the septal flaps were sutured with 5 - 0 nylon to the allograft dermal matrix at the anterior margin to fix the interpositional graft. This step provides a template for perforation healing. The Killian incision site was then closed with 4 - 0 vicryl. The repaired septal flaps were protected from drying during the healing phase by placing a silastic sheet on both sides of the septal flap and securing these with nonabsorbable 5 - 0 sutures transseptally (Fig 1). Repair sites can be visualized to ensure that the mucosa has healed before silastic sheets are removed, and they are commonly left in place 4 - 10 weeks. Both nasal cavities were lightly packed with Merocel® and vaseline gauze; this packing is usually removed after postoperative day two.
Fig. 1.
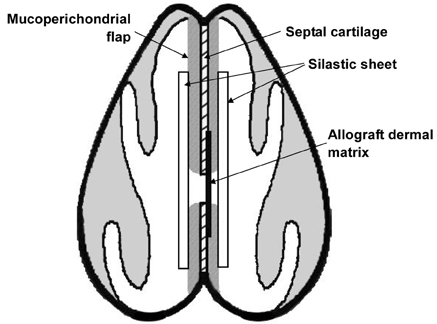
Schematic figure of the surgical technique.
RESULTS
The most common symptoms encountered preoperatively were nasal obstruction in 50% of cases and nasal discharge in 33%; followed by epistaxis, nasal dryness, whistling, and pain. Preoperative symptoms all improved significantly after surgery. Total perforation closure with the allograft dermal matrix was accomplished in 10 of the 11 cases (Fig. 2). The septal cartilage became necrotic due to the button battery in one case, and thus wide debridement of the septal mucosa was accomplished with septal repair. Ten of the 11 patients achieved complete closure with a mean healing period of 50 days. The patient with septal perforation caused by a button battery achieved a reduction in diameter from 2 cm to only 0.5 cm. Complications such as saddle nose, reperforation, or infection were not reported in any of the 10 patients during a mean postoperative follow up of 15 months.
Fig. 2.
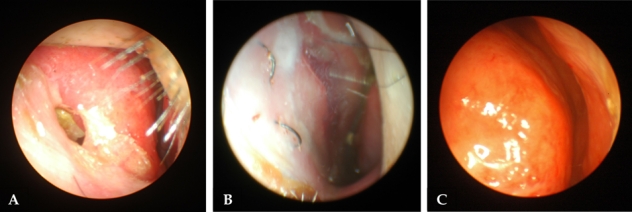
Preoperative view of septal perforation (A). A silastic sheet was inserted into both nasal cavities to protect Surederm (B). Postoperative view showing good healing of the perforated septum (C).
DISCUSSION
The most common cause of septal perforation is trauma.6 Other etiologies such as inflammation, neoplasm, and chemical irritants can also cause septal perforation. Mucociliary action is more active in the anterior septum; therefore the more anterior a perforation, the more likely the patient will present with nasal crusting or nasal obstruction. When a crust is present around a perforation, lamellar airflow is disturbed and turbulence occurs, and, if protracted, this may result in further destruction of nasal mucosa, which will become dry.7
Thus, surgery should include not only perforation repair but also the restoration of normal nasal physiology. In particular, repair using a skin or buccal mucosal graft may leave a patient with a dry nose because normal respiratory epithelium is absent.8,9 Furthermore, locally advanced flaps have the disadvantage that they are hard to use in cases with a large perforation, a posterior perforation, or in patients with extrusion of the maxillary crest.10 The advantages of an inferior turbinate flap are abundant vascularity, a wide arc of rotation, and combined skeletal and epithelial support; but this modality requires a second stage procedure to release the pedicle and airway obstruction caused by the turbinate flaps themselves.2 Temporalis muscle fascia or auricular conchal cartilage also require a second-stage procedure. Conversely, an allograft dermal matrix as described requires only a single procedure and is an acellular dermal graft used to treat acute burns.9 Dermis appears to be a better choice for grafting material because it vascularized and mucosalized, while temporalis fascia is not.11
We were able to choose a dermal graft with a size and thickness tailored for perforation sites. In the described patients a 1-mm-thick allograft dermal matrix was used, which we found was enough to act as a template for nasal mucosal healing. An allograft dermal matrix is composed of collagen, elastic tissue, and proteoglycan. It does not elicit an immune response due to its acellular nature therefore avoiding comorbidities associated with donor sites. Moreover, the collagen and elastic fibers in an allograft dermal matrix provide a supporting structure for regenerating mucoepithelium and vessels. Proteoglycan also provides a reservoir for growth factors, which guide collagen assembly and promote angiogenesis.12
Successful operative outcome depends on numerous factors, e.g., the surgical method, the cause of the perforation, its size, and postoperative care.13 Adolfo14 reported a 92% closure rate for small perforations (< 1 cm), but in patients with a large perforation (> 2 cm) complete closure was accomplished in only 25%. In the present study, one case (No. 2) caused by a button battery experienced incomplete closure. However the perforation was greatly reduced in size, which leaves open the possibility of reoperation. The remaining 10 cases with perforations of less than 2 cm all achieved complete healing, with healing times ranging from 4 to 8 weeks. Importantly, the silastic sheet should be left in position until complete healing has occurred, which protects the graft from air flow drying and allows safe postoperative care. When a perforation was caused by a button battery, reperforation seemed to be attributable to the large size of the perforation.
Generally, an open external approach is adequate for a superior perforation or a posterior perforation with restricted surgical visualization.5 An endonasal approach can minimize cosmetic deformities, but usually does not achieve adequate surgical visualization during operation. However, it is not difficult using our technique to repair a perforation even if the endonasal approach provides restricted surgical visualization. This is because there are no complicated procedures during the operation, only a transseptal suture with silastic sheet is required to prevent displacement allograft. In addition, other procedures like endoscopic sinus surgery (ESS), rhinoplasty, septoplasty, can be performed simultaneously to augment treatment if necessary. Although the efficacy of septal repair in a superior or large perforation remains to be proven in future investigations, our technique using an allograft dermal matrix as compared with other septal repair methods has a high success rate without cosmetic deformity, and can be performed easily through an endonasal approach without sacrificing a donor site. Moreover, it provided good cosmetic and functional outcomes, and we advocate its use as an effective tool for the treatment of nasal septal perforation.
ACKNOWLEDGEMENTS
We thanks to the Alumni Association of Department of Otorhinolaryngology, Kangbuk Samsung Hospital.
References
- 1.Gollom J. Perforation of the nasal septum. The reverse flap technique. Arch Otolaryngol. 1968;88:518–522. doi: 10.1001/archotol.1968.00770010520012. [DOI] [PubMed] [Google Scholar]
- 2.Friedman M, Ibrahim H, Ramakrishnan V. Inferior turbinate flap for repair of nasal septal perforation. Laryngoscope. 2003;113:1425–1428. doi: 10.1097/00005537-200308000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Nuñez-Fernández D, Vokurka J, Chrobok V. Bone and temporal fascia graft for the closure of septal perforation. J Laryngol Otol. 1998;112:1167–1171. doi: 10.1017/s0022215100142744. [DOI] [PubMed] [Google Scholar]
- 4.Lee HM, Kim ST, Cho JH, Lee JH, Choi CS, Hwang SJ, et al. Reconstruction of septal perforation with alloderm. Korean J Otolaryngol. 2000;43:1323–1327. [Google Scholar]
- 5.Kuriloff DB. Nasal septal perforations and nasal obstruction. Otolaryngol Clin North Am. 1989;22:333–350. [PubMed] [Google Scholar]
- 6.Brain D. The nasal septum. In: Kerr AG, editor. Scott-Brown's Otolaryngology. 6th ed. Oxford: Butterworth-Heinemann; 1997. p. 27. [Google Scholar]
- 7.Kridel RWH. Considerations in the etiology, treatment, and repair of septal perforations. Facial Plast Surg Clin North Am. 2004;12:435–450. doi: 10.1016/j.fsc.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Gillies H, Millard DR., Jr . Principles and art of plastic surgery. Boston: Little, Brown and Company; 1957. p. 555. [Google Scholar]
- 9.Fairbanks DN, Fairbanks GR. Nasal septal perforation: prevention and management. Ann Plast Surg. 1980;5:452–459. doi: 10.1097/00000637-198012000-00007. [DOI] [PubMed] [Google Scholar]
- 10.André RF, Lohuis PJ, Vuyk HD. Nasal septum perforation repair using differently designed, bilateral intranasal flaps, with nonopposing suture lines. J Plast Reconstr Aesthet Surg. 2006;59:829–834. doi: 10.1016/j.bjps.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Lee D, Joseph EM, Pontell J, Turk JB. Long-term results of dermal grafting for the repair of nasal septal perforations. Otolaryngol Head Neck Surg. 1999;120:483–486. doi: 10.1053/hn.1999.v120.a92930. [DOI] [PubMed] [Google Scholar]
- 12.Livesey SA, Herndon DN, Hollyoak MA, Atkinson YH, Nag A. Transplanted acellular allograft dermal matrix. Potential as a template for the reconstruction of viable dermis. Transplantation. 1995;60:1–9. [PubMed] [Google Scholar]
- 13.Goh AY, Hussain SS. Different surgical treatments for nasal septal perforation and their outcomes. J Laryngol Otol. 2007;121:419–426. doi: 10.1017/S002221510700566X. [DOI] [PubMed] [Google Scholar]
- 14.Sarandeses-García A, Sulsenti G, López-Amado M, Martínez-Vidal J. Septal perforations closure utilizing the backwards extraction-reposition technique of the quadrangular cartilage. J Laryngol Otol. 1999;113:721–724. doi: 10.1017/s0022215100145025. [DOI] [PubMed] [Google Scholar]