Abstract
Necrotizing aortitis is a rare and life-threatening complication of local or generalized bacterial infections and most commonly affects the abdominal aorta. We described a case of a 79-year-old man with an acupuncture-induced bacterial aortitis associated with pseudoaneurysm formation causing near rupture. The patient underwent emergent explolapartomy, resection of the infected aorta, wide debridement of surrounding infected tissues, and extra-anatomic axillary to bifemoral graft bypass. The microbiologic examination revealed Escherichia coli and methicillin resistant Staphylococcus aureus (MRSA). Necrotizing aortitis is very serious and fatal disease, careful history taking as well as rapid diagnosis and urgent treatment are of critical importance.
Keywords: Acupuncture, necrotiwing aortitis, pseudoaneurysm
INTRODUCTION
Acupuncture is an important alternative medical treatment that has been used in China and other Asian countries for thousands of years to treat a variety of diseases and symptoms, most commonly for chronic pain, Although most acupuncturists consider the procedure to be noninvasive, many complications, including physical injuries due to acupuncture needles, and problems related to wounds or systemic infections have been reported.1 Necrotizing bacterial aortitis is a rare and fatal entity that may result in vessel rupture or pseudoaneurysm formation. In this report, we describe a rare case of bacterial aortitis that resulted from a long acupuncture needle.
CASE REPORT
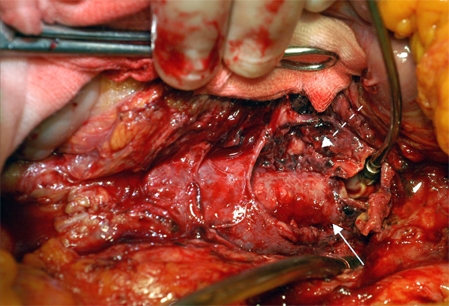
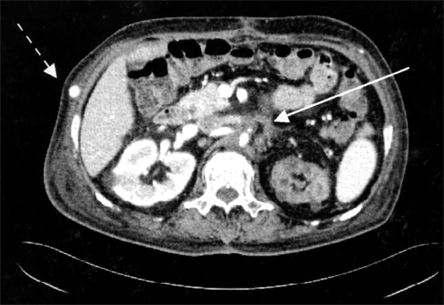
A 79-year-old man was admitted emergently with a 3-week history of fever, chill, and abdominal pain. His past history was remarkable for hypertension and diabetes. He also had a history of receiving acupuncture on his back about a month before the onset of symptoms. Clinical examination revealed tender abdomen, tachycardia of 98 beats per min, and temperature of 38℃. Laboratory evaluation revealed a white blood cell count of 28,580/mm3 with 95.6% neutrophils. Abdominal computed tomogram performed at local clinic confirmed the presence of an abdominal aortic pseudoaneurysm from infrarenal to the level of both common iliac arteries with periaortic gangrenous gas formation (Fig. 1). Because of the presence of retroperitoneal pseudoaneurysm and probable rupture, an emergent explo-laparotomy was performed. At emergency laparotomy, a pseudoaneurysm containing gas-forming inflamed friable tissue with hematoma was observed, and the adventitia of the aorta was almost completely destroyed (Fig. 2). The hematoma was partly evacuated and the cavity was debrided. During removal of the infected adventitial tissue, a part of the abdominal aorta suddenly ruptured. By careful management of the patient's vital signs, the ruptured aorta was firmly compressed and the uncontaminated portion of infrarenal abdominal aorta and both common iliac arteries were secured for cross clamping. After the proximal and distal parts were cross clamped, the infected friable aortic walls and pseudoaneurysm were completely removed. Since there was on going inflammation and bacterial infection was highly suspected, we decided to resect the entire infected abdominal aorta and perform an extra-anatomical correction. The aorta was resected obliquely abovel the pseudoaneurysm, preserving the right renal artery. The left renal artery had to be ligated, and both common iliac arteries were also obliterated by applying continuous sutures of prolene 4/0. In addition, right axillary artery to right femoral artery bypass grafting and right femoral to left femoral artery bypass grafting were performed using 8 mm ringed Goretex grafts.
Fig. 1.

Preoperative abdominal CT showed infected aortic pseudoaneurysmm of 5 cm in diameter with periaortic gangrenous gas formation (white arrow).
Fig. 2.
Intraoperative finding revealed a pseudoaneurysm, containing gas-forming inflamed friable tissue with hematoma (dotted arrow), and the adventitia of the aorta wsa almost completely destroyed (solid arrow).
Histological examination of the resected abdominal aorta showed far advanced atherosclerosis, which was complicated with ulceration, severe aneurysm, and superimposed necrotizing inflammatory infiltrates involving mural and adventitial soft tissue, consistent with necrotizing aortitis. The cultures of the aortic wall and atheroma revealed many Escherichia coli and methicillin-resistant Staphylococcus aureus (MRSA).
Postoperatively, the recommended antimicrobial therapy with vancomycin, meropen, and metronidazole was continued during hospitalization. Postoperative follow-up abdominal CT performed after one month revealed organized fibrotic tissue at the aortic resection area and the patent bypass grafts (Fig. 3). After 30 days of ICU treatment because of acute renal failure, pneumonia, and 46 days of hospitalization, the patient was discharged.
Fig. 3.
Postoperative abdominal CT showed a 3 cm sized organizing fibrotic tissue around the area where the aorta was resected (solid arrow), and patent axillo-femoral prosthetic bypass graft (dotted arrow).
DISCUSSION
Necrotizing aortitis is a rare and life-threatening complication of local or generalized bacterial infections, and most commonly affects the abdominal aorta. It involves the infection of normal or atherosclerotic vessels, resulting from septic embolization to the vasa vasorum, hematogenous seeding of an existing aneurysm, extension from a contiguous site of infection, direct invasion from an extra-vascular source, and traumatic inoculation.2-4 In contrast to infective endocarditis, aortitis is associated with a broader array of microorganisms. Staphylococcus aureus accounts for the majority of Gram-positive infections, however, Gram-negative bacilli, such as Salmonella and proteus species and Escherichia coli, have been described.5
Patients often include men over 50 years of age with atherosclerosis with fever, abdominal or back pain, palpable abdominal mass, and leukocytosis with or without positive blood cultures.2 Computed tomography (CT) is the most useful imaging modality. When the CT scan shows a leak of contrast material from the aorta, prompt management is mandatory to avoid fatal complications since the mortality of ruptured necrotizing aortitis has been reported to be as high as 90%.5 A CT scan can also accurately visualize the aortic wall and differentiates a primary pseudoaneurysm from a true aneurysm.6 Optimal management of aortic infections requires surgical debridement and revascularization followed by prolonged antibiotic administration. Without a surgical approach, the infected aorta may continue to enlarge and rupture despite aggressive antimicrobial therapy, and the mortality associated with nonsurgical management may approach 90%.5 The intent of surgery is to control hemorrhage if the aneurysm has ruptured, confirm the diagnosis, control sepsis, and reconstruct the arterial vasculature.2 For revascularization, prosthetic grafts may be placed in situ or in an extra- anatomic fashion. The most significant concern for revascularization is graft infection since pus contaminates the reconstructed aorta.7
In the present case, a long acupuncture needle penetrated from the patient's back is the most suspicious cause for the aortic infection. Since the aorta was ruptured during manipulation, surgical treatment involved resection of the infected aorta, wide debridement of surrounding infected tissues, and extra-anatomic axillary to bifemoral graft bypass through clean tissue planes. Because it is a very serious and fatal disease, careful history taking as well as rapid diagnosis and urgent surgical treatment are of critical importance.
References
- 1.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72–83. [PubMed] [Google Scholar]
- 2.Foote EA, Postier RG, Greenfield RA, Bronze MS. Infectious Aortitis. Curr Treat Options Cardiovasc Med. 2005;7:89–97. doi: 10.1007/s11936-005-0010-6. [DOI] [PubMed] [Google Scholar]
- 3.Dawas K, Hicks RCJ. Pneumococcal aortitis causing aortic rupture. EJVES Extra. 2003;6:70–72. [Google Scholar]
- 4.Luo CY, Ko WC, Kan CD, Lin PY, Yang YJ. In situ reconstruction of septic aortic pseudoaneurysm due to Salmonella or Streptococcus microbial aortitis: long-term follow-up. J Vasc Surg. 2003;38:975–982. doi: 10.1016/s0741-5214(03)00549-4. [DOI] [PubMed] [Google Scholar]
- 5.Bronze MS, Shirwany A, Corbett C, Schaberg DR. Infectious aortitis: an uncommon manifestation of infection with Streptocuccus pneumoniae. Am J Med. 1999;107:627–630. doi: 10.1016/s0002-9343(99)00306-x. [DOI] [PubMed] [Google Scholar]
- 6.Coppin T, Kassabian E, Costanzo A, Fabiani JN, Chemla E. Primary supraceliac aortic pseudoaneurysm due to a septic aortic rupture. J Cardiovasc Surg (Torino) 2005;46:88–89. [PubMed] [Google Scholar]
- 7.Kitamura T, Morota T, Motomura N, Ono M, Shibata K, Ueno K, et al. Management of infected grafts and aneurysms of the aorta. Ann Vasc Surg. 2005;19:335–342. doi: 10.1007/s10016-005-0006-4. [DOI] [PubMed] [Google Scholar]


