Abstract
Rapid arterial rethrombosis is associated with high-grade residual stenosis and usually occurs at the site of the initial occlusion, resulting in reocclusion of the recanalized artery. Platelets may play an active role in such rethrombosis after thrombolytic-induced clot lysis. Given that glycoprotein IIb/IIIa receptor blockers, like tirofiban, prevent thrombus formation by inhibiting the final common pathway of platelet aggregation, they may be helpful for treating rethrombosis after thrombolysis. A 64-year-old man presented with an acute ischemic stroke due to internal carotid artery (ICA) occlusion. The ICA was recanalized by intravenous thrombolysis but reoccluded shortly after recanalization. The reoccluded ICA was successfully recanalized using intra-arterial tirofiban. A carotid stent was subsequently inserted to relieve severe stenosis and to prevent recurrent stroke. Here, we report a case of rescue treatment of a successfully recanalized ICA by intra-arterial tirofiban. We suggest that rescue use of intra-arterial tirofiban may be effective and safe, especially in hemorrhage prone situations, due to the relatively lower dose of tirofiban compared with intravenous doses.
Keywords: Carotid stent, glycoprotein IIb/IIIa receptor blocker, tissue plasminogen activator
INTRODUCTION
Reocclusion after successful arterial recanalization occurs commonly in acute ischemic stroke.1,2 Rapid rethrombosis is associated with high-grade residual stenosis and usually occurs at the site of the initial occlusion, resulting in reocclusion of the recanalized artery.3 Platelets may play an active role in such rethrombosis following thrombolytic-induced clot lysis.
Glycoprotein (GP) IIb/IIIa receptor blockers prevent thrombus formation by inhibiting the final common pathway of platelet aggregation. There are three GP IIb/IIIa receptor blockers (abciximab, tirofiban, eptifibatide) available for clinical use. There are significant differences in the biological and plasma half-lives of abciximab and the small molecule agents (tirofiban and eptifibatide). Tirofiban is a small, non-peptide molecule that has been used intravenously, in combination with recombinant tissue plasminogen activator (rt-PA), to treat patients with acute coronary artery disease. Some promising pilot results using intravenous tirofiban combined with thrombolytics for acute ischemic stroke have been demonstrated.4,5
CASE REPORT
A 64-year-old man was admitted to the hospital due to left-sided weakness and drowsiness. His initial National Institutes of Health Stroke Scale (NIHSS) score was 16. Brain CT showed no low-density lesions, but bilateral cervical internal carotid artery (ICA) occlusions were observed on CT angiography (Fig. 1). Intravenous rt-PA was administered 160 minutes after the initial onset of symptoms. Because there was no improvement at the end of the intravenous rt-PA infusion, we proceeded to cerebral angiography to perform intra-arterial thrombolysis. Cerebral angiography showed complete occlusion of the left cervical ICA and severe stenosis of the right cervical ICA (Fig. 2A) with delayed filling of the right middle cerebral artery and both anterior cerebral arteries. The left ICA territory was supplied by an ophthalmic collateral from the left external carotid artery and pial collateral flow from the left posterior cerebral artery. Due to the severe stenosis of the right ICA and delayed intracranial perfusion, plans were made to insert a carotid stent to prevent recurrent ischemic stroke. However, the right ICA was reoccluded approximately 20 minutes after the initial angiography (Fig. 2B). Tirofiban was administered through the microcatheter by hand injection. After injection of 200 µg of tirofiban over five minutes, the occluded ICA was recanalized with the remaining stenosis as severe as that seen on initial angiography (Fig. 2C). We inserted a self-expandable carotid stent (SMART, 7 × 80 mm Cordis, Warren, NJ, USA), and subsequent angiography showed no remaining stenosis (Fig. 2D). A brain MRI performed 10 days after thrombolysis showed acute cerebral infarctions involving the right fronto-parietal and medial frontal cortex. Four weeks following thrombolysis, the patient's NIHSS score had improved to six.
Fig. 1.
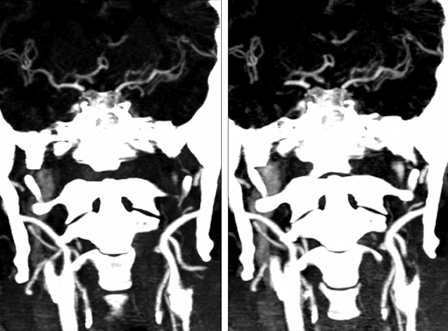
Initial brain CT angiography shows bilateral internal carotid artery occlusions.
Fig. 2.
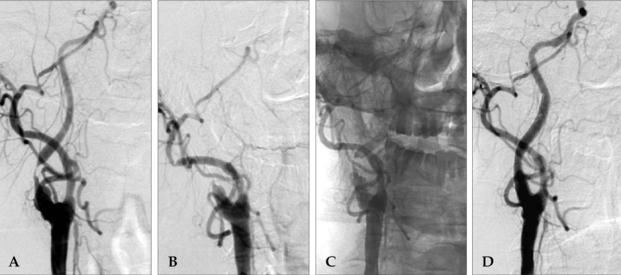
Serial cerebral angiography. (A) The initial angiography reveals severe stenosis of the right cervical ICA. (B) Reocclusion of the right ICA 20 minutes after initial angiography. (C) After intra-arterial tirofiban infusion, the occluded right ICA is recanalized and severe stenosis remains. (D) Final angiography after carotid stent insertion shows no stenosis of the right ICA. ICA, internal carotid artery.
DISCUSSION
Fibrinolysis by rt-PA heightens platelet activity and exposes clot-bound thrombin, facilitating rethrombosis via the cleavage of fibrinogen to fibrin.6 In addition, high blood flow velocity due to remaining arterial stenosis may further activate platelet aggregation. Thus, a blockade of platelet-mediated thrombotic mechanisms appeared to be a rational approach to the management of this patient, as platelets seemed to play a key role in the rethrombosis. Highly effective inhibition of platelet activity can be achieved by the introduction of potent inhibitors of the GP IIb/IIIa receptor.
It has been reported that GP IIb/IIIa receptor blockers can decrease the incidence of restenosis and ischemic complications after percutaneous transcoronary angioplasty.7 Recently, GP IIb/IIIa receptor blockers were advocated as potentially promising agents for acute stroke therapy, and there were some case studies reporting the successful rescue use of GP IIb/IIIa receptor blocker in acute ischemic stroke.6,8-10 Tirofiban is a non-peptide tyrosine derivative that mimics the RGD integrin recognition sequence. It has a very short platelet-bound half-life and a relatively long plasma half-life, therefore providing an advantage when the rapid reversal of antiplatelet action is required such as in cases of high-risk hemorrhage or in combined use with thrombolytics. It has been reported that tirofiban produces a dose-dependent, dethrombotic effect on thrombosis and inhibits acute de novo stent thrombosis under high-shear flow conditions in an ex vivo canine arteriovenous shunt model.11 Tirofiban is generally used intravenously in coronary artery disease, with a loading dose of 0.4 µg/kg/min for 30 minutes and a subsequent infusion of 0.1 µg/kg/min. We initially planned to use the standard intravenous loading dose (900 µg) intra-arterially; however, after use of only 200 µg intra-arterial tirofiban, the ICA was successfully recanalized. We speculate that intra-arterial drug delivery may reduce the dose of tirofiban required to dissolve the thrombus.
This case demonstrates that a GP IIb/IIIa receptor blocker is effective for the recanalization of reoccluded arteries, especially in the presence of arterial stenosis. The dose of GP IIb/IIIa receptor blocker can be reduced by intra-arterial use, as compared with intravenous use and may be effective at preventing hemorrhagic complications, especially when used in combination with thrombolytics. Although this case showed promising results of intra-arterial tirofiban use, further studies are necessary to verify the effect of intra-arterial use of tirofiban and to determine its proper dose.
References
- 1.Alexandrov AV, Grotta JC. Arterial reocclusion in stroke patients treated with intravenous tissue plasminogen activator. Neurology. 2002;59:862–867. doi: 10.1212/wnl.59.6.862. [DOI] [PubMed] [Google Scholar]
- 2.Qureshi AI, Siddiqui AM, Kim SH, Hanel RA, Xavier AR, Kirmani JF, et al. Reocclusion of recanalized arteries during intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol. 2004;25:322–328. [PMC free article] [PubMed] [Google Scholar]
- 3.Heo JH, Lee KY, Kim SH, Kim DI. Immediate reocclusion following a successful thrombolysis in acute stroke: a pilot study. Neurology. 2003;60:1684–1687. doi: 10.1212/01.wnl.0000063323.23493.98. [DOI] [PubMed] [Google Scholar]
- 4.Seitz RJ, Meisel S, Moll M, Wittsack HJ, Junghans U, Siebler M. The effect of combined thrombolysis with rtPA and tirofiban on ischemic brain lesions. Neurology. 2004;62:2110–2112. doi: 10.1212/01.wnl.0000129480.17345.4a. [DOI] [PubMed] [Google Scholar]
- 5.Straub S, Junghans U, Jovanovic V, Wittsack HJ, Seitz RJ, Siebler M. Systemic thrombolysis with recombinant tissue plasminogen activator and tirofiban in acute middle cerebral artery occlusion. Stroke. 2004;35:705–709. doi: 10.1161/01.STR.0000117094.41638.EE. [DOI] [PubMed] [Google Scholar]
- 6.Lee KY, Heo JH, Lee SI, Yoon PH. Rescue treatment with abciximab in acute ischemic stroke. Neurology. 2001;56:1585–1587. doi: 10.1212/wnl.56.11.1585. [DOI] [PubMed] [Google Scholar]
- 7.The EPIC Investigators. Use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. N Engl J Med. 1994;330:956–961. doi: 10.1056/NEJM199404073301402. [DOI] [PubMed] [Google Scholar]
- 8.Wallace RC, Furlan AJ, Moliterno DJ, Stevens GH, Masaryk TJ, Perl J., 2nd Basilar artery rethrombosis: successful treatment with platelet glycoprotein IIB/IIA receptor inhibitor. AJNR Am J Neuroradiol. 1997;18:1257–1260. [PMC free article] [PubMed] [Google Scholar]
- 9.Liebeskind DS, Pollard JR, Schwartz ED, Cucchiara BL, McGarvey ML, Hurst RW. Vertebrobasilar thrombolysis with intravenous tirofiban: case report. J Thromb Thrombolysis. 2002;13:81–84. doi: 10.1023/a:1016242713327. [DOI] [PubMed] [Google Scholar]
- 10.Ho DS, Wang Y, Chui M, Wang Y, Ho SL, Cheung RT. Intracarotid abciximab injection to abort impending ischemic stroke during carotid angioplasty. Cerebrovasc Dis. 2001;11:300–304. doi: 10.1159/000047657. [DOI] [PubMed] [Google Scholar]
- 11.Rukshin V, Azarbal B, Finkelstein A, Shah PK, Cercek B, Tsang V, et al. Effects of GP IIb/IIIa receptor inhibitor tirofiban (aggrastat) in ex vivo canine arteriovenous shunt model of stent thrombosis. J Cardiovasc Pharmacol. 2003;41:615–624. doi: 10.1097/00005344-200304000-00015. [DOI] [PubMed] [Google Scholar]


