Abstract
Background
Few data are available on the secular changes in sudden coronary heart disease (CHD) death in U.S. communities.
Methods
We examined trends in sudden CHD death from 1987 to 2004, using data from the Atherosclerosis Risk in Communities (ARIC) study. Sudden CHD deaths in residents aged 35–74 years of four communities were ascertained using multiple sources such as death certificates, informant and coroner interviews, and physician adjudications. Poisson regression was used to assess the trends for the six time periods: 1987–1989, 1990–1992, 1993–1995, 1996–98, 1999–2001, 2002–2004, after adjusting for demographic factors.
Results
Overall, 32.6% of CHD deaths were sudden, occurring within an hour after the onset of symptoms, 63.5% of which had no prior diagnosis of CHD. For women, the rate declined by 40% (P=0.059) for sudden deaths with CHD history, 27% (P=0.067) for those without CHD history, and 39% (P<0.001) for non-sudden CHD deaths. The trends did not differ by community. For men, the trends differed by community for sudden deaths with and without CHD history (Ps for the interaction=0.019 and 0.009, respectively) but not for non-sudden CHD death (P for the interaction=0.10). For all communities combined, the decline in men was greatest for sudden deaths with CHD history (by 58%, P<0.001), followed by non-sudden CHD deaths (by 39%, P<0.001) and sudden deaths without CHD history (by 31%, P=0.002). However, the proportion of CHD deaths that were sudden had remained stable over time.
Conclusion
Although the rate of sudden CHD deaths, with and without CHD history, declined over time, the trend pattern may differ by community and gender.
Keywords: Death, sudden, coronary disease, epidemiology, prevention
Sudden cardiac death (SCD) generally is defined as unexpected natural death due to a cardiac cause within an hour after the onset of acute symptoms.(1) The majority of SCD is a result of ventricular arrhythmia subsequent to coronary heart disease (CHD), often as the first manifestation of CHD.(2–4) Currently recommended strategies to reduce SCD are three-fold: 1) primary prevention of CHD, especially among those at high risk of CHD, 2) prevention of arrhythmias and sudden death among patients with coronary artery disease, and 3) improvement of survival after cardiac arrest through a chain of intervention strategies.(5;6)
The relative contribution of primary prevention versus treatment to the decline in CHD mortality in the U.S. has not been fully elucidated.(7–9) Recent studies attempted to measure the trend in SCD among persons without CHD history, as an indicator of primary prevention, and demonstrated that these “first event” SCD death rates have fallen over time.(2;3) These studies, however, differed in case definition, geographic area, and study population, and were limited by their generalizability due to study settings in confined geographic areas or in a single race cohort.
Since 1987, the Atherosclerosis Risk in Communities (ARIC) study has been monitoring the CHD incidence and mortality in four U.S. communities. All deaths have been ascertained uniformly using multiple sources such as death certificates, informant and coroner interviews, and physician adjudications. The ARIC study thus provides a unique opportunity to assess the magnitude of and trends in rates of sudden CHD death with and without CHD history, as compared with non-sudden CHD deaths, and to measure the changes by demographic subgroups and communities.
METHODS
The ARIC community surveillance is conducted in four communities: Forsyth County, NC; Jackson, MS; suburbs of Minneapolis, MN; and Washington County, MD. Hospitalized acute myocardial infarction (MI) cases and CHD deaths among residents aged 35–74 years (population about 360,000) were eligible for the surveillance registration. The study was approved by the institutional review committee of the participating field centers. The detailed design and methods used in the ARIC community surveillance has been described previously.(10)
Briefly, for CHD deaths, trained staff obtained death certificates that met criteria based on age, community residence, and underlying cause of death (ICD-9 codes 250, 401, 402, 410–414, 427–429, 440, 518.4, 798, and 799; for years 1999 and after, ICD-10 codes E10–14, I10–11, I21–25, I46–51, I70, I97, J81, J96, R96, R98–99). Various sampling fractions were applied to different classes of ICD codes for investigation.(11) For out-of-hospital deaths, next of kin and other informants, certifying and family physicians, and coroner or medical examiners were contacted to obtain information on the circumstances of death, prior symptoms, timing of symptoms before death, and medical history. Two physicians from the Morbidity and Mortality Classification Committee (MMCC) reviewed each out-of-hospital death independently and assigned a final diagnosis using the ARIC criteria.(10) When the two reviewers disagreed on the diagnosis, the MMCC Chair made the final classification.
Deaths were classified into definite or possible CHD deaths, non-CHD death, and unclassified.(12) Prior to 1995, Maryland state law prohibited the contact of next-of-kin, and therefore deaths occurring in Washington County were excluded from the main trend assessment for the full period 1987 to 2004 but were included in a separate analysis for Washington County data from 1996 to 2004.
In this analysis, sudden CHD death was defined as those assigned to a cause of definite or possible CHD death, that occurred within one hour after the onset of acute symptoms. Over the study period, the information on timing of the events was not available for 12.9% of CHD deaths, ranging from 10.8% to 17.4%. The percent missing over total CHD deaths did not systematically increase or decrease over time. Therefore, deaths with unknown timing of symptom onset were excluded from the analyses. Prior history of CHD was based on physician, coroner, or next of kin reports of a history of angina, coronary insufficiency, or MI. Those with unknown CHD history (17.6%), ranging from 13.8% to 20.4% over time, were excluded from the analyses. Compared with those included in the analysis, excluded cases were more likely to be women (36.8% vs. 32.8%, P=0.008) and African Americans (41.4% vs. 30.7%, P<0.001). Mean age for the excluded was slightly younger than the included (62.4 vs. 63.0 years, P=0.030). The proportions of the excluded were similar among the communities. A sensitivity analysis was performed to address the impact of the exclusions on the trend assessment. It addressed the uncertainties of the values by conducting analyses with various assumptions surrounding unknown CHD history (with or without CHD history) and timing of symptom onset (sudden or not-sudden).
Death rates were computed based on population estimates derived by interpolation from U.S. census data. The direct standardization method was used to calculate age-and race-adjusted death rates using the 2000 population as the standard. To assess the relative impact of changes in sudden CHD deaths on total CHD mortality, non-sudden CHD death rate was also estimated.
The trend analyses were based on combined data from the three communities (Forsyth County, Jackson, and Minneapolis) with complete data from 1987 to 2004. To improve the precision of point estimates, we grouped data into six time periods: 1987–89, 1990–92, 1993–95, 1996–98, 1999–2001, and 2002–04, with the period 1987–89 as the referent period. Poisson regression was used to assess trends in the death rates. Risk ratios for the death rates by time periods were estimated after adjusting for age, race, and community. Because previously reported CHD mortality trends in ARIC communities differed by gender (In this analysis, P value for the interaction between year and gender is 0.1888 for sudden CHD deaths with history of CHD, 0.7853 for sudden deaths without history of CHD, and 0.2678 for non-sudden CHD deaths), the analyses were stratified by gender. Comparison of time trends by communities, between race groups, and across age groups was accomplished by including two way interaction terms (year-group x age groups, year-group x race, and year-group x community) at alpha level of 0.20. All analyses were conducted using SUDAAN (Research Triangle Park, NC) to account for the stratified sampling scheme.
RESULTS
From 1987 to 2004, 7,434 CHD deaths with known CHD history and timing of the events were identified from the three communities with complete data, 32.6% of which occurred suddenly. Of those who died suddenly from CHD, 63.5% did not have a prior CHD diagnosis. Similarly in Washington County, 32.2% of CHD deaths were sudden deaths; 55.9% of those sudden deaths occurred as a first CHD event.
Table 1 shows the population characteristics and crude CHD death rates by community. During the study period, the percent of younger residents (35–54 years) and African Americans increased slightly over time. Overall, the proportion of African Americans was 22% in Forsyth County; 56% in Jackson; 5% in suburbs of Minneapolis; and 6% in Washington County. The crude death rates (total CHD and sudden CHD deaths) declined over time in the three communities, with greater declines in Minneapolis.
Table 1.
Population characteristics and crude death rates from coronary heart disease in the three communities: ARIC Community Surveillance Study 1987–2004
| Community Characteristic | 1987–1989 | 1990–1992 | 1993–1995 | 1996–1998 | 1999–2001 | 2002–2004 |
|---|---|---|---|---|---|---|
| Total population (in 1,000) | 262 | 277 | 287 | 296 | 306 | 316 |
| Percent distribution | ||||||
| Age Group | ||||||
| 35–54 | 62 | 63 | 65 | 66 | 67 | 68 |
| 55–64 | 22 | 21 | 20 | 20 | 19 | 18 |
| 65–74 | 16 | 16 | 15 | 15 | 14 | 14 |
| Men | 46 | 46 | 47 | 47 | 47 | 47 |
| Race* | ||||||
| African American | 20 | 21 | 23 | 24 | 25 | 26 |
| White | 80 | 79 | 77 | 76 | 75 | 74 |
| Community | ||||||
| Forsyth County, NC | 42 | 42 | 43 | 44 | 45 | 45 |
| Jackson, MS | 27 | 26 | 25 | 24 | 23 | 22 |
| Minneapolis, MN | 31 | 32 | 32 | 32 | 32 | 32 |
| Crude CHD death rate†, per 1,000 | ||||||
| Community | ||||||
| Forsyth County, NC | 2.07 | 1.52 | 1.55 | 1.47 | 1.14 | 1.07 |
| Jackson, MS | 2.54 | 2.45 | 2.15 | 1.98 | 2.17 | 1.49 |
| Minneapolis, MN | 1.13 | 1.03 | 1.13 | 0.87 | 0.57 | 0.45 |
| Crude sudden CHD death rate†, per 1,000 | ||||||
| Forsyth County, NC | 0.72 | 0.53 | 0.49 | 0.50 | 0.40 | 0.33 |
| Jackson, MS | 0.70 | 0.73 | 0.79 | 0.63 | 0.72 | 0.53 |
| Minneapolis, MN | 0.37 | 0.32 | 0.41 | 0.21 | 0.19 | 0.11 |
Races other than African American or white were excluded.
Excludes those with missing timing or missing prior history of CHD diagnosis.
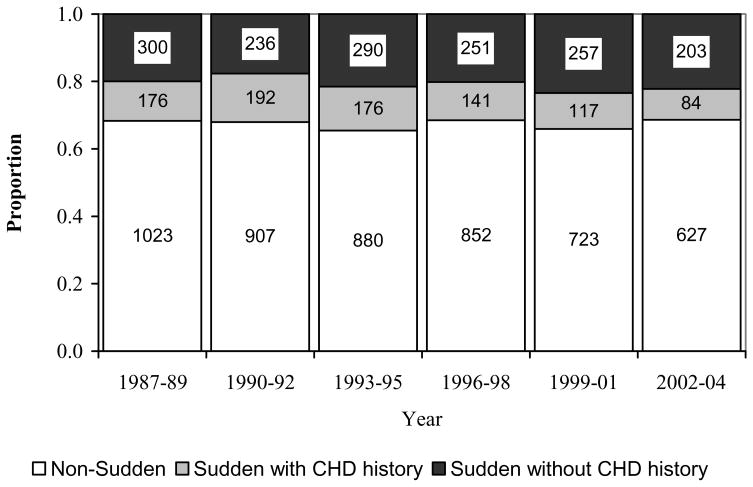
The proportion of CHD deaths that were sudden with a prior CHD diagnosis, sudden without prior CHD diagnosis, or non-sudden remained relatively stable during the six time periods (Figure 1). Stratified analysis by community revealed the same pattern for Forsyth County, suburbs of Minneapolis, and Washington County (data not shown). For Jackson, however, the proportion of sudden deaths without prior CHD diagnosis increased significantly from 19.4% in 1987–89 to 28.2% in 2002–04.
Figure 1.
Proportion of deaths due to coronary heart disease (CHD) that were sudden without prior CHD history, sudden with prior CHD history, and non-sudden CHD: ARIC Community Surveillance study 1987–2004
Table 2 shows the characteristics of sudden and non-sudden CHD deaths during the six study periods. Among all sudden CHD deaths, the proportion without a prior CHD diagnosis increased slightly from 63.0% in 1987–89 to 70.7% in 2002–04 (age, sex, race adjusted P for linear trend =0.013). Throughout the study period, approximately half of non-sudden CHD deaths and almost all sudden CHD deaths occurred out of the hospital. For Washington County (data not shown), the proportion of sudden deaths without prior CHD history also increased from 47.8% in 1996–98 to 62.7% in 1999–2001and 62.5% in 2002–04. Similarly, approximately half of non-sudden CHD deaths and almost all sudden CHD deaths occurred out of the hospital.
Table 2.
Characteristics of the sudden and non-sudden CHD deaths: ARIC Community Surveillance Study 1987–2004
| Characteristic | 1987–89 | 1990–92 | 1993–95 | 1996–98 | 1999–01 | 2002–04 | Trend P-value* |
|---|---|---|---|---|---|---|---|
| Total CHD deaths | 1,499 | 1,335 | 1,346 | 1,244 | 1,096 | 914 | |
| Percent† | |||||||
| Sudden | 31.7 | 32.1 | 34.6 | 31.5 | 34.1 | 31.4 | 0.799 |
| Non-sudden | 68.3 | 67.9 | 65.4 | 68.5 | 65.9 | 68.6 | 0.799 |
| Sudden CHD deaths | |||||||
| Age group, years | |||||||
| 35–54 | 17.9 | 23.1 | 21.3 | 24.8 | 28.1 | 28.5 | 0.002 |
| 55–64 | 32.9 | 30.4 | 27.7 | 30.3 | 28.3 | 29.4 | 0.234 |
| 65–74 | 49.3 | 46.5 | 50.9 | 44.8 | 43.5 | 42.1 | 0.095 |
| Men | 76.5 | 69.9 | 77.1 | 70.5 | 73.4 | 70.4 | 0.403 |
| African American | 30.1 | 26.5 | 29.2 | 35.4 | 40.1 | 41.3 | <0.001 |
| First event | 63.0 | 55.1 | 62.2 | 64.0 | 68.7 | 70.7 | 0.013 |
| Out-of-Hospital | 99.6 | 97.8 | 99.8 | 100.0 | 99.4 | 98.9 | 0.798 |
| Community | |||||||
| Forsyth County | 50.1 | 43.1 | 39.1 | 49.9 | 43.9 | 49.3 | 0.311 |
| Jackson | 31.3 | 37.3 | 36.8 | 34.4 | 41.4 | 39.1 | 0.846 |
| Minneapolis | 18.6 | 19.5 | 24.1 | 15.6 | 15.0 | 11.6 | 0.003 |
| Non-sudden CHD deaths | |||||||
| Age group, years | |||||||
| 35–54 | 13.6 | 13.7 | 16.1 | 17.3 | 19.8 | 19.5 | 0.001 |
| 55–64 | 30.4 | 28.6 | 23.3 | 24.4 | 28.8 | 26.2 | 0.083 |
| 65–74 | 55.9 | 57.7 | 60.7 | 58.3 | 51.4 | 54.3 | 0.465 |
| Men | 65.2 | 64.2 | 62.7 | 64.2 | 62.7 | 66.7 | 0.640 |
| African American | 25.6 | 30.0 | 26.0 | 26.8 | 38.0 | 34.9 | <0.001 |
| First event | 50.1 | 53.1 | 55.0 | 52.9 | 63.2 | 65.3 | <0.001 |
| Out-of-Hospital | 50.5 | 56.1 | 50.0 | 46.6 | 53.6 | 48.5 | 0.052 |
| Community | |||||||
| Forsyth County, NC | 43.4 | 37.8 | 44.1 | 43.9 | 41.6 | 50.9 | 0.002 |
| Jackson, MS | 38.7 | 41.5 | 33.5 | 34.3 | 42.8 | 32.5 | 0.001 |
| Minneapolis, MN | 18.0 | 20.7 | 22.4 | 21.8 | 15.7 | 16.6 | 0.212 |
Linear trend P-value from a logistic regression model adjusted for age, race, and sex where appropriate.
Unadjusted percents.
Note: Excludes decedents with race other than African American or white, and deaths from Washington County, MD. Also excludes those with missing timing or missing prior history of CHD diagnosis.
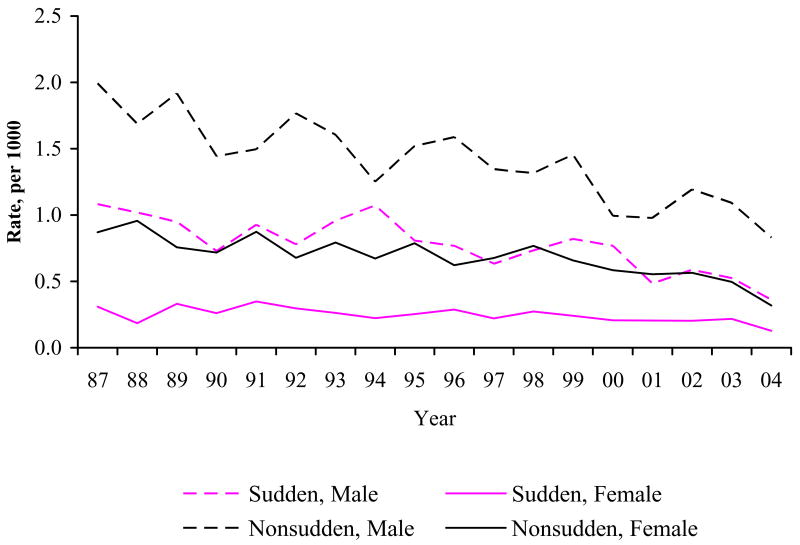
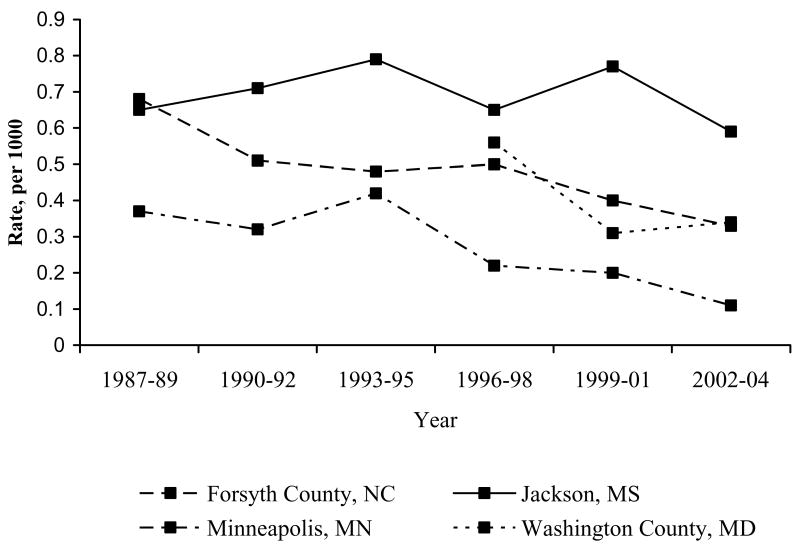
Figure 2 shows age- and race-adjusted death rates from 1987 to 2004, by type of CHD deaths (sudden vs. non-sudden) and gender. A decreasing trend was seen in the sudden death rate for both men and women, although a greater decline was observed in the non-sudden death rate, especially for men. Figure 3 shows the trends in age- and gender-adjusted sudden CHD death rates by community during the six study periods. A fall in sudden CHD death rate was seen in Forsyth County and suburbs of Minneapolis, but not in Jackson. During 1996 to 2004, the sudden CHD death rate also declined in Washington County.
Figure 2.
Age-and race-adjusted rate of sudden and non-sudden deaths from coronary heart disease, by gender: ARIC Community Surveillance Study 1987–2004
Figure 3.
Age- and gender adjusted rate of sudden death from coronary heart disease, by community and study period: ARIC Community Surveillance Study 1987–2004
Trends in sudden and non-sudden CHD death rates after adjusting for age, race, and community are shown in Tables 3 (for women) and 4 (for men). For women, the trends in the rates of sudden death with CHD history and non-sudden CHD death did not differ significantly by community (Ps for the interaction = 0.292 and 0.253, respectively), but the trend in sudden deaths without CHD history marginally differed by community (P for interaction = 0.073). For all three communities combined, the rate in women declined by 40% for sudden deaths with prior CHD diagnosis and 27% for those without prior CHD diagnosis, but the reductions did not reach statistical significance (Ps = 0.059 and 0.067, respectively). However, a significant decline (39% reduction) was seen in non-sudden death (with or without CHD history) among women in all three communities (36% to 55%) during the study period. For men, the trends differed by community for sudden deaths with and without prior CHD diagnosis (Ps for the interaction = 0.019 and 0.008, respectively) but not for non-sudden death (P for the interaction =0.10). The male rate of sudden deaths without prior CHD diagnosis declined by 45% in Forsyth County and 46% in Minneapolis, but stayed flat in Jackson. A decreasing trend was seen in all three communities for sudden deaths with prior CHD diagnosis, although the reduction was smaller (not statistically significant) in Jackson compared with other two communities. For all communities combined, the decline in men was greatest for sudden deaths with prior CHD diagnosis (by 58%), followed by non-sudden deaths (by 39%) and sudden deaths without prior CHD diagnosis (by 31%).
Table 3.
Rate ratio of sudden deaths with prior CHD, sudden death without prior CHD diagnosis, and non-sudden CHD deaths among women: ARIC Community Surveillance Study 1987–2004
| 1987–89 | 1990–1992
|
1993–1995
|
1996–1998
|
1999–2001
|
2002–2004
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | Trend P-Value | ||
| Sudden CHD Death, with history of CHD | ||||||||||||
| All communities | 1.00 | 0.90 | 0.81, 1.00 | 0.81 | 0.66, 1.01 | 0.73 | 0.53, 1.01 | 0.66 | 0.43, 1.02 | 0.60 | 0.35, 1.02 | 0.059 |
| Forsyth County, NC | 1.00 | 0.93 | 0.81, 1.05 | 0.86 | 0.66, 1.11 | 0.79 | 0.54, 1.16 | 0.73 | 0.44, 1.22 | 0.68 | 0.36, 1.28 | 0.234 |
| Jackson, MS | 1.00 | 0.97 | 0.76, 1.23 | 0.93 | 0.57, 1.52 | 0.90 | 0.43, 1.87 | 0.87 | 0.33, 2.31 | 0.84 | 0.25, 2.85 | 0.778 |
| Minneapolis, MN | 1.00 | 0.78 | 0.63, 0.95 | 0.60 | 0.40, 0.91 | 0.47 | 0.25, 0.87 | 0.36 | 0.16, 0.82 | 0.28 | 0.10, 0.79 | 0.015 |
| Sudden CHD Death, without history of CHD | ||||||||||||
| All communities | 1.00 | 0.94 | 0.88, 1.00 | 0.88 | 0.77, 1.01 | 0.83 | 0.68, 1.01 | 0.78 | 0.59, 1.02 | 0.73 | 0.52, 1.02 | 0.067 |
| Forsyth County, NC | 1.00 | 0.93 | 0.84, 1.03 | 0.86 | 0.70, 1.06 | 0.80 | 0.59, 1.09 | 0.75 | 0.50, 1.13 | 0.70 | 0.42, 1.16 | 0.165 |
| Jackson, MS | 1.00 | 0.99 | 0.90, 1.08 | 0.97 | 0.81, 1.18 | 0.96 | 0.72, 1.28 | 0.95 | 0.65, 1.38 | 0.93 | 0.58, 1.50 | 0.779 |
| Minneapolis, MN | 1.00 | 0.77 | 0.64, 0.93 | 0.60 | 0.41, 0.87 | 0.46 | 0.26, 0.81 | 0.36 | 0.17, 0.75 | 0.27 | 0.11, 0.70 | 0.007 |
| Non Sudden CHD Death (with or without history of CHD) | ||||||||||||
| All communities | 1.00 | 0.91 | 0.88, 0.94 | 0.82 | 0.77, 0.88 | 0.75 | 0.67, 0.83 | 0.68 | 0.59, 0.78 | 0.61 | 0.52, 0.73 | 0.000 |
| Forsyth County, NC | 1.00 | 0.91 | 0.88, 0.95 | 0.84 | 0.78, 0.90 | 0.77 | 0.68, 0.86 | 0.70 | 0.60, 0.81 | 0.64 | 0.53, 0.77 | 0.000 |
| Jackson, MS | 1.00 | 0.92 | 0.87, 0.98 | 0.85 | 0.75, 0.97 | 0.79 | 0.65, 0.95 | 0.73 | 0.57, 0.94 | 0.67 | 0.49, 0.92 | 0.014 |
| Minneapolis, MN | 1.00 | 0.85 | 0.79, 0.92 | 0.73 | 0.62, 0.85 | 0.62 | 0.49, 0.79 | 0.53 | 0.39, 0.73 | 0.45 | 0.31, 0.67 | 0.000 |
Rate ratio (RR) estimates using year group as a continuous variable in Poisson regression model. Dependent variable is number of deaths, adjusted for race, age group and community.
Further stratified analysis by race and gender showed that in Jackson, age-adjusted death rates for sudden CHD death without prior CHD diagnosis remained stable over time for both whites and African Americans (data not shown). The pattern did not differ by gender. Similarly, the decline in sudden death rate with prior CHD history did not differ by race in Jackson men. For Forsyth County, however, age-adjusted rates of sudden deaths with and without prior CHD history significantly declined in white men (similar to whites in Minneapolis, Ps = 0.188 and 0.935) but not in African American men.
Sensitivity analysis indicated that regardless of whether all CHD deaths with an unknown timing of symptom onset to death were assumed to be sudden or non-sudden, the trend patterns observed by community stayed similar for both women and men (data now shown). However, when all deaths with unknown history of CHD were assumed to be “present,” the magnitude of decline in sudden deaths with CHD history for Jackson community became diluted and non-statistically significant, whether all deaths with missing timing of symptom onset were assumed to be sudden or non-sudden.
DISCUSSION
This study provides the 17-year trends (1987 to 2004) in sudden CHD deaths, with and without prior CHD diagnosis, based on a large community-based surveillance study of residents aged 35–74 years. The classification of sudden CHD death was enhanced by multiple sources of ascertainment and information. The results reveal a decreasing trend in the overall sudden CHD death rate comparable to the decline in the non-sudden CHD death rate. The rate for sudden deaths without prior CHD diagnosis declined in the communities combined, significantly in men and marginally significantly in women. Importantly, this decline was found to differ by community, significantly in men and marginally significantly in women.
The findings from this study regarding the reduced mortality from sudden deaths as a first CHD event is congruent with findings presented recently by two other population-based studies.(2;3) A decline in “unexpected” SCD, defined as SCD deaths without prior CHD diagnosis, was noted in Olmsted County, MN from 1979 to 1998, although the study defined SCD as out-of-hospital physician validated CHD death occurring less than 24 hours after symptom onset.(3) The Framingham Heart Study, which used a definition similar to the present study but based on a single cohort, reported that the risk of sudden CHD deaths for those without CHD history or heart failure was 39% lower in 1990–1999 than in 1950–1969.(2) By analyzing data from a population-based surveillance study in several U.S. communities, the present study provides additional evidence for the important role of primary prevention in the reduction of total CHD mortality.
Compared with other studies including coronary deaths only, the estimated sudden CHD death rates from this study were lower, possibly due to the differences in case definition, study populations, and exclusion of deaths with unknown timing of event or CHD history.(2;3) Various criteria have been used to define sudden cardiac death in population-based studies, with major differences in the time frame used to define “sudden” (<1 hour vs.<24 hours) and ascertainment of cause or cardiac origin of death (by death certificates alone or by multiple sources of information). The “1 hour” time frame is used to account for a more likely arrhythmic mechanism, but may result in underestimating the “true” sudden cases because of the unwitnessed deaths. Using “out of hospital” as a surrogate of SCD based on death certificates was found to overestimate SCD incidence when compared with the results from multiple source surveillance.(13) This view is supported by our finding that nearly 50% of non-sudden CHD deaths in this study occurred outside a hospital.
Geographic variation in sudden coronary heart disease death in the U.S. was reported more than 10 years ago.(14) The present study identified community disparities in the trend pattern in sudden CHD deaths, especially among men. The decline in sudden deaths without prior CHD diagnosis was noticed for men in Forsyth County, Minneapolis, and Washington County, but not for men in Jackson. The same pattern was also noticed in women but the differences were not statistically significant. These disparities were not explained by differences in race distribution. Race-stratified analysis showed similar patterns in the trends for both whites and African Americans in Jackson men and women. The reasons for the disparities are unclear, but possible causes include the differences in the extent and effectiveness of primary prevention (e.g., blood pressure and lipid control, smoking cessation, weight management, and regular physical activity) and secondary prevention activities (e.g., awareness of the symptoms and signs of cardiac arrest, the number of trained bystanders, the usage of implantable cardioverter defibrillator (ICD), and availability and use of automated external defibrillators (AED) in public places). Further study is needed to examine the impact of community characteristics, such as household income and education (by linking death records to the Census data), and access and utilization of needed emergency care, on the occurrence of sudden deaths.
The findings in this report are subject to some limitations. First, the reported CHD and sudden CHD death rates are underestimated because of excluding a significant proportion of CHD deaths with unknown history of CHD or unknown timing between onset of symptoms and deaths. However, the percent missing over total CHD deaths did not systematically increase or decrease over time, and should not affect trend assessment in CHD death rates. Also, our sensitivity analysis showed that the time trend in CHD death rate or sudden CHD death rate was qualitatively similar whether all or none of cases with missing CHD history were counted as first CHD events, or whether all or none of the missing timing values were included as sudden CHD death. Secondly, this study did not collect detailed information such as the role of witnesses and resuscitation attempts, and thus cannot evaluate the impact of resuscitation advances on the reduction of sudden and non-sudden CHD deaths. Thirdly, the information on prior diagnosis of CHD for sudden deaths was mainly obtained from informants, which might have resulted in some misclassification of the CHD history. Nevertheless, we are not aware of any evidence for a systematic change over time in this reporting, and thus any misclassification should not impact on the trend assessment. Furthermore, due to a lack of community and decedent data on specific risk factors, such as smoking, blood pressure, and complete medical history, this study cannot delineate the reasons for declining sudden cardiac deaths. Finally, the study was conducted in residents aged 35–74 years of several U.S. communities, and may not applicable to other age groups and geographic areas.
Notwithstanding these limitations, ARIC study provides unique advantages for the study of sudden CHD death and its impact on the total CHD mortality. It is important to note that the proportion of CHD deaths that were sudden had remained relatively stable in ARIC study communities during the study period. Further efforts are needed to identify and support best practices in treatment and prevention for CHD and SCD.
Table 4.
Rate ratio of sudden deaths with prior CHD, sudden death without prior CHD diagnosis, and non-sudden CHD deaths among men: ARIC Community Surveillance Study 1987–2004
| 1987–1989 | 1990–1992 | 1993–1995 | 1996–1998 | 1999–2001 | 2002–2004 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | RR* | 95% CI | Trend P-Value | ||
| Sudden CHD Death, History of CHD | ||||||||||||
| All communities | 1.00 | 0.84 | 0.80, 0.88 | 0.71 | 0.65, 0.78 | 0.60 | 0.52, 0.69 | 0.50 | 0.42, 0.61 | 0.42 | 0.34, 0.53 | 0.000 |
| Forsyth County, NC | 1.00 | 0.84 | 0.79, 0.89 | 0.71 | 0.63, 0.80 | 0.60 | 0.50, 0.71 | 0.50 | 0.40, 0.63 | 0.42 | 0.32, 0.57 | 0.000 |
| Jackson, MS | 1.00 | 0.91 | 0.85, 0.99 | 0.84 | 0.72, 0.97 | 0.76 | 0.61, 0.96 | 0.70 | 0.52, 0.95 | 0.64 | 0.44, 0.93 | 0.020 |
| Minneapolis, MN | 1.00 | 0.76 | 0.69, 0.85 | 0.58 | 0.47, 0.72 | 0.44 | 0.32, 0.61 | 0.34 | 0.22, 0.51 | 0.26 | 0.15, 0.43 | 0.000 |
| Sudden CHD Death, No history of CHD | ||||||||||||
| All communities | 1.00 | 0.93 | 0.89, 0.97 | 0.86 | 0.79, 0.95 | 0.80 | 0.70, 0.92 | 0.75 | 0.62, 0.90 | 0.69 | 0.55, 0.88 | 0.002 |
| Forsyth County, NC | 1.00 | 0.89 | 0.83, 0.96 | 0.79 | 0.68, 0.91 | 0.70 | 0.56, 0.87 | 0.62 | 0.47, 0.83 | 0.55 | 0.39, 0.80 | 0.001 |
| Jackson, MS | 1.00 | 1.00 | 0.94, 1.07 | 1.01 | 0.89, 1.15 | 1.01 | 0.84, 1.23 | 1.02 | 0.79, 1.32 | 1.02 | 0.74, 1.41 | 0.887 |
| Minneapolis, MN | 1.00 | 0.88 | 0.83, 0.94 | 0.78 | 0.68, 0.89 | 0.69 | 0.56, 0.84 | 0.61 | 0.47, 0.79 | 0.54 | 0.39, 0.75 | 0.000 |
| Non Sudden CHD Death (with or without history of CHD) | ||||||||||||
| All communities | 1.00 | 0.91 | 0.88, 0.94 | 0.82 | 0.77, 0.88 | 0.75 | 0.68, 0.82 | 0.68 | 0.60, 0.77 | 0.61 | 0.52, 0.72 | 0.000 |
| Forsyth County, NC | 1.00 | 0.90 | 0.86, 0.95 | 0.81 | 0.74, 0.90 | 0.74 | 0.63, 0.85 | 0.66 | 0.54, 0.81 | 0.60 | 0.47, 0.77 | 0.000 |
| Jackson, MS | 1.00 | 0.94 | 0.90, 0.98 | 0.88 | 0.80, 0.97 | 0.83 | 0.72, 0.95 | 0.78 | 0.64, 0.94 | 0.73 | 0.58, 0.92 | 0.009 |
| Minneapolis, MN | 1.00 | 0.86 | 0.81, 0.92 | 0.74 | 0.65, 0.84 | 0.64 | 0.53, 0.77 | 0.55 | 0.43, 0.71 | 0.48 | 0.35, 0.65 | 0.000 |
Rate ratio (RR) estimates using year group as a continuous variable in Poisson regression model. Dependent variable is number of deaths, adjusted for race, age group and community.
Acknowledgments
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022. The authors thank the staff and participants of the ARIC study for their important contributions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98:2334–51. doi: 10.1161/01.cir.98.21.2334. [DOI] [PubMed] [Google Scholar]
- 2.Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004;110:522–27. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 3.Goraya TY, Jacobsen SJ, Kottke TE, Frye RL, Weston SA, Roger VL. Coronary heart disease death and sudden cardiac death: a 20-year population-based study. Am J Epidemiol. 2003;157:763–70. doi: 10.1093/aje/kwg057. [DOI] [PubMed] [Google Scholar]
- 4.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 5.Priori SG, Aliot E, Blomstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, et al. Task Force on Sudden Cardiac Death of the European Society of Cardiology. Eur Heart J. 2001;22:1374–450. doi: 10.1053/euhj.2001.2824. [DOI] [PubMed] [Google Scholar]
- 6.Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) J Am Coll Cardiol. 2006;48:e247–e346. doi: 10.1016/j.jacc.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Levy D, Thom TJ. Death rates from coronary disease--progress and a puzzling paradox. N Engl J Med. 1998;339:915–17. doi: 10.1056/NEJM199809243391309. [DOI] [PubMed] [Google Scholar]
- 8.Rosamond WD. Invited commentary: Trends in coronary heart disease mortality - Location, location, location. American Journal of Epidemiology. 2003;157:771–73. doi: 10.1093/aje/kwg058. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 10.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years' experience. J Clin Epidemiol. 1996;49:223–33. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 11.Rosamond WD, Chambless LE, Sorlie PD, Bell EM, Weitzman S, Smith JC, et al. Trends in the sensitivity, positive predictive value, false-positive rate, and comparability ratio of hospital discharge diagnosis codes for acute myocardial infarction in four US communities, 1987–2000. Am J Epidemiol. 2004;160:1137–46. doi: 10.1093/aje/kwh341. [DOI] [PubMed] [Google Scholar]
- 12.Rosamond WD, Folsom AR, Chambless LE, Wang CH. Coronary heart disease trends in four United States communities. The Atherosclerosis Risk in Communities (ARIC) study 1987–1996. Int J Epidemiol. 2001;30(Suppl 1):S17–S22. doi: 10.1093/ije/30.suppl_1.s17. [DOI] [PubMed] [Google Scholar]
- 13.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–75. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 14.Gillum RF. Geographic variation in sudden coronary death. Am Heart J. 1990;119:380–389. doi: 10.1016/s0002-8703(05)80031-6. [DOI] [PubMed] [Google Scholar]