Abstract
An acyclic, non-provitamin A carotene, lycopene is responsible for the red pigmentation of ripe tomatoes and some other edible fruits such as watermelon and papaya. Lycopene is also a potent antioxidant and scavenger of free radicals. Multiple retrospective and prospective epidemiological studies have indicated that the consumption of tomato products containing lycopene is associated with a reduced risk of prostate cancer. These epidemiological studies are supported by numerous in vitro assays using cell cultures that show anti-cancer activities and cancer chemoprevention activities of lycopene in many cell lines including prostate cancer cells. These activities include inducing apoptosis, inhibiting metastasis, preventing oxidative stress, and up-regulating the antioxidant response element so that cells can produce cytoprotective enzymes against prooxidants and electrophiles. In vivo animal studies and Phase I and II clinical trials have shown that lycopene supplements are non-toxic and that lycopene is orally bioavailable. Furthermore, lycopene is concentrated in prostate tissue and localized to the nucleus. In addition, some oxygenated metabolites of lycopene have been identified, and might be active as chemoprevention agents. The next phase of research concerning lycopene as a chemoprevention agent will be Phase II clinical trials of efficacy that are placebo-controlled, randomized and double blind. These clinical trials are required to establish the efficacy of lycopene supplementation.
1. Chemistry of lycopene
Lycopene (ψ,ψ-carotene), one of more than 600 carotenoids synthesized by plants and photosynthetic microorganisms [1], is a tetraterpene hydrocarbon containing 40 carbon atoms and 56 hydrogen atoms with a molecular mass of 536 (see structure in Figure 1) [2]. Lycopene is a lipophilic hydrocarbon that is soluble in chloroform, benzene and ether and practically insoluble in methanol, ethanol and water. Absorbance maxima of lycopene occur at 444, 470 and 502 nm (petroleum) resulting in its characteristic red color and ability to accept energy from various electronically excited species [3].
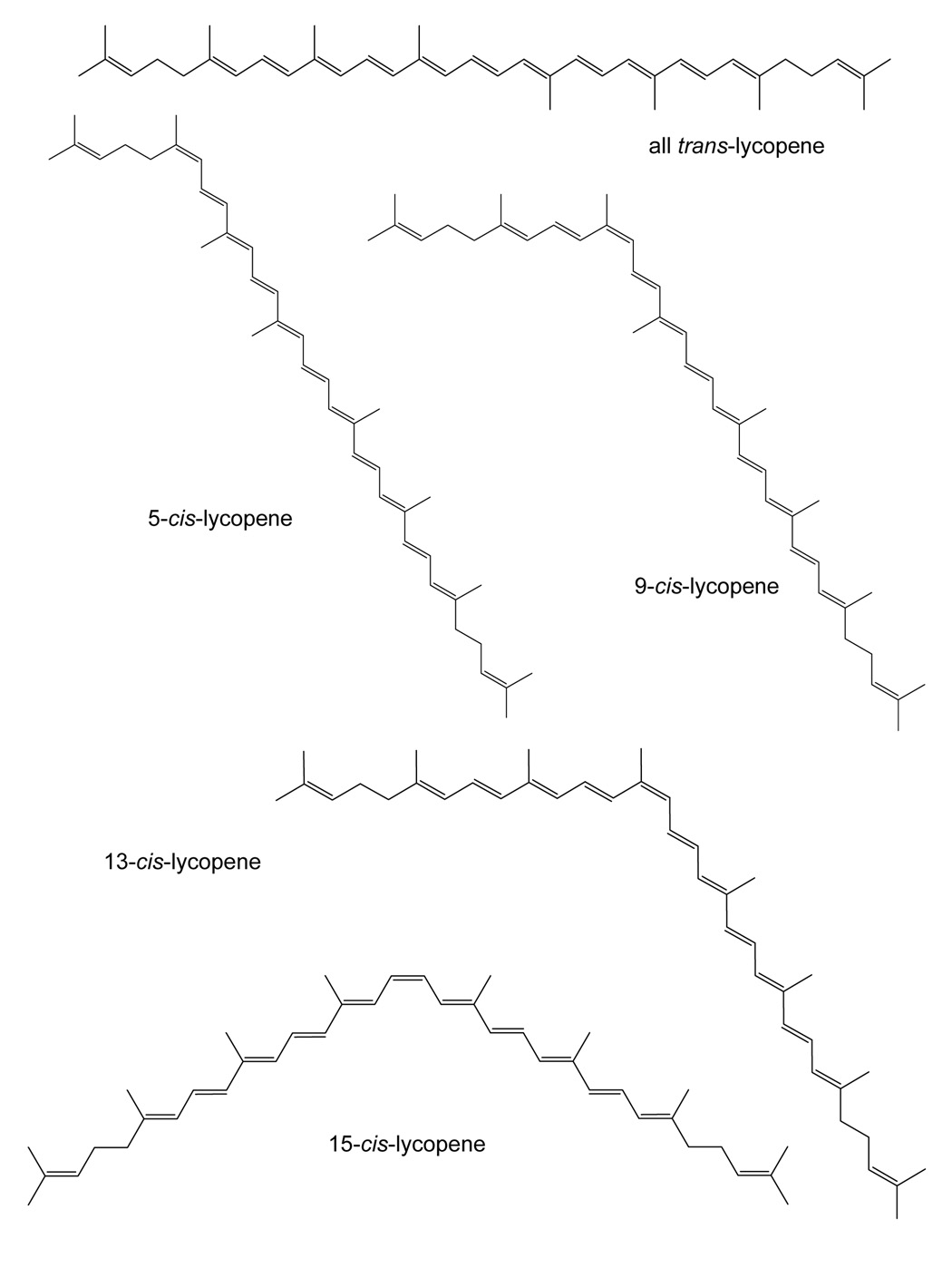
Figure 1.
Structures of all trans-lycopene and some of its most common cis-isomers.
Lycopene is the most abundant carotenoid in tomatoes (Lycopersicon esculentum L.) with concentrations ranging from 0.9–4.2 mg/100 g depending upon the variety [4]. Tomato sauce and ketchup are concentrated sources of lycopene (33–68 mg/100g) compared to unprocessed tomatoes [5]. Other edible sources of lycopene include rosehips [6], watermelon, papaya, pink grapefruit, and guava [7].
Belonging to the hydrocarbon carotene class of carotenoids, lycopene is acyclic and contains 11 conjugated and 2 non-conjugated double bonds (see Figure 1). Because it is acyclic and lacks a β-ionone ring, lycopene has no pro-vitamin A activity which sets its biochemistry apart from carotenes such as β-carotene and α-carotene. Synthesized biologically as the all-trans-isomer, lycopene in natural sources is predominantly present in the all-trans form. However, upon exposure to light, heat or through chemical reactions of these double bonds, isomerization can occur producing various mono- or poly-cis isomers of lycopene [4]. Although dietary lycopene is predominantly all-trans, more than 50% of the lycopene present in human serum and tissues is in cis-forms [8] (see Figure 1 for the structures of the most abundant cis-isomers of lycopene).
The extended conjugated polyene chain of lycopene is an electron-rich system, susceptible to attack by electrophilic reagents. Therefore, carotenoids like lycopene are unstable and highly reactive towards oxygen and free radicals [9]. Lycopene is rapidly destroyed by oxidation and by free radicals such as OH. and various peroxy radicals. This reactivity of lycopene is the basis for its anti-oxidant activity in biological systems that might contribute to its efficacy as a chemoprevention agent.
While in the plant matrix or in solid form, lycopene is relatively stable, but after extraction from the matrix and dissolution in a non-polar organic solvent, lycopene is quite unstable. For example, Fang et al. [10] evaluated the stability of lycopene in a mixture of methyl-tert-butyl ether and acetonitrile (50:50, v/v) protected from light and air and found that its half-life was ~16 h at 4 °C. Using a model aqueous system, Henry et al. [11] measured the degradation rates of several carotenes including lycopene and found that lycopene was the least stable of the carotenoids evaluated. In this system, the half-lives of lycopene exposed to water at 30 °C containing oxygen or nitrogen were ~1.7 h or 5.5 h, respectively; furthermore, lycopene was more than 8-fold less stable than all trans-β-carotene. In contrast to its instability in solution in its pure form, lycopene can be stabilized by encapsulation in water dispersible beadlets or in liposomes (see section on in vitro studies below for details). Therefore, the stability of lycopene must be a consideration during the preparation of samples containing lycopene or during in vitro or in vivo experiments with various lycopene preparations.
2. Molecular targets
In plants, carotenoids absorb light, transfer energy to chlorophyll in the process of photosynthesis and protect against photo-oxidative damage [12,13]. In humans, carotenoids function primarily as dietary sources of provitamin A. However, lycopene lacks the β-ionone ring structure required to form vitamin A and has no provitamin A activity. Therefore, lycopene has no known physiological function in humans. However, some potential molecular targets in cells have been identified for lycopene.
Antioxidant activity
Reactive oxygen species include superoxide (O2−.), and hydroxyl (OH.), peroxyl (RO2.) and alkoxyl (RO.) radicals, as well as non-radical species such as singlet oxygen, ozone (O3) and H2O2, which act either as oxidizing agents or can be easily converted to radicals [14]. The superoxide anion radical (O2−.) can be generated from oxygen during mitochondrial respiration by single electron transfer and is a major source of hydroxyl radicals. In addition, O2−. is converted either spontaneously or by the enzyme superoxide dismutase to hydrogen peroxide which can be transported across the nuclear membrane where it can react with metal ions to produce hydroxyl radicals [15]. In the presence of O2−. transition metals can be reduced and then catalyze the formation of hydroxyl radical from hydrogen peroxide by a Fenton-type reaction. Iron and copper are the most likely promoters of hydroxyl radical in vivo [16]. Finally, singlet oxygen 1O2 is another highly reactive oxygen species which can be formed by photooxidation, enzymatically or in the process of lipid peroxidation of biomembranes.
Due to its extended system of conjugated double bonds, lycopene can quench singlet oxygen and free radicals [17] and has been reported to be the most effective singlet oxygen quencher among approximately 600 naturally occurring carotenoids [18]. Oxidative stress caused by reactive oxygen species can result in damage to macromolecules such as carbohydrates, proteins, lipids, and DNA and may be involved in carcinogenesis, aging and the development of cardiovascular disease. As a quencher of singlet oxygen and a scavenger of free radicals, lycopene should be able to protect against oxidative stress. Lycopene can function as an antioxidant by several mechanisms, and one of the best documented mechanisms is through the quenching singlet oxygen (1O2). Physical quenching of 1O2 by lycopene can occur as follows [19]:
Lycopene in the excited state (3lycopene) has insufficient energy to cause excitation of other molecules and generate reactive species. Its excess energy is dissipated through a series of rotational and vibrational interactions with surrounding molecules, and then the regenerated carotenoid is able to quench additional singlet oxygen molecules. In this way, thousands of singlet oxygen molecules can be quenched by a single molecule of lycopene before it becomes degraded [20]. The quenching capacity of a carotenoid depends primarily on the number of conjugated double bonds it contains, which explains why lycopene is so efficient in quenching singlet oxygen [21].
Another mechanism for the antioxidant activity of lycopene is reaction with free radicals [9]. Carbon-centered carotenoid radicals formed in these reactions are resonantly stabilized by the long polyene chain. Electron density is not uniform along the chain but greater towards the ends, which are thus preferred sites for the reaction. Therefore, more than one free radical can be quenched by a single lycopene molecule [19].
It has also been suggested that lycopene might act as an antioxidant in vivo by repairing vitamin E and vitamin C radicals [22]:
In cell culture, lycopene at 0.31 to 10 µM was shown to inhibit nitration of proteins and DNA strand breakage caused by peroxynitrite treatment of Chinese hamster lung fibroblasts [23]. Oxidative DNA damage caused by the redox-cycling of catechol-estrogens in plasmid DNA and Chinese hamster lung fibroblasts was also reduced by lycopene at 0.25 to 10 µM [24]. In Hep3B cells treated with H2O2, lycopene was found to reduce DNA damage in a dose-dependent manner as indicated by the comet assay in Hep3B cells treated with [25]. Liu et al. [26] investigated the subcellular localization of lycopene in prostate cancer cells treated with lycopene in cell culture, and determined that 81% was localized to the nucleus (55% in the nuclear membrane and 26% in the nuclear matrix). Localization of lycopene in the nucleus is consistent with the DNA protective effects exhibited by lycopene in several studies [23–25].
Antioxidant response element
In addition to direct quenching of free radicals and reactive oxygen species, lycopene can upregulate the antioxidant response element (ARE) and thereby stimulate the production of cellular enzymes such as superoxide dismutase, glutathione S-transferase and quinone reductase that protect cells from reactive oxygen species and other electrophilic molecules. For example, Ben-Dor et al. [27] reported that lycopene upregulates the ARE in HepG2 and MCF-7 cells through the Nrf2 nuclear transcription pathway. In addition, Goo et al. [28] used quantitative proteomics to show that lycopene upregulates the expression of proteins regulated by the ARE in the androgen-sensitive human prostate cell line LNCaP. These proteins included epoxide hydrolase 1 (EPHX1), superoxide dismutase-1 (SOD-1), catalase (CAT), and the metal binding protein transferrin (TF). Therefore, lycopene not only functions as an antioxidant, but it can stimulate cells to produce enzymes that help protect against reactive oxygen species and other electrophilic species that can damage DNA, lipids and proteins.
Apoptosis
A programmed sequence of events leading to the elimination of cells without damaging surrounding cells or tissues, apoptosis helps maintain health by eliminating unhealthy, excess or abnormal cells. When damaged cells fail to undergo apoptosis, they become immortal and can become cancer cells. Recently, several in vitro studies with human prostate cancer cells and cell lines derived from other tissues have indicated that lycopene can promote apoptosis in these cells and therefore might have potential as a chemotherapeutic agent.
Hantz et al. [ 29 ] reported that lycopene at 0.3–3.0 μM induced apoptosis in a concentration dependent manner in the androgen sensitive human prostate cancer cell line LNCaP. Specific indicators of apoptosis were observed in the LNCaP cells including decreased mitochondrial function, reduction of mitochondrial transmembrane potential, release of mitochondrial cytochrome c, and increased annexin V binding. Since plasma lycopene concentrations of up to 1.4 µM have been obtained through intervention [30], the range of concentrations tested by Hantz et al. included those that are physiologically relevant. In a similar study using the androgen sensitive human prostate cancer cell line LNCaP and the androgen independent cell line PC3, Ivanov et al. [31] reported that lycopene concentrations as low as 10 nM induced apoptosis in LNCaP cells. However, they found that lycopene concentrations up to 1 µM (physiologically attainable levels) had no effect on apoptosis on PC3 cells. In contrast, Kanagaraj et al. [32] reported that lycopene induced apoptosis in PC3 cells based on increases in levels of insulin-like growth factor binding protein 3 (IGFBP-3) and confirmation based on increased annexin V/propidium iodide binding. Since Kanagraraj et al. used concentrations of lycopene from 20–60 µM, which are more than an order of magnitude higher than physiologically attainable levels, this might explain the discrepancy in their results compared to those of Ivanov et al. [31].
Treatment of human colon carcinoma (HuCC) cells with lycopene at 2.0 or 4.0 µM was reported by Salman et al. [33] to induce apoptosis, but incubation with the physiologically relevant concentration of 1.0 µM lycopene was ineffective. This same group also reported that 2.0 µM lycopene induced apoptosis in Raji cells, a prototype Burkitt lymphoma cell line. No anti-apoptotic effects were observed for in B chronic lymphocytic leukemia (EHEB) cells or human erythroleukemia (K562) cells treated with lycopene at concentrations up to 4 µM. Therefore, lycopene appears to be much more effective at inducing apoptosis in human prostate cancer cells than in any of the other cell lines tested to date.
Cell cycle arrest
Cancer cells have lost the ability to regulate the cell cycle and control their rate of proliferation. A rate-limiting step in the cell cycle that is often unregulated in cancer is the progression of cells through the first gap (G1) phase [34]. Recently, there have been several reports that lycopene can induce cell cycle arrest at the G1 phase. Park et al. [25] reported that the growth of Hep3B human hepatoma cells was inhibited 20–50% by lycopene at physiologically significant concentrations as low as 0.2 µM. Specifically, lycopene was found to induce G0/G1 arrest and S phase block. In a similar study with the human prostate cancer cell lines LNCaP and PC3, Ivanov et al. [31] also found that lycopene induced mitotic arrest at the G0/G1 phase mediated by decreased levels of cyclins D1 and E and cyclin dependent kinase 4. Using human breast MCF-7 and endometrial ECC-1 cancer cells, Nahum et al. [35] showed that lycopene inhibits cell cycle progression in the G0/G1 phase through reduction of cyclin D1. Through suppression of phosphorylation of p53 and Rb anti-oncogenes, Matsushima-Nishiwaki reported that lycopene inhibited cell division of mouse hepatocytes at the G0G1 cell cycle phase [36].
In studies with the lycopene degradation product apo-10’-lycopenoic acid at concentrations from 0.5 to 10 µM, Lian et al. [37] observed that the growth of the human non-small cell lung cancer cell line A549 was arrested at the G1/S phase with decreased levels of cyclin E and increased levels of the cell cycle regulatory proteins p21 and p27. Antiproliferative effects of lycopene without details regarding the mechanism of action have also been reported for the human breast cancer cell line MCF-7 [38], rat prostate cancer AT3 cells [39], primary human prostate epithelial cells [40], the human erythroleukemia cell line K562, Raji cells, and human colon cancer HuCC cells [33].
Growth factors and signaling pathways: Platelet-derived growth factor (PDGF-BB)
PDGF functions as a mitogen for dermal fibroblast chemotaxis [41] and can stimulate tumor angiogenesis [42]. Since PDGF-BB facilitates the growth, invasion and metastasis of melanoma, inhibition of these PDGF-BB effects can be a mechanism for arresting melanoma progression. In vitro studies with the human foreskin fibroblast cell line Hs68 and the human metastatic melanoma cell line A2058 both individually and in a co-culture system indicate that lycopene can inhibit PDGF-BB induced human Hs68 skin fibroblast migration, attenuate PDGF-BB induced phosphorylation, and reduce PDGF-BB induced signaling [ 43 ]. In addition, lycopene was shown to bind to PDGF-BB in human plasma. Therefore, these in vitro studies suggest that lycopene might help control the progression of melanoma.
Cell invasion and metastasis
In studies of the highly invasive human hepatoma cell line SK-Hep-1, lycopene was shown to have antimetastatic and anti-invasion activity. Hwang and Lee [44] showed that lycopene at 5 and 10 µM (higher than physiologically relevant concentrations) could decrease the gelatinolytic activities of the matrix metalloproteinases MMP-2 and MMP-9 and inhibit the adhesion, invasion and migration of SK-Hep1 cells. At similar lycopene concentrations, Huang et al. confirmed that MMP-9 expression was suppressed in SK-Hep-1 cells [45] and found that the metastasis suppressor gene nm23-H1 was induced [46]. These studies indicate that lycopene, at least at high doses that might not be physiologically attainable, can inhibit metastasis and invasion by hepatocarcinoma cells.
3. In vitro studies of lycopene
Lycopene is an extremely hydrophobic compound, which presents an obstacle for conducting cell culture studies using lycopene. Not only is lycopene insoluble in water, but it is practically insoluble in most co-solvents which are often used to promote dissolution of test agents in cell culture media including dimethylsulfoxide [47]. The use of unusual solvents or additives to help improve the solubility of lycopene in aqueous media can by itself alter the response of the cells being studies in culture. Therefore, the variety of strategies that have been employed to promote the dispersal or dissolution of lycopene in cell culture media might be responsible, at least in part, for the wide variations in results that have been observed to date for in vitro studies of lycopene and its potential mechanisms of action (see the section on Molecular targets of lycopene).
To enhance the solubility of lycopene in cell culture media, Cooney et al. [48] used tetrahydrofuran as a co-solvent. However, tetrahydrofuran is toxic to some cell lines such as the human prostate cancer cell line LNCaP. Furthermore, lycopene is unstable in aqueous tetrahydrofuran solutions with a half-life of less than 2 h, and this length of time can be too short for cell proliferation studies [47]. As an alternative, Xu et al. [47] developed a liposomal (also called micelles in the literature) delivery system that both solubilizes and stabilizes lycopene in cell culture media. Although lycopene in liposomes was stable for at least 96 h at 37 °C in cell culture media, the liposomes were composed of compounds such as sodium taurocholate that might be toxic toward some cell lines.
Water-dispersible beadlets have become available from commercial sources to facilitate the stabilization of lycopene in solution, and these beadlets have been used to deliver lycopene to cells in culture media. Using a beadlet formulation, Liu et al. [26] found that lycopene was stable for at least 72 h at 37 °C in cell culture media. However, beadlets contain ascorbic acid and α-tocopherol, which are antioxidants that might themselves have activity as chemoprevention agents. In addition, Liu et al. reported that use of beadlets containing no lycopene showed measurable inhibition of the rate of proliferation of prostate cancer cells.
Other approaches for the delivery of lycopene to cells in culture have included using Tween 40 and Tween 80 [49] and fetal bovine serum [50]. Tween 40 and Tween 80 function as emulsifiers to facilitate the delivery lycopene to cells in culture, and lipoproteins probably function as the delivery vehicle for lycopene in the fetal bovine serum method. Although lower cytoxicities were reported for these alternatives compared to beadlets or liposomes, emulsification using Tween 40 and Tween 80 or solubilization using fetal bovine serum did not stabilize lycopene as effectively as did beadlets or liposomes.
Since lycopene is insoluble in water, steps must be taken to enhance its solubility in cell culture media or buffers before in vitro studies may be carried out. Approaches that have been implemented to deliver lycopene to cells in culture have included the use of organic solvents such as tetrahydrofuran, liposomes, emulsifiers, lipoproteins in fetal bovine serum, and water-dispersible beadlets. In addition to solubilization or emulsification, enhancing the stability of lycopene in cell culture media is an important issue, since the half-life of free lycopene in solution at 37 °C is less than 2 h. In this regard, liposomes and beadlets provide the best stabilization of lycopene. Another problem with some of these methods, especially co-solvents, beadlets and liposomes, is cytotoxicity. Until a method of solubilizing lycopene in aqueous buffers and cell culture media is developed that overcomes all of these limitations, in vitro studies of the effects of lycopene on living cells will continue to show considerable variation between laboratories and cell lines and should be interpreted with caution.
4. In vivo studies of lycopene
The first reported biological activities of lycopene in vivo were protection of mice against bacterial infection by intraperitoneally injected lycopene (Lingen et al., 1959) and protection against radiation and development of certain types of ascites tumors (Forssberg et al., 1959). Considerable time elapsed before epidemiological studies linking tomato consumption with a lower risk of prostate cancer (see the Clinical trials section) renewed interest in lycopene as a chemoprevention agent. Since then, multiple animal models including rats, mice and ferrets have been used to explore the efficacy of lycopene in the prevention of cancer in various tissues. However, no consensus has been reached concerning an ideal model for dietary lycopene or lycopene supplements.
Since the strongest clinical evidence for the benefits of lycopene in cancer are for prostate cancer chemoprevention, the majority of animal studies with lycopene have concerned prostate cancer. Tang et al. [51] evaluated the effect of lycopene on the growth rate of human DU145 prostate cancer cells in a xenograft model using BALB/c nude mice. At dosages of 100 and 300 mg/kg lycopene, the tumor growth rates were inhibited 55.6 and 75.8%, respectively. In contrast, Limpens et al. [52] used the PC-346C orthotopic mouse model of prostate cancer but found no effect on tumor volume when lycopene was administered orally at 5 or 50 mg/kg. However, tumor volume was reduced with lycopene was combined with α-tocopherol acetate. Using the MatLyLu Dunning prostate tumor model, Siler et al. [53] found that administration of 200 µg lycopene/g diet increased the necrotic area of the prostate tumors ~36%, compared to ~20% in the control groups. In addition, they found that this effect was associated with down-regulation of local androgen signaling as well as IGF-1 and IL-6 expression.
There have been relatively few animal studies regarding chemoprevention of other forms of cancer by lycopene. For example, in SHN virgin mice, Nagasawa et al. [54] reported in 1995 that a diet enriched in lycopene significantly reduced development of spontaneous mammary tumors. In 1997, Sharoni et al. [55] showed that i.p. injection of rats with a lycopene-enriched tomato oleoresin developed fewer mammary tumors after treatment with the mammary carcinogen 7,12-dimethyl-benz[a]anthracene. Using a multi-organ carcinogenesis model consisting of B6C3F1 mice treated with diethylnitrosamine, N-methyl-N-nitrosourea and 1,2-dimethylhydrazine, Kim et al. [ 56 ] found that the incidence of lung tumors was reduced significantly in male but not female mice. In addition, no reduction in tumors of colon, kidney or liver was observed. This lack of efficacy toward the prevention of liver cancer is consistent with the results of Watanabe et al. [57] who reported that dietary lycopene did not prevent liver cancer in Long-Evans Cinnamon rats, a model of spontaneous hepatocarcinogenesis.
Several in vivo studies using animal models have provided support for specific molecular targets or mechanisms of action for chemoprevention by lycopene. Using ferrets exposed to cigarette smoke, Liu et al. [58] found that lycopene supplementation reduced smoke-induced changes in cell proliferation and apoptosis in the gastric mucosa. In addition, Gitenay et al. [59] used a vitamin E deficient rat model to show that lycopene could reduce markers of oxidative stress such as thiobarbituric reactive species and increase levels of cytoprotective enzymes that help prevent oxidative stress such as superoxide dismutase.
5. Clinical trials
Epidemiological studies indicate that a tomato-rich diet is associated with lower risk of prostate cancer [60]. In a study conducted in a cohort of 14,000 Seventh Day Adventist men the consumption of tomato products was significantly associated with a lower risk of prostate cancer [61]. In addition to retrospective epidemiological studies, several prospective dietary studies have evaluated the relationship between consumption of tomatoes and the risk of prostate cancer [62]. Lycopene has been suggested to be responsible for the beneficial effect of tomatoes and tomato-based products in the prevention of prostate cancer [63]. Among 72 epidemiological studies that investigated the relationship between intake of tomato-based foods or lycopene and risk of cancer, 57 showed an inverse relationship between tomato intake or lycopene plasma levels and risks of several types of cancer [62].
As part of the Health Professionals Follow-up Study, the relationship between tomato consumption, including the measurement of lycopene plasma levels, and prostate cancer risk was investigated in more than 40,000 men [64]. High estimated lycopene intake was inversely related to risk of prostate cancer while the estimated intakes of total carotenoids, β-carotene, α-carotene, lutein, and β-cryptoxanthin were not associated with a risk of prostate cancer. The inverse correlation was stronger for more advanced or aggressive prostate cancer (relative risk 0.47) [65]. In a prospective study of the same population and analysis of all data from 1986 through 1998, lycopene intake was again determined to reduce the risk of prostate cancer [66]. In this 2002 report, Giovannucci et al. [66] indicated that the magnitude of this association was moderate and might be missed in studies of smaller populations or with substantial errors in measurement or design. In two more recent but smaller prospective epidemiological studies reported in 2006 [67] and 2007 [68], no association was detected between lycopene intake and prostate cancer risk.
Although multiple large epidemiological studies indicate that lycopene intake can lower the risk of prostate cancer, there is no consistent evidence that consumption of tomatoes or lycopene lowers the risks of other forms of cancer. For example, in other studies of the participants in the Health Professsionals Follow-up Study, no association was observed between lycopene intake and the risk of oral premalignant lesions [69] or between tomato consumption and the risk of bladder cancer [70]. In a pooled analysis of food frequency questionnaires from 11 cohort studies including more than 700,000 participants and 7,885 incident cases of colorectal cancer, tomato consumption was found to provide no reduction in the risk of colorectal cancer [71].
Compared to the epidemiological studies of tomato consumption and cancer risk, there have been few clinical trials of lycopene intervention and cancer risk that are randomized, placebo controlled and double blind. However, there have been several studies that lack one or more of these design features such as placebo control, blinding, randomization, or adequate sample size to be significant. Based on the epidemiological evidence, it is not surprising that most of the intervention studies to date have concerned prostate cancer. Usually, these intervention trials have been of relatively short duration (weeks instead of years), and as a result, the outcomes that have been measured have usually been intermediate endpoints or markers of risk such as oxidative stress instead of cancer incidence. To date, no Phase III studies of lycopene and cancer prevention have been reported. The most significant and recent of these studies will be discussed.
In 2001, Chen et al. [30] examined the effects of 30 mg lycopene per day for 3 weeks in the form of tomato sauce on 32 men with localized prostate adenocarcinoma preceding scheduled radical prostatectomy. Although this study was not blinded and not placebo controlled, serum lycopene levels increased approximately 2-fold and prostate levels of lycopene increased almost 3-fold compared to baseline. In addition, total serum levels of prostate-specific antigen (PSA) levels, which was used as a surrogate endpoint for prostate cancer progression, decreased ~20% and DNA oxidation in leukocytes (measured as 8-oxo-dG released from DNA) decreased ~21% compared to baseline. Also in 2001, Kucuk et al. [72] reported on a randomized, placebo controlled but unblinded study in which 26 men recently diagnosed with prostate cancer were administered 30 mg of lycopene or placebo daily for 21 days before radical prostatectomy. In this study, lycopene levels were not measured and no conclusions could be drawn due to the small sample size of this study.
Clark et al. [73] reported in 2006 on a dose-escalating trial of lycopene from 15 to 120 mg/day in 36 men with biochemical relapse of prostate cancer. There was no randomization or placebo group, and this study was unblinded. Lycopene levels in serum were similar after 3 month dosages of 15, 30, 45, 60, or 90 mg/day, and no change in serum PSA was detected as a result of intervention. In an unblinded, randomized intervention study of 81 men with high-grade prostatic intraepithelial neoplasia, Bunker et al. [74] administered 30 mg/day lycopene (in the form of a tomato oleoresin) plus a multivitamin or just a multivitamin for 4 months. After 1 month of intervention, total serum PSA declined, but PSA levels were identical in both groups after 4 months. In an unblinded intervention study without a control group reported in 2007, Jatoi et al. [75] evaluated 46 men with androgen-independent prostate cancer who received 30 mg lycopene/day for 16 months. Lycopene was not effective in preventing the progression of prostate cancer in this group. Although the outcomes of these intervention trials were negative, lycopene was well tolerated and no significant side effects were observed.
Clinical trials are needed to evaluate the efficacy of lycopene as a chemoprevention agent that are placebo controlled, randomized and double-blind, and several such studies are in progress. For example, van Breemen [76] is carrying out a randomized, placebo-controlled, double-blind clinical Phase II clinical trial exploring the effects of 30 mg/day lycopene for 3 weeks in 120 men with prostate cancer or benign prostate hyperplasia. In addition to lycopene levels, lipid peroxidation and DNA oxidation in blood and prostate tissue are intermediate endpoints that will be measured.
6. Bioavailability, pharmacodynamics, pharmacokinetics, and metabolism
Lycopene is tightly bound to macromolecules within the food matrix, so that its bioavailability from food is relatively poor [77]. However, cooking or processing lycopene rich foods like tomatoes can liberate lycopene from protein complexes and enhance its oral bioavailability. Since lycopene is highly lipophilic, co-consumption with lipids can also increase its bioavailability [78].
In the small intestine, lycopene is solubilized as micelles that are formed from bile salts and dietary lipids and then absorbed via passive transport [79]. Incorporated into chylomicrons, lycopene and other carotenoids are transported from the intestinal mucosa to the general circulation via the lymphatic system. In the blood, carotenoids are transported by lipoproteins. In particular, LDL is the primary carrier of lycopene [79]. In a single dose Phase I study of the pharmacokinetics of lycopene delivered in tomato paste food formulation, Gustin et al. [80] reported that the elimination half-life of lycopene ranged from 28 to 62 h depending on dosage (10 to 120 mg) and the maximum total lycopene concentration was reached in 16 to 33 h with maximum levels of 0.075 to 0.210 µM.
Even when administered as the all-trans-isomer, lycopene rapidly isomerizes during absorption to a mixture of isomers that are >50% cis-isomers in the blood stream and tissues [81]. For example, van Breemen et al. [81] reported that administration of primarily all-trans-lycopene in tomato sauce to human subjects for 3 weeks resulted in lycopene in prostate tissue that was only 22.7% all-trans-lycopene. Liver, seminal vesicles and prostate tissue are the primary sites of lycopene accumulation in vivo [82]. Furthermore, Liu et al. [26] found that lycopene can be selectively accumulated by androgen-sensitive prostate cells and localized to the nuclear membrane and nuclear matrix, suggesting a possible role for a lycopene receptor or transporter.
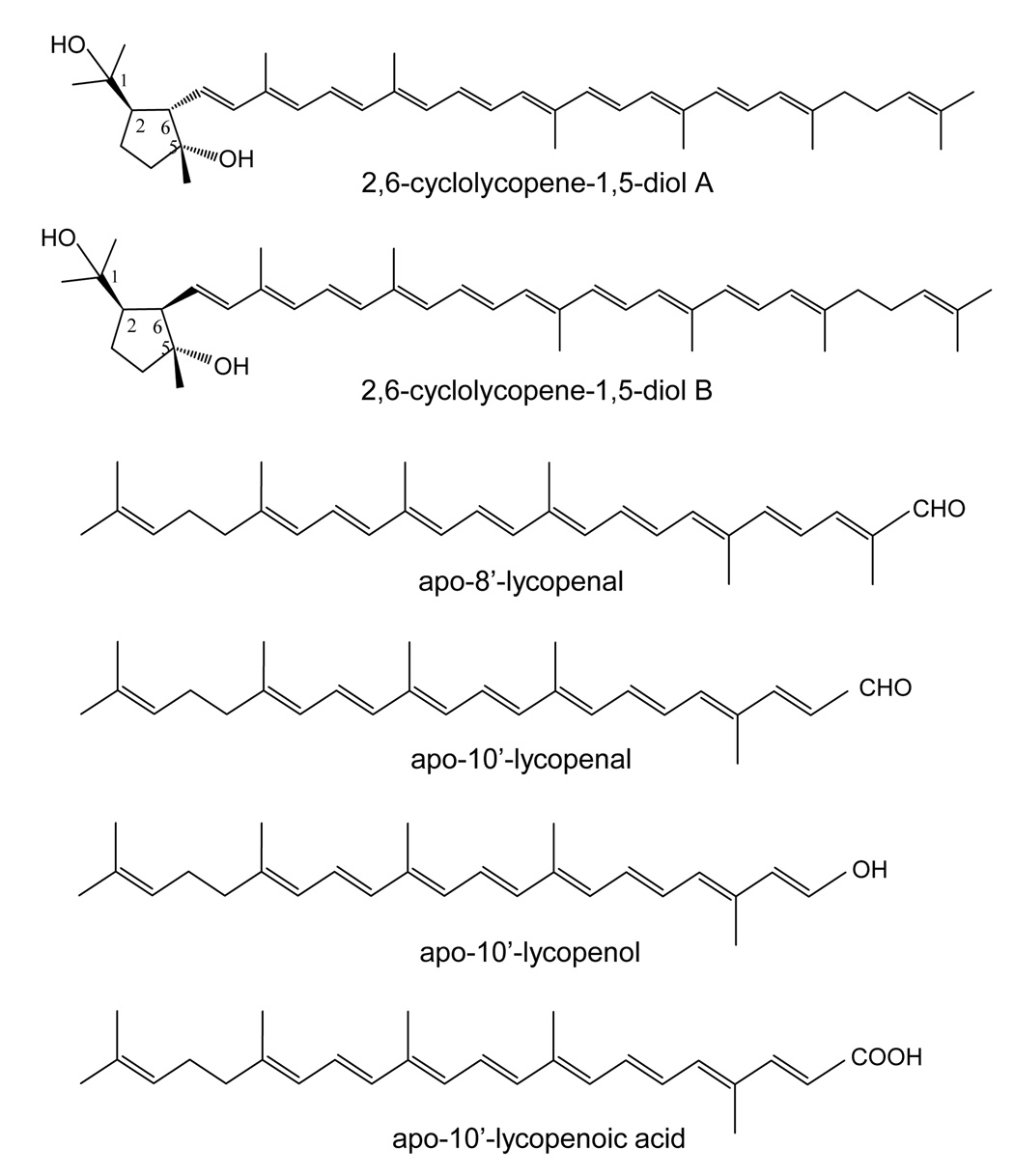
Since lycopene is unstable and easily oxidized, it can form polar multiple polar oxygenated species even without metabolic transformation. For example, Khackic et al. [83] reported detection of 2,6-cyclolycopene-1,5-diols A and B in human serum, milk and organs (see structures in Figure 2). These compounds were also detected at low levels in tomatoes. Using radiolabeled lycopene administered orally to rats, Zaripheh and Erdman [82] found that polar radioactive derivatives appeared in tissues by 3 h after dosing. Two of these derivatives were identified as apo-8’-lycopenal and apo-10’-lycopenal (Figure 2) based on spectroscopic comparison to synthetic compounds [84]. Other oxygenated derivatives were detected but could not be identified due to lack of standards.
Figure 2.
Structures of mammalian metabolites of lycopene.
Using ferret enzyme, Hu et al. [85] showed that carotene-9’,10’-monooxygenase (CMO2) can convert 5-cis- and 13-cis-lycopene but not all-trans-lycopene to apo-10’-carotenal. Furthermore, apo-10’-carotenal was shown to be oxidized by the post-nuclear fraction of hepatic homogenates from ferrets to form apo-10’-lycopenoic acid, and apo-10’-lycopenol was detected in ferret lung tissue following supplementation with all trans-lycopene. The structures of these compounds are shown in Figure 2.
7. Conclusions
Prospective epidemiological studies provide strong support for the hypothesis that the consumption of tomato products and probably lycopene reduce the risk of prostate cancer. However, there is no clear relationship between lycopene or tomato consumption and the risks of other forms or sites of cancer. The epidemiological studies indicating the inverse relationship between lycopene intake and prostate cancer risk are supported by in vitro and in vivo experiments showing that oral lycopene is bioavailable, accumulates in prostate tissue and is localized in the nucleus of prostate epithelial cells.
As the most potent quencher of singlet oxygen and free radicals among the carotenoids, antioxidant activity is at least one probable mechanism of action for lycopene, and this activity has been observed experimentally both in vitro and in vivo. In vitro experiments have also indicated other mechanisms of action, but these studies have been hindered by the insolubility of lycopene in cell culture media. Despite the use of a variety of solubilization and emulsification methods that can produce undesirable effects on cells, several mechanisms of action of lycopene have been indicated by these in vitro systems. For example, lycopene can upregulate the antioxidant response element in prostate cells and thereby induce them to synthesize enzymes that protect against electrophilic metabolites and oxidative stress. In addition, lycopene can induce apoptosis in cancer cells and inhibit their proliferation by producing cell cycle arrest. Anti-metastatic activity of lycopene has also been shown in models of prostate cancer.
Because lycopene degrades so quickly in solution, it is challenging to distinguish metabolites from degradation products. Nevertheless, lycopene has been determined to be a substrate for carotene-9’,10’-monooxygenase (CMO2) and can be converted to apo-10’-carotenal. Furthermore, apo-10’-carotenal and a few other oxygenated derivatives of lycopene have been identified in vivo following lyocopene administration to animals. Additional metabolites and lycopene degradation products with anti-cancer or chemoprevention activity will probably be identified in the next several years.
Perhaps the most important studies that are expected to be reported during the next several years will be Phase II clinical trials that are placebo-controlled, randomized and double blind. Although some Phase I and II studies have been published that establish the safety of lycopene supplementation, these studies do not address definitively the potential efficacy of lycopene as a chemoprevention agent. Well designed and adequately powered clinical studies of lycopene efficacy are still needed.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature cited
- 1.Straub O. Lists of natural carotenoids. In: Pfander H, editor. Key to carotenoids. Birkhauser Verlag: Basel; 1987. [Google Scholar]
- 2.Olson JA, Krinsky NI. Introduction: the colorful, fascinating world of the carotenoids: important physiologic modulators. FASEB J. 1995;9:1547–1550. doi: 10.1096/fasebj.9.15.8529833. [DOI] [PubMed] [Google Scholar]
- 3.Miller ES, Mackinney G, Zscheile FP., Jr Absorption spectra of alpha and beta carotenes and lycopene. Plant Physiol. 1935:375–381. doi: 10.1104/pp.10.2.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinton SK. Lycopene: chemistry, biology, and implications for human health and disease. Nutr. Rev. 1998;56:35–51. doi: 10.1111/j.1753-4887.1998.tb01691.x. [DOI] [PubMed] [Google Scholar]
- 5.Tonucci LH, Holden JM, Beecher G, Khachik F, Davis CS, Mulokozi G. Carotenoid content of thermally processed tomato-based food products. J. Agric. Food Chem. 1995;43:579–586. [Google Scholar]
- 6.Bohm V, Frohlich K, Bitsch R. Rosehip -- a "new" source of lycopene? Mol. Aspects Med. 2003;24:385–389. doi: 10.1016/s0098-2997(03)00034-7. [DOI] [PubMed] [Google Scholar]
- 7.Mangels AR, Holden JM, Beecher GR, Forman MR, Lanza E. Carotenoid content of fruits and vegetables: an evaluation of analytic data. J. Am. Diet. Assoc. 1993;93:284–296. doi: 10.1016/0002-8223(93)91553-3. [DOI] [PubMed] [Google Scholar]
- 8.Stahl W, Schwarz W, Sundquist AR, Sies H. cis-trans Isomers of lycopene and beta-carotene in human serum and tissues. Arch. Biochem. Biophys. 1992;294:173–177. doi: 10.1016/0003-9861(92)90153-n. [DOI] [PubMed] [Google Scholar]
- 9.Krinsky NI. The antioxidant and biological properties of the carotenoids. Ann. N. Y. Acad. Sci. 1998;854:443–447. doi: 10.1111/j.1749-6632.1998.tb09923.x. [DOI] [PubMed] [Google Scholar]
- 10.Fang L, Pajkovic N, Wang Y, Gu C, van Breemen RB. Quantitative analysis of lycopene isomers in human plasma using high-performance liquid chromatography-tandem mass spectrometry. Anal. Chem. 2003;75:812–817. doi: 10.1021/ac026118a. [DOI] [PubMed] [Google Scholar]
- 11.Henry LK, Pspitasari-Nienaber NL, Jaren-Galan J, van Breemen RB, Catignani GI, Schwartz SJ. Effects of ozone and oxygen on the degradation of carotenoids in an aqueous model system. J. Agric. Food. Chem. 2000;48:5008–50013. doi: 10.1021/jf000503o. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong G, Hearst J. Carotenoids 2: genetics and molecular biology of carotenoid pigment biosynthesis. FASEB J. 1966;10:228–237. doi: 10.1096/fasebj.10.2.8641556. [DOI] [PubMed] [Google Scholar]
- 13.Demmig-Adams B, Gilmore A, Adams W. Carotenoids 3: in vivo function of carotenoids in higher plants. FASEB J. 1996;10:403–412. doi: 10.1096/fasebj.10.4.8647339. [DOI] [PubMed] [Google Scholar]
- 14.Wiseman H, Halliwell B. Damage to DNA by reactive oxygen and nitrogen species: role in infammatory disease and progression to cancer. Biochem. J. 1996;313:17–29. doi: 10.1042/bj3130017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang HY, Helzlsouer KJ, Appel LJ. The effects of vitamin C and vitamin E on oxidative DNA damage: results from a randomized controlled trial. Cancer Epidemiol. Biomarkers. Prev. 2000;9:647–652. [PubMed] [Google Scholar]
- 16.Frelon S, Douki T, Favier A, Cadet J. Hydroxyl radical is not the main reactive species involved in the degradation of DNA bases by copper in the presence of hydrogen peroxide. Chem. Res. Toxicol. 2003;16:191–197. doi: 10.1021/tx025650q. [DOI] [PubMed] [Google Scholar]
- 17.Britton G. Carotenoids 1: structure and properties of carotenoids in relation to function. FASEB J. 1995;9:1551–1558. [PubMed] [Google Scholar]
- 18.Di Mascio P, Kaiser S, Sies H. Lycopene as the most efficient biological carotenoid singlet oxygen quencher. Arch. Biochem. Biophys. 1989;274:532–538. doi: 10.1016/0003-9861(89)90467-0. [DOI] [PubMed] [Google Scholar]
- 19.Krinsky NI. Mechanism of action of biological antioxidants. Proc. Soc. Exp. Biol. Med. 1992;200:248–254. doi: 10.3181/00379727-200-43429. [DOI] [PubMed] [Google Scholar]
- 20.Krinsky NI. Overview of lycopene, carotenoids, and disease prevention. Proc. Soc. Exp. Biol. Med. 1988;218:95–97. doi: 10.3181/00379727-218-44273. [DOI] [PubMed] [Google Scholar]
- 21.Ukai N, Lu Y, Etoh H. Photosensitized oxygenation of lycopene. Biosci. Biotechnol. Biochem. 1994;58:1718–1719. [Google Scholar]
- 22.Bast A, Haenen GR, van den Berg R, van den Berg H. Antioxidant effects of carotenoids. Int. J. Vitam. Nutr. Res. 1998;68:399–403. [PubMed] [Google Scholar]
- 23.Muzandu K, Ishizuka M, Sakamoto KQ, Shaban Z, El Bohi K, Kazusaka A, Fujita S. Effect of lycopene and beta-carotene on peroxynitrite-mediated cellular modifications. Toxicol. Appl. Pharmacol. 2006;215:330–340. doi: 10.1016/j.taap.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 24.Muzandu K, El Bohi K, Shaban Z, Ishizuka M, Kazusaka A, Fujika S. Lycopene and beta-carotene ameliorate catechol estrogen-mediated DNA damage. Jpn. J. Vet. Res. 2005;52:173–184. [PubMed] [Google Scholar]
- 25.Park YO, Hwang ES, Moon TW. The effect of lycopene on cell growth and oxidative DNA damage of Hep3B human hepatoma cells. Biofactors. 2005;23:129–139. doi: 10.1002/biof.5520230302. [DOI] [PubMed] [Google Scholar]
- 26.Liu A, Pajkovic N, Pang Y, Zhu D, Calamini B, Mesecar AL, van Breemen RB. Absorption and subcellular localization of lycopene in human prostate cancer cells. Mol. Cancer Ther. 2006;5:2879–2885. doi: 10.1158/1535-7163.MCT-06-0373. [DOI] [PubMed] [Google Scholar]
- 27.Ben-Dor A, Steiner M, Gheber L, Danilenko M, Dubi N, Linnewiel K, Zick A, Sharoni Y, Levy J. Carotenoids activate the antioxidant response element transcription system. Mol. Cancer Ther. 2005;4:177–186. [PubMed] [Google Scholar]
- 28.Goo YA, Li Z, Pajkovic N, Shaffer S, Taylor G, Chen J, Campbell D, Arnstein L, Goodlett DR, van Breemen RB. Systematic investigation of lycopene effects in LNCaP cells by use of novel large-scale proteomic analysis software. Proteomics Clin. Appl. 2007;1:513–523. doi: 10.1002/prca.200600511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hantz HL, Young LF, Martin KR. Physiologically attainable concentrations of lycopene induce mitochondrial apoptosis in LNCaP human prostate cancer cells. Exp. Biol. Med. (Maywood) 2005;230:171–179. doi: 10.1177/153537020523000303. [DOI] [PubMed] [Google Scholar]
- 30.Chen L, Stacewicz-Sapuntzakis M, Duncan C, Sharifi R, Ghosh L, van Breemen R, Ashton D, Bowen PE. Oxidative DNA damage in prostate cancer patients consuming tomato sauce-based entrees as a whole-food intervention. J. Natl. Cancer Inst. 2001;93:1872–1879. doi: 10.1093/jnci/93.24.1872. [DOI] [PubMed] [Google Scholar]
- 31.Ivanov NI, Cowell SP, Brown P, Rennie PS, Guns ES, Cox ME. Lycopene differentially induces quiescence and apoptosis in androgen-responsive and -independent prostate cancer cell lines. Clin. Nutr. 2007;26:252–263. doi: 10.1016/j.clnu.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Kanagaraj P, Vijayababu MR, Ravisankar B, Anbalagan J, Aruldhas MM, Arunakaran J. Effect of lycopene on insulin-like growth factor-I, IGF binding protein-3 and IGF type-1 receptor in prostate cancer cells. J. Cancer Res. Clin. Oncol. 2007;133:351–359. doi: 10.1007/s00432-006-0177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salman H, Bergman M, Djaldetti M, Bessler H. Lycopene affects proliferation and apoptosis of four malignant cell lines. Biomed. Pharmacother. 2007;61:366–369. doi: 10.1016/j.biopha.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 34.Diehl JA. Cycling to cancer with cyclin D1. Cancer Biol. Ther. 2003;1:226–231. doi: 10.4161/cbt.72. [DOI] [PubMed] [Google Scholar]
- 35.Nahum A, Zeller L, Danilenko M, Prall OW, Watts CK, Sutherland RL, Levy J, Sharoni Y. Lycopene inhibition of IGF-induced cancer cell growth depends on the level of cyclin D1. Eur. J. Cancer. 2006;45:275–282. doi: 10.1007/s00394-006-0595-x. [DOI] [PubMed] [Google Scholar]
- 36.Matsushima-Nishiwaki R, Shidoji Y, Nishiwaki S, Yamada T, Moriwaki H, Muto Y. Suppression by carotenoids of microcystin-induced morphological changes in mouse hepatocytes. Lipids. 1995;30:1029–1034. doi: 10.1007/BF02536288. [DOI] [PubMed] [Google Scholar]
- 37.Lian F, Smith DE, Russell RM, Wang XD. apo-10’-lycopenoic acid inhibits lung cancer cell growth in vitro, and suppresses lung tumorigenesis in the A/J mouse model in vivo. Carcinogenesis. 2007;28:1567–1574. doi: 10.1093/carcin/bgm076. [DOI] [PubMed] [Google Scholar]
- 38.Fornelli F, Leone A, Verdesca I, Minervini F, Zacheo G. The influence of lycopene on the proliferation of human breast cell line(MCF-7) Toxicol. In Vitro. 2007;21:217–223. doi: 10.1016/j.tiv.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 39.Gunasekera RS, Sewgobind K, Desai S, Dunn L, Black HS, McKeehan WL, Patil B. Lycopene and lutein inhibit proliferation in rat prostate carcinoma cells. Nutr. Cancer. 2007;58:171–177. doi: 10.1080/01635580701328339. [DOI] [PubMed] [Google Scholar]
- 40.Barber NJ, Zhang X, Zhu G, Pramanik R, Barber JA, Martin FL, Morris JD, Muir GH. Lycopene inhibits DNA synthesis in primary prostate epithelial cells in vitro and its administration is associated with a reduced prostate-specific antigen velocity in a phase II clinical study. Prostate Cancer Prostatic Dis. 2006;9:407–413. doi: 10.1038/sj.pcan.4500895. [DOI] [PubMed] [Google Scholar]
- 41.Heldin CH, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol. Rev. 1999;79:1283–1316. doi: 10.1152/physrev.1999.79.4.1283. [DOI] [PubMed] [Google Scholar]
- 42.Ruiter D, Bogenrieder T, Elder D, Herlyn M. Melanoma–stroma interactions: structural and functional aspects. Lancet Oncol. 2002;3:35–43. doi: 10.1016/s1470-2045(01)00620-9. [DOI] [PubMed] [Google Scholar]
- 43.Chiang HS, Wu WB, Fang JY, Chen DF, Chen BH, Huang CC, Chen YT, Hung CF. Lycopene inhibits PDGF-BB-induced signalling and migration in human dermal fibroblasts through interaction with PDF-BB. Life Sci. 2007;81:1509–1517. doi: 10.1016/j.lfs.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 44.Hwang ES, Lee HJ. Inhibitory effects of lycopene on the adhesion, invasion, and migration of SK-Hep1 human hepatoma cells. Exp. Biol. Med. (Maywood) 2006;231:322–327. doi: 10.1177/153537020623100313. [DOI] [PubMed] [Google Scholar]
- 45.Huang CS, Fan YE, Lin CY, Hu ML. Lycopene inhibits matrix metalloproteinase-9 expression and down-regulates the binding activity of nuclear factor-kappa B and stimulatory protein-1. J. Nutr. Biochem. 2007;18:449–456. doi: 10.1016/j.jnutbio.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 46.Huang CS, Shih MK, Chuang CH, Hu ML. Lycopene inhibits cell migration and invasion and upregulates nm23-h1 in a highly invasive hepatocarcinoma, SK-Hep-1 cells. J. Nutr. 2005;135:2119–2123. doi: 10.1093/jn/135.9.2119. [DOI] [PubMed] [Google Scholar]
- 47.Xu X, Wang Y, Constantinou AI, Stacewicz-Sapuntzakis M, Bowen PE, van Breemen RB. Solubilization and stabilization of carotenoids using micelles: delivery of lycopene to cells in culture. Lipids. 1999;34:1031–1036. doi: 10.1007/s11745-999-0454-9. [DOI] [PubMed] [Google Scholar]
- 48.Cooney RV, Kappock TJ, Pung A, Bertram JS. Solubilization, cellular uptake and activity of β-carotene and other carotenoids as inhibitors of neoplastic transformation in cultured cells. Methods Enzymol. 1993;214:55–68. doi: 10.1016/0076-6879(93)14053-l. [DOI] [PubMed] [Google Scholar]
- 49.O’Sullivan SM, Woods JA, O’Brien NM. Use of Tween 40 and Tween 80 to deliver a mixture of phytochemicals to human colonic adenocarcinoma cell (CaCo-2) monolayers. Br. J. Nutr. 2004;91:757–764. doi: 10.1079/BJN20041094. [DOI] [PubMed] [Google Scholar]
- 50.Lin CY, Huang CS, Hu ML. The use of fetal bovine serum as delivery vehicle to improve the uptake and stability of lycopene in cell culture studies. Br. J. Nutr. 2007;98:226–232. doi: 10.1017/S0007114507691752. [DOI] [PubMed] [Google Scholar]
- 51.Tang L, Jin T, Zeng X, Wang JS. Lycopene inhibits the growth of human androgen-independent prostate cancer cells in vitro and in BALB/c nude mice. J. Nutr. 2005;135:287–290. doi: 10.1093/jn/135.2.287. [DOI] [PubMed] [Google Scholar]
- 52.Limpens J, Schröder FH, de Ridder CM, Bolder CA, Wildhagen MF, Obermüller-Jevic UC, Krämer K, van Weerden WM. Combined lycopene and vitamin E treatment suppresses the growth of PC-346C human prostate cancer cells in nude mice. J. Nutr. 2006;136:1287–1293. doi: 10.1093/jn/136.5.1287. [DOI] [PubMed] [Google Scholar]
- 53.Siler U, Herzog A, Spitzer V, Seifert N, Denelavas A, Buchwald Hunziker P, Barella L, Huziker W, Lein M, Goralczyk R, Wertz K. Lycopene effects on rat normal prostate and prostate tumor tissue. J. Nutr. 2005;135:2050S–2052S. doi: 10.1093/jn/135.8.2050S. [DOI] [PubMed] [Google Scholar]
- 54.Nagasawa H, Mitamura T, Sakamoto S, Yamamoto K. Effects of lycopene on spontaneous mammary tumour development in SHN virgin mice. Anticancer Res. 1995;15:1173–1178. [PubMed] [Google Scholar]
- 55.Sharoni Y, Giron E, Rise M, Levy J. Effects of lycopene-enriched tomato oleoresin on 7,12-dimethyl-ben[a]anthracene-induced rat mammary tumors. Cancer Detect. Prev. 1997;21:118–123. [PubMed] [Google Scholar]
- 56.Kim DJ, Takasuka N, Kim JM, Sekine K, Ota T, Asamoto M, Murakoshi M, Nishino H, Nir Z, Tsuda H. Chemoprevention by lycopene of mouse lung neoplasia after combined initiation treatment with DEN, MNU and DMH. Cancer Lett. 1997;120:15–22. doi: 10.1016/s0304-3835(97)00281-4. [DOI] [PubMed] [Google Scholar]
- 57.Watanabe S, Kitade Y, Masaki T, Nishioka M, Satoh K, Nishino H. Effects of lycopene and Sho-saiko-to on hepatocarcinogenesis in a rat model of spontaneous liver cancer. Nutr. Cancer. 2001;39:96–101. doi: 10.1207/S15327914nc391_13. [DOI] [PubMed] [Google Scholar]
- 58.Liu C, Russell RM, Wang XD. Lycopene supplementation prevents smoke-induced changes in p53, p53phosphorylation, cell proliferation, and apoptosis in the gastric mucosa of ferrets. J. Nutr. 2006;136:106–111. doi: 10.1093/jn/136.1.106. [DOI] [PubMed] [Google Scholar]
- 59.Gitanay D, Lyan B, Rambeau M, Mazur A, Rock E. Comparison of lycopene and tomato effects on biomarkers of oxidative stress in vitamin E deficient rats. Eur. J. Nutr. 2007;46:468–475. doi: 10.1007/s00394-007-0687-2. [DOI] [PubMed] [Google Scholar]
- 60.Giovannucci E. Tomatoes, tomato-based products, lycopene, and cancer: review of the epidemiologic literature. J. Natl. Cancer Inst. 1999;99:317–331. doi: 10.1093/jnci/91.4.317. [DOI] [PubMed] [Google Scholar]
- 61.Mills PK, Beeson WL, Phillips RL, Fraser GE. Cohort study of diet, lifestyle, and prostate cancer in Adventist men. Cancer. 1989;64:598–604. doi: 10.1002/1097-0142(19890801)64:3<598::aid-cncr2820640306>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 62.Giovannucci E. A review of epidemiologic studies of tomatoes, lycopene, and prostate cancer. Exp. Biol. Med. (Maywood) 2002;227:852–859. doi: 10.1177/153537020222701003. [DOI] [PubMed] [Google Scholar]
- 63.Fleshner NE, Klotz LH. Diet, androgens, oxidative stress and prostate cancer susceptibility. Cancer Metastasis Rev. 1998;17:325–330. doi: 10.1023/a:1006118628183. [DOI] [PubMed] [Google Scholar]
- 64.Giovannucci E, Ascherio A, Rimm EB, Stampfer MJ, Colditz GA, Willett WC. Intake of carotenoids and retinol in relation to risk of prostate cancer. J. Natl. Cancer Inst. 1995;87:1767–1776. doi: 10.1093/jnci/87.23.1767. [DOI] [PubMed] [Google Scholar]
- 65.Giovannucci E, Clinton SK. Tomatoes, lycopene, and prostate cancer. Proc. Soc. Exp. Biol. Med. 1998;218:129–139. doi: 10.3181/00379727-218-44277. [DOI] [PubMed] [Google Scholar]
- 66.Giovannucci E, Rimm EB, Liu Y, Stampfer MJ, Willett WC. A prospective study of tomato products, lycopene, and prostate cancer. J. Natl. Cancer Inst. 2002;94:391–398. doi: 10.1093/jnci/94.5.391. [DOI] [PubMed] [Google Scholar]
- 67.Kirsh VA, Mayne ST, Peters U, Chatterjee N, Leitzmann MF, Dixon LB, Urban DA, Crawford ED, Hayes RB. A prospective study of lycopene and tomato product intake and risk of prostate cancer. Cancer Epidemiol. Biomarkers Prev. 2006;15:92–98. doi: 10.1158/1055-9965.EPI-05-0563. [DOI] [PubMed] [Google Scholar]
- 68.Peters U, Leitzmann MF, Chatterjee N, Wang Y, Albanes D, Gelmann EP, Friesen MD, Riboli E, Hayes RB. Serum lycopene, other carotenoids, and prostate cancer risk: a nested case-control study in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiol. Biomarkers Prev. 2007;16:962–968. doi: 10.1158/1055-9965.EPI-06-0861. [DOI] [PubMed] [Google Scholar]
- 69.Maserejian NN, Giovannucci E, Rosner B, Joshipura K. Prospective study of vitamins C, E, and A and carotenoids and risk of oral premalignant lesions in men. Int. J. Cancer. 2007;120:970–977. doi: 10.1002/ijc.22448. [DOI] [PubMed] [Google Scholar]
- 70.Michaud DS, Spiegelman D, Clinton SK, Rimm EB, Willett WC, Giovannucci EL. Fruit and vegetable intake and incidence of bladder cancer in a male prospective cohort. J. Natl. Cancer Inst. 1999;91:605–613. doi: 10.1093/jnci/91.7.605. [DOI] [PubMed] [Google Scholar]
- 71.Männistö S, Yuan SS, Hunter DJ, Spiegelman D, Adami HO, Albanes D, van den Brandt PA, Buring JE, Cerhan JR, Colditz GA, Freudenheim JL, Fuchs CS, Giovannucci E, Goldbohm RA, Harnack L, Leitzmann M, McCullough ML, Miller AB, Rohan TE, Schatzkin A, Virtamo J, Willett WC, Wolk A, Zhang SM, Smith-Warner SA. Dietary carotenoids and risk of colorectal cancer in a pooled analysis of 11 cohort studies. Am. J. Epidemiol. 2007;165:246–255. doi: 10.1093/aje/kwk009. [DOI] [PubMed] [Google Scholar]
- 72.Kucuk O, Sarkar FH, Sakr W, Djuric Z, Pollak MN, Khachik F, Li YW, Banerjee M, Grignon D, Bertram JS, Crissman JD, Pontes EJ, Wood DP., Jr Cancer Epidemiol. Biomarkers Prev. 2001;10:861–868. [PubMed] [Google Scholar]
- 73.Clark PE, Hall MC, Borden LS, Jr, Miller AA, Hu JJ, Lee WR, Stindt D, D’Agostino R, Jr, Lovato J, Harmon M, Torti FM. Phase I–II prospective dose-escalating trial of lycopene in patients with biochemical relapse of prostate cancer after definitive local therapy. Urology. 2006;67:1257–1261. doi: 10.1016/j.urology.2005.12.035. [DOI] [PubMed] [Google Scholar]
- 74.Bunker CH, McDonald AC, Evans RW, de la Rosa N, Boumosleh JM, Patrick AL. A randomized trial of lycopene supplementation in Tobago men with high prostate cancer risk. Nutr. Cancer. 2007;57:130–137. doi: 10.1080/01635580701274046. [DOI] [PubMed] [Google Scholar]
- 75.Jatoi A, Burch P, Hillman D, Vanyo JM, Dakhil S, Nikcevich D, Rowland K, Morton R, Flynn PJ, Young C, Tan W. North Central Cancer Treatment Group, A tomato-based, lycopene-containing intervention for androgen-independent prostate cancer: results of a Phase II study from the North Central Cancer Treatment Group. Urology. 2007;69:289–294. doi: 10.1016/j.urology.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 76.van Breemen RB. How do intermediate endpoint markers respond to lycopene in men with prostate cancer or benign prostate hyperplasia? J. Nutr. 2005;135:2062S–2064S. doi: 10.1093/jn/135.8.2062S. [DOI] [PubMed] [Google Scholar]
- 77.Erdman JW, Jr, Bierer TL, Gugger ET. Absorption and transport of carotenoids. In: Olson JA, editor. Carotenoids in human health. New York: New York Academy of Sciences; 1993. pp. 76–85. [DOI] [PubMed] [Google Scholar]
- 78.Stahl W, Sies H. Uptake of lycopene and its geometrical isomers is greater from heat-processed than from unprocessed tomato juice in humans. J. Nutr. 1992;122:2161–2166. doi: 10.1093/jn/122.11.2161. [DOI] [PubMed] [Google Scholar]
- 79.Parker RS. Absorption, transport and metabolism of carotenoids. FASEB J. 1996;10:542–5451. [PubMed] [Google Scholar]
- 80.Gustin DM, Rodvold KA, Sosman JA, Diwadkar-Navsariwala V, Stacewicz-Sapuntzakis M, Viana M, Crowell JA, Murray J, Tiller P, Bowen PE. Single-dose pharmacokinetic study of lycopene delivered in a well-defined food-based lycopene delivery system (tomato paste-oil mixture) in healthy adult male subjects. Cancer Epidemiol. Biomarkers Prev. 2004;13:850–860. [PubMed] [Google Scholar]
- 81.van Breemen RB, Xu X, Viana MA, Chen L, Stacewicz-Sapuntzakis M, Duncan C, Bowen PE, Sharifi R. Liquid chromatography-mass spectrometry of cis- and all-trans-lycopene in human serum and prostate tissue after dietary supplementation with tomato sauce. J. Agric. Food Chem. 2002;50:2214–2219. doi: 10.1021/jf0110351. [DOI] [PubMed] [Google Scholar]
- 82.Zaripheh S, Erdman JW., Jr The biodistribution of a single oral dose of [14C]-lycopene in rats prefed either a control or lycopene-rich diet. J. Nutr. 2005;135:2212–2218. doi: 10.1093/jn/135.9.2212. [DOI] [PubMed] [Google Scholar]
- 83.Khachik F, Carvalho L, Bernstein PS, Muir GJ, Zhao DY, Katz NB. Chemisitry, distribution, and metabolism of tomato carotenoids and their impact on human health. Exp. Biol. Med. (Maywood) 2002;227:845–851. doi: 10.1177/153537020222701002. [DOI] [PubMed] [Google Scholar]
- 84.Gajic M, Zaripheh S, Sun F, Erdman JW., Jr Apo-8’-lycopenal and apo-12’-lycopenal are metabolic products of lycopene in rat liver. J. Nutr. 2006;136:1552–1557. doi: 10.1093/jn/136.6.1552. [DOI] [PubMed] [Google Scholar]
- 85.Hu KQ, Liu C, Hansgeorg E, Krinsky NI, Russell RM, Wang XD. The biochemical characterization of ferret carotene-9’-10’-monooxygenase catalyzing cleavage of carotenoids in vitro and in vivo. J. Biol. Chem. 2006;281:19327–19338. doi: 10.1074/jbc.M512095200. [DOI] [PMC free article] [PubMed] [Google Scholar]