Abstract
Rationale: Many physicians are reluctant to discuss a patient's prognosis when there is significant prognostic uncertainty.
Objectives: We sought to understand surrogate decision makers' views regarding whether physicians should discuss prognosis in the face of uncertainty.
Methods: We conducted semi-structured interviews with 179 surrogates for 142 incapacitated patients at high risk of death in four intensive care units at an academic medical center. The interviews explored surrogates' attitudes about whether physicians should discuss prognosis when they cannot be certain their prognostic estimates are correct. We used constant comparative methods to analyze the transcripts. Validation methods included triangulation by multidisciplinary analysis and member checking.
Measurements and Main Results: Eighty-seven percent (155/179) of surrogates wanted physicians to discuss an uncertain prognosis. We identified five main reasons for this, including surrogates' belief that prognostic uncertainty is unavoidable, that physicians are their only source for prognostic information, and that discussing prognostic uncertainty leaves room for realistic hope, increases surrogates' trust in the physician, and signals a need to prepare for possible bereavement. Twelve percent (22/179) of surrogates felt that discussions about an uncertain prognosis should be avoided. The main explanation was that it is not worth the potential emotional distress if the prognostications are incorrect. Surrogates suggested that physicians should explicitly discuss uncertainty when prognosticating.
Conclusions: The majority of surrogates of patients that are critically ill want physicians to disclose their prognostic estimates even if they cannot be certain they are correct. This stems from surrogates' belief that prognostic uncertainty is simultaneously unavoidable and acceptable.
Keywords: surrogate decision making, ethics, critical care, prognostication
AT A GLANCE COMMENTARY
Scientific Knowledge on the Subject
Prognostic uncertainty is inherent in caring for many critically ill patients. Previous research suggests that physicians are reluctant to prognosticate in the face of uncertainty, but little is known about surrogates' views on this topic.
What This Study Adds to the Field
Most surrogates see prognostic uncertainty as unavoidable and acceptable and desire a discussion of uncertain prognoses. These insights may contribute to the goal of improving physician–surrogate communication.
Prognostic uncertainty is an uncomfortable reality in the care of many patients with life-threatening diseases (1). Critically ill patients often present with multiple acute problems that evolve quickly. Other patients have multiple comorbidities, making disease-specific prognostications fraught with difficulty. Some patients have diseases for which few valid outcome data exist. In the face of an uncertain prognosis, many physicians believe that discussions about prognosis should be avoided (2). Previous work by our group revealed that physicians frequently avoid discussing important aspects of prognosis with surrogate decision makers in intensive care units (3). However, the ethical justification for providing prognostic information is well established: it allows decisions to be informed by the likely outcomes of treatment (4).
Little is known about the perspective of patients or their surrogates on prognostic uncertainty. Studies of patients' perspectives on uncertainty in general reveal that individuals vary in how they react to it. Some view uncertainty as a source of hope, whereas others view it as anxiety-provoking (5–7). In the critical care setting, several investigators have reported that surrogates want complete and honest communication about their loved one's prognosis (8–10). However, these studies did not address the fact that most prognostication in critical illness is shrouded in uncertainty and is based on the physician's expert judgment rather than validated prediction rules. To our knowledge, no investigation has addressed surrogates' views on whether the inherent uncertainty in prognosis changes their desire for this information. Furthermore, although there is a body of literature on uncertainty and the physician–patient relationship (7, 11, 12), little is known about uncertainty and the physician–surrogate relationship.
These gaps in knowledge limit our ability to develop evidence-based interventions to improve surrogate decision making for incapacitated patients. We therefore conducted this study to determine the perspectives of surrogates about whether and how physicians should discuss prognosis in the face of uncertainty.
METHODS
Study Design, Participants, and Setting
Between January 2006 and October 2007 we conducted face-to-face, semi-structured interviews with surrogate decision makers in a prospectively defined cohort of critically ill patients at high risk of death in four intensive care units (ICUs) at the University of California, San Francisco Medical Center. The ICUs included two medical-surgical ICUs, a neurological ICU, and a cardiac ICU. Inclusion criteria for patients included (1) greater than 18 years of age, (2) respiratory failure requiring mechanical ventilation, (3) lack of decision-making capacity and (4) an APACHE II score of 25 or greater (predicting in-hospital mortality of at least 40%). Patients who died within 48 hours of receiving mechanical ventilation were not eligible due to Internal Review Board requirements. All interviews took place between Days 3 and 5 of the patients' mechanical ventilation.
Eligible subjects for this study were at least 18 years of age, spoke English well enough not to require the use of an interpreter, and self-identified as a surrogate decision maker for the patient. If the responsibility for surrogate decision making was shared between family members, we enrolled those who self-reported having the most responsibility for decision making. Thus more than one subject per patient could be enrolled. Study investigators identified eligible surrogates by screening daily in each ICU. Before approaching potential subjects, we obtained permission from the patient's attending physician to do so. All subjects provided written consent to participate in the study. The Institutional Review Board at UCSF approved all study procedures.
Surrogates who agreed to participate completed a demographic questionnaire and participated in a 30-minute, one-on-one, semi-structured interview that was audiotaped and then transcribed. The interview focused on surrogates' attitudes about discussing prognosis in ICUs. The current report focuses on their responses to the following prompt and question: “Sometimes doctors are hesitant to talk about a patient's prognosis because they fear they might be wrong. They're concerned that the family will be upset with them if their predictions turn out to be wrong. Should doctors discuss prognosis when they cannot be certain their estimates are correct?” The interviewer followed up participant's responses, pursued themes as they arose, and sought clarification or elaboration. All interviews were conducted by one interviewer who was trained in techniques of cognitive interviewing. As part of the iterative approach to data collection that is central to qualitative research, the content of the semi-structured interview was expanded over time to pursue and clarify themes that emerged in earlier interviews (13–15).
Qualitative Data Coding
The audiotaped interviews were transcribed verbatim by a medical transcriptionist. We used constant comparative methods to inductively develop a framework to describe participants' attitudes about discussing prognosis in the face of prognostic uncertainty. Constant comparative methods are a general methodology for inductively analyzing systematically gathered qualitative data. The method is most useful when existing conceptual frameworks for the topics under study are inadequate (13–15).
To develop the preliminary coding scheme, four investigators independently coded a subset of transcripts line-by-line. We identified recurrent themes relating to surrogates' attitudes about disclosure of prognostic information in the face of uncertainty. As themes and concepts accumulated, we refined distinctions between concepts and then grouped similar concepts into conceptual categories. These categories were developed further by comparing across transcripts. All investigators collaborated on developing the preliminary framework and, through a series of investigator meetings, arrived at consensus on the final coding framework. We modified the framework iteratively over the study period as interviews yielded new insights.
Reliability of the Coding
Using the final coding framework, two investigators independently coded all 179 interviews by listening to the audiotapes and reading the transcripts. Both coders were blinded to the demographic characteristics of the subjects and to one another's coding. To assess intercoder reliability, we calculated a kappa statistic on a random sample of 20% of interviews, excluding any interviews that were used in development of the coding framework. The average kappa statistic for identifying individual themes within an interview was 0.86 (range, 0.71–1.00). A kappa value greater than 0.8 represents excellent interrater reliability (16). All discrepancies between coders were reviewed and resolved through dialogue between the coders and the senior author.
Validity of the Findings
We used two techniques to ensure the validity of our findings (17, 18). First, we used a multidisciplinary approach in developing the coding framework. Areas of investigator expertise included critical care medicine, bioethics, sociology, general internal medicine, doctor–patient communication, and end-of-life care. A multidisciplinary approach reduces the chance that individual bias threatens the validity of the findings. Second, we presented the preliminary conceptual framework to a sample of study subjects for confirmation and/or modification, a process known as member checking (18). There was strong support for the framework among participants. No new themes were raised during the process of member checking.
RESULTS
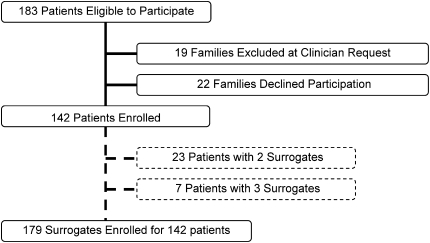
Among 183 eligible patients, the families of 19 (10%) were not approached at the request of the attending physician, and 22 (12%) families declined to participate after learning about the study (Figure 1). The overall enrollment rate was 78% (142/183). In some cases the family indicated that more than one individual would be involved in surrogate decision making and therefore, for 23 patients, 2 surrogates were enrolled and for 7 patients, 3 surrogates were enrolled. The mean number of surrogates interviewed per family was 1.3. Restricting the analyses to one surrogate per patient did not significantly change the findings; therefore, we present the data from all surrogates.
Figure 1.
Flow diagram describing the enrollment of patients and surrogates.
The demographic characteristics of the surrogate decision makers and patients who participated in the study are shown in Table 1. The sample was diverse in terms of gender, race, ethnicity, religious affiliation, and level of education. At the time of enrollment, the patients had a mean acute physiology and chronic health evaluation II (APACHE II) score of 30 ± 4. Their in-hospital mortality rate was 45% (64/142). Of the 179 surrogates interviewed, 142 (79%) reported having spoken to a doctor about their loved one's prognosis at some point before the interview.
TABLE 1.
DEMOGRAPHIC CHARACTERISTICS OF PATIENTS AND SURROGATE DECISION MAKERS
| Characteristics of Patients and Families | N (%) |
|---|---|
| Patients | 142 |
| Male | 78 (55) |
| Race/ethnicity* | |
| White | 83 (58) |
| Asian/Pacific Islander | 30 (21) |
| Hispanic | 17 (12) |
| African American | 14 (10) |
| Native American | 2 (1) |
| Other/multiethnic/undocumented | 3 (2) |
| Admission diagnosis | |
| Neurological failure | 40 (28) |
| Respiratory failure | 38 (27) |
| Cardiac failure/shock (includes sepsis) | 34 (24) |
| Gastrointestinal failure (includes pancreatitis) | 11 (8) |
| Hepatic failure | 11 (8) |
| Metastatic cancer | 5 (4) |
| Renal failure | 3 (2) |
| Mortality | 64 (45) |
| APACHE II Score† | 30 (4) |
| Family members | 179 |
| Female | 125 (70) |
| Race/ethnicity* | |
| White | 109 (61) |
| Asian/Pacific Islander | 28 (16) |
| Hispanic | 26 (15) |
| African American | 19 (11) |
| Other/multiethnic/undocumented | 12 (7) |
| Native American | 2 (1) |
| Relationship to patient | |
| Child | 66 (37) |
| Spouse/Partner | 39 (22) |
| Other | 31 (17) |
| Sibling | 23 (13) |
| Parent | 18 (10) |
| Friend | 2 (1) |
| Level of education | |
| Some college or trade school | 58 (32) |
| Some high school (including diploma or GED) | 48 (27) |
| Graduate or professional school | 38 (21) |
| 4-yr college degree | 35 (20) |
| 8th grade or less | 0 (0) |
| Primary language | |
| English | 145 (81) |
| Spanish | 13 (7) |
| Other‡ | 10 (6) |
| Tagalog | 6 (3) |
| Cantonese | 5 (3) |
| Religious preference | |
| Catholic | 57 (32) |
| None/agnostic/atheist | 38 (21) |
| Protestant | 37 (21) |
| Other Christian (LDS/Mormons, JW) | 22 (12) |
| No response | 12 (7) |
| Jewish | 5 (3) |
| Other (including Spiritualist) | 5 (3) |
| Hindu | 1 (0.5) |
| Buddhist | 1 (0.5) |
| Muslim | 1 (0.5) |
| Importance of religion/spiritual beliefs in everyday life | |
| Very important | 86 (48) |
| Fairly important | 38 (21) |
| Not too important | 30 (17) |
| Declined response | 13 (7) |
| Not at all important | 12 (7) |
| Self-reported discussion of prognosis with doctor prior to interview | |
| Yes | 142 (79) |
Definition of abbreviation: APACHE = Acute Physiology, and Chronic Health Evaluation.
Sums are greater than n = 142 or n = 179 because some individuals identified with more than one race/ethnicity.
APACHE score is expressed as mean (SD).
Includes Vietnamese, Mandarin, Korean, Russian, Italian, Farsi, Greek, and Unspecified.
Overall, 87% (155/179) of surrogates wanted physicians to discuss prognosis even in the face of uncertainty; 12% (22/179) felt physicians should avoid discussing an uncertain prognosis. Two (1%) surrogates were unsure whether doctors should discuss an uncertain prognosis.
We identified five main reasons surrogates wanted physicians to discuss prognosis in the face of uncertainty, including surrogates' beliefs that prognostic uncertainty is unavoidable, that physicians are the best and only source for prognostic information, and that discussing prognostic uncertainty leaves room for realistic hope, increases surrogates' trust in the physician, allows surrogates time to prepare to make difficult life support decisions, and to prepare for possible bereavement. Table 2 contains additional examples of the themes discussed.
TABLE 2.
FAMILIES' REASONS TO DISCUSS PROGNOSIS IN THE FACE OF UNCERTAINTY
| Reasons to Discuss Uncertain Prognosis |
|---|
| Theme |
| Examples |
| Prognostic Uncertainty Is Unavoidable, but Acceptable |
| Uncertainty is inevitable |
| “Well, I think everybody always goes with the premise that nothing is set in stone. Like, you know, the way things are, you never know, so that's why … like I always think the doctor should give prognosis … what they think. But, what he thinks and what actually happens could always be totally different.” |
| “Well, he can't … he can't know … he can't predict the future. He can have a very good idea of what's gonna happen, but he doesn't know, one-hundred percent, until it happens.” |
| Doctors are a valuable source of prognostic information |
| “I think that the doctors are far more educated and professional than the average lay person. And it's like having an inside track on a horse race. If you know that the winning odds are such'n'such, then you're more apt to bet heavily on that particular horse.” |
| “As a patient, I think it is not very responsible if the doctor is unwilling to give prognosis, because there's no way the family know.” |
| The Value of Even Uncertain Prognostic Information |
| Prognostic information allows families to prepare for possible bereavement |
| “But I do think that, you know, I would want a prognosis. I feel like I would want to know what's going on. ‘Cause it also helps you prepare, too. If the prognosis is good, or bad, it helps you prepare, either way, mentally. And … you have to be, I guess, tough, you know, for any kind of situation like this.” |
| “Just because it's warning …The way I see it, it's warning you for what could happen. And even though they're not sure, they should mention it to the family. You know [by saying] ‘We think …’ they're not assuring that that's exactly what's gonna happen, but they are just letting the family know what could happen.” |
| Prognostic estimates allow families to make decisions |
| “At least give them what may have led them to this and the possible diversions that may lead to a different prognosis, I think, would … give me the knowledge that I would need to make any decisions, a ‘know where they're at’ type of a thing.” |
| Families can hope for the best, prepare for the worst |
| “You plan for the worst and pray for the best, because if you're ready for the worst, anything other than the worst is ‘Yea!’” |
| Sharing information fosters trust in doctors |
| “I would assume, if the doctor's not sure, then he would tell me that. And tell me that, you know, ‘This is what we're looking toward. This is the direction we're going. And … and we don't know for sure.’ I would respect that much more.” |
| “If they could admit that they could be wrong … because not everything is known in the medical field … And not everybody's perfect [chuckle] … I would trust ‘em more.” |
Prognostic Uncertainty Is Unavoidable, but Acceptable
Uncertainty is inevitable.
Many surrogates' first and strongest statements addressed their belief that uncertainty is inevitable when trying to predict an individual patient's outcome. Some believed that the complexity of the human body and the unique personal qualities of each patient cannot be fully understood even by well-trained physicians, making it difficult to predict who would survive. For others, the changeable nature of a critically ill patient's condition made accurate prediction hard. Others felt that any given patient's outcome is “up to God” and that physicians could not know this with certainty. The comments of a 29-year-old woman were typical: “Well, clearly, the doctors do not have 100% vision of what's gonna happen in the future, a hundred percent accurate. It's impossible.” Surrogates felt that attempts by physicians to convey certainty about prognosis was problematic because doctors “do not have a crystal ball.”
Doctors are a valuable source of prognostic information.
Nonetheless, surrogates welcomed physicians' prognostic estimates. Many surrogates said they would not “blame” or “hold responsible” a doctor whose prognostic estimate proved incorrect. One said, “We're not gonna take ‘em to court because they made a prognosis and it turned out not to be true.” Several framed their comments about acceptance of uncertainty in terms of the humanness or “fallibility” of doctors. The surrogate of a patient with respiratory failure said: “I don't think I would be upset, as far as their predictions, because, you know, they are also human and they are making their predictions based on the best medical knowledge they have.”
According to surrogates, the combination of the uncertainty of critical illness and their own lack of medical knowledge made physicians' expertise very valuable. These surrogates saw the prognostications of doctors as “educated” or “expert” estimates. One stated: “They know more than I know about it. So, I'd appreciate hearing their best guess.” For some, information gathering and “knowing” was part of how they dealt with having a loved one in the ICU, and in this way, a doctor's estimate could ease the anxiety of uncertainty. One stated that, “the more information I know, the better it is for me to cope.”
A few surrogates mentioned that families would be left “wondering” or “guessing” without prognostic information from doctors. As this 49-year-old surrogate points out, doctors are often the only source of prognostic information families have: “If they don't say it, if they don't say what the prognosis are [sic], even though it's wrong, I always think, you know, who else are the loved ones gonna go to, to get the answers?”
In general terms, certainty was not what surrogates expected from a doctor. The more important goal was communication of the physicians' best prognostic estimate. As this surrogate stated, “I want to have a discussion with the doctor about what the prognosis is, and I don't expect him to know for sure.” Overall, these comments revealed the belief among many surrogates that physicians and surrogates must work together within the “reality” of prognostic uncertainty.
The Value of Even Uncertain Prognostic Information
Preparing for possible bereavement.
Many surrogates felt that, although imperfect, physicians' prognostic estimates would provide them a “rough ballpark” or a “warning … for what could happen.” Prognostications allowed surrogates to begin the emotional work of preparing for a potentially bad outcome. The surrogate of a patient with endocarditis and multiorgan system failure said: “I'd rather have them tell me that she's maybe really not gonna make it … I think I would be more prepared, if they had told me that she wouldn't.” Several surrogates felt that by mentioning both the positive and negative sides of uncertainty, doctors could help families balance hope and realism: “In one way we are prepared for the worst and another way, we have some good hopes.”
Making decisions.
Surrogates spoke about the need for prognostic information to carry out their role as surrogate decision maker. Importantly, many expressed a willingness to “make the best decision, based on the information that you have.” The timeliness of the information was important; some surrogates referred directly to a need for early discussion about prognosis “so that everybody can start making some kind of plan.” Another pointed out that “the more warning … the more time … to prepare a course of action that's well thought through.” Another surrogate worried that without prognostic information to base a decision on, her mother might be left to linger longer, something she wanted to avoid.
Sharing information fosters trust in doctors.
Although skepticism about prognostic certainty was common, surrogates felt that acknowledgment of uncertainty would indicate honesty on the part of the physician rather than being a source of confusion or anxiety. Some indicated that they would trust a doctor who was willing to admit uncertainty more than they might otherwise: “If he was to be honest and say he could be wrong, yeah, that makes me feel more, ‘Ok, you're givin' us your honest opinion. I trust … I trust you more, now.’”
Families Who Did Not Want to Discuss an Uncertain Prognosis
Twelve percent (22/179) of surrogates felt that discussions about an uncertain prognosis should be avoided. Twelve were concerned that uncertain estimates had the potential of being unnecessarily upsetting to the family. Five surrogates who initially indicated they would not want uncertain prognostic information suggested a desire to be told of the prognosis at a certain point or in a certain way. For example, one said, “If they're not sure, I think they should wait until they're more sure—even if it has to be on a day-to-day basis.”
Practical Suggestions from Surrogates
Although we did not specifically inquire about how physicians should discuss an uncertain prognosis, many surrogates volunteered suggestions (Table 3). Most suggestions centered on ways to make uncertainty an integral part of the conversation about prognosis. Some surrogates wanted physicians to simply avoid making absolute predictions about a given outcome: “If a doctor says, ‘I am absolutely 100% certain that this is going to end one way,’ I might be inclined to say, ‘Don't you think that's a little strong?’” Surrogates suggested doctors could use explicit statements about prognostic uncertainty, such as using phrases like, “There are chances…” “My experience is…” or, “Most often, I see this…” The important thing, according to a 56-year-old woman is to “make it clear that you can't be a hundred percent.”
TABLE 3.
SUGGESTIONS FROM SURROGATE DECISION MAKERS ABOUT HOW TO TALK ABOUT AN UNCERTAIN PROGNOSIS
| Use language that conveys uncertainty | “Uhm, example would be uhm, ‘No one can predict, with 100% certainty, what the outcome's gonna be.’ And ‘I have some experience with it, but I'm not gonna tell that I know what's going to happen, but here's what I think is going to happen.’ And that might be an example.” |
| “That's basically you just … you're giving the information, but you're letting … you're letting them know, ‘Hey, this is information, as I see it right now. And further down the line, it can change.’” | |
| “I think that also, if they're not sure that it's correct, that there should be some kind of, ‘This is what we think it is. We're not entirely sure …’” | |
| Avoid absolutes | “Where doctors get themselves in trouble is, you know, ‘I see x, y, and z. And this is what's gonna happen,’ you know.” |
| “A doctor doesn't absolutely go, ‘This person's gonna die.’ Right? That doesn't do anybody any good, probably. Right? … So better to hear, ‘We're gonna give … odds are very poor. Odds are not in the patient's favor, but we're gonna give it every shot we got,’ would be much better to hear.” | |
| Use percentages or ranges | “I think that, when they give a prognosis, it should be based on statistics and fact. I think they should be able to say, ‘Out of the 80 cases of this that I've studied, 35 people survived out of the 80.’” |
| “What they need is to come across as, you know, ‘I have the best information available, based on what we've seen in the past, this is what has happened. Twenty percent go this way, eighty percent go this way.’” | |
| “We always can't, you know, pinpoint a prognosis, you know, on something. I think he should lay out the scenarios, you know what I'm sayin'? | |
| Err on the side of ‘complete honesty’ | “Don't—don't—don't just drag us along saying there's hope and then it does go bad and then you're like well you know, ‘I should have mentioned that it could have gone bad.’” |
| “I would assume, if the doctor's not sure that he would tell me that. And tell me that, you know, ‘This is what we're looking toward. This is the direction we're going. And this … and we don't know for sure.’ I would respect that much more. I want to be treated as an intelligent adult, not as a child. That's bottom line.” |
When faced with prognostic uncertainty, many surrogates felt it was important to err on the side of “complete honesty.” Surrogates felt doctors “shouldn't hold anything back,” because as one put it, “it's better to over-communicate it rather than under-communicate it.” In explaining his desire for complete disclosure, another surrogate mentioned a past experience with the hospitalization and death of a loved one: “I just had my mother pass away a couple years ago, so the doctors were pretty straight with us. And I liked it. I know it was rough for us, because you know, it was our mom, but … we wanted to hear the truth. And we wanted to hear, you know, everything.”
DISCUSSION
We found that most—but not all—surrogates of critically ill patients want physicians to disclose their prognostic estimates even if they cannot be sure they are correct. Families perceive uncertainty as an unavoidable reality when prognosticating for critically ill patients. Most surrogates accept this uncertainty, want physicians to openly acknowledge it, and are willing to work within it in their role as surrogate decision makers.
Physicians are profoundly affected by prognostic uncertainty. In a survey of internists, 80% believed that physicians should avoid discussing prognosis when the prognosis is uncertain (2). The SUPPORT (Study to Understand Prognoses and Preferences for Outcomes and Risk of Treatments) trial, a randomized controlled trial to improve end of life care for seriously ill hospitalized patients by providing computer derived prognostic estimates to physicians, revealed that less than 20% of physicians discussed this prognostic information with patients or their surrogates (19). One explanation for this is that physicians may have been uncomfortable discussing prognostic information that was probabilistic and that did not provide definitive information for the individual patient (20, 21). We speculate that these conversations may also be difficult for physicians because they involve acknowledging the limits of medical knowledge.
Our data suggest that physicians' inclination to avoid discussing an uncertain prognosis will not meet the needs of most surrogates. Most surrogates in our study believed that uncertainty is an unavoidable reality of life-threatening illness. Rather than desiring less information in the face of uncertainty, most surrogates want more information, including clear communication about uncertainty itself. The act of discussing uncertainty was viewed by some surrogates as a sign that the physician was trustworthy. Prognostications that were expressed as certainties were viewed skeptically. Eggenberger, in her study of family experiences in ICUs, described the uncertainty families dealt with as “enduring” and “unrelenting” (22). She wrote, “They were forced to endure unknown outcomes of treatment, vacillating symptoms, doubts about healthcare decisions, and other unexpected events” (23). Our results suggest that most surrogates see physicians' prognostic estimates as valuable information that helps to reduce this sense of pervasive uncertainty. This interpretation fits with prior empirical work from the outpatient setting that revealed that patients preferred certainty when making difficult medical decisions, but that when certainty is not possible, approaches to decision making that ignore uncertainty are viewed negatively (11).
Another reason that doctors withhold prognostic information, especially when the prognosis is poor, is to avoid causing patients or families undue distress (12, 24, 25). Our results suggest that this approach may be misguided. Specifically, some surrogates reported that early, open discussions about prognosis may allow families to begin to prepare for the possibility that the patient may die. There is a growing body of evidence that lack of preparation for bereavement is a risk factor for adverse psychological outcomes such as depression and complicated grief (26, 27). Taken together, these observations raise the possibility that an intervention involving early disclosure about prognosis could improve bereavement outcomes for families.
However, the observation that 12% of surrogates in this study did not want doctors to discuss uncertain prognostic information highlights that a “one size fits all” approach will not suffice for this difficult aspect of medical practice. Instead, our findings suggest that physicians need to develop the skills to understand the unique needs of surrogates and then tailor their approach to discussing prognosis to meet those needs. This is an area in need of well-designed quantitative and qualitative studies.
We feel that the suggestion from surrogates to openly discuss prognostic uncertainty is particularly important. This suggestion mirrors that of risk communication experts who emphasize the importance of acknowledging the uncertainty of both the risks and effectiveness of most medical treatments when helping patients make informed medical decisions (28, 29). It also reflects the reality of prognostication in ICUs: certainty is rarely possible. Prognostic scoring systems can provide accurate probabilistic survival estimates, but generally cannot prospectively identify patients certain to have a nonsurvivable condition (30). In most circumstances, physicians also cannot predict with certainty whether a particular patient will live or die until the latest stages of illness (31). Our findings suggest that most families do not expect this level of certainty from physicians' prognostications and that open acknowledgments of uncertainty may, in fact, foster family's trust in the physician.
This study has several strengths. The sample size is large for a qualitative study. The participants were diverse in terms of race, ethnicity, and socioeconomic status. The use of semi-structured interviews allowed us to understand not only what participants believed, but why they held their beliefs. The use of an inductive approach to data analysis allowed us to create a framework that emerged from the data rather than attempting to fit the data to a preconceived framework. Our use of a multidisciplinary team in analyzing the data allowed our interpretations to be informed by multiple perspectives. Finally, we received strong endorsements of the validity of our findings from study participants during the process of member checking in which we presented preliminary results back to study participants for comment and refinement.
This study also has several limitations. Our study did not include participants from two ethnic groups (Navajo Indians and Hmong individuals) in which there is a belief that discussing the possibility of death can cause harm to the patient (32, 33). In general, because of the cultural variability in attitudes on discussing death, our findings should be applied only with great caution to these ethnic groups and others—including African Americans—for whom similar beliefs are common (34). We interviewed subjects at only one timepoint during a patient's ICU stay (between Days 3 and 5 of the patient receiving mechanical ventilation). It is possible that their perspectives on uncertainty would be different if they were interviewed retrospectively or at another point in the hospitalization. However, we feel that a strength of the study was that we sought to understand the perspectives of surrogates at the time that they are actively confronted with prognostic uncertainty.
In summary, prognostic uncertainty is a difficult reality in the care of many patients with life-threatening illness. We found that most—but not all—surrogates accept this uncertainty as unavoidable, want physicians to discuss it openly, and see physicians' prognostications as an important way to help individuals navigate the difficulties of surrogate decision making.
Supported by National Institutes of Health grant KL2 RR024130 and the Greenwall Foundation (D.B.W.).
Originally Published in Press as DOI: 10.1164/rccm.200806-969OC on October 17, 2008
Conflict of Interest Statement: None of the authors has a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Barnato AE, Angus DC. Value and role of intensive care unit outcome prediction models in end-of-life decision making. Crit Care Clin 2004;20:345–362. (vii–viii.). [DOI] [PubMed] [Google Scholar]
- 2.Christakis NA, Iwashyna TJ. Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med 1998;158:2389–2395. [DOI] [PubMed] [Google Scholar]
- 3.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med 2007;35:442–448. [DOI] [PubMed] [Google Scholar]
- 4.Beauchamp TL, Childress JF. Principles of biomedical ethics, 5th ed. New York, NY: Oxford University Press; 2001.
- 5.Lynn JT III. On medical uncertainty. Am J Med 1994;96:186–187. [DOI] [PubMed] [Google Scholar]
- 6.Thorne S, Hislop TG, Kuo M, Armstrong EA. Hope and probability: patient perspectives of the meaning of numerical information in cancer communication. Qual Health Res 2006;16:318–336. [DOI] [PubMed] [Google Scholar]
- 7.Ogden J, Fuks K, Gardner M, Johnson S, McLean M, Martin P, Shah R. Doctors expressions of uncertainty and patient confidence. Patient Educ Couns 2002;48:171–176. [DOI] [PubMed] [Google Scholar]
- 8.Hickey M. What are the needs of families of critically ill patients? Focus Crit Care 1985;12:41–43. [PubMed] [Google Scholar]
- 9.Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Peters S, Tranmer JE, O'Callaghan CJ. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med 2003;29:75–82. [DOI] [PubMed] [Google Scholar]
- 10.LeClaire MM, Oakes JM, Weinert CR. Communication of prognostic information for critically ill patients. Chest 2005;128:1728–1735. [DOI] [PubMed] [Google Scholar]
- 11.Johnson CG, Levenkron JC, Suchman AL, Manchester R. Does physician uncertainty affect patient satisfaction? J Gen Intern Med 1988;3:144–149. [DOI] [PubMed] [Google Scholar]
- 12.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of adl: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 13.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. Thousand Oaks, CA: Sage Publications; 2006.
- 14.Glaser BG, Strauss AL. Discovery of grounded theory. Chicago: Adline Publishing Company; 1967.
- 15.Strauss AL, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage Publications; 1998.
- 16.Sackett DL. Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. 2nd ed. Boston: Little, Brown and Company; 1991.
- 17.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res 1999;34:1189–1208. [PMC free article] [PubMed] [Google Scholar]
- 18.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA 2000;284:357–362. [DOI] [PubMed] [Google Scholar]
- 19.SUPPORT. A controlled trial to improve care for seriously ill hospitalized patients. JAMA 1995;274:1591–1598. [PubMed] [Google Scholar]
- 20.Lo B. Improving care near the end of life. Why is it so hard? JAMA 1995;274:1634–1636. [PubMed] [Google Scholar]
- 21.Lynn J, De Vries KO, Arkes HR, Stevens M, Cohn F, Murphy P, Covinsky KE, Hamel MB, Dawson NV, Tsevat J. Ineffectiveness of the SUPPORT intervention: review of explanations. J Am Geriatr Soc 2000;48:S206–S213. [DOI] [PubMed] [Google Scholar]
- 22.Eggenberger SK, Nelms TP. Family interviews as a method for family research. J Adv Nurs 2007;58:282–292. [DOI] [PubMed] [Google Scholar]
- 23.Eggenberger SK, Nelms TP. Being family: the family experience when an adult member is hospitalized with a critical illness. J Clin Nurs 2007;16:1618–1628. [DOI] [PubMed] [Google Scholar]
- 24.Rich BA. Defining and delineating a duty to prognosticate. Theor Med Bioeth 2001;22:177–192. [DOI] [PubMed] [Google Scholar]
- 25.Christakis NA. Death foretold: prophecy and prognosis in medical care. Chicago, IL: University of Chicago Press; 1999.
- 26.Barry LC, Prigerson HG. Perspectives on preparedness for a death among bereaved persons. Conn Med 2002;66:691–696. [PubMed] [Google Scholar]
- 27.Hebert RS, Prigerson HG, Schulz R, Arnold RM. Preparing caregivers for the death of a loved one: a theoretical framework and suggestions for future research. J Palliat Med 2006;9:1164–1171. [DOI] [PubMed] [Google Scholar]
- 28.Paling J. Strategies to help patients understand risks. BMJ 2003;327:745–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomson R, Edwards A, Grey J. Risk communication in the clinical consultation. Clin Med 2005;5:465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berge KH, Maiers DR, Schreiner DP, Jewell SM, Bechtle PS, Schroeder DR, Stevens SR, Lanier WL. Resource utilization and outcome in gravely ill intensive care unit patients with predicted in-hospital mortality rates of 95% or higher by APACHE III scores: the relationship with physician and family expectations. Mayo Clin Proc 2005;80:166–173. [DOI] [PubMed] [Google Scholar]
- 31.Halevy A, Neal RC, Brody BA. The low frequency of futility in an adult intensive care unit setting. Arch Intern Med 1996;156:100–104. [PubMed] [Google Scholar]
- 32.Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation: benefit or harm? JAMA 1995;274:826–829. [PubMed] [Google Scholar]
- 33.Fadiman A. The spirit catches you and you fall down: a Hmong child, her American doctors, and the collision of two cultures. New York: Farrar, Straus, & Giroux; 1997.
- 34.Perkins HS, Shepherd KJ, Cortez JD, Hazuda HP. Exploring chronically ill seniors' attitudes about discussing death and postmortem medical procedures. J Am Geriatr Soc 2005;53:895–900. [DOI] [PubMed] [Google Scholar]