Abstract
Purpose
To determine whether performing near activities, while patching for amblyopia, enhances improvement in visual acuity.
Design
Randomized clinical trial
Participants
425 children, 3 to <7 years old, with amblyopia (20/40 to 20/400) due to anisometropia, strabismus or both, and which persisted after treatment with spectacles.
Methods
Children were randomized to 2 hours of patching per day with near activities or 2 hours of patching per day with distance activities. Instruction sheets describing common near and distance activities were given to the parents. Study visits were scheduled at 2, 5, 8 and 17 weeks. In weeks without a visit, weekly telephone calls were made to the parent to monitor and encourage compliance, during the first 8 weeks.
Main Outcome measure
Masked assessment of visual acuity by isolated crowded HOTV optotypes at 8 weeks.
Results
At 8 weeks, improvement in amblyopic eye visual acuity averaged 2.6 lines in the distance activities group and 2.5 lines in the near activities group (mean difference in acuity between groups, adjusted for baseline acuity, 0.0 lines; 95% confidence interval, -0.3 to 0.3). The two groups also appeared statistically similar at the 2-week, 5-week, and 17-week visits. At the 17-week examination, children with severe amblyopia improved a mean of 3.7 lines with two hours of daily patching.
Conclusions
Performing common near activities does not improve visual acuity outcome when treating anisometropic, strabismic or combined amblyopia with two hours of daily patching. Children with severe amblyopia may respond to two hours of daily patching.
Near visual activities are often prescribed during patching for amblyopia based on the assumption that those activities stimulate the visual system. A number of uncontrolled case series have suggested a benefit to prescribing near activities,1-4 but the question has not been rigorously studied. In recent randomized clinical trials comparing patching regimes for amblyopia conducted by the Pediatric Eye Disease Investigator Group, near activities were incorporated into each of the prescribed treatment regimes.5, 6 Most children completing these studies showed significant improvement of visual acuity, but it was unknown whether concurrent near activities enhanced the effect of patching.
As a prelude to a randomized clinical trial investigating the role of near activities, we performed a 4-week pilot randomized trial in which 64 children (age 3 to <7 years) with amblyopia performed either near activities or distance activities while patching two hours per day.7 Parents completed daily calendars recording the activities performed while patched, and received a weekly telephone call in which they were asked to describe the activities performed during the previous two hours of patching. This pilot study determined that separation of treatment groups could be achieved with respect to time spent performing near activities while patching, and therefore a formal randomized trial was feasible. Although not designed to compare visual acuity outcomes between treatment groups, the pilot study found greater improvement with near activities than with distance activities while patching in children with severe amblyopia (20/100 to 20/400) but not with moderate amblyopia (20/40 to 20/80).
We now report the results of the larger randomized clinical trial designed to determine whether prescribing near activities to be performed during patching therapy enhances the visual acuity outcome in amblyopic children 3 to <7 years old.
Methods
The study was supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health, Department of Health and Human Services and was conducted by the Pediatric Eye Disease Investigator Group (PEDIG) at 44 clinical sites. The protocol and Health Insurance Portability and Accountability Act (HIPAA) compliant informed consent forms were approved by institutional review boards, and a parent or guardian (referred to subsequently as “parent”) of each study patient gave written informed consent. Study oversight was provided by an independent Data Safety Monitoring Committee. The study is listed on www.clinicaltrials.gov, identifier NCT00315198 (accessed May 10, 2008). The protocol, which is available on the PEDIG website (www.pedig.net, accessed May 10, 2008), is summarized below.
Synopsis of Study Design
The major eligibility criteria for the trial included (1) age 3 to <7 years, (2) visual acuity in the amblyopic eye between 20/40 and 20/400 inclusive, (3) visual acuity in the sound eye of 20/40 or better, (4) interocular acuity difference of ≥ 3 logarithm of the minimum angle of resolution (logMAR) lines, (5) the presence or history of an amblyogenic factor meeting study-specified criteria for strabismus and/or anisometropia, and (6) the wearing of optimal spectacle correction for a minimum of 16 weeks or until stability of visual acuity was documented (no improvement in amblyopic eye visual acuity at 2 consecutive visits at least 4 weeks apart). The decision to require a period of spectacle wear until stability, or for 16 weeks, was based on a previous PEDIG study that showed effectiveness of spectacles alone in a proportion of children with amblyopia.8 Exclusion criteria included (1) myopia greater than -6.00 diopters (D) spherical equivalent in the amblyopic eye and (2) treatment for amblyopia (other than spectacle correction) for more than one month within the 6 months prior to enrollment. Table 1 provides a complete listing of the eligibility and exclusion criteria.
Table 1. Eligibility and Exclusion Criteria.
Eligibility Criteria
|
Exclusion Criteria
|
D = diopters. ATS = Amblyopia Treatment Study
After informed consent was obtained and eligibility was confirmed, data were entered on the PEDIG website to randomly assign each patient with equal probability to one of two treatment groups: near activities or distance visual activities to be performed during two hours of daily patching. A permuted blocks randomization schedule, stratified by site and amblyopic eye visual acuity, was used.
Follow-up visits were scheduled at 2 weeks (± 3 days), 5 weeks (± 1 week), 8 weeks (± 1 week), and 17 weeks (± 1 week). In weeks without a visit during the first 8 weeks, telephone calls were made to the parent to monitor and encourage compliance. The primary outcome was amblyopic eye visual acuity at the 8-week visit. The timing of the primary outcome was chosen because we felt it was not feasible to continue weekly telephone calls to the family for the entire 17 weeks to encourage compliance with the treatment group assignment. The visual acuity examiner was masked to treatment group assignment for testing at the 8-week and 17-week visits.
Treatment Protocols
Parents were instructed to patch their child's sound eye for 2 hours per day. Treatment-group specific instruction sheets were given to the parent listing examples of “near” or “distance” activities. Near activities included some tasks that specifically required hand-eye coordination in close proximity such as crafts, reading, writing, and computer or video games. Distance activities included supervised outdoor play and watching television (at a distance of at least 6 feet). Additional examples of the near activities and distance activities are given in Table 2 (available at http://aaojournal.org).
Table 2. Classification of activities recorded on the calendars as “near” and “distance” in both treatment groups.
| Distance Activities Group | Near Activities Group | |||
|---|---|---|---|---|
| Number of times reported | Total time spent (hours) | Number of times reported | Total time spent (hours) | |
| Near activities | ||||
| Arts & crafts | 414 | 276 | 6615 | 5471 |
| Blocks/marbles/dominoes | 153 | 88 | 1605 | 1111 |
| Board games/puzzles/card games | 387 | 242 | 3909 | 3038 |
| Cars up close | 28 | 23 | 230 | 158 |
| Computer/video game | 802 | 650 | 6760 | 7064 |
| Counting up close | 16 | 9 | 45 | 19 |
| Dolls/action figures up close | 18 | 13 | 164 | 123 |
| Homework | 402 | 394 | 1986 | 1452 |
| Lite Brite | 3 | 2 | 81 | 70 |
| Playing with toys up close | 39 | 21 | 442 | 288 |
| Sorting/stringing beads | 3 | 2 | 233 | 167 |
| Stacking coins | 3 | 2 | 17 | 8 |
| Tying shoes | 1 | 1 | 7 | 4 |
| Writing/reading/activity books | 306 | 197 | 5802 | 4069 |
| Total | 2575 | 1920 | 27899 | 23044 |
| Distance activities | ||||
| Active/physical games | 3900 | 3373 | 422 | 292 |
| Cars at a distance | 1 | 1 | 1 | 1 |
| Chores | 2147 | 1339 | 386 | 181 |
| Counting at distance | 199 | 150 | 9 | 6 |
| Dolls/action figures at a distance | 2 | 2 | 0 | 0 |
| Dressing | 556 | 148 | 67 | 16 |
| Errands/car rides | 3979 | 4111 | 206 | 136 |
| General indoor play | 1002 | 938 | 80 | 68 |
| General outdoor play | 2361 | 2626 | 114 | 97 |
| Indoor events / locations | 468 | 728 | 64 | 81 |
| Listening/singing | 800 | 415 | 203 | 89 |
| Make-believe games | 580 | 496 | 153 | 108 |
| Outdoor events/locations | 727 | 1096 | 22 | 23 |
| Playing | 1018 | 922 | 308 | 226 |
| Playing ball | 957 | 733 | 126 | 77 |
| Playing with toy at a distance | 43 | 52 | 1 | 0 |
| Remote control toys | 49 | 23 | 3 | 2 |
| Riding bike | 863 | 622 | 107 | 70 |
| Television | 9111 | 9886 | 1669 | 1268 |
| Visiting/playing with friends/family | 962 | 902 | 126 | 89 |
| Total | 29725 | 28562 | 4068 | 2829 |
| Uncertain | ||||
| Cars | 234 | 128 | 578 | 396 |
| Counting | 114 | 75 | 80 | 40 |
| Dolls/action figures | 364 | 270 | 1320 | 1025 |
| Eating | 4767 | 2312 | 2248 | 961 |
| Flying kite | 13 | 10 | 2 | 2 |
| Grooming | 649 | 247 | 161 | 58 |
| Making food | 417 | 211 | 315 | 180 |
| Picking fruit | 102 | 67 | 52 | 38 |
| Playing pool | 32 | 22 | 40 | 26 |
| Playing with toys | 713 | 589 | 1094 | 824 |
| Spelling | 2 | 2 | 19 | 9 |
| Total | 7407 | 3933 | 5909 | 3558 |
Adhesive skin patches, provided by the study (Coverlet Eye Occlusors, Beiersdorf-Jobst, Inc., Rutherford College, NC), were used. In cases where wearing the patch was associated with a skin allergy or irritation unresponsive to both local treatment with a skin emollient and a change in brand of patch, a hypoallergenic brand or a spectacle-mounted occluder was prescribed (13 patients). At the 8-week visit, daily patching hours could be increased at investigator discretion, and parents were instructed to have their child continue activities while patched in accordance with his/her randomization assignment.
Parents were given calendars to complete each day recording the number of patching hours and the activities the child performed while patched. Calendars were mailed to the coordinating center in postage-paid envelopes at the end of each week of the study. Weekly calendars were defined as “complete” if they had at least one activity entry on each of the seven days. “Partially complete” weekly calendars were defined as at least one day with activity data, but less than seven days. Telephone interviews were conducted in weeks without a visit. The interviewer followed a script and recorded the duration of activities performed during the most recent 2-hour patching period, either earlier that day or on the previous day. All recorded activities were classified by coordinating center personnel as “distance” or “near” without reference to treatment group. At each visit, adherence to the treatment protocol was also assessed by the investigator, who had access via the study website to any telephone and calendar compliance data that were available at the time of the visit. Based on discussion with the parents and review of telephone call and calendar data, the investigator made an assessment of both patching compliance and activities compliance as excellent (76%-100% of prescribed treatment completed), good (51%-75%), fair (26%-50%), or poor (≤ 25%).
Examination Procedures
At baseline and at each protocol-specified visit, visual acuity was measured in each eye using the Amblyopia Treatment Study (ATS) visual acuity testing protocol (which uses single-surrounded HOTV optotypes),9 administered by a study-certified vision examiner using an electronic visual acuity tester.10
Additional baseline testing included (1) an ocular examination, (2) a cycloplegic refraction, (3) measurement of ocular alignment with a simultaneous prism and cover test (SPCT) at distance and near, and (4) assessment of binocularity with the Titmus Test (fly only) and the Randot Preschool Stereoacuity Test (Stereo Optical Co., Chicago, IL). Ocular alignment was assessed and stereoacuity was measured at the 17-week visit.
Statistical Methods
The pilot trial7 suggested that a treatment effect might exist for severe amblyopia but not for moderate amblyopia. Therefore, the sample size was estimated in order to provide sufficient power for each of two preplanned subgroup analyses based on baseline amblyopic eye visual acuity. For moderate amblyopia (baseline visual acuity 20/40 to 20/80), a sample size of 266 patients was needed to provide 80% power to detect a 0.05 difference in mean logMAR visual acuity at 8 weeks, assuming a common standard deviation of 0.15 and correlation between the baseline and outcome acuity of 0.35. For severe amblyopia (baseline visual acuity 20/100 to 20/400), we anticipated enrolling approximately half the numbers of patients during the same period, based on concurrent enrollment during previous studies, and 134 patients would provide 80% power to detect a 0.12 difference in mean logMAR acuity at 8 weeks, assuming a common standard deviation of 0.25 and correlation between the baseline and outcome acuity of 0.29. For the primary overall analysis, the total sample size of 400 patients provided 90% power to detect a difference of 0.06 logMAR between treatment groups in mean visual acuity at 8 weeks, assuming a common standard deviation of 0.20 and correlation between the baseline and outcome acuity of 0.44. All sample size calculations were based on a 2-sided type I error of 0.05, and used assumptions for standard deviation of mean logMAR visual acuity and correlation between baseline and follow-up visual acuity derived from previous ATS studies, with allowance for 5% loss to follow up.
The primary analysis was a treatment group comparison including all patients with baseline amblyopic eye visual acuity 20/40 – 20/400 of logMAR visual acuity scores in an analysis of covariance model adjusting for baseline acuity. All analyses followed the intent-to-treat principle. To be included in the primary analysis, the 8-week examination could be performed no earlier than 6 weeks and no later than 12 weeks after randomization. Similar results were also obtained from alternative analyses (1) including only visits completed in the visit window of 8±1 weeks from randomization and (2) using the last-observation-carried-forward method to impute for missing data (data not shown). Preplanned subgroup analyses for subgroups of moderate and severe amblyopia mirrored the primary analysis. The exact Wilcoxon rank sum test was used for treatment group comparison of stereoacuity test scores.
Time spent per day patching and performing near and distance activities were tabulated by treatment group. Activities that could not be classified as either distance or near were counted as “distance” activities for the primary analysis of activities. Nevertheless, a separate analysis counting unclassifiable activities as “near” activities produced similar results (data not shown). In a secondary analysis, visual activities were reclassified based on whether they involved hand-eye coordination. The association between the average daily proportion of time spent performing hand-eye coordination activities while patched and improvement in amblyopic eye acuity was evaluated in a multiple linear regression model adjusting for baseline amblyopic eye visual acuity.
Results
Between February 2005 and June 2007, 425 patients entered the trial at 44 sites (range 1 to 42 patients per site, median 5.5), with 218 assigned to the distance activities group and 207 assigned to the near activities group. The average age of the patients was 5.4 years; 47% were female, and 77% were white. The mean visual acuity in the amblyopic eye at enrollment was 0.57 logMAR (approximately 20/80), with a mean difference in acuity between eyes of 5.2 lines. The baseline characteristics of the 2 groups are provided in Table 3 (baseline characteristics are reported separately for the cases with moderate amblyopia and severe amblyopia in Table 4, available at http://aaojournal.org).
Table 3. Baseline Data for all Randomized Patients.
| Distance Activities
Group N=218 |
Near Activities
Group N=207 |
|
|---|---|---|
| n (%) | n (%) | |
| Gender: Female | 100 (46) | 98 (47) |
|
| ||
| Race / Ethnicity | ||
| White | 171 (78) | 156 (75) |
| African-American | 12 (6) | 11 (5) |
| Hispanic or Latino | 23 (11) | 23 (11) |
| Asian | 4 (2) | 7 (3) |
| More than one race | 2 (1) | 3 (1) |
| Unknown/not reported | 6 (3) | 7 (3) |
|
| ||
| Age at Enrollment | ||
| 3 to <4 years | 24 (11) | 27 (13) |
| 4 to <5 years | 53 (24) | 42 (20) |
| 5 to <6 years | 64 (29) | 74 (36) |
| 6 to <7 years | 77 (35) | 64 (31) |
| Mean (SD) | 5.4 (1.0) | 5.4 (1.0) |
|
| ||
| Prior Treatment for Amblyopia at Enrollment | ||
| None | 199 (91) | 193 (93) |
| Patching | 15 (7) | 8 (4) |
| Atropine | 1 (<1) | 2 (1) |
| Patching and Atropine | 3 (1) | 4 (2) |
|
| ||
| Cause of Amblyopia | ||
| Strabismus | 58 (27) | 61 (29) |
| Anisometropia | 115 (53) | 100 (48) |
| Strabismus and anisometropia | 45 (21) | 46 (22) |
|
| ||
| Distance Visual Acuity in Amblyopic Eye | ||
| 20/100 to 20/400 | 69 (32) | 66 (32) |
| 20/40 to 20/80 | 149 (68) | 141 (68) |
| Mean (SD) logMAR | 0.58 (0.22) | 0.56 (0.23) |
|
| ||
| Distance Visual Acuity in Sound Eye | ||
| 20/40 | 6 (3) | 13 (6) |
| 20/32 | 29 (13) | 25 (12) |
| 20/25 | 56 (26) | 51 (25) |
| 20/20 | 94 (43) | 91 (44) |
| 20/16 | 33 (15) | 27 (13) |
| Mean (SD) logMAR | 0.05 (0.10) | 0.05 (0.11) |
|
| ||
| Intereye Acuity Difference | ||
| Mean (SD) logMAR lines | 5.4 (2.3) | 5.1 (2.1) |
|
| ||
| Refractive Error in Amblyopic Eye | ||
| <0 D | 13 (6) | 13 (6) |
| 0 to <+1.00D | 11 (5) | 11 (5) |
| +1.00 to <+2.00D | 15 (7) | 16 (8) |
| +2.00 to <+3.00D | 20 (9) | 21 (10) |
| +3.00 to <+4.00D | 30 (14) | 16 (8) |
| ≥+4.00D | 129 (59) | 130 (63) |
| Mean (SD) logMAR | +4.07 (2.59) | +4.06 (2.56) |
|
| ||
| Refractive Error in Sound Eye | ||
| <0 D | 7 (3) | 7 (3) |
| 0 to <+1.00D | 46 (21) | 56 (27) |
| +1.00 to <+2.00D | 60 (28) | 48 (23) |
| +2.00 to <+3.00D | 32 (15) | 20 (10) |
| +3.00 to <+4.00D | 23 (11) | 28 (14) |
| ≥+4.00D | 50 (23) | 48 (23) |
| Mean (SD) logMAR | +2.38 (1.99) | +2.37 (2.12) |
SD = standard deviation; logMAR = logarithm of the minimum angle of resolution; D = diopters.
Table 4. Baseline Data for all Randomized Patients by Severity.
| Baseline Amblyopic Eye Acuity
|
||||
|---|---|---|---|---|
| 20/40 to 20/80 | 20/100 to 20/400 | |||
| Distance Activities
Group N=149 |
Near Activities
Group N=141 |
Distance Activities
Group N=69 |
Near Activities
Group N=66 |
|
| n (%) | n (%) | n (%) | n (%) | |
| Gender: Female | 67 (45) | 67 (48) | 33 (48) | 31 (47) |
|
| ||||
| Race / Ethnicity | ||||
| White | 115 (77) | 105 (74) | 56 (81) | 51 (77) |
| African-American | 7 (5) | 8 (6) | 5 (7) | 3 (5) |
| Hispanic or Latino | 17 (11) | 15 (11) | 6 (9) | 8 (12) |
| Asian | 4 (3) | 5 (4) | 0 | 2 (3) |
| More than one race | 1 (1) | 3 (2) | 1 (1) | 0 |
| Unknown/not reported | 5 (3) | 5 (4) | 1 (1) | 2 (3) |
|
| ||||
| Age at Enrollment | ||||
| 3 to <4 years | 14 (9) | 15 (11) | 10 (14) | 12 (18) |
| 4 to <5 years | 40 (27) | 26 (18) | 13 (19) | 16 (24) |
| 5 to <6 years | 41 (28) | 52 (37) | 23 (33) | 22 (33) |
| 6 to <7 years | 54 (36) | 48 (34) | 23 (33) | 16 (24) |
| Mean (SD) | 5.4 (1.0) | 5.5 (1.0) | 5.4 (1.1) | 5.1 (1.1) |
|
| ||||
| Prior Treatment for Amblyopia at Enrollment | ||||
| None | 139 (93) | 130 (92) | 60 (87) | 63 (95) |
| Patching | 6 (4) | 5 (4) | 9 (13) | 3 (5) |
| Atropine | 1 (1) | 2 (1) | 0 | 0 |
| Patching and Atropine | 3 (2) | 4 (3) | 0 | 0 |
|
| ||||
| Cause of Amblyopia | ||||
| Strabismus | 42 (28) | 42 (30) | 16 (23) | 19 (29) |
| Anisometropia | 85 (57) | 71 (50) | 30 (43) | 29 (44) |
| Strabismus and anisometropia | 22 (15) | 28 (20) | 23 (33) | 18 (27) |
|
| ||||
| Distance Visual Acuity in Amblyopic Eye | ||||
| Mean (SD) logMAR | 0.46 (0.10) | 0.42 (0.10) | 0.84 (0.17) | 0.85 (0.16) |
|
| ||||
| Distance Visual Acuity in Sound Eye | ||||
| 20/40 | 4 (3) | 3 (2) | 2 (3) | 10 (15) |
| 20/32 | 17 (11) | 13 (9) | 12 (17) | 12 (18) |
| 20/25 | 41 (28) | 34 (24) | 15 (22) | 17 (26) |
| 20/20 | 64 (43) | 68 (48) | 30 (44) | 23 (35) |
| 20/16 | 23 (15) | 23 (16) | 10 (14) | 4 (6) |
| Mean (SD) logMAR | 0.04 (0.10) | 0.03 (0.09) | 0.05 (0.10) | 0.10 (0.12) |
|
| ||||
| Intereye Acuity Difference | ||||
| Mean (SD) logMAR lines | 4.2 (1.1) | 3.9 (1.0) | 7.9 (2.0) | 7.5 (1.9) |
|
| ||||
| Refractive Error in Amblyopic Eye | ||||
| <0 D | 7 (5) | 9 (6) | 6 (9) | 4 (6) |
| 0 to <+1.00D | 8 (5) | 10 (7) | 3 (4) | 1 (2) |
| +1.00 to <+2.00D | 12 (8) | 13 (9) | 3 (4) | 3 (5) |
| +2.00 to <+3.00D | 18 (12) | 17 (12) | 2 (3) | 4 (6) |
| +3.00 to <+4.00D | 24 (16) | 14 (10) | 6 (9) | 2 (3) |
| ≥+4.00D | 80 (54) | 78 (55) | 49 (71) | 52 (79) |
| Mean (SD) logMAR | 3.89 (2.34) | 3.73 (2.39) | 4.47 (3.05) | 4.76 (2.77) |
|
| ||||
| Refractive Error in Sound Eye | ||||
| <0 D | 4 (3) | 5 (4) | 3 (4) | 2 (3) |
| 0 to <+1.00D | 29 (19) | 43 (30) | 17 (25) | 13 (20) |
| +1.00 to <+2.00D | 44 (30) | 32 (23) | 16 (23) | 16 (24) |
| +2.00 to <+3.00D | 24 (16) | 11 (8) | 8 (12) | 9 (14) |
| +3.00 to <+4.00D | 16 (11) | 18 (13) | 7 (10) | 10 (15) |
| ≥+4.00D | 32 (21) | 32 (23) | 18 (26) | 16 (24) |
| Mean (SD) logMAR | 2.39 (1.93) | 2.26 (2.10) | 2.36 (2.13) | 2.58 (2.15) |
SD = standard deviation; logMAR = logarithm of the minimum angle of resolution; D = diopters.
Protocol Adherence
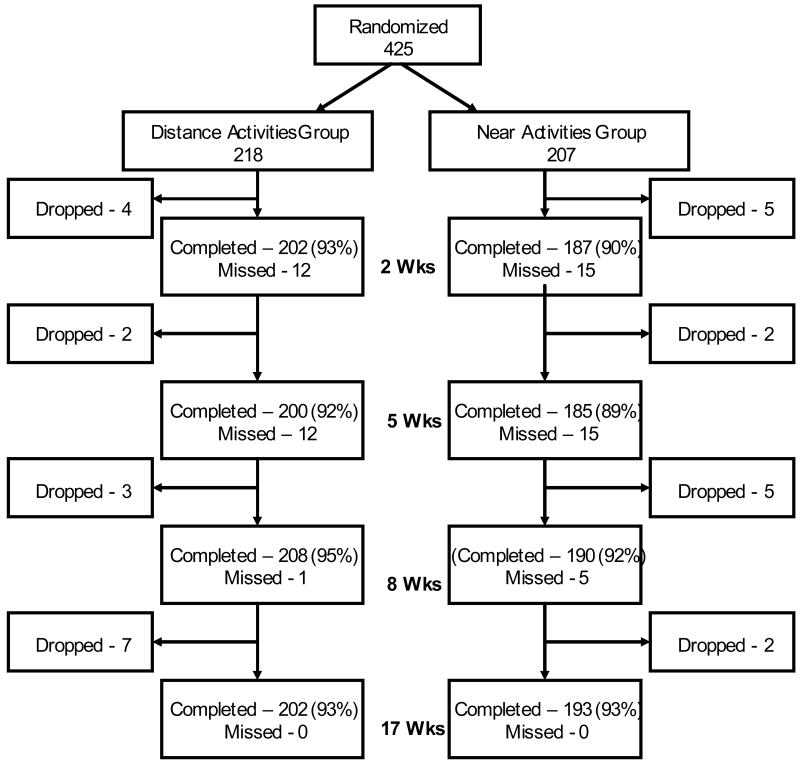
Figure 1 provides the visit completion rates for the 2-week, 5-week, 8-week, and 17-week visits. The 8-week (primary outcome) examination was completed by 208 (95%) of the 218 patients in the distance activities group and 190 (92%) of the 207 patients in the near activities group. The vision tester was masked as to treatment group for 97% of these tests in each group.
Figure 1. Visit Completion.
Flow chart showing study completion in each treatment group.
During the first 8 weeks, 87% of the distance activities group and 89% of the near activities group submitted at least 4 of the expected 8 calendars, and 75% and 82% respectively submitted at least 7. Telephone call completion averaged 4.3 ± 0.9 calls (81% completing at least 4 of the 5 calls) in the distance activities group and 4.3 ± 0.8 calls (85% completing at least 4 of the 5 calls) in the near activities group.
Based on the submitted calendars during the first 8 weeks of the study, the mean duration of patching was 1.9 ± 0.2 hours per day in the distance activities group and 1.9 ± 0.3 hours per day in the near activities group. Between the 8-week visit and the 17-week visit, the mean number of hours patched per day was 2.1 ± 0.7 and 1.9 ± 0.5 in distance and near groups respectively. Data obtained during the telephone interviews revealed similar estimates of patching to those obtained from the calendars. During the 17 weeks of the study, patient adherence with the prescribed patching treatment was judged by the investigator to be excellent in 72%, good in 17%, fair in 6%, and poor in 6% of patients in the distance activities group, and to be excellent in 64%, good in 20%, fair in 9%, and poor in 7% of patients in the near activities group.
Among the patients completing the 8-week outcome examination, the patching prescription was 2 hours per day throughout 17 weeks of follow-up for 181 (87%) of the 208 patients in the distance activities group and for 172 (91%) of the 190 patients in the near activities group. For 20 patients in the distance activities group and 11 patients in the near activities group, patching hours were increased after the 8-week outcome exam at investigator discretion. For 5 patients in the distance activities group and 5 patients in the near activities group, patching and activities were stopped or reduced after the 8-week outcome exam because acuity in the amblyopic eye was the same as or better than that of the sound eye. Patching and activities were stopped for one patient in the near activities group after the 5-week exam. Two patients in the distance activities group and one patient in the near activities group were switched to atropine after initially patching, prior to the 8-week outcome exam (all changes to atropine were at parents' request).
Based on calendar entries from the first 8 weeks of the study, the distance activities group averaged 1.9 ± 0.2 hours per day of distance activities and 0.1 ± 0.1 hours per day of near activities during patching, while the near activities group averaged 1.5 ± 0.4 hours per day of near activities and 0.4 ± 0.4 hours per day of distance activities. Between the 8-week visit and the 17-week visit, the mean number of hours per day of distance activities while patching was 2.0 ± 0.7 for the distance activities group and 0.4 ± 0.4 in the near activities group. Between the 8-week visit and the 17-week visit, the mean number of hours per day of near activities while patching was 0.1 ± 0.3 for the distance activities group and 1.5 ± 0.5, for the near activities group. The estimate of time spent in near activities obtained from the telephone interviews was similar to the calendars. During the 17 weeks of the study, patient adherence to hours spent in assigned visual activities was judged by the investigator to be excellent in 72%, good in 16%, fair in 8%, and poor in 5% of patients in the distance activities group, and to be excellent in 66%, good in 18%, fair in 10%, and poor in 7% of patients in the near activities group.
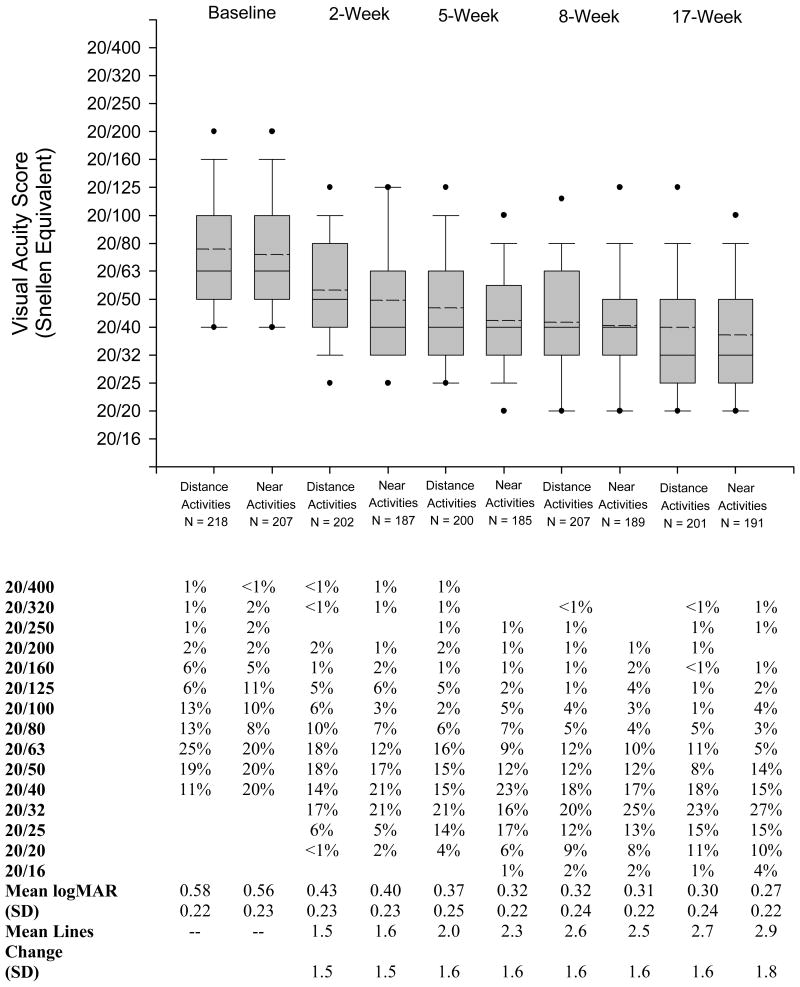
Effect of Treatment on Visual Acuity in the Amblyopic Eye
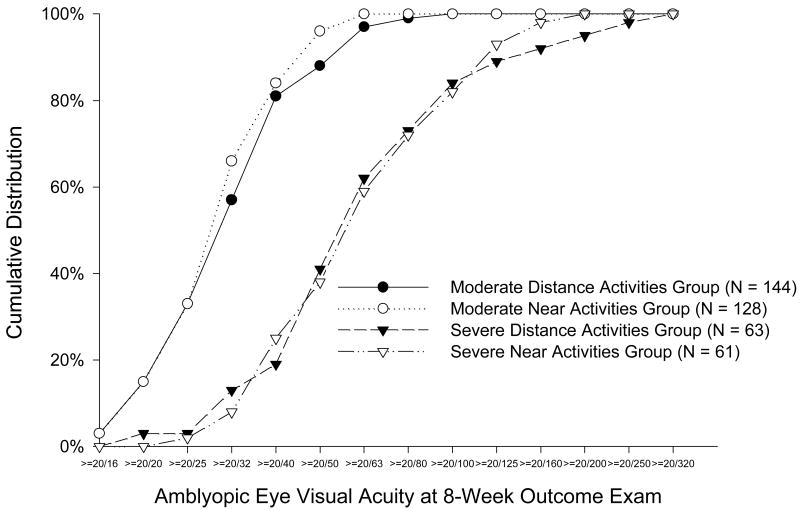
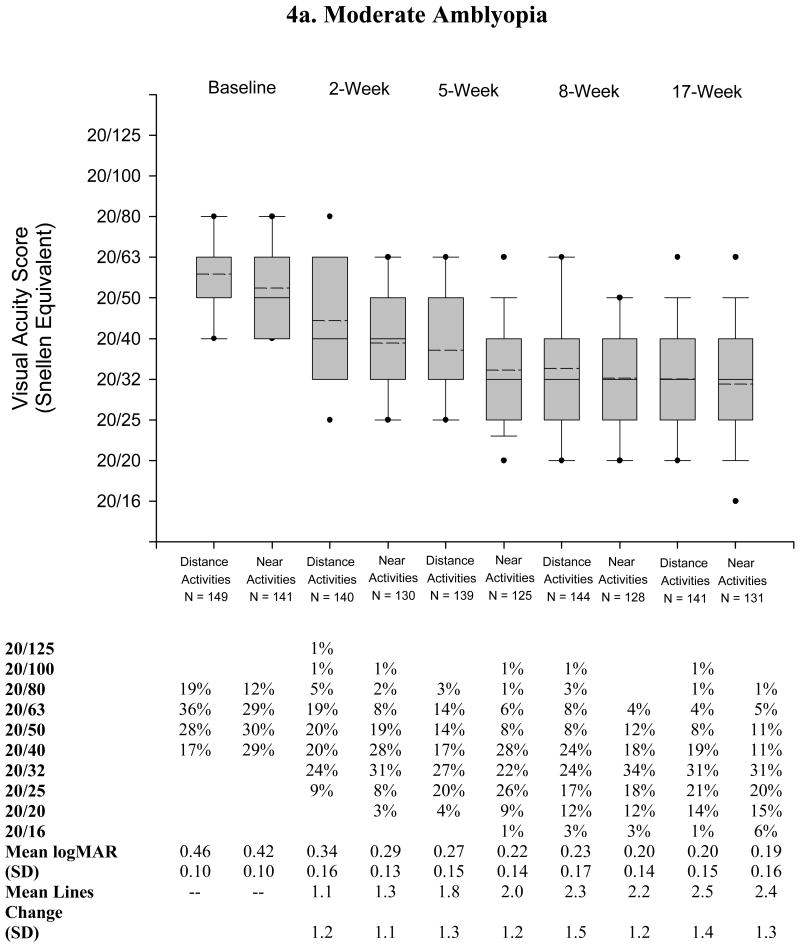
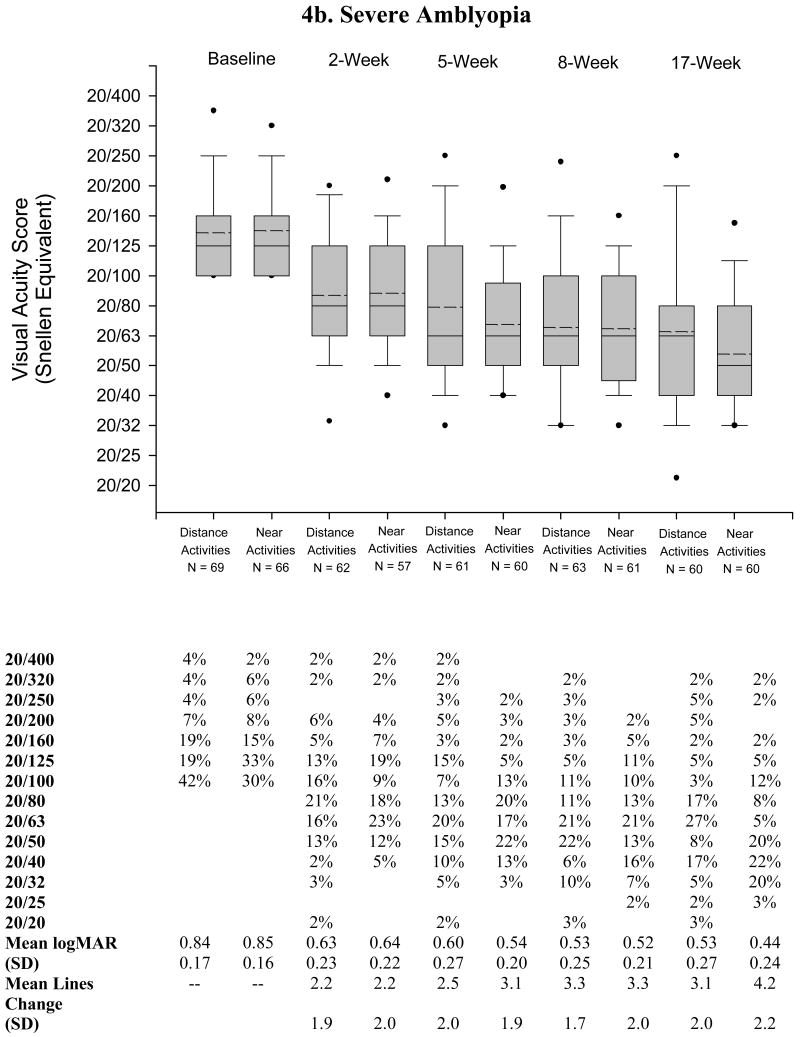
At the 8-week (primary outcome) examination, improvement in amblyopic eye visual acuity averaged 2.6 lines in the distance activities group and 2.5 lines in the near activities group (mean difference in acuity between groups adjusted for baseline acuity = 0.0 lines; 95% confidence interval, -0.3 to 0.3). The two groups were also statistically similar at the 2-week, 5-week, and 17-week visits (Table 5, Figure 2). In the preplanned analysis of moderate and severe subgroups at the 8-week visit, there was no difference between treatment groups for either moderate (mean difference in acuity between treatment groups = 0.0 lines; 95% confidence interval, -0.3 to 0.4) or severe amblyopia (mean difference in acuity between treatment groups = 0.0 lines; 95% confidence interval, -0.7 to 0.7) (Table 5, Figure 3). For moderate amblyopia, the two treatment groups also were statistically similar at the 2-, 5-, and 17-week visits (Figure 4a, available at http://aaojournal.org), but, there was a suggestion of greater visual acuity improvement in the near activities group at 17 weeks in those who had severe amblyopia at baseline (mean difference in acuity between groups, -1.0 lines; 95% confidence interval, -1.8 to -0.3) (Table 5, Figure 4b, available at http://aaojournal.org). It was noteworthy that children with severe amblyopia improved a mean of 3.7 lines at the 17-week examination, with the prescribed regime of two hours daily patching. Six patients with severe amblyopia had complete resolution of their amblyopia (within one line of sound eye) by the 17-week outcome visit.
Table 5. Mean Lines Change in Amblyopic Eye Visual Acuity from Baseline to Each Visit.
| Distance Activities
Group |
Near Activities
Group |
Mean Difference
(95% Confidence Interval) |
||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Overall | 2 Wk Visit | 202 | 1.5 (1.5) | 187 | 1.6 (1.5) | -0.2 (-0.5, 0.1) |
| 5 Wk Visit | 200 | 2.0 (1.6) | 185 | 2.3 (1.6) | -0.3 (-0.7, 0.0) | |
| 8 Wk Visit | 207 | 2.6 (1.6) | 189 | 2.5 (1.6) | 0.0 (-0.3, 0.3) | |
| 17 Wk Visit | 201 | 2.7 (1.6) | 191 | 2.9 (1.8) | -0.3 (-0.6, 0.1) | |
|
| ||||||
| 20/40 to 20/80 | 2 Wk Visit | 140 | 1.1 (1.2) | 130 | 1.3 (1.1) | -0.3 (-0.5, 0.0) |
| 5 Wk Visit | 139 | 1.8 (1.3) | 125 | 2.0 (1.2) | -0.2 (-0.5, 0.1) | |
| 8 Wk Visit | 144 | 2.3 (1.5) | 128 | 2.2 (1.2) | 0.0 (-0.3, 0.4) | |
| 17 Wk Visit | 141 | 2.5 (1.4) | 131 | 2.4 (1.3) | 0.1 (-0.2, 0.4) | |
|
| ||||||
| 20/100 to 20/400 | 2 Wk Visit | 62 | 2.2 (1.9) | 57 | 2.2 (2.0) | 0.0 (-0.7, 0.7) |
| 5 Wk Visit | 61 | 2.5 (2.0) | 60 | 3.1 (1.9) | -0.6 (-1.3, 0.1) | |
| 8 Wk Visit | 63 | 3.3 (1.7) | 61 | 3.3 (2.0) | 0.0 (-0.7, 0.7) | |
| 17 Wk Visit | 60 | 3.1 (2.0) | 60 | 4.2 (2.2) | -1.0 (-1.8, -0.3) | |
SD = standard deviation.
Figure 2. Amblyopic Eye Visual Acuity in Each Group at Baseline, 2 Weeks, 5 Weeks, 8 Weeks, and 17 Weeks.
Amblyopic eye visual acuity in each group at baseline, 2 weeks, 5 weeks, 8 weeks, and 17 weeks. Box-whisker plot demonstrating mean (dashed horizontal line), median (solid horizontal line), 25 – 75th percentiles (extremes of the box), 10-90th percentiles (whiskers), and 5-95th percentiles (solid circles) of visual acuity at the visit. (logMAR = logarithm of minimum angle of resolution)
Figure 3. Cumulative Distribution of Amblyopic Eye Visual Acuity Scores at the 8-Week Outcome Examination According to Treatment Group.
Cumulative distribution of amblyopic eye visual acuity scores at 8-week outcome exam according to treatment group and amblyopia severity group at baseline.
Figure 4. Amblyopic Eye Visual Acuity in Each Group at Baseline, 2 Weeks, 5 Weeks, 8 Weeks, and 17 Weeks By Severity.
Amblyopic eye visual acuity in each treatment and amblyopia severity group at baseline, 2 weeks, 5 weeks, 8 weeks, and 17 weeks. Box-whisker plot demonstrating mean (dashed horizontal line), median (solid horizontal line), 25 – 75th percentiles (extremes of the box), 10-90th percentiles (whiskers), and 5-95th percentiles (solid circles) of visual acuity at the visit. (logMAR = logarithm of minimum angle of resolution)
In a secondary analysis in which activities were reclassified based on whether they involved eye-hand coordination, there was no association between the amount of time spent performing eye-hand coordination activities and the improvement in amblyopic eye acuity (P= 0.72)
Sound eye visual acuity, alignment and stereoacuity
The change in sound eye acuity from baseline to 17 weeks averaged 0.3 ± 0.9 lines of improvement in the distance activities group and 0.3 ± 0.9 lines in the near activities group. There were no cases of reverse amblyopia. Eighteen (9%) in the distance activities group developed a new ocular misalignment (tropia at either distance or near) during the 17 week study, compared with 13 (7%) in the near activities group. One patient (<1%) in the distance activities group, and 3 (2%) in the near activities group, had an increase in magnitude of their tropia of at least 10 prism diopters (either distance or near). The distribution of responses to the Preschool randot stereoacuity test was similar in the two treatment groups at the 17-week visit (P=0.25).
Discussion
In this randomized clinical trial, we found no difference in visual acuity improvement between children who performed common near activities and those who performed distance activities during patching treatment for amblyopia. This finding is in contrast to the results of our previous randomized pilot study7 and in contrast to several case series reporting the effect of near activities or activities involving eye-hand coordination.2-4
When we designed our previous studies of patching regimes,5, 6, 10 comparing prescribed full-time patching to 6 hours/day in severe amblyopia and comparing prescribed 6 hours/day to 2 hours/day in moderate amblyopia, we included instructions to perform one hour of near activities per day. This decision was made at that time to standardize the treatment regimen because polling our investigator group revealed that near activities were commonly prescribed during patching. Based on similar visual acuity improvement between prescribed full-time patching and 6 hours/day in severe amblyopia5 and between prescribed 6 hours/day and 2 hours/day in moderate amblyopia6 we have previously recommended that initial amblyopia treatment might start with 6 hours/day for severe amblyopia and 2 hours/day for moderate amblyopia. Nevertheless, a number of questions remained unanswered including: 1) were near activities important for the effectiveness of the 2 hours/day regime in moderate amblyopia? and 2) would a lower intensity of patching such as 2 hours/day be effective in severe amblyopia?
To compare the effect of near and distance activities on amblyopia treatment in the current study, it was necessary to have similar amounts of patching in the two groups and a large separation between groups in the amount of time spent performing near activities while patching. This was accomplished by designing the study to have weekly contacts with the patients for the first 8 weeks, either with an office visit or a telephone contact. Although it is appealing to postulate that near activities might enhance compliance with patching, our study found no evidence supporting this suggestion. Reported patching hours were similar between treatment groups. Therefore it does not seem reasonable to advocate near activities, solely for the purpose of enhancing compliance with prescribed patching.
We believe that the small difference in amblyopic eye acuity between treatment groups at 17 weeks in the children with severe amblyopia is most likely due to chance, since 1) there was no difference between groups at the 2-, 5- and 8-week visits, and the previous pilot study had suggested an early effect, not a late effect, and 2) we are unable to postulate a biologically plausible mechanism for a late effect with severe amblyopia but not moderate amblyopia.
We are not aware of any previous randomized trials evaluating the question of the value of near activities while patching other than our own previous randomized pilot study. In view of the results of the present larger trial, the finding of a mean one logMAR line difference between the near activities group and non-near activities group in the pilot study7 was likely due to chance. Others have reported case series in which near activities, or activities requiring hand-eye coordination, were prescribed during patching for amblyopia.1-4 None of these reports included a concurrent comparison group or randomization, so it is difficult to interpret their findings. It is possible that activities, other than those performed in the present study, such as more highly structured near activities specifically aimed at improving accommodation, might enhance the effect of patching. Based on the uncontrolled case series described above, it is conceivable that activities involving hand-eye coordination, rather than strictly near activities might be more beneficial. Nevertheless, when we performed a secondary analysis, recategorizing activities into those that involved hand-eye coordination and those that did not, we found no evidence of a beneficial effect of activities involving hand-eye coordination on visual acuity outcome. In addition, we only studied the effect of distance versus near activities during two hours of daily patching, and we cannot extrapolate to shorter or longer periods of prescribed patching.
A secondary but important finding of our study is that children with severe amblyopia (20/100 to 20/400) showed improvement in visual acuity with 2 hours/day of prescribed patching (regardless of near or distance activities). At 17 weeks, visual acuity was improved from baseline by a mean of 3.6 lines. This improvement was less than we found in a previous clinical trial comparing prescribed full time patching to prescribed 6-hours/day patching, where mean visual acuity improvement at 17-weeks was 4.7 and 4.8 lines respectively. However, an important difference between the present study and the previous patching regime study was the requirement to have worn glasses until visual acuity stability (or for 16 weeks) prior to randomization in the current study, rather than “for at least 4 weeks” in the prior study. Therefore the difference between the magnitudes of treatment effect in these studies might be attributable to the ongoing beneficial effect of optical treatment after enrollment in the earlier study.
In summary, we found no difference in amblyopic eye visual acuity improvement comparing children who performed common near activities and those who performed distance activities during patching. We therefore would not specifically recommend the prescription of common near activities for children undergoing patching for amblyopia. An additional finding was that many children with severe amblyopia (20/100 to 20/400), secondary to anisometropia, strabismus or both, have substantial improvement with 2 hours of patching per day (regardless of prescribed activities during patching). Therefore, 2 hours of patching per day is an option in the treatment of severe amblyopia.
Supplementary Material
This article contains additional online-only materials. The following should appear online-only: Table 2, Table 4, Figure 4, and the study group listing.
Acknowledgments
Funding/Support: Supported by National Eye Institute of National Institutes of Health, Department of Health and Human Services EY011751 (PEDIG)
Footnotes
Financial Disclosure: No conflicting relationships exist
Writing Committee: Lead authors: Jonathan M. Holmes BM, BCh; Don W. Lyon OD; Samara F. Strauber MS. Additional writing committee members (alphabetical): Eileen E. Birch PhD; Roy W. Beck MD, PhD; Yasmin S. Bradfield MD; Rhonda Hodde; Deborah L. Klimek MD; Dave H. Lee MD; B. Michele Melia, ScM; Erin R. Nosel OD; Michael X. Repka MD; Diane L. Tucker OD.
References
- 1.Francois J, James M. Comparative study of amblyopic treatment. Am Orthopt J. 1955;5:61–4. [PubMed] [Google Scholar]
- 2.Callahan WP, Berry D. The value of visual stimulation during contact and direct occlusion. Am Orthopt J. 1968;18:73–4. [PubMed] [Google Scholar]
- 3.von Noorden GK, Springer F, Romano P, Parks M. Home therapy for amblyopia. Am Orthopt J. 1970;20:46–50. [PubMed] [Google Scholar]
- 4.Watson PG, Sanac AS, Pickering MS. A comparison of various methods of treatment of amblyopia: a block study. Trans Ophthalmol Soc UK. 1985;104:319–28. [PubMed] [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–87. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–11. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 7.Pediatric Eye Disease Investigator Group. A randomized pilot study of near activities versus non-near activities during patching therapy for amblyopia. J AAPOS. 2005;9:129–36. doi: 10.1016/j.jaapos.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Pediatric Eye Disease Investigator Group. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113:895–903. doi: 10.1016/j.ophtha.2006.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes JM, Beck RW, Repka MX, et al. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 10.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article contains additional online-only materials. The following should appear online-only: Table 2, Table 4, Figure 4, and the study group listing.