Abstract
Background: Renal pelvis dilatation (RPD) occurs in 1% of fetuses. Severe RPD (>15 mm) is frequently associated with urinary tract pathology. For the majority with mild (5 to 9 mm) to moderate (10 to 15 mm) RPD, however, there is uncertainty about the risk of abnormalities and how much postnatal investigation is required.
Study design: Systematic review of cohort studies of fetuses with RPD ≤ 15 mm and metaregression to estimate risks of postnatal RPD, obstruction, and VUR.
Results: Of 506 potentially relevant papers, 18 met the inclusion criteria. Risk of postnatal RPD increased with fetal RP size and earlier gestation. Odds ratios for postnatal RPD doubled per millimeter increase in fetal RP size: At 20 wk gestation, for example, 18% of fetuses with mean RP of 6 mm were estimated to have persistent postnatal RPD, compared with 95% of fetuses with 12 mm RPD, but risks were decreased by 16% to 18% per week of presentation gestation. Estimated risks of obstruction and VUR were substantially lower, particularly in the mild group such as the 6 mm example above: obstruction 2%, VUR 4%.
Conclusions: Our novel risk estimates are useful for antenatal counseling at presentation. The low frequency of obstruction/VUR in mild RPD raises questions over the most appropriate investigation of these cases but further data are required before establishing definitive postnatal management pathways. We suggest the need for a large prospective multicenter study to collect individual patient parameters/results and search for additional prognostic indicators.
To screen, or not to screen, that is the question:
Whether ′tis nobler in the nephron to suffer The slings and arrows of outrageous infection, Or to weight obstruction against a sea of refluxes, And, by meds or surgery end them?
To flow, to reflux no more, and by clinical trial to say we end the loin-ache and thousand p-values that medicine is heir to, ‘tis evidence-based practice devoutly to be wish’d.
Routine fetal ultrasound has revolutionized management of pregnancies by improving accuracy of gestational age assessment and detection of fetal anomalies. These benefits come at a cost because some “abnormalities” are probably normal variants with minimal or uncertain clinical significance. Neveretheless, an abnormal finding can affect parental attitudes toward the pregnancy and their unborn baby (1–3) and lead to unnecessary postnatal investigations. Renal pelvis dilatation (RPD) is the most common organ-specific fetal condition detected antenatally (4) and one of the most difficult diagnostic challenges.
RPD occurs in approximately 1% of fetuses (range 0.6% to 4.3%; 4,5). The diagnosis is based on an increased anteroposterior RP size in mm, with variable ascertainment criteria between studies. Although fetal RPD > 15 mm is strongly associated with pathology such as urinary tract obstruction requiring postnatal treatment (8–12), lesser degrees of fetal RPD (≤15 mm) may resolve spontaneously by early infancy or have no adverse long-term sequelae (6,7). There is a lack of consensus among clinicians as to the management of these mildly or moderately affected fetuses. Some recommend ultrasound, micturating cysto-urethrogram (MCUG), and a renogram for all (i.e. using the same battery of invasive tests as one would utilize in more severe cases), whereas others limit invasive postnatal investigations to RPD above a certain size; for example, to fetuses with RP greater than 4 mm in the second trimester or 7 mm in the third trimester, or above the 95th percentile for gestational age (13–16).
One reason for the inconsistencies surrounding postnatal management of mild RPD is uncertainty about prognosis, because no previous study has separately reported prognostic information for fetuses with mild to moderate RPD. We undertook a systematic review and metaregression analysis of cohort studies that reported outcomes of fetal RPD, for fetuses with an RPD of ≤15 mm. The primary analyses were based on fetuses identified by routine fetal ultrasound screening (17–28). Secondary analyses evaluated studies that included pregnancies referred for specialist obstetric/fetal medicine reasons (29–34). To facilitate parental counseling during pregnancy and planning of postnatal investigations, we present estimated risks of postnatal RPD, obstruction, and vesicoureteric reflux (VUR) for fetuses with mild to moderate RPD.
Materials and Methods
Search Strategies
Studies that described the outcome of fetal RPD were identified from Medline (up to 2006) and Embase (1988 to 2005) by using the following search terms: antenatal, fetal, renal pelvis dilatation, pyelectasis, hydronephrosis, renal, and prognosis. Reference lists of included studies, review articles, nephrology textbooks, and proceedings of scientific meetings were also searched.
Inclusion Criteria
Two reviewers (DH, PW) independently reviewed titles and abstracts of all studies, and discrepancies were resolved by discussion. Studies were included if they prospectively followed children with fetal RP size ≤ 15 mm, and reported both gestation at antenatal diagnosis and postnatal RPD rates at any age. To avoid selection bias from referral of women with pregnancy complications, we based the primary analyses on cohorts of fetuses identified by routine antenatal ultrasound screening. We included studies that included referred pregnancies in secondary analyses.
Data Extraction
Data extraction was carried out independently by D.H. and P.W., and discrepancies were resolved by discussion. We extracted data on fetal RP size and gestational age. Most studies reported fetal RPD as a minimum size or value between two measurements, such as 4 to 7 mm or 7 to 10 mm. Both midpoint and minimum values were extracted for each subgroup, and data for fetuses with RP sizes > 15 mm were excluded where possible. Midpoint and minimum gestations were also extracted for the gestational age at diagnosis (18 to 24 wk, third trimester, etc.); subgroups with different gestations were extracted when here possible. Most studies reported the number of babies with fetal RPD and the number with RPD or renal complication postnatally, without reporting whether both kidneys were affected. Fewer studies reported results for individual kidneys. The major outcome was persistence of postnatal RPD within the first 6 wk after birth and/or by the end of each reported assessment period, as assessed by renal ultrasound and defined by individual studies. Other outcomes were detection of urinary tract obstruction or VUR, by MCUG or radioisotope studies.
Quality Assessment
Study quality assessment was based on the proportion of recruited children who were then investigated for postnatal RPD, obstruction, and VUR, and on whether the RP size for diagnosing postnatal RPD was reported.
Statistical Analysis
We report the probability of postnatal RPD according to the midpoint measurement of fetal RPD for each study population, or for subgroups defined by a specific RP range measured at a defined gestational age. The outcomes for all included study groups (routinely screened and referred) are shown according to the average gestational age at fetal ultrasound. Meta-regression analyses were confined to cohorts identified by routine antenatal screening. Missing outcomes were excluded from the denominator. We performed sensitivity analyses, using both minimum and mean values and assuming that all children with missing data either had the outcome (RPD, obstruction, or VUR; worst-case scenario), or did not (best-case scenario). RPD analyses were based on postnatal RPD outcome during the first 6 wk of life, as this corresponds to the initial assessment for most babies, and at the end of each study (i.e., the longest follow up reported). The presence of obstruction and VUR were analyzed wherever reported. We used hierarchical logistic regression models (35) to investigate the cross-study associations between outcomes and mean fetal RP size, taking into account mean gestational age (MLwin v2.00). Fitted estimates using second order penalized quasi-likelihood are presented, and these accorded well with those obtained using Markov chain Monte Carlo estimation. The estimated change in odds of each outcome after adjustment for within-study correlations per mm increase in fetal RP size are reported. The fitted models were used to generate estimates and confidence intervals (CIs) for the proportion of fetuses that developed postnatal RPD, VUR, or obstruction according to mean fetal RP size and gestational age. All estimates are presented with 95% CIs.
Results
Study Characteristics
Five hundred and six potentially relevant studies were identified, of which 18 met the inclusion criteria (17–34). Two studies reported overlapping patient cohorts but different outcomes (27,28). Subgroups were identified within studies when distinct cohorts were reported with different RP sizes or gestational ranges. Twelve of the included studies were based on fetuses identified by routine antenatal screening (17–28; Table 1) and six studies included fetuses referred for investigation (29–34; Table 2). Eighteen subgroups were identified in the studies on the basis of routinely screened pregnancies, 12 of which reported data for fetuses/children, and 6 of which reported outcomes per kidney. Fifteen subgroups were derived from referred cohorts (eight patient based and seven kidney).
Table 1.
Characteristics of studies based on fetal RPD identified by routine antenatal screeninga
| Study author and year | Gestational age at fetal RPD measurement | Cohort size | No. (%) assessed for postnatal outcomes
|
No. (%) of children with postnatal outcome/total with outcome measured
|
No. (%) of kidneys with postnatal outcome total with outcome measured
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Ultrasound for RPD• Renogram for obstruction •MCUG for VUR | RPD • Early (<6 wk) • End of study | Obstruction | VUR | RPD | Obstruction | VUR | |||
| Grignon et al. 1986 | 20 to 39 wk, mean 29 wk | 60 | 60 (100%) | Not stated | Not stated | Not stated | 17 (28%) | 1 (2%) | Not stated |
| 52 (87%) | Not stated | ||||||||
| 50 (83%) | |||||||||
| Rosendahl 1990 | 18 wk & 34 wk | 26 | 26 (100%) | 21 (81%) | Not stated | Not stated | 18 (75%) | Not stated | Not stated |
| not stated | 21 (81%) | ||||||||
| not stated | |||||||||
| Anderson et al. 1997 | 16 wk, mean 28 wk | 408 | 386 (95%) | 129 (33%) | Not stated | 38 (10%) | Not stated | Not stated | Not stated |
| 29 (7%) | 129 (33%) | ||||||||
| 94 (23%) | |||||||||
| Dremsek et al. 1997 | 22 to 30 wk, mean 26 wk | 30 | 30 (100%) | 9 (30%) | 2 (7%) | 1 (3%) | Not stated | Not stated | Not stated |
| 2 (7%) | 13.5 mo: | ||||||||
| 7 (23%) | 9 (30%) | ||||||||
| Dudley et al. 1997 | 14 to 18 wk, mean 25 wk | 100 | 100 (100%) | 64 (64%) | 5 (5%) | 28 (28%) | Not stated | Not stated | Not stated |
| 18 (18%) | 5.5 yr: | ||||||||
| 48 (48%) | 44 (44%) | ||||||||
| Jaswon et al. 1999c | 20 wk, mean 20 wk | 139 | 106 (76%) | 82 (77%) | 4 (4%) | 9 (8%) | Not stated | Not stated | Not stated |
| 63 (45%) | 18 mo: | ||||||||
| 125 (90%) | 60 (5 7%) | ||||||||
| Aviram et al. 2000b | 2nd & 3rd trimester | 56 | 56 (100%) | 39 (70%) | Not stated | 5 (9%) | 69 (78%) | 44 (49%) | Not stated |
| 34 (61%) | 39 (70%) | ||||||||
| 56 (100%) | |||||||||
| Kent et al. 2000b | 16 to 21 wk, mean 18 wk | 40 | 37 (93%) | 25 (68%) | 9 (24%) | 2 (5%) | Not stated | Not stated | Not stated |
| 15 (38%) | 6 mo: | ||||||||
| 18 (45%) | 17 (46%) | ||||||||
| Sairam et al. 2001b,c | 18 to 23 wk, mean 20 wk | 268 | 230 (86%) | 32 (14%) | 5 (2%) | 3 (1%) | Not stated | Not stated | Not stated |
| not stated | 77 (33%) | ||||||||
| not stated | |||||||||
| Gloor et al. 2002b | 2nd trimester, excluding resolution of RPD in 3rd trimester | 39 | 32 (82%) | 22 (69%) | Not stated | 5 (16%) | 44 (76%) | Not stated | Not stated |
| not stated | 22 (69%) | ||||||||
| 39 (100%) | |||||||||
| Ismaili et al. 2003b | 2nd & 3rd trimester, excluding RPD > 15 mm | 121 | 121 (100%) | Not stated | Not stated | Not stated | 35 (29%) | Not stated | Not stated |
| not stated | Not stated | ||||||||
| 121 (100%) | |||||||||
| Ismaili et al. 2004b | 2nd & 3rd trimester, excluding RPD > 15 mm | 258 | 213 (83%) | 177 (83%) | 27 (13%) | 23 (11%) | Not stated | Not stated | Not stated |
| not stated | 144 (68%) | ||||||||
| 258 (100%) | 144 (68%) | ||||||||
RPD, renal pelvis dilation; VUR, vesicoureteric reflux; MCUG, micturating cysto-urethrogram.
Authors stated that fetuses with anatomical or chromosomal abnormalities were excluded
Authors stated that terminations of pregnancy were excluded.
Table 2.
Characteristics of studies that included referred patientsa
| Study author and year | Gestational age at fetal RPD measurement | Cohort size | No. (%) assessed for postnatal outcomes
|
No. (%) of children with postnatal outcome
|
No. (%) of kidneys with postnatal outcome
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Ultrasound for RPD · Renogram for obstruction · MCUG for VUR | RPD · Early (<6 wk) · End of study | Obstruction | VUR | RPD | Obstruction | VUR | |||
| Johnson et al. 1992 | >20 wk, mean 30 wk | 47 | 47 (100%) | 17 (36%) | 10 (21%) | 4 (9%) | 8 (16%) | Not stated | Not stated |
| 27 (57%) | 5 yr: 17 (36%) | ||||||||
| 27 (57%) | |||||||||
| Langer et al. 1996 | Min 15 wk mean 21 wk, 33 wk | 95 | 89 (94%) | Not stated | Not stated | Not stated | Not stated | Not stated | Not stated |
| not stated | 19 (21%) | ||||||||
| not stated | |||||||||
| Kitagawa et al. 1998b | Min 17 wk, mean 19 wk, 25 wk, 35 wk | 65 | 65 (100%) | Not stated | 2 (3%) | 2 (3%) | Not stated | Not stated | Not stated |
| not stated | 3 yr: 43 (66%) | ||||||||
| not stated | |||||||||
| Liang et al. 2002b | 33 wk, mean 33 wk | 18 | 18 (100%) | 16 (89%) | 4 (19%) | 0 (0%) | 12 (57%) | Not stated | 0 (0%) |
| 7 (39%) | 6 yr: 9 (50%) | ||||||||
| 16 (89%) | |||||||||
| Aksu et al. 2005 | Min 20 wk, mean 33 wk (5 to 9 mm, 10 to 14 mm) | 156 | 156 (100%) | Not stated | Not stated | Not stated | 5 to 9 mm: 57 (68%) 10 to 14 mm: 75 (78%) | 107 (55%) | 24 (12%) |
| not stated | Not stated | ||||||||
| 156 (100%) | |||||||||
| Gramellini et al. 2006b | Min 19 wk, mean 23 wk | 133 | 133 (100%) | Not stated | Not stated | Not stated | 69 (52%) | 9 (7%) | 16 (12%) |
| not stated | Not stated | ||||||||
| 133 (100%) | |||||||||
RPD, renal pelvis dilation; VUR, vesicoureteric reflux; MCUG, micturating cysto-urethrogram.
Authors stated that fetuses with anatomical or chromosomal abnormalities were excluded.
Half of the studies reported including fetuses with a minimum RP size of 4 mm (19,24–27,29–31). Other studies did not state the minimum RP measure. Most studies measured fetal RP size at approximately 20 wk of gestation, corresponding to the timing of routine second trimester anomaly scan. The earliest reported fetal ultrasound was at 14 wk of gestation (21). Most studies reported that postnatal scans were not performed within 2 d after birth(17,20,22,23,27–31), which may be important because newborns are initially oliguric and false-negative results are common at this time: 4 studies did not specify the earliest age at postnatal ultrasound assessment(18,29,30,33).
Study Quality
Completeness of follow up for RPD was similar for studies based on routinely screened fetuses and those bases on referred fetuses, and ranged from 76% to 100%. Three studies lacked information on completeness of postnatal RP size assessment. Only six reported the postnatal RP size that was used to diagnose postnatal RPD: ≥5 mm was used in two routinely screened cohorts(20,24) and one referred cohort (33); ≥7 mm was used in two routinely screened cohorts (27,28), and Dudley et al. reported results for multiple categories (5 to 9 mm; 10 to 14 mm; 15 to 19 mm, and >19 mm) (21). These differences raise the possibility that some “persistent” RPD cases may have been considered normal (i.e. resolved) in other centers.
Completeness of follow up was variable for obstruction and VUR (Tables 1 and 2). Between 7% and 86% of the study cohort were assessed for obstruction by radioisotope studies and 9 studies (five routinely screened, four referred) did not give figures. Five of the cohorts based on routine antenatal screening (19,23,26 to 28) and three based on referred pregnancies (31,33,34) reported VUR assessment by MCUG in all patients.
Prevalence of Postnatal RPD, Obstructive Nephropathy, and VUR
Results for Patients.
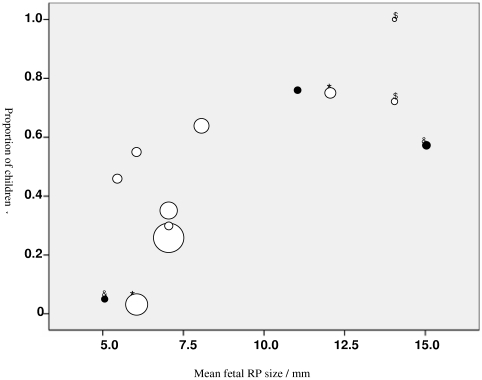
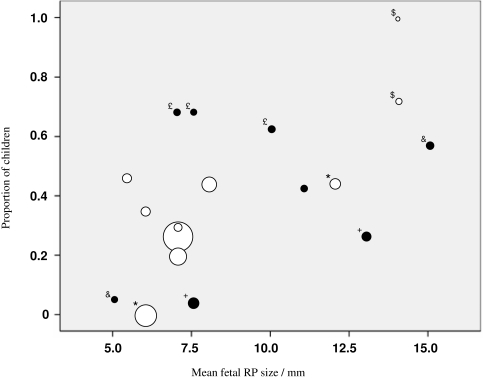
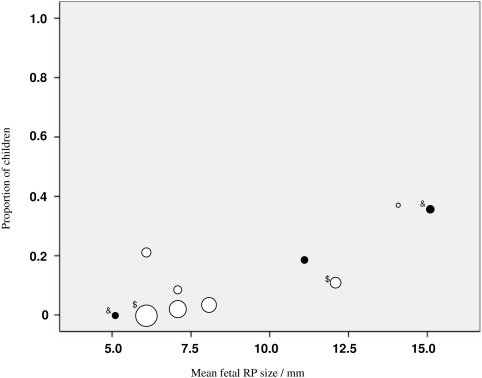
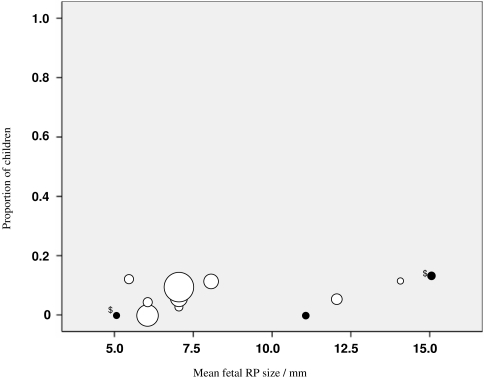
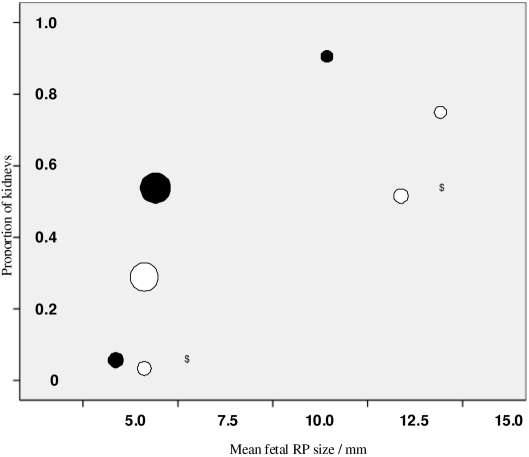
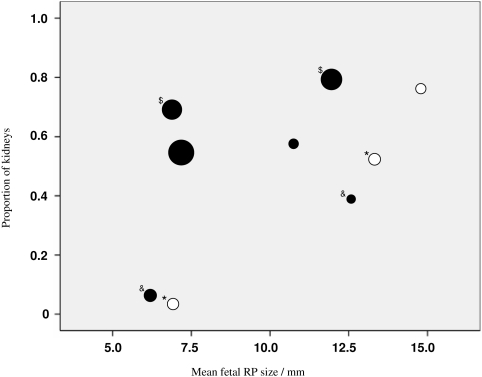
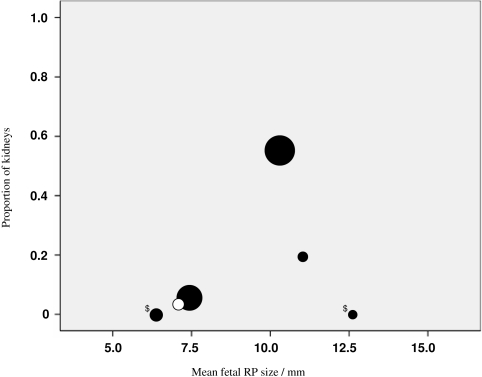
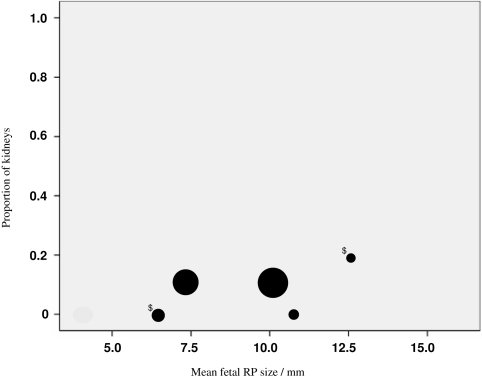
The risk of postnatal RPD increased with mean fetal RP size. This association was consistent whether postnatal RP size was measured before 6 wk of age or at the end of follow up (Figures 1 and 2). The odds of postnatal RPD more than doubled for each mm increase in mean fetal RP size: For routinely screened cohorts, the odds ratio (adjusted for gestational age at fetal ultrasound) was 2.03 (95% CI 1.71 to 2.42) for RPD measured by 6 wk after birth and 2.12 (95% CI 1.65 to 2.72) for RPD measured over the whole study. Results were similar for referred cohorts, and in sensitivity analyses using minimum instead of mean values for fetal RP size and gestational age. The risk of postnatal RPD for a given fetal RP size decreased by 16% to 18% for every week later in pregnancy. The odds of obstruction or VUR increased with each mm increase in fetal RP size: odds ratio for obstruction 1.56 (95% CI 1.21 to 2.01), and for VUR 1.25 (95% CI 0.99 to 1.59) (Figures 3 and 4).
Figure 1.
Proportion of children diagnosed with RPD by 6 weeks of age. Unfilled circles represent routine studies whereas filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size. S, * and & represent sub-groups within the same studies.
Figure 2.
Proportion of children diagnosed with RPD at the end of each study. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size. $, *, &, £, and + represent subgroups within the same studies.
Figure 3.
Proportion of children diagnosed with obstruction. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size. $ and & represent subgroups within the same studies.
Figure 4.
Proportion of children diagnosed with vesicoureteric reflux (VUR). Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size. $ and & represent subgroups within the same study.
Table 3 demonstrates fitted estimates from these models with the associated 95% CIs. For example, with a mean fetal RPD size of 6 mm at 20 wk, 31% of babies would be expected to have postnatal RPD by 6 wk of age (95% CI:14, 54). This proportion increases with fetal RP size at the same gestational age but decreases with the same fetal RP size at later gestational ages. For example, a fetal RP size of 7 mm at 28 wk is associated with lower rates of persistence (15% at 6 wk; 5,35) compared with the same measurement at 20 wk (47%; 25,71). The regression equations for cohorts based on routinely screened fetuses are shown in the Table 3 legend.
Table 3.
Estimated risk of postnatal RPD, obstruction, or VUR according to RP size and gestational age at diagnosisa
| Gestation | 20 wk, 6 mm | 20 wk, 7 mm | 20 wk, 12 mm | 25 wk, 8 mm | 28 wk, 7 mm | 34 wk, 14 mm |
|---|---|---|---|---|---|---|
| Size | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) |
| Postnatal RPD at 6 wk | 31% | 47% | 97% | 40% | 15% | 88% |
| (14 to 54) | (25 to 71) | (89 to 99) | (22 to 60) | (5 to 35) | (52 to 98) | |
| Postnatal RPD at study end | 18% | 31% | 95% (77 to 99) | 29% | 10% (3,33) | 89% |
| (5 to 44) | (11 to 62) | (12 to 55) | (40 to 99) | |||
| Obstruction | 2% | 4% | 26% | 4% | * | * |
| (1, 9) | (1, 12) | (9, 57) | (1, 20) | |||
| VUR | 4% | 5% | 15% | 6% | 5% | 18% |
| (2 to 10) | (2 to 12) | (4 to 45) | (3 to 11) | (2 to 12) | (4 to 55) |
Fitted estimates of patient-based data from unselected groups were generated from the following equations:
a) Odds of persistent RPD within first 6 wk = 0.37 × (2.03)RP size × (0.82)gestation
b) Odds of persistent RPD at the end of study = 0.07 × (2.12)RP size × (0.84)gestation
c) Odds of obstruction = 0.01 × (1.56)RP size × (0.92)gestation
d) Odds of VUR = 0.01 × (1.25)RP size × (0.99)gestation
Note: These are estimated equations and estimates must be viewed with caution because of potential for uncontrolled confounding within meta-analyses.
There were no studies with values for obstruction after 26 wk so it was not possible to generate statistically robust estimates at the 28- and 34-wk stages.
RPD, renal pelvis dilation; VUR, vesicoureteric reflux; MCUG, micturating cysto-urethrogram; CI, confidence interval.
Results Reported for Each Kidney.
Fetal RP size was associated with an increased risk of postnatal RPD (i.e. similar to results for patient-based studies), but there were fewer studies and smaller numbers in the subgroups (Figures 5 and 6). There was only one routine study that reported kidney-based data for obstruction and none for VUR, which prevented statistical analysis of results in routine versus selected studies, although risks did again appear higher as RP size increased (Figures 7 and 8).
Figure 5.
Proportion of kidneys diagnosed with renal pelvis dilation (RPD) by 6 wk of age. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size for all the kidney data. $ represents subgroups within the same study.
Figure 6.
Proportion of kidneys diagnosed with RPD at end of each study. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size for all kidney data. $, *, and & represent subgroups within the same studies.
Figure 7.
Proportion of kidneys diagnosed with obstruction. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size for all the kidney data. $ represents subgroups within the same study.
Figure 8.
Proportion of kidneys diagnosed with VUR. Unfilled circles represent routine studies, and filled (black) circles represent cohorts that included referred patients. Area of circles is proportional to group sample size for all the kidney data. $ represents the subgroups within the same study.
Discussion
RPD presents a common clinical dilemma. Of the 1% of fetuses diagnosed with RPD, the majority have mild-to-moderate dilatation, yet there is little consensus on optimal postnatal investigations and management. In our unique study of mild-to-moderate RPD, we found that the risk of postnatal RPD and obstruction/VUR increased as the mean fetal RP increased from 5 to 15 mm. For a given measure of fetal RP, the risk of postnatal RPD decreased with gestational age at presentation. These findings should assist parental counseling at the time of antenatal diagnosis and should influence decisions on postnatal investigation.
Many individual studies have attempted to define criteria for “safe,” nonpathologic fetal RPD. Important determinants are size and gestation (Table 3). The latter is unsurprising because fetal RP size increases with gestational age in an almost linear fashion, with the 50th centile being at approximately 4 mm at 20 wk and 7 mm at term (16). Hence, analyses must take into account the gestational age at fetal ultrasound measurement of RP size, and corrections for gestation should be included in analyses, as we have done with our risk estimates. Similar age-specific measurement criteria may need to be applied to postnatal assessment of RPD, because we detected lower RPD rates at later time points (i.e. end of studies) compared with the first, 6-wk analysis. This may reflect resolution of dilation as the infant grows older, but we lacked sufficient time points to investigate this possibility.
Our results are broadly supported by two other systematic reviews/meta-analyses that recently reported on all grades of fetal RPD (i.e. mild to severe), including alternative grading systems, and considered alternative end-points including specific pathologies (11,12). Sidhu et al. generated odds ratio for the likelihood of RPD resolving postnatally on the basis of data from three studies (11). Lee et al. reported differences across 13 studies that reported outcomes for mild-to-moderate RPD but without consideration of presentation gestational age in their final analyses. In addition, they included three studies that reported a minimum RP size used to diagnose RPD but gave no indication of the maximum antenatal RP size within those patient cohorts (12). In spite of these differences, they both linked larger RP size with worse outcome, but they did not generate risk estimates for the clinically contentious mild-to-moderate group: Sidhu et al. concluded that lesser degrees of pelvic dilation were more likely to stabilize or improve (11), whereas Lee et al. stressed the significant risk of postnatal pathology in moderate and severe cases (12).
A weakness of all meta-regression analyses, ours included, is that the results are based on aggregate data, a method which assumes that associations observed between group-level variables are applicable for individuals. This may not always hold true (the “ecological fallacy”) (36–38). Avoiding this possibility would require meta-analysis of individual patient data, using raw data sets from previous studies. Other potential weaknesses of such studies relate to both collection and description of clinical data within the individual studies included. For example, lack of uniformity and consistent reporting between papers prevented analysis of potentially important clinical features. We would like to have seen information on changes in fetal RP size during the pregnancy, but reporting was inconsistent, and some studies actually excluded fetuses in whom RPD resolved before birth, which biases their results toward worse outcomes (23,24,26–28), and few mentioned details such as calyceal dilation, which has been reported to be useful indicators of poorer prognosis (8). Timing of initial postnatal ultrasound may also be critical as babies become relatively dehydrated and oliguric for the first 48 h postnatally (39), but several studies did not mention excluding measurements during this period (18,29,30,33). Differences in measurement and interpretation of outcomes also varied. Only six studies defined their diagnostic criteria for postnatal RPD, and many regarded 5 to 6 mm as normal, whereas others recorded this as persistent RPD, which would bias the latter toward negative outcomes. Indications for assessment of obstruction and VUR were also unclear. This may be indicative of an absence of universally agreed on clinically important outcome measures that can be applied to all patients to define their risk of significant disease. Selective assessment may introduce bias because the investigated group may have other factors associated with poorer prognosis that prompted investigation. When everyone is assessed, however, one may detect a higher proportion of ′pathology’ but this raises the question of whether the increased numbers of milder abnormalities detected are clinically important.
It is clear that severe fetal RPD > 15 mm is frequently associated with obstructive uropathy (29,42), although Ransley et al. and colleagues suggest that surgery is needed only in fetal RP size > 12 mm (43,44). However, clinical significance is less certain for mild-to-moderate fetal RPD: In earlier studies, Dicke et al. concluded that only 10% of fetuses with RP size ≤ 10 mm had an obstructive process (15), whereas Gramellini's report included in this meta-analysis suggested that an 11-mm cut-off had the greatest diagnostic accuracy (93%) in the second trimester for defining those that needed surgery, with a positive predictive value of 87% and a sensitivity of up to 70%. Our meta-analysis data show that it is rare to make a diagnosis of obstruction in mild-to- moderate RPD, but risk rises significantly with fetal RP size. This association remains significant after adjusting for incomplete data (i.e. losses to follow up and investigation) using best/worst case sensitivity analyses. Even when obstruction was diagnosed in mild RPD, surgery was still not required in a high proportion of patients. For example, Ismaili et al. reported 27 patients with pelvicoureteric junction obstruction after antenatal screening of mild RPD. Only two patients required surgery; in the remainder, dilation remainder stable (n = 9) or diminished after 2 yr of follow up (n = 16) (28). It follows that in the absence of long-term follow-up data, the clinical importance of diagnosing obstruction in this mild RPD group and appropriate management remain unclear.
There is growing evidence for the low sensitivity and poor predictive value of fetal RP size in predicting the presence and severit of VUR (45,46). We analyzed VUR as a secondary outcome (which may bias study selection) and report a nonsignificant correlation between increasing fetal RP size and postnatal VUR, with VUR rates of approximately 4% to 6% in the mild group and up to 18% in the moderate, third trimester group. This finding is similar to the meta-analysis of Lee et al. that described increased VUR from 4.4% to 10.8% in mild versus moderate fetal RPD (12), but it contradicts the report by McIlroy et al. describing clustering of VUR with mild fetal RPD (47). In contrast, several studies including two herein, have reported a finding of VUR in children with fetal RPD that resolved postnatally (21,22). The overriding concern for patients with VUR is the development of renal scarring. Plant et al. demonstrated that scarring rates among children with 5 to 15 mm fetal RPD were not significantly different from those of the general population (48). Furthermore, VUR has been demonstrated to be only a weak predictor of renal damage in pediatric patients hospitalized with UTI (49). It has been postulated that there are two types of VUR in fetal RPD: mild reflux associated with normal kidneys, usually affecting females, and severe congenital reflux predominantly in males, which results in scarring in utero (50). It is the latter that we endeavor to detect with antenatal screening for antenatal renal pelvis dilatation (ARPD), but what remains unclear is whether earlier detection will attenuate congenital VUR related morbidity.
Taking all these data together, we question whether the pursuit of a diagnosis of obstruction or VUR through invasive investigations is justified in mild fetal RPD because our analyses and others suggest that the likelihood of detecting clinically significant pathology is low, even bearing in mind potential confounders and limitations inherent in this and other meta-analyses. Instead, we raise the possibility that it is worth considering a less invasive approach involving monitoring with ultrasound alone unless there are other features of complex disease. A key objective in future RPD studies might therefore be to identify indicators that distinguish patients with significant disease, which might include progression during gestation, calyceal dilation, bladder abnormalities, other clinical features, or family history. A less aggressive approach is supported by a recent study focusing on mild RPD in a Brazilian population (40), and mirrors the approach mandated in the latest United Kingdom National Institute for Clinical Excellence guidelines for assessment of urinary tract infections in children (41).
Conclusion
We estimated risk ratios for fetuses with mild-to-moderate RPD for the outcomes of persistent postnatal RPD, obstruction, and VUR on the basis of meta-regression of grouped data. These novel results should facilitate more accurate counseling of parents of fetuses with RPD when they present in utero. Further data are required before establishing definitive postnatal management pathways on the basis of RP size alone, and we suggest the need for a large multicenter study that could also consider factors such as progression of RPD and calyceal dilation. In the meantime, we face a clinical dilemma regarding acceptable levels of risk. Without conclusive evidence, it is up to physicians and parents to discuss the consequences of potential over- and under-investigation.
Disclosures
None.
Acknowledgments
None.
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Filly RA: Obstetrical sonography: The best way to terrify a pregnant woman. J. Ultrasound Med 19: 1–5, 2000 [DOI] [PubMed] [Google Scholar]
- 2.Kleinveld JH, Timmermans DR, de Smit DJ, Ader HJ, van der WG, ten Kate LP: Does prenatal screening influence anxiety levels of pregnant women? A longitudinal randomised controlled trial. Prenat Diagn 26: 354–361, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Marteau TM, Kidd J, Cook R, Michie S, Johnston M, Slack J, Shaw RW: The psychological effects of false-positive results in prenatal screening for fetal abnormality: A prospective study. Prenat Diagn 12: 205–214, 1992 [DOI] [PubMed] [Google Scholar]
- 4.Chudleigh T: Mild pyelectasis. Prenat Diagn 21: 936–941, 2001 [PubMed] [Google Scholar]
- 5.Livera LN, Brookfield DS, Egginton JA, Hawnaur JM: Antenatal ultrasonography to detect fetal renal abnormalities: A prospective screening programme. BMJ 298: 1421–1423, 1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farhat W, McLorie G, Geary D, Capolicchio G, Bägli D, Merguerian P, Khoury A: The natural history of neonatal vesicoureteral reflux associated with antenatal hydronephrosis. J. Urol 164: 1057–1060, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Morin L, Cendron M, Crombleholme TM, Garmel SH, Klauber GT, D'Alton ME: Minimal hydronephrosis in the fetus: Clinical significance and implications for management. J. Urol 155: 2047–2049, 1996 [DOI] [PubMed] [Google Scholar]
- 8.Fernbach SK, Maizels M, Conway JJ: Ultrasound grading of hydronephrosis: Introduction to the system used by the Society for Fetal Urology. Pediatr Radiol 23: 478–480, 1993 [DOI] [PubMed] [Google Scholar]
- 9.Anderson N, Clautice-Engle T, Allan R, Abbott G, Wells JE: Detection of obstructive uropathy in the fetus: predictive value of sonographic measurements of renal pelvic diameter at various gestational ages. Am J Roentgenol 164: 719–723, 1995 [DOI] [PubMed] [Google Scholar]
- 10.Odibo AO, Raab E, Elovitz M, Merrill JD, Macones GA: Prenatal mild pyelectasis: Evaluating the thresholds of renal pelvic diameter associated with normal postnatal renal function. J Ultrasound Med 23: 513–517, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Sidhu G, Beyene J, Rosenblum ND: Outcome of isolated antenatal hydronephrosis: A systematic review and meta-analysis. Pediatr Nephrol 21: 218–224, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Lee RS, Cendron M, Kinnamon DD, Nguyen HT: Antenatal hydronephrosis as a predictor of postnatal outcome: A meta-analysis. Pediatrics 118: 586–593, 2006 [DOI] [PubMed] [Google Scholar]
- 13.Odibo AO, Marchiano D, Quinones JN, Riesch D, Egan JF, Macones GA: Mild pyelectasis: Evaluating the relationship between gestational age and renal pelvic anterior-posterior diameter. Prenat Diagn 23: 824–827, 2003 [DOI] [PubMed] [Google Scholar]
- 14.Corteville JE, Gray DL, Crane JP: Congenital hydronephrosis: Correlation of fetal ultrasonographic findings with infant outcome. Am J Obstet Gynecol 165: 384–388, 1991 [DOI] [PubMed] [Google Scholar]
- 15.Dicke JM, Blanco VM, Yan Y, Coplen DE: The type and frequency of fetal renal disorders and management of renal pelvis dilatation. J Ultrasound Med 25: 973–977, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Chitty LS, Altman DG: Charts of fetal size: Kidney and renal pelvis measurements. Prenat Diagn 23: 891–897, 2003 [DOI] [PubMed] [Google Scholar]
- 17.Grignon A, Filion R, Filiatrault D, Robitaille P, Homsy Y, Boutin H, Leblond R: Urinary tract dilatation in utero: Classification and clinical applications. Radiology 160: 645–647, 1986 [DOI] [PubMed] [Google Scholar]
- 18.Rosendahl H: Ultrasound screening for fetal urinary tract malformations: A prospective study in general population. Eur J Obstet Gynecol Reprod Biol 36: 27–33, 1990 [DOI] [PubMed] [Google Scholar]
- 19.Anderson NG, Abbott GD, Mogridge N, Allan RB, Maling TM, Wells JE: Vesicoureteric reflux in the newborn: Relationship to fetal renal pelvic diameter. Pediatr Nephrol 11: 610–616, 1997 [DOI] [PubMed] [Google Scholar]
- 20.Dremsek PA, Gindl K, Voitl P, Strobl R, Hafner E, Geissler W, Hruby W, Sacher M: Renal pyelectasis in fetuses and neonates: Diagnostic value of renal pelvis diameter in pre- and postnatal sonographic screening. Am J Roentgenol 168: 1017–1019, 1997 [DOI] [PubMed] [Google Scholar]
- 21.Dudley JA, Haworth JM, McGraw ME, Frank JD, Tizard EJ: Clinical relevance and implications of antenatal hydronephrosis. Arch Dis Child Fetal Neonatal Ed 76: F31–F34, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jaswon MS, Dibble L, Puri S, Davis J, Young J, Dave R, Morgan H: Prospective study of outcome in antenatally diagnosed renal pelvis dilatation. Arch Dis Child Fetal Neonatal Ed 80: F135–F138, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aviram R, Pomeranz A, Sharony R, Beyth Y, Rathaus V, Tepper R: The increase of renal pelvis dilatation in the fetus and its significance. Ultrasound Obstet Gynecol 16: 60–62, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Kent A, Cox D, Downey P, James SL: A study of mild fetal pyelectasia - Outcome and proposed strategy of management. Prenat Diagn 20: 206–209, 2000 [PubMed] [Google Scholar]
- 25.Sairam S, Al Habib A, Sasson S, Thilaganathan B: Natural history of fetal hydronephrosis diagnosed on mid-trimester ultrasound. Ultrasound Obstet Gynecol 17: 191–196, 2001 [DOI] [PubMed] [Google Scholar]
- 26.Gloor JM, Ramsey PS, Ogburn PL, Jr., Danilenko-Dixon DR, DiMarco CS, Ramin KD: The association of isolated mild fetal hydronephrosis with postnatal vesicoureteral reflux. J Matern Fetal Neonatal Med 12: 196–200, 2002 [DOI] [PubMed] [Google Scholar]
- 27.Ismaili K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE: Results of systematic screening for minor degrees of fetal renal pelvis dilatation in an unselected population. Am J Obstet Gynecol 188: 242–246, 2003 [DOI] [PubMed] [Google Scholar]
- 28.Ismaili K, Avni FE, Wissing KM, Hall M: Long-term clinical outcome of infants with mild and moderate fetal pyelectasis: Validation of neonatal ultrasound as a screening tool to detect significant nephrouropathies. J Pediatr 144: 759–765, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Johnson CE, Elder JS, Judge NE, Adeeb FN, Grisoni ER, Fattlar DC: The accuracy of antenatal ultrasonography in identifying renal abnormalities. Am J Dis Child 146: 1181–1184, 1992 [DOI] [PubMed] [Google Scholar]
- 30.Langer B, Simeoni U, Montoya Y, Casanova R, Schlaeder G: Antenatal diagnosis of upper urinary tract dilation by ultrasonography. Fetal Diagn Ther 11: 191–198, 1996 [DOI] [PubMed] [Google Scholar]
- 31.Kitagawa H, Pringle KC, Stone P, Flower J, Murakami N, Robinson R: Postnatal follow-up of hydronephrosis detected by prenatal ultrasound: The natural history. Fetal Diagn Ther 13: 19–25, 1998 [DOI] [PubMed] [Google Scholar]
- 32.Liang CC, Cheng PJ, Lin CJ, Chen HW, Chao AS, Chang SD: Outcome of prenatally diagnosed fetal hydronephrosis. J Reprod Med 47: 27–32, 2002 [PubMed] [Google Scholar]
- 33.Aksu N, Yavaşcan O, Kangin M, Kara OD, Aydin Y, Erdoğan H, Tuncel TC, Cetinkaya E, Ozbay E, Sandikçioğlu TG: Postnatal management of infants with antenatally detected hydronephrosis. Pediatr Nephrol 20: 1253–1259, 2005 [DOI] [PubMed] [Google Scholar]
- 34.Gramellini D, Fieni S, Caforio E, Benassi G, Bedocchi L, Beseghi U et al.: Diagnostic accuracy of fetal renal pelvis anteroposterior diameter as a predictor of significant postnatal nephrouropathy: second versus third trimester of pregnancy. Am J ObstetGynecol 194: 167–173, 2006 [DOI] [PubMed] [Google Scholar]
- 35.Brown H, Prescott R: Applied Mixed Models in Medicine, 1st Ed., Hoboken, NJ, John Wiley & Sons, 1999
- 36.Simmonds MC, Higgins JP, Stewart LA, Tierney JF, Clarke MJ, Thompson SG: Meta-analysis of individual patient data from randomized trials: A review of methods used in practice. Clin Trials 2: 209–217, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Lambert PC, Sutton AJ, Abrams KR, Jones DR: A comparison of summary patient-level covariates in meta-regression with individual patient data meta-analysis. J Clin Epidemiol 55: 86–94, 2002 [DOI] [PubMed] [Google Scholar]
- 38.Teramukai S, Matsuyama Y, Mizuno S, Sakamoto J: Individual patient-level and study-level meta-analysis for investigating modifiers of treatment effect. Jpn J Clin Oncol 34: 717–721, 2004 [DOI] [PubMed] [Google Scholar]
- 39.Laing FC, Burke VD, Wing VW, Jeffrey RB, Jr., Hashimoto B: Postpartum evaluation of fetal hydronephrosis: Optimal timing for follow-up sonography. Radiology 152: 423–424, 1984 [DOI] [PubMed] [Google Scholar]
- 40.Coelho GM, Bouzada MC, Pereira AK, Figueiredo BF, Leite MR, Oliveira DS, Oliveira EA: Outcome of isolated antenatal hydronephrosis: A prospective cohort study. Pediatr Nephrol 22: 1727–1734, 2007 [DOI] [PubMed] [Google Scholar]
- 41.Urinary tract infection in children: diagnosis, treatment and long-term management. National Institute for Health and Clinical Excellence. 2007. http://guidance.nice.org.uk/CG54 [PubMed]
- 42.Coplen DE, Austin PF, Yan Y, Blanco VM, Dicke JM: The magnitude of fetal renal pelvic dilatation can identify obstructive postnatal hydronephrosis, and direct postnatal evaluation and management. J Urol 176: 724–727, 2006 [DOI] [PubMed] [Google Scholar]
- 43.Ransley PG, Dhillon HK, Gordon I, Duffy PG, Dillon MJ, Barratt TM: The postnatal management of hydronephrosis diagnosed by prenatal ultrasound. J Urol 144: 584–587, 1990 [DOI] [PubMed] [Google Scholar]
- 44.Dhillon HK: Prenatally diagnosed hydronephrosis: The Great Ormond Street experience. Br J Urol 81 [Suppl 2]: 39–44, 1998 [DOI] [PubMed] [Google Scholar]
- 45.Anderson NG, Wright S, Abbott GD, Wells JE, Mogridge N: Fetal renal pelvic dilatation–Poor predictor of familial vesicoureteral reflux. Pediatr Nephrol 18: 902–905, 2003 [DOI] [PubMed] [Google Scholar]
- 46.Phan V, Traubici J, Hershenfield B, Stephens D, Rosenblum ND, Geary DF: Vesicoureteral reflux in infants with isolated antenatal hydronephrosis. Pediatr Nephrol 18: 1224–1228, 2003 [DOI] [PubMed] [Google Scholar]
- 47.McIlroy PJ, Abbott GD, Anderson NG, Turner JG, Mogridge N, Wells JE: Outcome of primary vesicoureteric reflux detected following fetal renal pelvic dilatation. J Paediatr Child Health 36: 569–573, 2000 [DOI] [PubMed] [Google Scholar]
- 48.Plant ND, Hornung RJ, Coulthard MG, Keir MJ, Matthews JN, Robson SC: Does antenatal pelvic dilation predict renal scarring? Arch Dis Child Fetal Neonatal Ed 90: F339–F340, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gordon I, Barkovics M, Pindoria S, Cole TJ, Woolf AS: Primary vesicoureteric reflux as a predictor of renal damage in children hospitalized with urinary tract infection: A systematic review and meta-analysis. J Am Soc Nephrol 14: 739–744, 2003 [DOI] [PubMed] [Google Scholar]
- 50.Yeung CK, Godley ML, Dhillon HK, Gordon I, Duffy PG, Ransley PG: The characteristics of primary vesico-ureteric reflux in male and female infants with pre-natal hydronephrosis. Br J Urol 80: 319–327, 1997 [DOI] [PubMed] [Google Scholar]