Abstract
Rate of acceptance of deceased-donor kidneys decreases with donor age despite the growing number of aged transplant candidates on the waiting list. In the Eurotransplant Senior Program, HLA-unmatched kidneys from deceased donors aged ≥65 yr are transplanted regionally into recipients aged ≥65 yr. Because we have become more willing to accept kidneys from donors aged ≥75 yr than previous years, we performed a retrospective analysis of this subgroup. Kidneys were accepted from donors aged ≥75 yr provided a normal creatinine on admission to the hospital, a Cockcroft-Gault creatinine clearance >80 ml/min, and an absence of comorbidities. We compared outcomes of kidneys from donors aged ≥75 yr with both younger-donor kidneys transplanted in the Eurotransplant Senior Program and with younger-donor HLA-matched kidneys transplanted into recipients ≥60 yr. There were no differences in 5-yr graft and patient survival or rate of delayed graft function between groups. Graft function, measured by creatinine and creatinine clearance, differed without pattern at only three of 12 time points during 5 yr of follow-up. In conclusion, our data suggest that kidneys from deceased donors aged ≥75 yr can be transplanted safely into recipients aged ≥65 yr if similar donor criteria and local allocation practices are used.
Kidney transplantations (KTX) are beneficial also for old recipients.1,2 Because the number of aged kidney donors is constantly rising3,4 and donor shortage is the limiting factor for a timely transplant, Eurotransplant initiated the Eurotransplant Senior Program (ESP) in 1999. In this program, kidneys from deceased donors aged ≥65 are allocated according to waiting time and blood group compatibility without HLA matching to recipients ≥65. Because susceptibility to damage through cold ischemic time increases with donor age, transport time is kept short by local allocation.5,6 Donors of the age of the ESP are defined as expanded criteria donors (ECD), and kidneys were found to have a 1.7 times higher risk for graft failure compared with normal donors, and >50% of kidneys from deceased donors aged ≥60 are discarded in the United States.7,8 Discarding these donor kidneys is despite an increasing number of old patients on the waiting list9 and the findings of some authors who could show that kidneys refused because of donor age were successfully transplanted in other centers. Also, ECD kidneys were transplanted successfully into recipients aged ≥40.10,11
Our department has taken part in the ESP since its start in 1999.12 Our center criteria for acceptance of kidneys from ESP donors include absence of comorbidities (uncontrolled arterial hypertension, diabetes, proteinuria), creatinine on admission to the hospital in the normal range, and creatinine clearance (Cockcroft-Gault) of >80 ml/min. Because we observed an increasing number of donors aged ≥75 accepted into this program and because no publication on this subgroup of “very old for old” KTX exists, we performed a retrospective, single-center analysis.
During the studied period, kidneys from 48 deceased donors aged ≥75 yr were allocated locally to our center by Eurotransplant (mean number of offers per year 5.3 [0 to 12]). Fifteen (31%) donors fulfilled the inclusion criteria. We transplanted 18 kidneys into 18 recipients aged ≥65 yr (study group [“very old for old”]). Control group 1 were recipients in the ESP who received donor kidneys aged 65 to 74 yr (“old for old”; n = 73), control group 2 were recipients who were ≥60 and received a kidney from a donor in the usually applied Eurotransplant kidney allocation system (ETKAS), which also includes HLA matching (“ETKAS for old”; n = 30).
The surgical technique was extraperitoneal with intermittent ureteral stenting of the antirefluxive ureteral implantation, immunosuppression consisted of a standardized triple therapy (calcineurin inhibitor, mycophenolate mofetil, corticosteroids) with dosage reduction over time. Selected patients received an induction therapy with an IL receptor antibody. Rejections were treated by pulsed methylprednisolone bolus therapy, followed by conversion to tacrolimus and/or treatment with ATG in steroid-resistant cases. Delayed graft function (DGF) was defined as the need for dialysis in the first week after KTX. Data for the study were retrieved from our computer database, which stores all patient data, including the follow-up visits, in an electronic patient record system.
For demographic data, see Table 1. Moderate or severe donor atherosclerosis was found in 73% of the study group, in 45% of control group 1 (NS), and in 11% of control group 2 (P < 0.05). Recipient atherosclerosis was not different between the study group and control group 1 (50 versus 48%) but was lower in control group 2 (19%; P < 0.05). No significant difference in anastomosis time was found (48 versus 53 versus 44 min). Median cold ischemic time (CIT) was 9.9 h (4.0 to 17.0) for the study group, 7.7 h (4.0 to 23.0) for control group 1 (NS), and 14.5 h (4.5 to 27.0) for the control group 2 (P < 0.05). DGF did not differ between study and control groups (33 versus 36 versus 43%) as did rejections (17 versus 34 versus 30%; NS) and peri- and postoperative complications. Median hospital stay was significantly shorter for the study group (18 d) compared with control groups (control 1: 2; control 2: 28).
Table 1.
Demographic data
| Demographic | Very Old for Old(n = 18) | Old for Old(n = 73) | P | ETKAS for Old(n = 30) | P |
|---|---|---|---|---|---|
| Recipient age (median [range]) | 68 (65 to 74) | 66 (65 to 77) | <0.05 | 63 (60 to 70) | <0.05 |
| Donor age (median [range]) | 78 (75 to 88) | 68 (65 to 74) | <0.05 | 48 (15 to 63) | <0.05 |
| HLA-A/-B/-DR mismatches | 4 | 4 | NS | 2 | <0.05 |
| Time on dialysis (mo) | 28 | 36 | NS | 48 | <0.05 |
| Cerebrovascular donor death (%) | 72 | 83 | NS | 20 | <0.05 |
| Gender matching donor → recipient (m → m or f → f/m → f/f → m) | 9/3/6 | 31/11/30 | NS | 14/8/8 | NS |
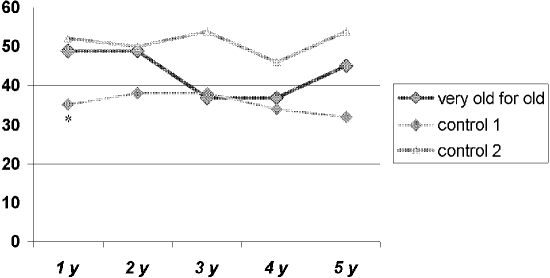
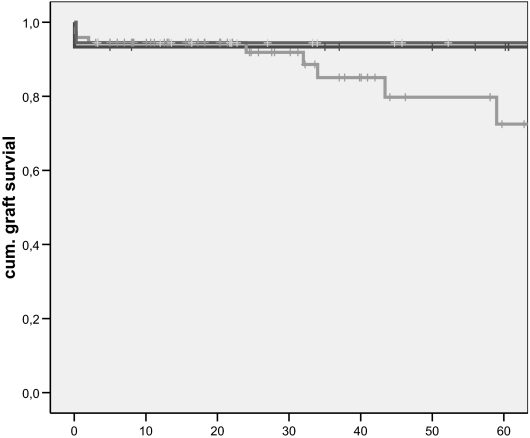
Graft function of the initial 5 yr after KTX assessed by median creatinine (Figure 1) differed significantly only at 3 mo and 3 yr between the study group and control group 2, whereas differences otherwise were not significant. Median creatinine clearance assessed by Cockcroft-Gault (Figure 2) did not differ between study group and control groups except for a significantly better clearance for control 1 at 1 yr. Censored (Figure 3) and uncensored (data not shown) graft survival did not differ between the groups, and DGF had no impact on graft survival of the study group (with versus without DGF, log rank 0.176) or in comparison with kidneys from control group 2 with DGF (log rank 0.29) or without DGF (log rang 0.91). No difference was found also for patient survival at 1, 3, and 5 yr: Study group 95, 83, and 83% versus control 1 96, 82, and 80% (log rank 0.686) versus control 2 90, 87, and 77% (log rank 0.297; Figure 3).
Figure 1.
Creatinine (mg/dl) after KTX. Only at two points in time did control group 2 show significantly better creatinine values than the study group (*).
Figure 2.
Creatinine clearance (ml/min) after KTX. Only at 1 yr was a significant difference (*) observed.
Figure 3.
Censored graft survival (months), death with functioning graft = no graft loss; red, study group (“very old for old”); green, control group 1 (old for old); blue, control group 2 (“ETKAS for old”). Differences were NS (see text).
Although other studies have shown the benefit of KTX of ECD kidneys into aged recipients exists,13,14 our study is the first to report on the outcome of donor kidneys aged ≥75 yr and transplanted into aged recipients (≥65 yr). We found that the rate of DGF did not differ in our study group from control groups, and rate of DGF was in the range found by other authors.5,15–17 In addition, we did not find a negative impact of DGF on graft survival in the ESP recipients as described by others.5,17 The favorable outcome in our study may be due to the very short CIT, because prolonged CIT is strongly associated with an increased rate of DGF. Every hour of CIT has also been found to reduce graft survival in the ESP setting by 3%5,18; therefore, it is of utmost importance for aged donor kidneys to keep CIT as short as possible. The earlier assumption of a reduced immunologic response of aged recipients, which is a crucial argument for allocating ESP kidneys without HLA matching, has proved to be wrong,5,19 and rejection rates in our study were in the range of control. Owing to the unexpected immunocompetence of aged recipients, a study to integrate HLA-DR matching into the allocation process was recently initiated by Eurotransplant.3
Graft survival in our study did not differ between HLA unmatched older and HLA matched younger donors (median age 48). This contradicts the findings of Frei et al.,5 who reported a significantly better survival of donor kidneys <60 yr in aged recipients compared with kidneys from donors aged ≥60, and our findings may be due to our selection criteria. Most recipient deaths occurred in the first year after KTX and were mainly due to cardiovascular or infectious reasons. Concerning graft loss, “death with functioning graft” was the main reason in our study. It has to be kept in mind that post-KTX mortality of aged kidney recipients is increased during the initial 12 to 18 mo, and the survival benefit of aged recipients is not realized until 1.0 to 1.5 yr after KTX.1 Nevertheless, even recipients aged ≥70 have been reported to have a significantly reduced risk for death after transplantation with ECD kidneys.14 Our task is to select the right patient for the waiting list and to perform a close follow-up after KTX.15,17
How can donor renal capacity and expected graft outcome best be predicted? Several criteria have been identified: Donor comorbidities and cause of death7,20; a histologic score for donors aged ≥60 for the decision to transplant one, both, or no kidney of the same donor21,22; and a score of demographic, medical, and CIT.23 Nevertheless, we found that donor creatinine clearance according to Cockcroft-Gault in combination with the aforementioned inclusion criteria are sufficiently reliable and easily applicable tools to predict graft outcome of ECD kidneys.
Overall, in our study, non–HLA-matched kidneys from donors aged ≥75 transplanted into recipients aged ≥65 showed as good graft function, graft survival, and patient survival as KTX with younger donor kidneys (HLA-matched or -unmatched). Even though the attitude toward the allocation of ECD kidneys has changed in the United States and dialysis patients today are offered additional allocation of ECD kidneys on a parallel waiting list,24 kidneys aged ≥75 are rarely accepted for KTX. Our study underlines that discarding of kidneys simply because of high donor age is not justified and must not be performed. These kidneys may very well provide good function and survival for the special subset of aged recipients for the rest of their lifespan as long as the aforementioned donor criteria are applied; a short CIT is guaranteed by handling old donor kidneys as urgent procedures around the clock; and a close pre-, peri-, and postoperative monitoring of aged recipients is performed.
Because a draw back of our study is the small sample size, we recommend a subgroup analysis of the Eurotransplant Senior Program data for the “very old for old” KTX.
We performed statistical analysis with SPSS 14.0 (SPSS, Chicago, IL). We compared categorical parameters by χ2 testing and assessed continuous variables by the Mann-Whitney U test. We calculated graft and patient survival by Kaplan-Meier analysis and tested for differences with the log-rank test. P < 0.05 was considered significant.
DISCLOSURES
None.
Acknowledgments
We thank Ineke Tieken, MD, Medical Staff Eurotransplant, for providing the allocation data.
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999 [DOI] [PubMed] [Google Scholar]
- 2.Oniscu GC, Brown H, Forsythe JL: How great is the survival advantage of transplantation over dialysis in elderly patients? Nephrol Dial Transplant 19: 945–951, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Eurotransplant International Report 2007, edited by Osterlee A, Rahmel A, Leiden, The Netherlands, 2007, p 25. Available at http://www.eurotransplant.nl/files/annual_report/AR2007_def.pdf
- 4.Organ Procurement and Transplantation Network. Available at http://www.optn.org
- 5.Frei U, Noeldeke J, Machold-Fabrizii V, Arbogast H, Margreiter R, Fricke L, Voiculescu A, Kliem V, Ebel H, Albert U, Lopau K, Schnuelle P, Nonnast-Daniel B, Pietruck F, Offermann R, Persijn G, Bernasconi C: Prospective age-matching in elderly kidney transplant recipients: A 5-year analysis of the Eurotransplant Senior Program. Am J Transplant 8: 50–57, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Smits JM, Persijn GG, van Houwelingen HC, Claas FH, Frei U: Evaluation of the Eurotransplant Senior Program: The results of the first year. Am J Transplant 2: 664–670, 2002 [DOI] [PubMed] [Google Scholar]
- 7.Metzger RA, Delmonico FL, Feng S, Port FK, Wynn JJ, Merion RM: Expanded criteria donors for kidney transplantation. Am J Transplant 3[Suppl 4]: 114–125, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Port FK, Bragg-Gresham JL, Metzger RA, Dykstra DM, Gillespie BW, Young EW, Delmonico FL, Wynn JJ, Merion RM, Wolfe RA, Held PJ: Donor characteristics associated with reduced graft survival: An approach to expanding the pool of kidney donors. Transplantation 74: 1281–1286, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Cecka JM, Cohen B, Rosendale J, Smith M: Could more effective use of kidneys recovered from older deceased donors result in more kidney transplants for older patients? Transplantation 81: 966–970, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Lee CM, Scandling JD, Shen GK, Salvatierra O, Dafoe DC, Alfrey EJ: The kidneys that nobody wanted: Support for the utilization of expanded criteria donors. Transplantation 62: 1832–1841, 1996 [DOI] [PubMed] [Google Scholar]
- 11.Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon TE, Metzger RA, Ojo AO, Port FK: Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 294: 2726–2733, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Giessing M, Budde K, Fritsche L, Slowinski T, Tuerk I, Schoenberger B, Neumayer HH, Loening SA: “Old-for-old” cadaveric renal transplantation: Surgical findings, perioperative complications and outcome. Eur Urol 44: 701–708, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Oniscu GC, Brown H, Forsythe JL: Impact of cadaveric renal transplantation on survival in patients listed for transplantation. J Am Soc Nephrol 16: 1859–1865, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Rao PS, Merion RM, Ashby VB, Port FK, Wolfe RA, Kayler LK: Renal transplantation in elderly patients older than 70 years of age: Results from the Scientific Registry of Transplant Recipients. Transplantation 83: 1069–1074, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Bodingbauer M, Pakrah B, Steininger R, Berlakovich G, Rockenschaub S, Wekerle T, Muehlbacher F: The advantage of allocating kidneys from old cadaveric donors to old recipients: A single-center experience. Clin Transplant 20: 471–475, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Fabrizii V, Kovarik J, Bodingbauer M, Kramar R, Hörl WH, Winkelmayer WC: Long-term patient and graft survival in the Eurotransplant senior program: A single-center experience. Transplantation 80: 582–589, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Cohen B, Smits JM, Haase B, Persijn G, Vanrenterghem Y, Frei U: Expanding the donor pool to increase renal transplantation. Nephrol Dial Transplant 20: 34–41, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Ojo AO, Wolfe RA, Held PJ, Port FK, Schmouder RL: Delayed graft function: Risk factors and implications for renal allograft survival. Transplantation 63: 968–974, 1997 [DOI] [PubMed] [Google Scholar]
- 19.Fritsche L, Hörstrup J, Budde K, Reinke P, Giessing M, Tullius S, Loening S, Neuhaus P, Neumayer HH, Frei U: Old-for-old kidney allocation allows successful expansion of the donor and recipient pool. Am J Transplant 3: 1434–1439, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Pessione F, Cohen S, Durand D, Hourmant M, Kessler M, Legendre C, Mourad G, Noël C, Peraldi MN, Pouteil-Noble C, Tuppin P, Hiesse C: Multivariate analysis of donor risk factors for graft survival in kidney transplantation. Transplantation 75: 361–367, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Gill J, Cho YW, Danovitch GM, Wilkinson A, Lipshutz G, Pham PT, Gill JS, Shah T, Bunnapradist S: Outcomes of dual adult kidney transplants in the United States: An analysis of the OPTN/UNOS database. Transplantation 85: 62–68, 2008 [DOI] [PubMed] [Google Scholar]
- 22.Remuzzi G, Cravedi P, Perna A, Dimitrov BD, Turturro M, Locatelli G, Rigotti P, Baldan N, Beatini M, Valente U, Scalamogna M, Ruggenenti P: Long-term outcome of renal transplantation from older donors. N Engl J Med 354: 343–352, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Nyberg SL, Matas AJ, Kremers WK, Thostenson JD, Larson TS, Prieto M, Ishitani MB, Sterioff S, Stegall MD: Improved scoring system to assess adult donors for cadaver renal transplantation. Am J Transplant 3: 715–721, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Merion RM: Expanded criteria donors for kidney transplantation. Transplant Proc 37: 3655–3657, 2005 [DOI] [PubMed] [Google Scholar]