Abstract
Objective To determine the effectiveness of screening for visual impairment in people aged 75 or over as part of a multidimensional screening programme.
Design Cluster randomised trial.
Setting General practices in the United Kingdom participating in the MRC trial of assessment and management of older people in the community.
Participants 4340 people aged 75 years or over randomly sampled from 20 general practices, excluding people resident in hospitals or nursing homes.
Intervention Visual acuity testing and referral to eye services for people with visual impairment. Universal screening (assessment and visual acuity testing) was compared with targeted screening, in which only participants with a range of health related problems were offered an assessment that included acuity screening.
Main outcome measures Proportion of people with visual acuity less than 6/18 in either eye; mean composite score of 25 item version of the National Eye Institute visual function questionnaire.
Results Three to five years after screening, the relative risk of having visual acuity < 6/18 in either eye, comparing universal with targeted screening, was 1.07 (95% confidence interval 0.84 to 1.36; P = 0.58). The mean composite score of the visual function questionnaire was 85.6 in the targeted screening group and 86.0 in the universal group (difference 0.4, 95% confidence interval -1.7 to 2.5, P = 0.69).
Conclusions Including a vision screening component by a practice nurse in a pragmatic trial of multidimensional screening for older people did not lead to improved visual outcomes.
Introduction
In population based surveys undertaken in the United Kingdom, visual acuity of less than 6/12 (below the United Kingdom driving requirement) has been found in around 20% of people aged 75 or older.1-3 A recent survey estimated that more than 70% of visual impairment in people aged 65 or older was potentially remediable.4 Visual impairment is associated with reduced functional status and quality of life,5 low social contact,6 depression,7 and falls and hip fractures.8 It is therefore unsurprising that primary care based screening of older people for visual impairment has repeatedly been called for.9-12
In practice, screening for visual impairment is likely to be only one part of a multidimensional assessment. Since 1990 in the United Kingdom the primary care team has been required to offer an annual screening, including an assessment of vision, to all patients aged 75 or over.13 Screening for visual problems is specifically included in the single assessment process to be offered to all older people proposed in the national service framework for older people.14 However, the effectiveness of screening older people for visual impairment has not been established. A systematic review in 1998 of the five trials to date found no evidence that screening reduced the prevalence of visual impairment.15,16 The lack of effectiveness in those trials may have been due to the use of self reported measures of vision as a screening instrument and the lack of clear plans of intervention for the problems that were identified.
To assess the effectiveness of screening for visual impairment, we measured visual outcomes among a random sample of participants in each arm of the MRC trial of the assessment and management of older people in the community.
Methods
The MRC trial of the assessment and management of older people in the community is a community based cluster randomised trial comparing different methods of multidimensional screening in people aged 75 years or over; it is taking place in 106 general practices from the Medical Research Council's general practice research framework.3,17,18 People aged 75 years or over who were registered with participating general practices were included in the study unless they were resident in a long stay hospital or nursing home or were terminally ill.
Baseline screening occurred between 1995 and 1999. Practices were randomised to two forms of screening: targeted or universal. Randomisation was performed centrally at the London School of Hygiene and Tropical Medicine, using a computer generated randomisation list stratified by thirds of Jarman score and of standardised mortality ratio. Because of the nature of the intervention, participants or researchers could not be blinded to the group assignment.
Interventions
Universal screening group
All participants in the trial were invited to complete a brief assessment followed by a detailed health assessment by a trained nurse that included measurement of visual acuity. Acuity was measured using a Glasgow acuity chart, which measures vision on the logMAR scale.19 For ease of interpretation, we give the Snellen equivalent acuity. Binocular vision was measured first, followed by vision in each eye. Measurements were repeated in people with visual acuity less than 6/18 in either eye, using a pinhole occluder to provide an estimate of acuity corrected for refractive error.20
For people with a pinhole vision of less than 6/18 in either eye, referral to an ophthalmologist was recommended unless they had been seen by an ophthalmologist in the previous year, or were registered blind or partially sighted. People with presenting vision of less than 6/18 in either eye that improved with pinhole to better than 6/18 were advised to see an optician. People with visual acuity less than 6/18 who could not complete a pinhole assessment were recommended for referral to an ophthalmologist.
Targeted screening group
At the time the trial was started, the contractual obligation on general practitioners to offer all patients aged over 75 years an annual health assessment meant it was not possible to have a control group that was offered no screening. In practices randomised to the targeted screening strategy, participants were invited to complete a brief screening assessment.17 This assessment covered all areas specified in the general practitioner contract, including a question about difficulty seeing, but did not include measurement of visual acuity. Only people found to have a specified range and level of problems during the brief assessment were invited to have a detailed assessment. Although reporting a lot of difficulty seeing was one possible factor contributing to eligibility for a more detailed assessment, it was not on its own sufficient to lead to an offer of a detailed assessment. The trial was designed such that about 20% of people in the targeted group would be eligible for a more detailed assessment.
Sampling
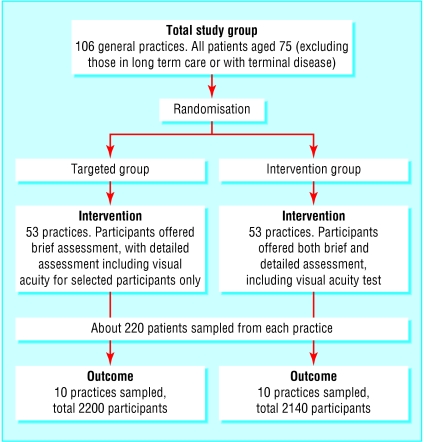
We randomly sampled 10 practices from each arm of the trial and 220 participants from each sampled practice and asked them to participate in the collection of visual outcomes (fig 1).
Fig 1.
Randomisation and sampling
At baseline the prevalence of visual acuity < 6/18 in one or both eyes was 30% with an intracluster correlation coefficient of 0.022. We estimated that outcome data for 2000 participants would provide over 80% power significant at the 5% level to detect a 30% difference in the prevalence of visual impairment. To allow for deaths and other losses to follow up we randomly sampled 220 eligible participants from each practice. Two practices in the universal screening group had fewer than 220 eligible people: 170 in one practice and 210 in the other. The final sample therefore included 2140 people in the universal screening group and 2200 people in the targeted screening group.
Outcome assessment
Three to five years after the baseline screening, sampled participants in the 20 practices included were invited to have an assessment of their vision. Research nurses assessed visual acuity and visual function and asked participants about contact with any eye services. In addition they searched medical records for information relating to vision. The two primary outcomes were the proportion of people with presenting visual acuity < 6/18 in one or both eyes, and the composite score of the 25 item version of the National Eye Institute visual function questionnaire. The questionnaire has been shown to be a reliable and valid measure of visual function;21,22 the highest available score is 100 representing no disability related to vision.
Analysis
All analyses used the "survey" commands in Stata 7.0 and took account of the cluster design. The intention to treat principle was applied as far as possible. Participants with outcome data available were analysed in the group to which they were randomised, regardless of whether they actually had a screening assessment at baseline.23
Results
Response rates and baseline characteristics
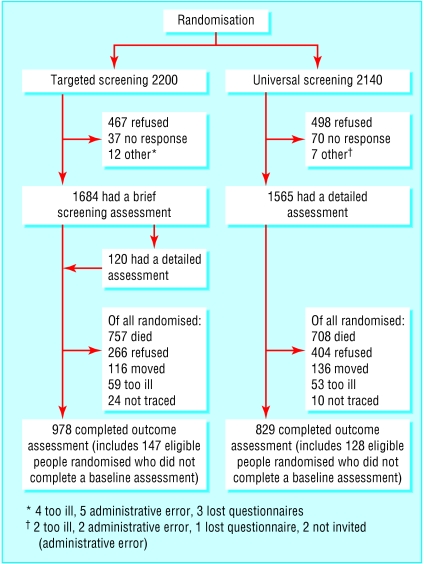
In the targeted screening group, 76.5% (1684/2200) of participants completed a brief screening assessment; 150 (6.8%) had sufficient number or severity of problems to be eligible for a more detailed assessment including visual acuity; and 120 (5.5%) completed the detailed assessment. In the universal screening group, 73.1% (1565/2140) completed a detailed assessment including visual acuity (fig 2). Table 1 shows the characteristics of participants at baseline.
Fig 2.
Flow of participants through the study
Table 1.
Baseline characteristics of participants. Values are percentages (numbers)
| Targeted screening group (n=1684) | Universal screening group (n=1662) | |
|---|---|---|
| Men | 36.8 (620) | 39.8 (661) |
| Median age (years) | 79.9 | 80.3 |
| Reporting a lot of difficulty seeing newsprint | 9.7 (162/1672) | 7.7 (127/1668) |
| Socially isolated* | 15.1 (254/1657) | 16.8 (279/1666) |
| Reporting often or always having difficulty making ends meet | 2.1 (35/1672) | 2.3 (39/1669) |
| Reporting one or more falls at home in the previous six months | 17.7 (290/1665) | 20.4 (334/1636) |
| Taking 5 or more drugs regularly | 17.6 (278/1602) | 18.5 (286/1547) |
Defined as reporting seeing friends, neighbours, or relatives less than twice a week.
Vision screening and eligibility for referral
In the universal screening group, 451/1565 people (28.8%) had a visual acuity < 6/18 in either eye. Of these, 79 (18%) were eligible for referral to an optician and 220 (49%) were eligible for referral to an ophthalmologist. Among the 120 people in the targeted screening group who had a visual acuity test, the proportion of people with reduced visual acuity was higher than in the universal screening group (43% v 29%), as were the proportions eligible for referral to the eye services (7% v 5% for referral to optician, 24% v 14% for referral to ophthalmologist) (table 2), reflecting the fact that eligibility for vision screening was based on having a specified level of problems detected at the brief assessment.
Table 2.
Screening findings and eligibility for referral in people who had visual acuity screening. Values are percentages (numbers)
| Findings | Targeted screening (n=120) | Universal screening (n=1565) |
|---|---|---|
| Detailed assessment | ||
| Visual acuity <6/18 in either eye | 43 (53) | 29 (451) |
| Pinhole assessment carried out | 51 (27/53) | 50 (223/451) |
| Visual acuity <6/18 in either eye that corrected to >6/18 with pinhole correction | 6 (8) | 50 (79) |
| Seen by ophthalmologist in previous 12 months | 7 (8) | 8 (130) |
| Registered: | ||
| Blind | 3 (4) | 1 (18) |
| Partially sighted | 5 (6) | 2 (35) |
| Data on registration status missing | 3 (3) | 1 (24) |
| Eligible for referral to optician | 7 (8) | 5 (79) |
| Eligible for referral to ophthalmologist | 24 (29) | 14 (220) |
| Other visual findings | ||
| Visual acuity <6/18 binocular | 22 (26)* | 12 (179)† |
| Visual acuity <6/12 in either eye | 60 (72) | 47 (736) |
| Visual acuity <6/12 binocular | 46 (54)* | 34 (508)† |
| Owned glasses | 88 (105) | 88 (1382) |
Excluding two people with missing data.
Excluding 84 people with missing data.
Outcome assessment
A total of 1807 outcome assessments were completed, 90.4% of the target of 2000 (fig 2). Excluding the 1465 people who died before assessment of outcome, the response rate was 62.8% (1807/2875). The response rate was 5.7% lower in the universal screening group (829/1432 v 978/1443), largely because two practices in the universal screening arm had low response rates because of problems with nurses' workload. The median time between baseline screening and outcome assessment was 3.9 years (interquartile range 3.3-4.5 years) in the targeted screening group and 3.9 (3.4-4.3) years in the universal group.
Primary outcomes
Comparing universal with targeted screening, we found that the relative risk of visual acuity less than 6/18 in either eye was 1.07 (95% confidence interval 0.84 to 1.36; P = 0.58) (table 3). The mean composite score of the National Eye Institute visual function questionnaire was 85.6 in the targeted screening group and 86.0 in the universal group, a difference of 0.4 (-1.7 to 2.5; P = 0.69). The standard deviation for the composite score was 17.8 overall and was similar in both groups.
Table 3.
Visual acuity outcomes. Values are percentages (numbers)
| Targeted screening group(n=978) | Universal screening group(n=829) | Risk ratio (95% CI) | P value | |
|---|---|---|---|---|
| Visual acuity <6/18 in either eye | 34.7 (339/978) | 37.0 (307/829) | 1.07 (0.84 to 1.36) | 0.58 |
| Visual acuity <6/18 binocular vision | 16.6 (160/962) | 14.0 (114/817) | 0.84 (0.64 to 1.10) | 0.20 |
| Visual acuity <6/12 in either eye | 59.7 (584/978) | 58.6 (486/829) | 0.98 (0.82 to 1.17) | 0.83 |
| Visual acuity <6/12 binocular vision | 36.5 (351/962) | 31.3 (256/817) | 0.86 (0.65 to 1.13) | 0.27 |
Adjustment for age, sex, level of self reported visual difficulty at baseline, and time until follow up had no impact on the results. Stratification by age, sex, level of self reported visual difficulty at baseline, social isolation, or time until follow up produced no evidence of subgroup effects. For the subgroup with time to follow up of 1.6 to 2.9 years, the relative risk of visual acuity less than 6/18 in either eye was 1.06, compared with 1.07 for follow up of 3.0 to 3.9 years and 1.09 for follow up of 3.9 to 5.8 years.
Restricting the analysis to people who had completed their allocated baseline screening assessments made little difference to the results. The relative risk of visual acuity < 6/18 in either eye on universal compared with targeted screening was 1.08 and difference in the mean composite score on the National Eye Institute visual function questionnaire (universal arm minus targeted arm) was 0.33 (86.1 in the targeted group and 86.4 in the universal group, difference 0.3 (-2.1 to 2.8, P = 0.78)).
Causes of visual impairment
Of the 504 people with visual acuity < 6/18 in either eye, 87 (17.3%) had a pinhole corrected acuity > 6/18, suggesting that the reduced vision could be attributed at least partly to refractive error (table 2). Because many people with reduced acuity did not complete a pinhole assessment the proportion attributable to refractive error will have been underestimated. The nurses reported that many participants found the pinhole occluder difficult to use or said they could not see properly through it.
Among the 249 people eligible for referral to an ophthalmologist after the baseline assessment, we obtained sufficient data to ascertain the likely causes of the visual loss for 113. Of these, 28 (25%) had age related macular degeneration, 59 (52%) had cataract (of whom 19 had no record of previous extraction), and 14 (12%) had both cataract and age related macular degeneration. Of the remaining 12, nine had a range of various diagnoses and three had never been seen by the eye services.
Referral to optician
The proportion of people advised to see an optician who reported attending an optician at least once after the baseline screening was high at 80% (32 out of 40 patients for whom data were available). New glasses or lenses had been recommended for 24 people and had been obtained by 18.
Referral to ophthalmologist
We obtained data for 75 people who had been eligible for referral to an ophthalmologist after baseline screening. There was clear evidence of a new referral for only 55% (41) of those eligible for referral. The proportion of people eligible for referral who were referred varied by practice, from 12% to 100%. Among the 41 people referred, uptake was high at 88% (36 patients), and 16 of these 36 people had a subsequent cataract extraction.
Discussion
Even though this trial overcame possible reasons for the lack of effectiveness of screening seen in previous trials (by using measured visual acuity rather than self reported problems, and by having a clear protocol for intervention), it showed that screening older people for visual impairment as part of a multidimensional screening assessment gave no benefit
Possible explanations for lack of effect
A "no screening" control arm was not possible, but this feature of the design is unlikely to explain the lack of effect: in the targeted screening group, only 2.2% of people were eligible for referral to the eye services, compared with 18.0% in the universal screening group.
Although a high prevalence of visual impairment was identified at screening, many affected people were already in contact with the eye services. In addition, the period between screening and assessment of outcome was quite long (median 3.9 years). Improvement or deterioration in vision between screening and follow up could have been missed. The intervention was, however, no more effective in a subgroup with a shorter time to assessment (1.6 to 3 years).
Response to outcome assessments seems low because just over a third of participants had died by the time of the assessment. The proportions who died were similar in the two groups. The follow up rate was 5.7% lower in the universal screening group. Although loss to follow up was not associated with baseline vision, a small effect on the results of the trial cannot be excluded.
Around half the people who had been advised to see an optician obtained new lenses. However, uncorrected refractive error was underdetected because a minority of participants completed the pinhole assessment, largely because of difficulties with using a pinhole occluder. Only 52% of people eligible for a referral had evidence of a new referral to an ophthalmologist; in previous trials of multidimensional screening, rates of clinicians' adherence to recommendations for referral have been in the range of 49% to 79%.24 Attendance at clinic of patients with evidence of a new referral to an ophthalmologist was 88%, higher than the range observed in previous trials (46% to 76%).24
Conclusion
Some people obtained beneficial interventions from vision screening, but the number of people benefiting was small in the context of a population based screening programme and was not sufficient to affect the prevalence of visual impairment overall. The evidence from randomised controlled trials undertaken to date does not support the inclusion of a vision screening component in multidimensional screening programmes for older people in a community setting.16
What is already known on this subject
Visual impairment is common and disabling and can often be improved with treatment
A previous systematic review found no evidence to support screening older people for visual impairment
The trials used self reported measures of vision as a screening instrument and lacked clear plans of intervention for visual problems identified
What this study adds
This randomised trial overcame the possible drawbacks of previous trials
Although a small number of people obtained beneficial interventions as a result of screening, this was not sufficient to reduce the prevalence of visual impairment at the population level
Barriers to improving vision among older people will need to be overcome before screening is likely to be effective
The recommendation that an assessment of vision be included in the single assessment process proposed in the national service framework for older people is not supported by the evidence. Given the importance of visual impairment among older people, other strategies to improve their vision is needed. The effectiveness of an optimised primary care based screening intervention that overcomes possible factors contributing to the observed lack of benefit in trials to date warrants assessment.
We thank Chris Bulpitt, Dee Jones, and Alistair Tulloch, co-investigators on the MRC trial of assessment and management of older people, and the nurses, GPs, the other staff and the patients in the participating practices: the MRC General Practice Research Framework Co-ordinating Centre (Madge Vickers, Jeannett Martin, and Nicky Fasey); the research team for the MRC trial of assessment and management of older people in the community; Elizabeth Breeze, Edmond Ng, Gill Price, Susan Stirling, Rakhi Kabiwala, and Janbibi Mazar at the London School of Hygiene and Tropical Medicine; Maria Nunes and Ruth Peters at Imperial College; Amina Latif and Elaine Stringer, University of Wales College of Medicine; the Trial Steering Committee (J Grimley Evans (chair), A Haines (previous chair), K Luker, C Brayne, M Vickers, M Drummond, L Davies, P Desai).
Contributors: LS, AF, RW, and JE developed the original idea for the study. AF is the principal investigator of the MRC trial of the assessment and management of older people in the community. AF, RW, and JE designed the baseline vision screening. SH coordinated the collection of visual outcomes. LS undertook the sampling, analysed the data, and wrote the paper. All authors commented on drafts of the paper and approved the final version. LS and AF are the guarantors.
Funding: The nested trial of vision screening was funded by the MRC under the MRC and Department of Health joint initiative in primary healthcare research. The MRC trial of the assessment and management of older people in the community was separately funded by the United Kingdom Medical Research Council, the Department of Health and the Scottish Office. LS was supported by a three year research fellowship from the NHS Executive Research and Development Directorate (Thames Region), and is now funded by an MRC Clinical Scientist Fellowship.
Ethical approval: Ethical approval for all aspects of the study was obtained from relevant ethics committees both for the original trial and for the practices involved in the repeat vision assessment.
References
- 1.Wormald RP, Wright LA, Courtney P, Beaumont B, Haines AP. Visual problems in the elderly population and implications for services. BMJ 1992;304: 1226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van der Pols JC, Bates CJ, McGraw PV, Thompson JR, Reacher M, Prentice A, et al. Visual acuity measurements in a national sample of British elderly people. Br J Ophthalmol 2000;84: 165-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans JR, Fletcher AE, Wormald RP, Ng ES, Stirling S, Smeeth L, et al. Prevalence of visual impairment in people aged 75 years and above in Britain: results from the MRC trial of assessment and management of older people in the community. Br J Ophthalmol 2002;86: 795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reidy A, Minassian DC, Vafidis G, Joseph J, Farrow S, Wu J, et al. Prevalence of serious eye disease and visual impairment in a north London population: population based, cross sectional study. BMJ 1998;316: 1643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott IU, Schein OD, West S, Bandeen-Roche K, Enger C, Folstein MF. Functional status and quality of life measurement among ophthalmic patients. Arch Ophthalmol 1994;112: 329-35. [DOI] [PubMed] [Google Scholar]
- 6.Carabellese C, Appollonio I, Rozzini R, Bianchetti A, Frisoni GB, Frattola L, et al. Sensory impairment and quality of life in a community elderly population. J Am Geriatr Soc 1993;41: 401-7. [DOI] [PubMed] [Google Scholar]
- 7.Rovner BW, Zisselman PM, Shmuely-Dulitzki Y. Depression and disability in older people with impaired vision: a follow-up study. J Am Geriatr Soc 1996;44: 181-4. [DOI] [PubMed] [Google Scholar]
- 8.Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 1996;348: 145-9. [DOI] [PubMed] [Google Scholar]
- 9.Hitchings RA. Visual disability and the elderly. BMJ 1989;298: 1126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strahlman E, Ford D, Whelton P, Sommer A. Vision screening in a primary care setting. A missed opportunity? Arch Intern Med 1990;150: 2159-64. [PubMed] [Google Scholar]
- 11.Wang F, Ford D, Tielsch JM, Quigley HA, Whelton PK. Undetected eye disease in a primary care clinic population. Arch Intern Med 1994;154: 1821-8. [PubMed] [Google Scholar]
- 12.Wun YT, Lam CC, Shum WK. Impaired vision in the elderly: a preventable condition. Fam Pract 1997;14: 289-92. [DOI] [PubMed] [Google Scholar]
- 13.Department of Health and the Welsh Office. General practice in the National Health Service. A new contract. London: DoH, 1989.
- 14.Department of Health. National service framework for older people. London: DoH, 2001. www.doh.gov.uk/nsf/olderpeople/docs.htm (accessed 28 Sep 2003).
- 15.Smeeth L. Assessing the likely effectiveness of screening older people for impaired vision in primary care. Fam Pract 1998;15(suppl 1): 24-9. [PubMed] [Google Scholar]
- 16.Smeeth L, Iliffe S. Community screening for visual impairment in the elderly. Cochrane Database Syst Rev 2000;2: CD001054. [DOI] [PubMed] [Google Scholar]
- 17.Smeeth L, Fletcher AE, Stirling S, Nunes M, Breeze E, Ng E, et al. Randomised comparison of three methods of administering a screening questionnaire to elderly people: findings from the MRC trial of the assessment and management of older people in the community. BMJ 2001;323: 1403-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fletcher AE, Jones DJ, Bulpitt CJ, Tulloch AJ. The MRC trial of assessment and management of older people in the community: objectives, design and interventions [ISRCTN23494848]. BMC Health Services Research 2002;2: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGraw P, Winn B. Glasgow acuity cards: a new test for the measurement of letter acuity in children. Ophthalmic Physiol Opt 1993;13: 400-4. [DOI] [PubMed] [Google Scholar]
- 20.Loewenstein JI, Palmberg PF, Connett JE, Wentworth DN. Effectiveness of a pinhole method for visual acuity screening. Arch Ophthalmol 1985;103: 222-4. [DOI] [PubMed] [Google Scholar]
- 21.Massof RW, Fletcher DC. Evaluation of the NEI visual functioning questionnaire as an interval measure of visual ability in low vision. Vision Res 2001;41: 397-413. [DOI] [PubMed] [Google Scholar]
- 22.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol 2001;119: 1050-8. [DOI] [PubMed] [Google Scholar]
- 23.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 2001;134: 663-94. [DOI] [PubMed] [Google Scholar]
- 24.Aminzadeh F. Adherence to recommendations of community-based comprehensive geriatric assessment programmes. Age Ageing 2000;29: 401-7. [DOI] [PubMed] [Google Scholar]