Short abstract
Focusing on prevention of HIV will not prevent the deaths of the millions already infected. The international community must adopt a strategy that links treatment and prevention
Despite recent proposals to expand access to antiretroviral treatment for people with HIV in resource poor settings, debate continues about the cost effectiveness of prevention and treatment strategies. This debate delays the urgent action needed to implement a comprehensive global AIDS strategy. To underscore the need to link prevention with treatment, we review the effect of HIV on economic and human development, the ways in which HIV prevention and treatment are mutually reinforcing, and the requirements for scaling up the response.
Why prevention is not enough
Prevention of HIV infection is often promoted as the only feasible option in resource poor settings despite the existence of drugs to treat it. As recently as 2002, experts argued that prevention should take priority over treatment for AIDS in Africa based on cost effectiveness.1,2 However, cost effectiveness analyses fail to take into account the most important reason for implementing widespread HIV treatment—treating sick people. Prevention strategies do nothing to improve the quality or length of life of the millions of people living with HIV. Moreover, the unchecked spread of HIV is resulting in indirect costs, ranging from orphaning to famine and from stigma to professional burnout, that are damaging already heavily burdened societies.
A poignant example of the shortcomings of the focus on prevention is the practice of prioritising the use of antiretroviral therapy for prevention of mother to child transmission without giving the drugs to mothers who are sick. Although this strategy protects babies, their untreated mothers develop AIDS and die. Clearly, both prevention of mother to child transmission and treatment of HIV positive parents are needed to protect the family and community.
Figure 1.
Patients with AIDS in a hospital in Mumbai, India
Credit: P VIROT/WHO
A comprehensive global AIDS strategy that links prevention to treatment is needed to save the lives of the 42 million people living with AIDS and to stop the humanitarian disaster that is being fuelled by the epidemic. Thailand and Uganda are often cited as models for HIV prevention and are unique because of their strong political commitment and the early implementation of HIV testing.3-5 Yet of 11 major randomised controlled trials that examined the effectiveness of HIV information, education, and communication interventions, none showed any effect on the epidemiology of the HIV epidemic.6 We are not arguing that prevention strategies should be abandoned but rather that prevention and treatment must be closely linked and strengthened to combat HIV and AIDS.
Effect of HIV and AIDS on social and economic development
Today, the average life expectancy in sub-Saharan Africa is 47 years; without AIDS, it would be 62. If widespread treatment of opportunistic infections (particularly tuberculosis) and antiretroviral drugs are not made available in the next two years Zimbabwe will lose 19% of its adult population, Botswana will lose 17%, South Africa 11%, Tanzania 9%, and the Ivory Coast 8%.7
The cost of not treating the AIDS epidemic can be seen by looking at the most salient economic indicators—family income, food, security, education, and health care. In Zambia, two thirds of families that lose the head of the household experience an 80% drop in monthly income. In the Ivory Coast, families that lose an adult to HIV experience a 50% decrease in household income. Agricultural productivity in Burkina Faso has fallen by 20% because of AIDS. In Ethiopia, HIV positive farmers spend between 11.6 and 16.4 hours a week farming compared with 33.6 hours weekly for healthy farmers.8
As more adults perish, the education of children is compromised. In Swaziland, school enrolment has fallen by 36%, mainly because girls have left school to care for sick relatives.9 The International Labor Organization estimated that in sub-Saharan Africa, 200 000 teachers will die from AIDS by 2010 (table 1).10 A report from the Ivory Coast indicated that in the 1996-7 academic year, more than 50% of deaths among elementary school teachers were from AIDS and 280 teaching hours a year were lost because of teacher absences.11
Table 1.
Effect of AIDS on predicted enrolment in primary school and on primary school teachers in sub-Saharan Africa by 201026
| Country | % fall in Nos of primary schoolchildren | No of teachers expected to die by 2010 |
|---|---|---|
| Kenya | 18 | 2 700 |
| Uganda | 12 | 6 700 |
| Zimbabwe | 24 | 12 400 |
| Zambia | 20 | 6 000 |
HIV is also having an effect on healthcare workers. In Malawi and Zambia the death rate of healthcare workers has increased sixfold since the early 1990s. In Southern Africa, 25-40% more doctors and nurses will need to be trained during 2001-2010 to compensate for deaths from AIDS.
Linking treatment with prevention
Where it is available, highly active antiretroviral therapy has resulted in 90% reduction in mortality and notable improvement in quality of life. In July 2002, however, less than 5% of people worldwide who require treatment had access to antiretroviral drugs. Half of the estimated 230 000 people currently receiving these drugs in resource poor countries live in Brazil. Fewer than 50 000 (under 2%) of HIV positive Africans receive antiretroviral therapy.
Some studies have linked the availability of treatment with an increase in risky behaviour.12 Yet rather than arguing against treatment, such studies provide further evidence that prevention remains critically important even when treatment is available. Experience with other infectious diseases, from tuberculosis to syphilis, has shown that even when a condition is treatable, controlling the disease requires a combination of prevention, education, and treatment. This type of comprehensive approach to the control of HIV has been implemented most successfully in Brazil. Under the national control strategy, HIV infections fell from 24 816 in 1998 to 17 504 in 2000 and were just 7361 in the first nine months of 2001.13
Treatment can provide an avenue of contact with the health provider, who can reinforce prevention messages. New prevention strategies proposed by the US Centers for Disease Control emphasise this secondary prevention approach, targeting HIV prevention messages at those who are known to be infected.14 Mathematical modelling suggests that limiting the spread of HIV in a community depends on the success of secondary prevention efforts.15
One of the most critical components of a comprehensive strategy is access to voluntary counselling and testing. The availability of treatment also increases the demand for counselling and testing. The uptake of voluntary counselling and testing at the Partners In Health clinic in rural Haiti increased by 300% after the introduction of antiretroviral drugs.16 Similar results have been reported in African countries.17 Data from voluntary counselling and testing programmes suggest that knowledge of serostatus is the most effective way to change behaviour.18-20 Yet 95% of people in Africa have no access to testing and remain unaware of their HIV status.21
Fewer than 12% of women in poor countries have access to prenatal HIV testing.22 Although prevention of mother to child transmission has been successful in the United States and Europe, fewer than 5% of pregnant women at risk of HIV infection have access to preventive treatment with antiretrovirals drugs. Widespread implementation of voluntary counselling and testing and programmes to prevent mother to child transmission can provide an essential foundation for the development of antiretroviral treatment programmes. They need to be backed up by drugs for prophylaxis and treatment of opportunistic infections.
Infrastructure: opportunities and constraints
A programme of antiretroviral treatment will need to be supported by an infrastructure to facilitate monitoring and support. But we cannot afford to wait for this infrastructure before starting treatment. Programmes could be started using community based infrastructure, as has been done with the directly observed therapy, short course (DOTS) programme for tuberculosis and the expanded programme on immunisations. The tuberculosis programme relies on community health workers to administer drugs and currently covers 50% of the African population. The expanded immunisation programme has developed structures to deliver immunisation in most resource poor countries that can provide immediate access to 80% of a country's newborn babies.23 The tuberculosis programme has been used to administer antiretroviral drugs in several pilot projects and Unicef has offered the vaccine delivery infrastructure as a possible mechanism for scaling up antiretroviral therapy.
Even if community based, non-traditional infrastructure is used to begin to implement a comprehensive global AIDS strategy, large scale investments in and sustained commitment to staff, facilities, and services are needed to meet the needs of the most heavily affected countries. Health workers require training in HIV prevention strategies, recognition and treatment of opportunistic infections, and use and management of antiretroviral therapy. Decent salaries in the public health sector will be needed to recruit and retain trained medical staff.
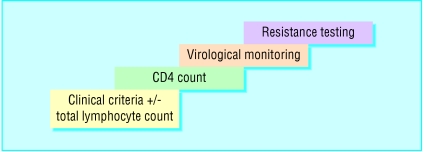
Limited laboratory infrastructure poses another problem to implementing HIV therapy in resource poor settings. Patients receiving treatment require virological monitoring. Again, the lack of availability of first world monitoring should not slow the initiation of life saving therapy. Services can be increased stepwise as laboratory capacity increases (figure).
Figure 2.
Stepwise approach to scaling up laboratory services for monitoring antiretroviral therapy
New initiatives
Awareness is increasing that responsibility for developing a comprehensive AIDS strategy is global and cannot be sustained solely within the health budgets of the world's poorest countries. International funding is beginning to be made available through the Global Fund to Fight AIDS, Tuberculosis, and Malaria24 and other initiatives (table 2). In its first and second round of grants, the global fund has disbursed $1.5bn (£900m, €1.3bn) to 160 programmes in 85 countries. This is a remarkable achievement within two years of inception. Yet the fund is facing a budget shortfall of $1.6bn for the third round of disbursements in October 2003.
Table 2.
New initiatives to fund comprehensive HIV prevention and treatment
| Initiative | Date | Money pledged ($) | Treatment and prevention aims cited |
|---|---|---|---|
| Global Fund to Fight AIDS, Tuberculosis, and Malaria | April 2002 | 378m allocated | 1 million/year receiving treatment |
| World Bank | February 2002 | 1bn grant to sub-Saharan Africa | To expand treatment and prevention in over 12 countries by 2002 |
| US emergency plan for AIDS relief | May 2003 | 15bn | 2 million being treated by 2004 |
| Senator Jesse Helms's statement of donation to global fund | March 2002 | 500m/year (in addition to US appropriation) | 400 000 mothers/year |
| Clinton Foundation | February 2003 | 3bn/year | |
| WHO and UNAIDS | July 2002 | No money pledged | 3 million being treated by 2005 |
Summary points
AIDS is causing a development crisis in Africa affecting economic stability, food supplies, education, and health care
A comprehensive global AIDS strategy must be implemented immediately
Prevention and treatment are mutually reinforcing components of controlling AIDS and should not be dichotomised
Infrastructure must be built and maintained to meet the increasing demands of the epidemic
Sustained, international funding is needed to implement a comprehensive global AIDS strategy
Among the reasons for the timid support of the fund by donors are the lack of proof that this new strategy will be effective25 and the political agendas that dictate allotment of foreign aid by donor countries. The US emergency plan, for example, has promised to earmark one third of the AIDS money for “abstinence only” education, a clear political statement to conservative American political groups. The crisis of HIV demands that the global community move beyond suspicion and national politics; it demands action and courage.
Controlling the HIV epidemic requires large scale investment in the public health infrastructure of resource poor countries as well as action to tackle factors such as poverty and external debt. So far the global community has been slow and less than generous in responding to HIV, but trends will be reversed and lives saved if we act now.
Contributors and sources: All information in this paper was collected from peer reviewed journals, international agency reports, and experience of Partners In Health in Haiti and the Ministry of Health in Brazil. JSM has worked since 1991 on the HIV epidemic in Kenya and Uganda and for the past four years in Haiti with Partners in Health. PF and PT have each had 29 years of experience in the HIV epidemic through Partners in Health in Haiti and the Brazilian National AIDS programme respectively. JYK has been involved in policy development for WHO and the Global Fund to Fight AIDS, Tuberculosis and Malaria and is involved in the WHO 3 million by 2005 campaign to accelerate access to antiretroviral drugs. CV, LM, and DN did the background research.
Competing interests: None declared.
References
- 1.Marseille E, Hoffman PB, Kahn JG. HIV prevention before HAART in sub-Saharan Africa. Lancet 2002;359: 1851-6. [DOI] [PubMed] [Google Scholar]
- 2.Creese A, Floyd K, Alban A, Guinness L. Cost-effectiveness of HIV/AIDS interventions in Africa: a systematic review of the evidence. Lancet 2002;359: 1635-43. [DOI] [PubMed] [Google Scholar]
- 3.Brody S. Decline in HIV infections in Thailand. N Engl J Med 1996;335: 1998-9. [DOI] [PubMed] [Google Scholar]
- 4.Okware S, Opio A, Musinguzi J, Waibale P. Fighting HIV/AIDS: is success possible? Bull World Health Organ 2001;79: 1113-20. [PMC free article] [PubMed] [Google Scholar]
- 5.Muller O, Barugahare L, Schwartlander B, Byaruhanga E, Kataaha P, Kyeyune D, et al. HIV prevalence, attitudes and behavior in clients of a confidential HIV testing and counseling center in Uganda. AIDS 1992;6: 869-74. [DOI] [PubMed] [Google Scholar]
- 6.Grassly NC, Garnett GP, Schwartlander B, Gregson S, Anderson RM. The effectiveness of HIV prevention and the epidemiological context. Bull World Health Organ 2001;79: 1121-32. [PMC free article] [PubMed] [Google Scholar]
- 7.UNAIDS. Report on the global HIV/AIDS epidemic. Geneva: UNAIDS, 2002.
- 8.Food and Agriculture Organization of the United Nations. Rural women carry family burdens. Focus, AIDS—a threat to rural Africa. Rome: FAO, 2001.
- 9.Urban Management Programme Regional Office for Africa. Making the linkages: HIV/AIDS, urban local government and the urban management programme in Sub-Saharan Africa. www.unhabitat.org/programmes/hiv/documents/UMP-ROA%20niche%20paper.pdf (accessed 26 Oct 2003).
- 10.Bennell P, Hyde K, Swainson, N. The impact of the HIV/AIDS epidemic on the education sector in Sub-Saharan Africa: a synthesis of findings and recommendations of three country studies. Brighton: University of Sussex, 2002.
- 11.Dzisah M. Cote d' Ivoire: AIDS is the main cause of death among teachers. Inter Press Service, 22 Jan 1999. www.aegis.com/news/ips/1999/IP990103.html (accessed 16 Oct 2003).
- 12.Blower SM, Aschenbach AN, Kahn JO. Predicting the transmission of drug-resistant HIV: comparing theory with data. Lancet Infect Dis 2003;3: 10. [DOI] [PubMed] [Google Scholar]
- 13.Dados epidemiológicos do Brasil. Boletim Epidemiológico—AIDS 2001 Jul-Sep:15(1). www.aids.gov.br/final/biblioteca/bol_set_2001/tab1.htm (accessed 16 Oct 2003).
- 14.Centers for Disease Control. Advancing HIV prevention: new strategies for a changing epidemic—United States. MMWR 2003;52(15): 329-32. [PubMed] [Google Scholar]
- 15.Blower SM, Farmer P. Predicting the public health impact of antiretrovirals: preventing HIV in developing countries. AIDScience 2003;3. www.aidscience.org/Articles/AIDScience033.asp
- 16.Farmer P, Leandre F, Mukherjee JS, Gupta R, Tarter L, Kim JY, et al. Community-based treatment of advanced HIV disease: introducing DOT-HAART. Bull World Health Organ 2001;79: 12. [PMC free article] [PubMed] [Google Scholar]
- 17.Lamptey PR. Reducing heterosexual transmission of HIV in poor countries. BMJ 2002;324: 207-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Voluntary HIV-1 Counselling and Testing Efficacy Study Group. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomized trial. Lancet 2000;356: 103-12. [PubMed] [Google Scholar]
- 19.Centers for Disease Control. Adoption of protective behaviors among persons with recent HIV infection and diagnosis—Alabama, New Jersey, and Tennessee, 1997-1998. MMWR 2000;49: 512-5. [PubMed] [Google Scholar]
- 20.Roth DL, Stewart KE, Clay OJ, van Der Straten A, Karita E, Allen S. Sexual practices of HIV discordant and concordant couples in Rwanda: effects of a testing and counseling program for men. Int J STD AIDS 2001;12: 181-8. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Scaling up the response to infectious diseases: a way out of poverty. Geneva: WHO, 2002.
- 22.De Cock KM, Fowler MG, Mercier E, de Vincenzi I, Saba J, Hoff E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA 2000;283: 1175-82. [DOI] [PubMed] [Google Scholar]
- 23.Batson A. Sustainable introduction of affordable new vaccines: the targeting strategy. Vaccine 1998;16(suppl): S93-8. [DOI] [PubMed] [Google Scholar]
- 24.Piot P, Coll Seck AM. International response to the HIV/AIDS epidemic: planning for success. Bull World Health Organ 2001;79: 1106-12. [PMC free article] [PubMed] [Google Scholar]
- 25.Bosch X. Europe refuses to match US cash to aid the ailing global fund. Lancet 2003;362: 299. [DOI] [PubMed] [Google Scholar]
- 26.Goliber T. Exploring the implications of the HIV/AIDS epidemic for selected African countries. Washington, DC: World Bank, 2000.