Abstract
Objective
To determine whether a history of preconceptional dieting and restrained eating was related to higher weight gains in pregnancy.
Design
Dieting practices were assessed among a prospective cohort of pregnant women using the Revised Restraint Scale. Women were classified on three separate subscales as restrained eaters, dieters, and weight cyclers.
Subjects
Participants included 1,223 women in the Pregnancy, Infection and Nutrition Study.
Main outcome measures
Total gestational weight gain and adequacy of weight gain (ratio of observed/expected weight gain based on Institute of Medicine (IOM) recommendations).
Statistical analyses performed
Multiple linear regression was used to model the two weight gain outcomes, while controlling for potential confounders including physical activity and weight gain attitudes.
Results
There was a positive association between each subscale and total weight gain, as well as adequacy of weight gain. Women classified as cyclers gained an average of 2 kg more than non-cyclers, and showed higher observed/expected ratios by 0.2 units. Among restrained eaters and dieters, there was a differential effect by BMI. With the exception of underweight women, all other weight status women with a history of dieting or restrained eating gained more weight during pregnancy and had higher adequacy of weight gain ratios. In contrast, underweight women with a history of restrained eating behaviors gained less weight compared to underweight women without those behaviors.
Conclusions
Restrained eating behaviors were associated with weight gains above the IOM recommendations for normal, overweight, and obese women, and weight gains below the recommendations for underweight women. Excessive gestational weight gain is of concern given its association with postpartum weight retention. The dietary restraint tool is useful for identifying women who would benefit from nutritional counseling prior to or during pregnancy in regards to achieving targeted weight gain recommendations.
Keywords: Dietary restraint, pregnancy, weight gain, weight cycling, dieting
Introduction
Concern over low birth weight and preterm birth led many to focus attention on determinants of inadequate weight gain during pregnancy. However, with the rising prevalence of obesity among women of childbearing age (1) and the high proportion of women who are gaining in excess of recommendations during pregnancy (2–4), the paradigm has shifted to a focus on the determinants of excessive weight gain during pregnancy.
Studies regarding the eating attitudes and dieting practices of women preconceptionally shed some light on the relationship between dietary intakes and maternal weight gain. It appears that women who diet habitually prior to becoming pregnant gain more weight during pregnancy and regard themselves as less accountable for their weight while pregnant (5, 6). Moreover, Conway and colleagues (7) found that those who were classified as restrained eaters (those who restricted their dietary intake or used other approaches for weight control) prior to pregnancy tended to gain more weight than recommended during pregnancy compared to unrestrained eaters, despite similarities in nutrient intakes (7). In the restrained group, energy intakes did not increase from early to late pregnancy as it did among women in the unrestrained group (7). These data suggest that repeated cycles of dieting and overeating may distort one’s ability to perceive internal hunger and satiety clues (8). This loss of control, in combination with the metabolic adaptations that occur among dieters, may be one of the reasons why overweight and obese women are more likely to gain above the recommended levels.
In non-pregnant populations, the concept of restrained eating has yielded mixed results. Among girls as young as 5 to 9 years old, restrained eaters showed significantly higher weight gains (9). Among adults, the results have been less clear. Klesges et al. (10) found no relationship between dietary restraint and weight gain among men or women, whereas Drapeau et al. (11) found a positive association among women and a negative association among men. Still others have found that restrained eating is associated with adiposity in normal-weight and not overweight participants, but that it does not necessarily promote weight gain (12). Lowe & Kral (13) observed that restrained eaters tended to increase their food intake when stressed and they argued that restrained eating may actually be a “proxy risk factor” for susceptibility to weight gain. Restrained eaters may be more susceptible because restrained eating behaviors include periods of eating less along with periods of disinhibition (14). These successive cycles of restrained and unrestrained eating may lead to more vulnerable weight cycles (15).
It is important to understand the factors that influence maternal weight gain so that proper counseling before and during pregnancy can be given. The purpose of this study was to determine whether a history of preconceptional dieting practices and restrained eating was related to higher weight gains in pregnancy, and whether this differed by pregravid BMI status. It is expected that individuals who have experienced large weight fluctuations, dieting, and restrained eating prior to pregnancy would gain more weight during pregnancy. Three studies completed on this topic have been done in the United Kingdom and have been limited by small samples sizes (5–7). This study involves a large cohort of pregnant women in the United States, with a high percentage of women gaining in excess of recommendations. In addition, data were collected on many potential confounding variables, allowing for the control of exercise and weight attitudes, for example, which previous studies have not been able to do.
Methods
Study sample
This study used data from the Pregnancy, Infection, and Nutrition (PIN) cohort, a prospective study that examines the risk factors for preterm birth and fetal growth. Women were recruited from both public and private prenatal clinics at the University of North Carolina Hospital in Chapel Hill, North Carolina. Potential subjects were identified by study staff through a review of all medical charts of new prenatal patients. Women who were less than age 16, non-English speaking, not planning to continue care or deliver at the study site, or carrying multiple gestations were not eligible to participate. The study staff recruited women at their second prenatal visit (mean gestation age of 14 weeks) and before 20 weeks gestation. Project staff explained the study, asked the woman to participate, and if she agreed, a consent form was signed. Recruitment extended from January 1, 2001 through June 30, 2005, with the weight gain attitudes and dietary restraint scales being added to the questionnaire on April 24, 2001. Of the 2006 women recruited, 1773 had information on pregravid height, weight, and weight gain. Stillbirths (n=13) were excluded from the analysis as well as those recruited prior to April 24, 2001 who did not have information on the restrained eating scale (n=463). There were 74 women in the cohort who were recruited for more than one pregnancy. The most recent pregnancy was kept in the analysis, except for the cases where more data were available for a prior pregnancy. The total number of women in our analysis was 1223. The protocols for this study were approved by the UNC School of Medicine Institutional Review Board.
Gestational weight gain
Prepregnancy weight was self-reported at screening and weight was measured at each subsequent prenatal visit. Total gestational weight gain was then calculated by subtracting prepregnancy weight from the weight at the last prenatal visit. The validity of self-reported weight by pregnant women has been examined previously and has been shown to be good if collected early in pregnancy and examined for biologically implausible values (16, 17). Height was measured during the 3 month postpartum home visit, which was then used with pregravid weight to calculate body mass index (BMI). Pregravid weight status was categorized using the 1990 Institute of Medicine (IOM) BMI cut points specific for the pregnancy state (<19.8 kg/m2 underweight, 19.8 to 26.0 kg/m2 normal weight, >26.0 to 29.0 kg/m2 overweight, and >29.0 kg/m2 obese) (18).
Adequacy of Weight Gain—main outcome
Adequacy of weight gain by pregravid BMI status was calculated as the ratio of the observed total weight gain over the expected total weight gain up to a woman’s last prenatal visit using the weight gain recommendations made in the 1990 IOM report (18). To calculate expected weight gain the following formula was used: expected first trimester total weight gain + [(gestational age at time of last weight measurement-13 weeks) × rate of weight gain expected for the second and third trimesters]. The expected total first trimester weight gains were 3.2, 2.2, 1.0, and 0.5 kg and the rates were 0.5, 0.4, 0.3, and 0.23 kg/wk for underweight, normal weight, overweight, and obese women, respectively (18). These rates adjust for the fact that not all women have a weight measurement at the time of delivery. Cut points to determine inadequate and excessive weight gains were based on the IOM BMI-specific recommendations. For example, it is recommended that underweight women gain between 12.5 and 18.0 kg which corresponds to an adequacy ratio of 0.75 to 1.10 if the pregnancy is carried to term (40 weeks). Thus, underweight women who have an adequacy ratio greater than 1.10 were defined as gaining above the IOM recommendation. This scale has been used previously in the literature (4, 19–21).
Revised Restraint Scale
To assess behaviors associated with restrained eating such as history of dieting, concern about eating too much food, and weight fluctuations, we used the revised restraint scale (RRS) (22, 23). Each woman in the study completed the RRS with the wording changed, as done by Conway and colleagues (7), so that it was clear the questions focused on the period prior to pregnancy, and not on weight changes associated with pregnancy. The RRS consists of 10 questions, each with 4–5 possible responses. Responses to questions regarding dieting behaviors were based on the Likert Scale (never, rarely, sometimes, often, always; or not at all, slightly, moderately, very much). Questions regarding weight fluctuations were based on specific categories of weight loss/gain. An overall score for Restrained Eating was calculated by summing the scores for all of the questions. Two sub-scales developed by Ruderman (24) were also used in the analysis. Specifically, the Concern with Dieting subscale was calculated by summing scores for questions regarding frequency of dieting, lifestyle changes after a weight fluctuation of 5 lbs, public and private eating behaviors, feelings of guilt after overeating, consciousness of food choices, and amount of time spent concerned about food. The Weight Cyclers subscale was calculated by summing scores from questions regarding typical weight fluctuations in the non-pregnancy state (0–1, 1.1–2, 2.1–3, 3.1–5, 5.1+ lbs), maximum weight ever lost within one month (0–4, 5–9, 10–14, 15–19, 20+ lbs), maximum weight gained within one week (0–1, 1.1–2, 2.1–3, 3.1–5, 5.1+ lbs), and the number of pounds over desired weight at maximum weight (0–1, 2–5, 6–10, 11–20, 21+ lbs). For each scale, comparisons were made between women with scores above and below the median (7, 23).
Potential Confounders
Data on potential confounders were collected via questionnaire, home visit, and medical chart abstraction. Poverty status was based on family income represented as percent of the poverty index according to the U.S. Bureau of the Census 1996(25). Variables assessed by questionnaire include maternal race, marital status, age, mother’s education, work status, parity, smoking status, and physical activity. The physical activity questionnaire was designed to capture moderate and vigorous activity during the past week. Metabolic equivalent levels (METs) were calculated based on the frequency, duration, and intensity of activities women reported doing during the previous week. This analysis adjusted for work (yes/no) and recreational activity (METs) during the second trimester.
Attitudes concerning gaining weight during pregnancy were assessed using the pregnancy and weight gain attitude scale (26). This scale is based on questions regarding concern about gaining too much weight, how much weight they would be willing to gain, if they enjoy wearing maternity clothes, embarrassment over being weighted, and how they feel about being pregnant. A composite score was calculated for each woman with higher scores representing positive attitudes.
Statistical analysis
Descriptive statistics were computed for all study variables. Chi-square tests were used to test for associations between demographic characteristics and restrained eating behaviors. Multiple linear regression was used to model the two outcomes related to weight gain (i.e. total gestational weight gain and the adequacy of weight gain ratio). Both potential outcomes were tested for normality. Normality assumptions were satisfied, and residual diagnostics were performed to check for validity of model fit and were found to be adequate. Regression models were fit while controlling for potential confounders; these included BMI, poverty, maternal race, maternal education, work, physical activity, age, marital status and weight gain attitudes. Covariates that changed the regression coefficient for restrained eating by more than 10% were retained in the final multivariable models. Testing for potential effect measure modification by BMI was conducted by comparing models with and without an interaction term for BMI and restrained eating. For the models where BMI was found to be an effect modifier, appropriate stratified analyses are shown. All statistical analyses were carried out using Stata software (Version 9.0, Release 2005, College Station, Texas). Results are presented as estimated weight gains or estimated weight gain adequacy ratios for restrained eaters and non-restrained eaters (as well as dieters, non-dieters, cyclers, and non-cyclers) at mean or reference levels of the other variables included in the multiple linear regression models (white race, age 29, delivered at term, working during the second trimester, middle income category, some college education, mean levels of recreational physical activity, and mean levels of weight gain attitudes).
Results
The cohort consisted of mostly white married women who had at least some college education and were living above the poverty line. Baseline sociodemographic characteristics (table 1) differed slightly by how the women are classified with regards to restrained eaters, cyclers, or dieters. In general, more overweight and obese women tended to be classified as restrained eaters, cyclers, or dieters. Cyclers had lower education and more women living below the poverty line. A greater percentage of cyclers were African American. In addition, dieters had more education, more women living above the poverty line, a greater percentage that were married, and lower prevalence of smoking during pregnancy. There were also a greater proportion of white women among the dieters.
Table 1.
Descriptive characteristics of women in the Pregnancy, Infection and Nutrition Study from 2002 to 2005 by Three Restrained Eating Subscales, n=1223
| Revised Restraint Scale | Weight Cyclers Subscale | Concern with Dieting Subscale | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Maternal characteristic | Overall | Restrained n = 559 | Non-restrained n = 557 | p-valuea | Cyclers n = 563 | Non-cyclers n = 557 | p-valuea | Dieters n = 622 | Non-dieters n = 595 | p-valuea |
| Age (y) (%) | ||||||||||
| < 20 | 5 | 3 | 7 | 0.000 | 2 | 7 | 0.003 | 3 | 8 | 0.000 |
| 20 – 30 | 53 | 52 | 55 | 53 | 54 | 49 | 58 | |||
| > 30 | 42 | 46 | 38 | 44 | 40 | 49 | 34 | |||
| Pregravid BMI (kg/m2)b (%) | ||||||||||
| Underweight | 14 | 6 | 23 | 0.000 | 5 | 24 | 0.000 | 9 | 19 | 0.000 |
| Normal | 51 | 45 | 58 | 41 | 61 | 48 | 53 | |||
| Overweight | 11 | 14 | 8 | 15 | 7 | 13 | 9 | |||
| Obese | 24 | 35 | 11 | 39 | 8 | 29 | 19 | |||
| Educational status (%) | ||||||||||
| High school | 20 | 16 | 23 | 0.009 | 20 | 19 | 0.000 | 15 | 25 | 0.000 |
| Some college | 47 | 51 | 44 | 52 | 42 | 48 | 47 | |||
| College graduate and above | 33 | 33 | 33 | 27 | 39 | 37 | 28 | |||
| Race (%) | ||||||||||
| White | 73 | 73 | 73 | 0.731 | 70 | 76 | 0.000 | 77 | 68 | 0.000 |
| African American | 19 | 19 | 18 | 23 | 14 | 15 | 23 | |||
| Other | 8 | 8 | 9 | 7 | 10 | 8 | 9 | |||
| Married (%) | 76 | 78 | 75 | 0.275 | 74 | 79 | 0.031 | 82 | 68 | 0.000 |
| Nulliparous (%) | 49 | 50 | 50 | 0.953 | 47 | 52 | 0.136 | 52 | 46 | 0.053 |
| Smoking during pregnancy (%) | 10 | 10 | 9 | 0.042 | 12 | 7 | 0.001 | 7 | 13 | 0.001 |
| Percent of poverty line (%) | ||||||||||
| <185% | 21 | 20 | 21 | 0.028 | 23 | 18 | 0.029 | 16 | 26 | 0.000 |
| 185–350% | 19 | 17 | 21 | 18 | 21 | 16 | 22 | |||
| >350% | 57 | 61 | 54 | 56 | 58 | 65 | 48 | |||
p value is based on a χ2 test of homogeneity to test for the association between maternal characteristics and restrained eating.
Prepregnancy BMI is categorized using the 1990 IOM BMI cutpoints specific for pregnancy: underweight, BMI <19.8 kg/m2; normal weight, BMI 19.8 to 25.9 kg/m2; overweight, BMI 26 to 29.9 kg/m2; and obese, BMI ≥ 30 kg/m2.
The average total weight gain among mothers that carried to term was 15.4 kg (SD 6.0) and the mean adequacy of weight gain ratio among the entire population was 1.52 (SD 0.84). This meant that on average the observed weight gain exceeded the expected by 52%. Average total weight gain, the percentage of women gaining in excess of the IOM recommendations, and the mean adequacy of weight gain ratio were compared across BMI categories to evaluate differences in weight change by BMI. The average total weight gain among mothers that carried to term was 15.5 kg (SD 4.3) for underweight, 16.7 kg (SD 5.2) for normal, 15.6 kg (SD 5.8) for overweight, and 12.1 kg (SD 7.4) for obese women, respectively. An analysis of variance (ANOVA) showed a significant association between average total weight gain and BMI (F=36.9, df 3, 1056, p<0.001). As should be expected, after adjusting for multiple comparisons, obese women were found to gain significantly less weight during pregnancy than women in all other BMI groups. The overall percentage of women who gained above the IOM recommendation was 63%, with 32% of underweight, 63% of normal weight, 85% of overweight, and 74% of obese women gaining in excess of recommendations (test of association between adequacy of weight gain and BMI: χ2=161.1, 6 df, p<0.001). The mean adequacy of weight gain ratio was 0.98 (SD 0.27) for underweight, 1.36 (SD 0.43) for normal, 1.85 (SD 0.67) for overweight, and 1.97 (SD 1.25) for obese women, respectively. There was a significant association between BMI and the mean adequacy of weight gain ratio (ANOVA: F=78.2, df 3, 1056, p<0.001). Bonferroni adjusted multiple comparisons showed that all groups were statistically different from one another, except for overweight and obese women.
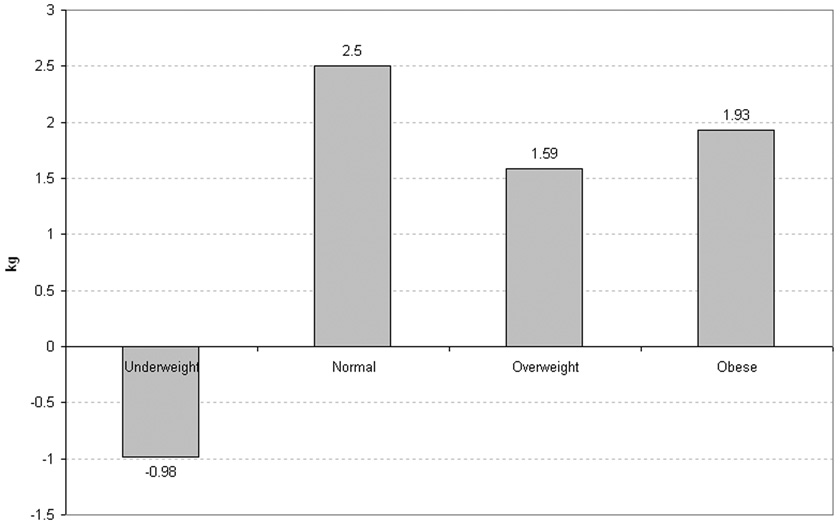
Multiple linear regression was used to model the association between the three restrained eating subscales and weight gain, while controlling for potential confounders. Overall, there was a positive association between each subscale and total weight gain (table 2), as well as between each subscale and the adequacy of weight gain ratio (table 3). On the weight cyclers subscale, women classified as cyclers gained an average of 2 kg more than non-cyclers (t=4.83, df 1, p<0.001). There was no effect modification by BMI status with this subscale. However, when classified as restrained eaters or dieters there was effect modification such that all weight status women, with the exception of underweight, gained more weight than their respective weight status groups who were non-restrained eaters or non-dieters (figure 1 displays this relationship among restrained eaters). Specifically, restrained eaters or dieters in the normal, overweight, and obese BMI categories gained between 1.6 and 2.8 kg more than non-restrained non-dieters of similar BMI status. In contrast, underweight women classified as restrained eaters or dieters gained an average of about 1 kg less than those who were not classified as such, although this was not statistically significant.
Table 2.
Estimated Weight Gain and 95% Confidence Intervals (CI) from Adjusted Multiple Linear Regression Models for Three Restrained Eating Subscales
| Restrained Eatersa | Non-restrained Eatersa | ||||||
|---|---|---|---|---|---|---|---|
| BMI | Estimated Weight Gain (kg) | 95% CI | Estimated Weight Gain (kg) | 95% CI | p valueb | ||
| Underweight | 14.42 | 12.44 | 16.40 | 15.40 | 14.33 | 16.47 | 0.388 |
| Normal | 18.03 | 17.25 | 18.81 | 15.53 | 14.84 | 16.23 | 0.000 |
| Overweight | 16.37 | 15.03 | 17.71 | 14.78 | 12.89 | 16.66 | 0.168 |
| Obese | 12.53 | 11.62 | 13.44 | 10.60 | 9.04 | 12.16 | 0.030 |
| Dietersc | Non-dietersc | ||||||
| Underweight | 14.11 | 12.44 | 15.79 | 15.10 | 13.83 | 16.38 | 0.293 |
| Normal | 16.99 | 15.98 | 18.00 | 15.26 | 14.30 | 16.23 | 0.000 |
| Overweight | 16.25 | 14.74 | 17.75 | 13.50 | 11.83 | 15.18 | 0.007 |
| Obese | 12.83 | 11.73 | 13.93 | 10.33 | 8.97 | 11.70 | 0.001 |
| Cyclersd | Non-cyclersd | ||||||
| Overall | 17.02 | 15.55 | 18.48 | 15.03 | 13.71 | 16.34 | 0.000 |
Models adjusted for BMI, work, physical activity, and weight gain attitudes. Estimated values are for women who delivered at term, were working during the second trimester, had mean levels of recreational physical activity, and mean levels of weight gain attitudes.
p-values test the effect of restrained eating, dieting, or weight cycling on total weight gain within each category of BMI
Models adjusted for BMI, maternal age, maternal race, and poverty. Estimated values are for white women age 29 (mean age) who delivered at term and were in the middle income category.
Models adjusted for BMI, work, physical activity, weight gain attitudes, maternal education, maternal race, and poverty. Estimated values are for white women who delivered at term, were working during the second trimester, had mean levels of recreational physical activity, mean levels of weight gain attitudes, some college education, and were in the middle income category. Estimated values shown are for underweight women, however there was no effect modification by BMI.
Table 3.
Estimated Adequacy of Weight Gain Ratio and 95% Confidence Intervals (CI) from Adjusted Multiple Linear Regression Models for Three Restrained Eating Subscales
| Restrained Eatersa | Non-restrained Eatersa | ||||||
|---|---|---|---|---|---|---|---|
| BMI | Estimated Adequacy of Weight Gain Ratio | 95% CI | Estimated Adequacy of Weight Gain Ratio | 95% CI | p valueb | ||
| Underweight | 0.94 | 0.68 | 1.19 | 1.02 | 0.89 | 1.16 | 0.544 |
| Normal | 1.50 | 1.40 | 1.60 | 1.31 | 1.23 | 1.40 | 0.004 |
| Overweight | 1.97 | 1.80 | 2.15 | 1.79 | 1.54 | 2.03 | 0.221 |
| Obese | 2.09 | 1.98 | 2.21 | 1.73 | 1.53 | 1.93 | 0.002 |
| Dietersc | Non-dietersc | ||||||
| Underweight | 0.88 | 0.66 | 1.11 | 0.94 | 0.77 | 1.11 | 0.662 |
| Normal | 1.38 | 1.25 | 1.52 | 1.25 | 1.12 | 1.37 | 0.033 |
| Overweight | 1.92 | 1.72 | 2.12 | 1.58 | 1.35 | 1.80 | 0.012 |
| Obese | 2.11 | 1.96 | 2.26 | 1.73 | 1.54 | 1.91 | 0.000 |
| Cyclersd | Non-cyclersd | ||||||
| Overall | 1.12 | 0.94 | 1.31 | 0.95 | 0.78 | 1.12 | 0.001 |
Models adjusted for BMI, work, physical activity, and weight gain attitudes. Estimated values are for women who were working during the second trimester, had mean levels of recreational physical activity, and mean levels of weight gain attitudes.
p-values test the effect of restrained eating, dieting, or weight cycling on adequacy of weight gain within each category of BMI
Models adjusted for BMI, maternal age, maternal race, and poverty. Estimated values are for white women age 29 (mean age), in the middle income category.
Models adjusted for BMI, work, physical activity, weight gain attitudes, maternal education, maternal race, and poverty. Estimated values are for white women who were working during the second trimester, had mean levels of recreational physical activity, mean levels of weight gain attitudes, some college education, and were in the middle income category. Estimated values shown are for underweight women, however there was no effect modification by BMI.
Figure 1.
Difference in estimated total gestational weight gain between restrained eaters and non-restrained eaters (kg). Estimates are based on multiple linear regression models adjusted for BMI, work status, physical activity, and weight gain attitudes.
For adequacy of weight gain, cyclers showed higher observed/expected ratios by 0.18 units (t=3.34, df 1, p=0.001). Among dieters and restrained eaters, there was a differential effect by BMI. For all BMI categories with the exception of underweight women, dieters and restrained eaters had higher weight gain adequacy ratios. Underweight women overall were closer to meeting their recommendations (ratios closer to 1) whereas, obese women had higher ratios indicating that they had surpassed their recommendation by almost 2 ½ fold. The pattern of increasing ratio with increasing BMI was evident.
Discussion
We found that restrained eating behaviors were associated with weight gains above the IOM recommendations. This association held whether women were classified as restrained eaters, dieters, or weight cyclers. Most importantly though is the fact that the effect of restrained eating on maternal weight gain varied by BMI status. Restrained eaters and dieters in the normal, overweight, and obese categories tended to gain in excess of recommendations, whereas underweight women gained less, when compared to women who did not display restrained eating behaviors. These results have important implications for both underweight and overweight and obese women.
For underweight women, being classified as a restrained eater may be indicative of an eating disorder and warrants further exploration. Underweight women with a history of restrained eating may also be at risk for adverse pregnancy outcomes (33–38). For overweight and obese women, restrained eating behaviors may be especially harmful because gaining outside of recommendations can lead to pregnancy complications as well as greater severity of their weight status (27–32). Following the weight gain recommendations can be especially difficult. Specific dietary recommendations for pregnant normal weight women include no increase in daily caloric consumption during the first trimester, with an addition of 340 to 450 kcal/day for the second and third trimesters, respectively (39). Currently there are no additional formal recommendations specifically for obese women. Failure to follow these recommendations could be due in part to misconceptions about eating for two during pregnancy. In addition, the availability of high-calorie and high-fat foods, which some have referred to as a “toxic food environment” (40), makes it increasingly hard for adults to avoid weight gain. It may be even more difficult during pregnancy to be in this type of environment, when there is less pressure to restrict intake (41)
This is the first study to examine the restrained eating scale in a large pregnancy cohort which had the ability to examine the effect of pregravid BMI status. In general, our results are consistent with the results from Conway et al. (7), Fairburn et al. (6), and Clark and Ogden (5), which all showed positive relationships between dieting and restrained eating behaviors and higher weight gains. The use of the RRS in pregnant populations needs further validation to ensure that the wording of the questions is appropriate for a pregnant population. In addition, the amount of weight fluctuations discussed on the RRS may not be appropriate for populations with an increasing prevalence of obesity. In addition, the use of a more standard cut point to identify restrained eaters versus non-restrained eaters would be helpful. Identification of a standard cut point will require additional research comparing the scale against a gold standard. Previous work has failed to report the median values used as cut points to define restrained versus non-restrained eaters in their studies, limiting the ability for comparison of the scale across populations.
There are several limitations worth noting. First, calculations of total weight gain include the starting point of self reported pregravid weight. It is well understood that underreporting of pregravid weight leads to higher total weight gains, which could overestimate the observed effect (42–44). Second, although the study was able to investigate the association of restrained eating behaviors while controlling for many possible confounders, such as physical activity during pregnancy and weight gain attitudes, there is still the possibility of residual confounding. Third, our population consists of mostly white, college educated women living above the poverty line. In addition, this cohort includes a smaller proportion of women under the age of 20, than would be expected in the general population since only women greater than 16 years of age were eligible to participate. These characteristics of the study population may limit generalizability and the applicability of the findings.
Conclusion
In summary, this study found an association between restrained eating and weight gain during pregnancy. The revised restraint scale could potentially be used by dieticians and health care providers at a preconception care visit or during family planning to identify women at risk for unhealthy eating behaviors. Women who are identified, particularly those that are underweight, should be followed up for potential eating disorders. For women who are not underweight, counseling and extra support could be given on healthy eating behaviors, increasing physical activity levels, and ways to eliminate stress which may increase the consumption of foods in certain social settings or in reaction to life events. During pregnancy it would be useful to target these women with similar nutritional and physical activity strategies in order to avoid excessive weight gain and adverse pregnancy outcomes such as gestational diabetes mellitus (GDM) (45–49), caesarean sections (29, 50–55), large-for-gestational age (LGA) (56–62), and breastfeeding duration (63–66).
Acknowledgments
Sources of Funding
This study received support from the National Institute of Child Health and Human Development, National Institutes of Health (HD37584, HD39373), the National Institute of Diabetes and Digestive and Kidney Diseases (DK61981), and the National Cancer Institute (CA109804). Biological specimen collection was supported by the General Clinical Research Center of the Division of Research Resources and funded by the National Institutes of Health (RR00046) at the University of North Carolina at Chapel Hill.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sunni L. Mumford, University of North Carolina at Chapel Hill, Department of Epidemiology, Carolina Population Center, 123 West Franklin St, University Square, Chapel Hill, North Carolina 27516, Phone: (919) 943-6678, Email: smumford@email.unc.edu.
Anna Maria Siega-Riz, University of North Carolina at Chapel Hill, Departments of Epidemiology and Nutrition, CB #7435 2105A McGavran-Greenberg, Chapel Hill, NC 27599-7435, Phone: (919) 962-8410, Fax: (919) 966-9159, Email: am_siegariz@unc.edu.
Amy Herring, University of North Carolina at Chapel Hill, Department of Biostatistics, CB #7420, School of Public Health, 3104D McGavran-Greenberg Hall, Chapel Hill, NC 27599-7420, Phone: (919) 843-6368, Fax: (919) 966-3804, Email: aherring@bios.unc.edu.
Kelly R. Evenson, University of North Carolina at Chapel Hill, Department of Epidemiology, Bank of America Center, 137 E Franklin Street, Suite 306, Chapel Hill, NC 27514, Phone: (919) 966-1967, Fax: (919) 966-9800, Email: kelly_evenson@unc.edu.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States 1999–2004. Jama. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Carmichael S, Abrams B, Selvin S. The pattern of maternal weight gain in women with good pregnancy outcomes. Am J Public Health. 1997;87(12):1984–1988. doi: 10.2105/ajph.87.12.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietz PM, Callaghan WM, Cogswell ME, Morrow B, Ferre C, Schieve LA. Combined effects of prepregnancy body mass index and weight gain during pregnancy on the risk of preterm delivery. Epidemiology. 2006;17(2):170–177. doi: 10.1097/01.ede.0000198470.26932.9a. [DOI] [PubMed] [Google Scholar]
- 4.Siega-Riz AM, Adair LS, Hobel CJ. Institute of Medicine maternal weight gain recommendations and pregnancy outcome in a predominantly Hispanic population. Obstet Gynecol. 1994;84(4):565–573. [PubMed] [Google Scholar]
- 5.Clark M, Ogden J. The impact of pregnancy on eating behaviour and aspects of weight concern. Int J Obes Relat Metab Disord. 1999;23(1):18–24. doi: 10.1038/sj.ijo.0800747. [DOI] [PubMed] [Google Scholar]
- 6.Fairburn CG, Stein A, Jones R. Eating habits and eating disorders during pregnancy. Psychosom Med. 1992;54(6):665–672. doi: 10.1097/00006842-199211000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Conway R, Reddy S, Davies J. Dietary restraint and weight gain during pregnancy. Eur J Clin Nutr. 1999;53(11):849–853. doi: 10.1038/sj.ejcn.1600864. [DOI] [PubMed] [Google Scholar]
- 8.Mela JRP. Food, eating and obesity: The psychobiological basis of appetite and weight control. London: Chapman & Hall; 1998. [Google Scholar]
- 9.Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc. 2004;104(7):1120–1126. doi: 10.1016/j.jada.2004.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klesges RC, Klem ML, Epkins CC, Klesges LM. A longitudinal evaluation of dietary restraint and its relationship to changes in body weight. Addict Behav. 1991;16(5):363–368. doi: 10.1016/0306-4603(91)90030-l. [DOI] [PubMed] [Google Scholar]
- 11.Drapeau V, Provencher V, Lemieux S, Despres JP, Bouchard C, Tremblay A. Do 6-y changes in eating behaviors predict changes in body weight? Results from the Quebec Family Study. Int J Obes Relat Metab Disord. 2003;27(7):808–814. doi: 10.1038/sj.ijo.0802303. [DOI] [PubMed] [Google Scholar]
- 12.de Lauzon-Guillain B, Basdevant A, Romon M, Karlsson J, Borys JM, Charles MA. Is restrained eating a risk factor for weight gain in a general population? Am J Clin Nutr. 2006;83(1):132–138. doi: 10.1093/ajcn/83.1.132. [DOI] [PubMed] [Google Scholar]
- 13.Lowe MR, Kral TV. Stress-induced eating in restrained eaters may not be caused by stress or restraint. Appetite. 2006;46(1):16–21. doi: 10.1016/j.appet.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 14.van Strien T. Success and failure in the measurement of restraint: notes and data. Int J Eat Disord. 1999;25(4):441–449. doi: 10.1002/(sici)1098-108x(199905)25:4<441::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 15.Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychol Bull. 1993;114(1):100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- 16.Stevens-Simon C, Roghmann KJ, McAnarney ER. Relationship of self-reported prepregnant weight and weight gain during pregnancy to maternal body habitus and age. J Am Diet Assoc. 1992;92(1):85–87. [PubMed] [Google Scholar]
- 17.Yu SM, Nagey DA. Validity of self-reported pregravid weight. Ann Epidemiol. 1992;2(5):715–721. doi: 10.1016/1047-2797(92)90016-j. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Nutrition during pregnancy. Part I, weight gain. Washington, DC: National Academy Press; 1990. [Google Scholar]
- 19.Bodnar LM, Siega-Riz AM, Cogswell ME. High prepregnancy BMI increases the risk of postpartum anemia. Obes Res. 2004;12(6):941–948. doi: 10.1038/oby.2004.115. [DOI] [PubMed] [Google Scholar]
- 20.Saldana TM, Siega-Riz AM, Adair LS, Suchindran C. The relationship between pregnancy weight gain and glucose tolerance status among black and white women in central North Carolina. Am J Obstet Gynecol. 2006;195(6):1629–1635. doi: 10.1016/j.ajog.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 21.Vahratian A, Zhang J, Troendle JF, Savitz DA, Siega-Riz AM. Maternal prepregnancy overweight and obesity and the pattern of labor progression in term nulliparous women. Obstet Gynecol. 2004;104(5 Pt 1):943–951. doi: 10.1097/01.AOG.0000142713.53197.91. [DOI] [PubMed] [Google Scholar]
- 22.Herman CP, Mack D. Restrained and unrestrained eating. J Pers. 1975;43(4):647–660. doi: 10.1111/j.1467-6494.1975.tb00727.x. [DOI] [PubMed] [Google Scholar]
- 23.Herman CPP. J. Restrained eating. In: Stunkard AJ, editor. Obesity. Philadelphia: Saunders; 1980. pp. 208–225. [Google Scholar]
- 24.Ruderman AJ. The restraint scale: a psychometric investigation. Behav Res Ther. 1983;21(3):253–258. doi: 10.1016/0005-7967(83)90207-3. [DOI] [PubMed] [Google Scholar]
- 25.Census USBot. U.S. Government Printing Office; Poverty in the United States. 1997
- 26.Palmer JL, Jennings GE, Massey L. Development of an assessment form: attitude toward weight gain during pregnancy. J Am Diet Assoc. 1985;85(8):946–949. [PubMed] [Google Scholar]
- 27.Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91(3):436–440. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castro LC, Avina RL. Maternal obesity and pregnancy outcomes. Curr Opin Obstet Gynecol. 2002;14(6):601–606. doi: 10.1097/00001703-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004;103(2):219–224. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 30.Galtier-Dereure F, Boegner C, Bringer J. Obesity and pregnancy: complications and cost. Am J Clin Nutr. 2000;71 5 Suppl:1242S–1248S. doi: 10.1093/ajcn/71.5.1242s. [DOI] [PubMed] [Google Scholar]
- 31.Hall LF, Neubert AG. Obesity and pregnancy. Obstet Gynecol Surv. 2005;60(4):253–260. doi: 10.1097/01.ogx.0000158509.04154.9e. [DOI] [PubMed] [Google Scholar]
- 32.Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25(8):1175–1182. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 33.Brinch M, Isager T, Tolstrup K. Anorexia nervosa and motherhood: reproduction pattern and mothering behavior of 50 women. Acta Psychiatr Scand. 1988;77(5):611–617. doi: 10.1111/j.1600-0447.1988.tb05175.x. [DOI] [PubMed] [Google Scholar]
- 34.Conti J, Abraham S, Taylor A. Eating behavior and pregnancy outcome. J Psychosom Res. 1998;44(3–4):465–477. doi: 10.1016/s0022-3999(97)00271-7. [DOI] [PubMed] [Google Scholar]
- 35.Lacey JH, Smith G. Bulimia nervosa. The impact of pregnancy on mother and baby. Br J Psychiatry. 1987;150:777–781. doi: 10.1192/bjp.150.6.777. [DOI] [PubMed] [Google Scholar]
- 36.Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: a longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res. 2007;63(3):297–303. doi: 10.1016/j.jpsychores.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 37.Stewart DE, Raskin J, Garfinkel PE, MacDonald OL, Robinson GE. Anorexia nervosa, bulimia, and pregnancy. Am J Obstet Gynecol. 1987;157(5):1194–1198. doi: 10.1016/s0002-9378(87)80293-4. [DOI] [PubMed] [Google Scholar]
- 38.Treasure JL. The ultrasonographic features in anorexia nervosa and bulimia nervosa: a simplified method of monitoring hormonal states during weight gain. J Psychosom Res. 1988;32(6):623–634. doi: 10.1016/0022-3999(88)90011-6. [DOI] [PubMed] [Google Scholar]
- 39.B. IoMFaN. Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Washington, DC: 2002. [DOI] [PubMed] [Google Scholar]
- 40.Brownell KDHK. Food fight: The inside story of the food industry, America's obesity crisis and what we can do about it. Chicago, IL: Contemporary Books; 2004. [Google Scholar]
- 41.Sarwer DB, Allison KC, Gibbons LM, Markowitz JT, Nelson DB. Pregnancy and obesity: a review and agenda for future research. J Womens Health (Larchmt) 2006;15(6):720–733. doi: 10.1089/jwh.2006.15.720. [DOI] [PubMed] [Google Scholar]
- 42.Brunner Huber LR. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11(2):137–144. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]
- 43.Engstrom JL, Paterson SA, Doherty A, Trabulsi M, Speer KL. Accuracy of self-reported height and weight in women: an integrative review of the literature. J Midwifery Womens Health. 2003;48(5):338–345. doi: 10.1016/s1526-9523(03)00281-2. [DOI] [PubMed] [Google Scholar]
- 44.Rowland ML. Self-reported weight and height. Am J Clin Nutr. 1990;52(6):1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 45.Catalano PM, Kirwan JP, Haugel-de Mouzon S, King J. Gestational diabetes and insulin resistance: role in short- and long-term implications for mother and fetus. J Nutr. 2003;133 5 Suppl 2:1674S–1683S. doi: 10.1093/jn/133.5.1674S. [DOI] [PubMed] [Google Scholar]
- 46.Gabbe SG, Graves CR. Management of diabetes mellitus complicating pregnancy. Obstet Gynecol. 2003;102(4):857–868. doi: 10.1016/j.obstetgynecol.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Langer O, Yogev Y, Xenakis EM, Brustman L. Overweight and obese in gestational diabetes: the impact on pregnancy outcome. Am J Obstet Gynecol. 2005;192(6):1768–1776. doi: 10.1016/j.ajog.2004.12.049. [DOI] [PubMed] [Google Scholar]
- 48.Solomon CG, Willett WC, Carey VJ, Rich-Edwards J, Hunter DJ, Colditz GA, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. Jama. 1997;278(13):1078–1083. [PubMed] [Google Scholar]
- 49.Xiong X, Saunders LD, Wang FL, Demianczuk NN. Gestational diabetes mellitus: prevalence, risk factors, maternal and infant outcomes. Int J Gynaecol Obstet. 2001;75(3):221–228. doi: 10.1016/s0020-7292(01)00496-9. [DOI] [PubMed] [Google Scholar]
- 50.LaCoursiere DY, Bloebaum L, Duncan JD, Varner MW. Population-based trends and correlates of maternal overweight and obesity, Utah 1991–2001. Am J Obstet Gynecol. 2005;192(3):832–839. doi: 10.1016/j.ajog.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 51.Ehrenberg HM, Durnwald CP, Catalano P, Mercer BM. The influence of obesity and diabetes on the risk of cesarean delivery. Am J Obstet Gynecol. 2004;191(3):969–974. doi: 10.1016/j.ajog.2004.06.057. [DOI] [PubMed] [Google Scholar]
- 52.Ray JG, Vermeulen MJ, Shapiro JL, Kenshole AB. Maternal and neonatal outcomes in pregestational and gestational diabetes mellitus, and the influence of maternal obesity and weight gain: the DEPOSIT study. Diabetes Endocrine Pregnancy Outcome Study in Toronto. Qjm. 2001;94(7):347–356. doi: 10.1093/qjmed/94.7.347. [DOI] [PubMed] [Google Scholar]
- 53.Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA. Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol. 2003;102(5 Pt 1):1022–1027. doi: 10.1016/j.obstetgynecol.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 54.Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH, et al. Obesity, obstetric complications and cesarean delivery rate--a population-based screening study. Am J Obstet Gynecol. 2004;190(4):1091–1097. doi: 10.1016/j.ajog.2003.09.058. [DOI] [PubMed] [Google Scholar]
- 55.Young TK, Woodmansee B. Factors that are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol. 2002;187(2):312–318. doi: 10.1067/mob.2002.126200. discussion 318–20. [DOI] [PubMed] [Google Scholar]
- 56.Caulfield LE, Stoltzfus RF, Witter FR. Implications of the Institute of Medicine weight gain recommendations for preventing adverse pregnancy outcomes in black and white women. Am J Public Health. 1988;88(8):1168–1174. doi: 10.2105/ajph.88.8.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stotland NE, Cheng YW, Hopkins LM, Caughey AB. Gestational weight gain and adverse neonatal outcome among term infants. Obstet Gynecol. 2006;108(3 Pt 1):635–643. doi: 10.1097/01.AOG.0000228960.16678.bd. [DOI] [PubMed] [Google Scholar]
- 58.Stevens-Simon C, McAnarney ER. Adolescent pregnancy. Gestational weight gain and maternal and infant outcomes. Am J Dis Child. 1992;146(11):1359–1364. doi: 10.1001/archpedi.1992.02160230117031. [DOI] [PubMed] [Google Scholar]
- 59.Parker JD, Abrams B. Prenatal weight gain advice: an examination of the recent prenatal weight gain recommendations of the Institute of Medicine. Obstet Gynecol. 1992;79(5 Pt 1):664–669. [PubMed] [Google Scholar]
- 60.Helms E, Coulson CC, Galvin SL. Trends in weight gain during pregnancy: a population study across 16 years in North Carolina. Am J Obstet Gynecol. 2006;194(5):32–34. doi: 10.1016/j.ajog.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 61.Devader SR, Neeley HL, Myles TD, Leet TL. Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index. Obstet Gynecol. 2007;110(4):745–751. doi: 10.1097/01.AOG.0000284451.37882.85. [DOI] [PubMed] [Google Scholar]
- 62.Kiel DW, Dodson EA, Artal R, Boehmer TK, Leet TL. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110(4):752–758. doi: 10.1097/01.AOG.0000278819.17190.87. [DOI] [PubMed] [Google Scholar]
- 63.Baker JL, Michaelsen KF, Sorensen TI, Rasmussen KM. High prepregnant body mass index is associated with early termination of full and any breastfeeding in Danish women. Am J Clin Nutr. 2007;86(2):404–411. doi: 10.1093/ajcn/86.2.404. [DOI] [PubMed] [Google Scholar]
- 64.Li R, Jewell S, Grummer-Strawn L. Maternal obesity and breast-feeding practices. Am J Clin Nutr. 2003;77(4):931–936. doi: 10.1093/ajcn/77.4.931. [DOI] [PubMed] [Google Scholar]
- 65.Rasmussen KM, Hilson JA, Kjolhede CL. Obesity as a risk factor for failure to initiate and sustain lactation. Adv Exp Med Biol. 2002;503:217–222. doi: 10.1007/978-1-4615-0559-4_25. [DOI] [PubMed] [Google Scholar]
- 66.Hilson JA, Rasmussen KM, Kjolhede CL. Excessive weight gain during pregnancy is associated with earlier termination of breast-feeding among White women. J Nutr. 2006;136(1):140–146. doi: 10.1093/jn/136.1.140. [DOI] [PubMed] [Google Scholar]