Abstract
BACKGROUND
Hematopoetic stem cell transplantation may be complicated by genital graft-versus-host (GVH) disease and may uncommonly result in labial fusion.
CASE
A 22-year-old woman with a history of Ewing's sarcoma and acute myelogenous leukemia received chemotherapy and total-body irradiation followed by a matched, unrelated donor hematopoetic stem cell transplantation. After transplantation, she developed chronic GVH disease involving the skin, eyes, mouth, and joints. Concomitant vulvar pruritus was presumed to be a fungal infection but, in fact, was genital GVH disease manifesting as labial fusion. Topical estrogen, topical steroids, and surgical division of the labia were successful.
CONCLUSION
Genital GVH disease should be considered in women with genital tract complaints after hematopoetic stem cell transplantation. Labial fusion secondary to chronic GVH disease may be treated successfully with surgery and medical therapy.
Allogeneic hematopoietic stem cell transplant is a treatment that is increasingly being used for a variety of malignant and nonmalignant diseases of the bone marrow and immune system. However, it may be complicated by chronic graft-versus-host (GVH) disease in 30% to 50% of transplants from human leukocyte antigens-matched siblings and 60% to 70% from matched unrelated donors.1,2 Acute VGH disease is prevented by immunosuppression. Frequently chronic GVH disease has an insidious onset over several weeks or months, varies from mild to severe disease, and is managed with immunosuppressive agents. The skin, mouth, eyes, liver, and intestines are the organs most commonly involved in chronic GVH disease. Compared with those receiving bone marrow transplant (BMT), patients receiving peripheral blood stem cell transplantation may have a more protracted course that more commonly involves the skin, vagina, and vulva.1
When the genital tract is affected in chronic GVH disease, this can add significant morbidity to patient's lives. Spinelli and colleagues3 demonstrated genital tract involvement in nearly 25% of patients with GVH disease, with the majority having vulvar disease manifested as erosions and fissures and a smaller proportion developing vaginal scarring, which often necessitated surgical treatment.3,4 Vulvar scarring is less commonly reported with chronic GVH disease and may result in labial fusion. Hypoestrogenism from chemotherapy-induced premature ovarian failure and chronic GVH disease can both cause vulvar or vaginal pain and irritation, which are distinguished by the appearance of the mucosa, which is pale in hypoestrogenism and reddened in chronic GVH disease. Here we describe a patient who developed labial fusion in the setting of hypoestrogenism and vulvar chronic GVH disease after receiving a peripheral blood stem cell transplantation.
CASE
A 22-year-old woman with a history of Ewing's sarcoma treated with radiation and chemotherapy developed myelodysplastic syndrome, which quickly progressed to acute myelogenous leukemia. She received additional chemotherapy and total-body irradiation followed by a matched unrelated donor peripheral blood stem cell transplantation.
Menarche had occurred at 13 years of age after normal breast and pubic hair development. The patient menstruated regularly before the diagnosis of Ewing's sarcoma, but became amenorrheic during her first month of chemotherapy, undergoing premature ovarian failure. She used oral contraceptive pills for hormone replacement.
Approximately 9 months after peripheral blood stem cell transplantation, the patient developed chronic GVH disease involving the skin, eyes, mouth, and joints. She originally presented to her collegiate health provider reporting vulvar pruritus. During this time, she was presumed to have a yeast infection and was treated with fluconazole without a pelvic examination. She sought further evaluation at a tertiary care when she was unable to insert a tampon. She had never been sexually active.
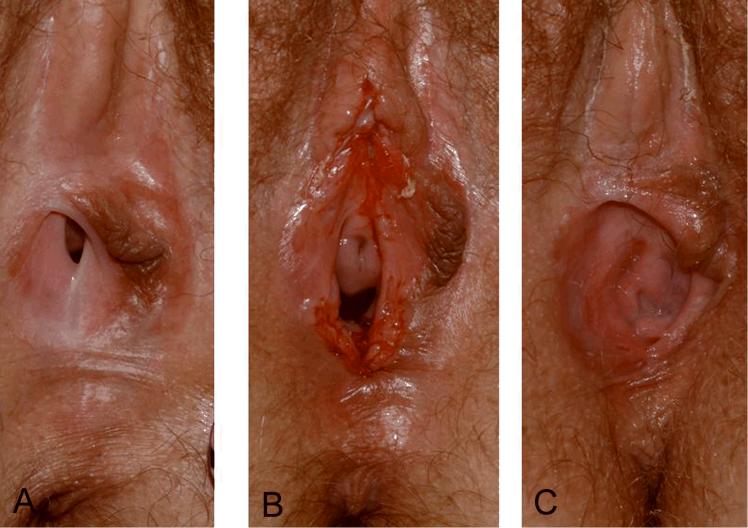
Pelvic examination revealed fusion of the labia minora anteriorly from the clitoris to the urethral meatus as well as posteriorly such that there was only a 1 cm opening for the urethra and vagina (Fig. 1A). The right labia minora was completely resorbed with the left labia minora pulled to the right side in a dense adhesion without an obvious raphe. As the adhesions were dense and extensive, speculum examination could not be done, and surgical management in conjunction with preoperative medical therapy was initiated. Pelvic magnetic resonance imaging revealed a normal uterus and ovaries, without any significant pathology.
Fig. 1.
A. Preoperative labial fusion with complete resorption of right labia minora and fusion of right and left labia minora. B. Labia immediately after surgical repair of labial fusion. C. Labia at 3 months after surgical repair. Norian. Labial Fusion After Stem Cell Transplant. Obstet Gynecol 2008.
After 2 weeks of topical estrogen cream, the patient was taken to surgery. At examination under general anesthesia, the adhesions in the posterior forchette were thinner, but the adhesions between labia minora were unchanged. Dissection of the labial adhesions was performed, and the raw mucosal surfaces were covered using a running suture of 3-0 vicryl (Fig. 1B). Vaginal examination revealed pale, minimally rugated, but otherwise normal, mucosa without any vaginal adhesions. Cervical cytology was normal. Postoperatively, the patient continued daily topical estrogen cream and applied hydrocortisone cream for occasional pruritus as needed.
At 3 months after surgery, the patient reported that her urinary stream was stronger, but she was unable to insert a tampon because of pain. On pelvic examination, the labia were open for a 3-4 cm area but had fused again only over the clitoral hood. On gentle palpation of a small adhesion on the posterior forchette, she experienced severe pain (Fig. 1C). Dilators coated with topical steroids and estrogen were prescribed. After a couple weeks, the patient was successfully able to insert a tampon without pain.
COMMENT
Vulvar scarring and labial fusion is an uncommon complication of chronic GVH disease in women after allogeneic hematopoietic stem cell transplant. As with labial fusion noted in young children and postmenopausal women, many patients with lower genital tract chronic GVH disease are hypoestrogenic5 and may respond to topical estrogen creams. However, when adhesions are dense and obstruct the urethral or vaginal opening, surgical intervention is often necessary in addition to the topical therapy.6,7
Vulvovaginal chronic GVH disease often manifests itself in patients with cutaneous and mucosal involvement, especially of the oral cavity and eyes. Symptoms are frequently under-reported by women and under-diagnosed by providers.3 Spinelli et al3 demonstrated genital manifestations of chronic GVH disease in 73% of patients with multi-organ involvement. At our institution, we have noted that women with vulvar complaints after peripheral blood stem cell transplantation and who have other sites of chronic GVH disease usually have vulvar GVH disease (96.2%, 28 of 29 patients). Our cohort who, in general, was referred for evaluation when they had vulvar symptoms, also had a high rate of chronic GVH disease in other skin and mucosal surfaces (Stratton P, Turner ML, Childs S, Barrett J, Bishop M, Wayne AS, et al. Vulvo-vaginal chronic graft-versus-host disease with allogeneic hematopoietic stem cell transplantation. Obstet Gynecol. In Press).8
Labial fusion from vulvar chronic GVH disease, especially fusion that precludes intercourse or interferes with voiding, is less common but is likely one manifestation of chronic GVH disease involving the lower genital tract. A thorough gynecologic history and examination should be undertaken in all females with vulvovaginal symptoms after allogeneic hematopoietic stem cell transplant, especially since these symptoms may indicate chronic GVH disease. As with vaginal scarring, labial fusion interferes with the capacity for sexual intimacy and may interfere with normal voiding. Furthermore, early detection and treatment of vulvar GVH disease with topical estrogen and steroids has been very successful in treating vulvar disease and might have prevented the need for surgery in this patient.
Acknowledgments
Supported by the intramural program of the National Institutes of Health Clinical Center, National Institute of Child Health and Human Development, and National Cancer Institute.
Footnotes
Financial Disclosure The authors have no potential conflicts of interest to disclose.PRINTER: Do not insert the copyright line on the proofs (this is a government work).
REFERENCES
- 1.Flowers ME, Parker PM, Johnston LJ, Matos AV, Storer B, Bensinger WI. Comparison of chronic graft-versus-host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-up of a randomized trial. Blood. 2002;100:415–9. doi: 10.1182/blood-2002-01-0011. [DOI] [PubMed] [Google Scholar]
- 2.Bhushan V, Collins RH., Jr Chronic graft-vs-host disease. JAMA. 2003;290:2599–603. doi: 10.1001/jama.290.19.2599. [DOI] [PubMed] [Google Scholar]
- 3.Spinelli S, Chiodi S, Costantini S, Van Lint MT, Raiola AM, Ravera GB. Female genital tract graft-versus-host disease following allogeneic bone marrow transplantation. Haematologica. 2003;88:1163–8. [PubMed] [Google Scholar]
- 4.Corson SL, Sullivan K, Batzer F, August C, Storb R, Thomas ED. Gynecologic manifestations of chronic graft-versus-host disease. Obstet Gynecol. 1982;60:488–92. [PubMed] [Google Scholar]
- 5.Opipari AW., Jr Management quandary: labial agglutination in a teenager. J Pediatr Adolesc Gynecol. 2003;16:61–2. doi: 10.1016/s1083-3188(02)00215-2. [DOI] [PubMed] [Google Scholar]
- 6.Costantini S, Di Capua E, Bosi S, Chiodi S, Spinelli S. The management of severe vaginal obstruction from genital chronic graft-versus-host disease: diagnosis, surgical technique and follow-up. Minerva Ginecologica. 2006;58:11–6. [PubMed] [Google Scholar]
- 7.Hatada Y. Two-step surgical approach to labial adhesions in a postmenopausal woman. Acta Obstet Gynecol Scand. 2003;82:1054–5. doi: 10.1034/j.1600-0412.2003.00028.x. [DOI] [PubMed] [Google Scholar]