INTRODUCTION
Pelvic floor muscles have two major functions; they provide 1; support or act as a “ floor” for the abdominal viscera including the rectum and 2; constrictor or continence mechanism to the urethral, anal and vaginal orifices (in females). Here, we will discuss the relevance of pelvic floor to the anal opening and closure function, and discuss new findings with regards to the role of these muscles in the vaginal and urethra closure mechanisms.
The bony pelvis is composed of sacrum, ileum, ischium, and pubis. It is divided into the false (greater) and true (lesser) pelvis by the pelvic brim. The sacral promontory, the anterior ala of the sacrum, the arcuate line of the ilium, the pectineal line of the pubis and the pubic crest that culminates in the symphsis pubis. The shape of the female bony pelvis can be classified into four broad categories: gynecoid, anthropoid, android, and platypelloid. The pelvic diaphragm is a wide but thin muscular layer of tissue that forms the inferior border of the abdominopelvic cavity. Composed of a broad, funnel-shaped sling of fascia and muscle, it extends from the symphysis pubis to the coccyx and from one lateral sidewall to the other. The urogenital diaphragm, also called the triangular ligament, is a strong, muscular membrane that occupies the area between the symphysis pubis and ischial tuberosities and stretches across the triangular anterior portion of the pelvic outlet. The urogenital diaphragm is external and inferior to the pelvic diaphragm. The pelvic ligaments are not classic ligaments but are thickenings of retroperitoneal fascia and consist primarily of blood and lymphatic vessels, nerves, and fatty connective tissue. Anatomists call the retroperitoneal fascia subserous fascia, whereas surgeons refer to this fascial layer as endopelvic fascia. The connective tissue is denser immediately adjacent to the lateral walls of the cervix and the vagina. The broad ligaments are a thin, mesenteric-like double reflection of peritoneum stretching from the lateral pelvic sidewalls to the uterus. The cardinal, or Mackenrodt's, ligaments extend from the lateral aspects of the upper part of the cervix and the vagina to the pelvic wall. The uterosacral ligaments extend from the upper portion of the cervix posteriorly to the third sacral vertebra.
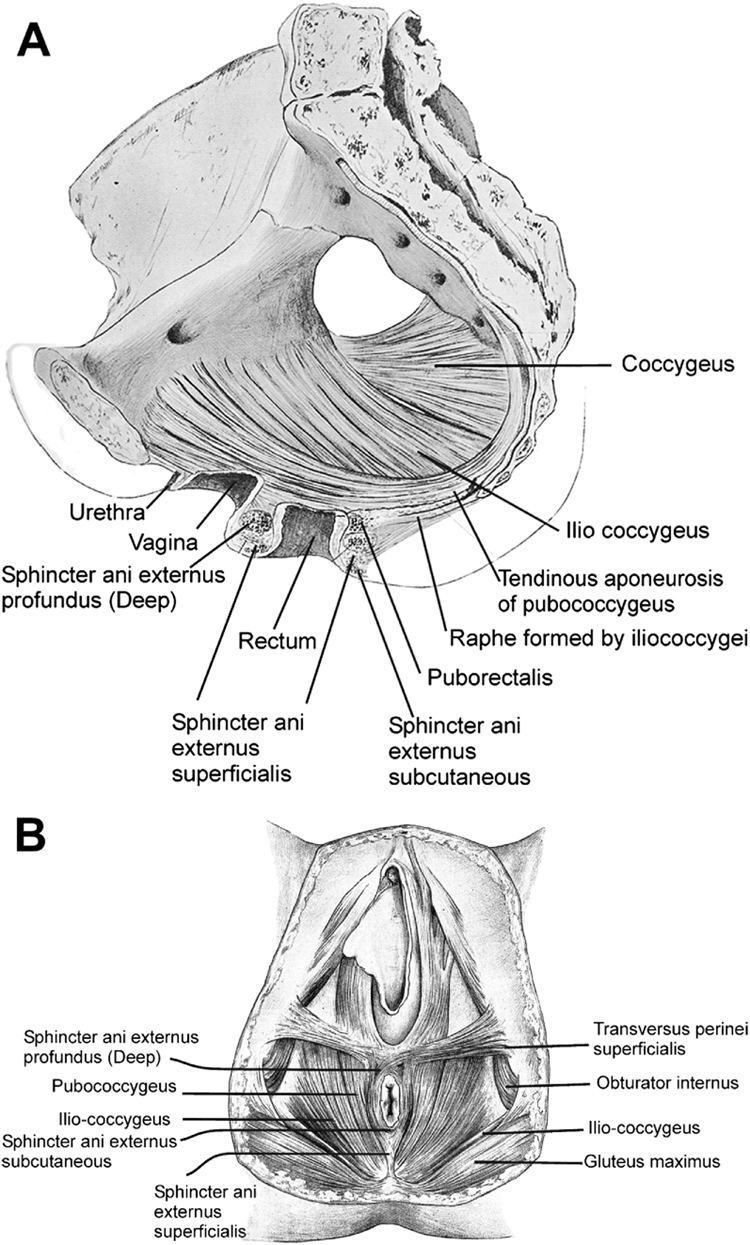
The pelvic floor is comprised of number of muscles and they are organized into superficial and deep muscle layers. There is significant controversy with regards to the nomenclature, but generally speaking, the superficial muscle layer and the muscles relevant to the anal canal function are the external anal sphincter, perineal body and possibly the puboperineal (or transverse perinei) muscles (Figures 1A and 1B). The deep pelvic floor muscles consist of pubococcygeus, ileococcygeuys, coccygeus and puborectalis muscles. In fact, puborectalis muscle is located in between the superficial and deep muscle layers, and it is better to view this as the middle muscle layer of the pelvic floor. In addition to the skeletal muscles of the pelvic floor, caudal extension of the circular and longitudinal smooth muscles from the rectum into the anal canal constitutes the internal anal sphincter and external anal sphincter of the anal canal respectively. First, we discuss the salient as well as some of the controversial aspects of anatomy of the pelvic floor and anal sphincter muscles, followed by a discussion of the function of each of component of the pelvic floor muscles and to their role in anal sphincter closure and opening.
Figure 1.
Figure 1a: Pelvic Floor Muscles Seen in the sagittal section of pelvis. Adapted from Thompson P. The Myology of the Pelvic Floor. Newton: McCorquoddale; 1899.
Figure 1b: Pelvic floor muscles as seen from the perineal surface. Adapted from Thompson P.
The Myology of the Pelvic Floor. Newton: McCorquoddale; 1899.
ANATOMICAL CONSIDERATIONS
INTERNAL ANAL SPHINCTER
Circular muscle layer of the rectum expands caudally into the anal canal and become the internal anal sphincter (IAS). The circular muscles in the sphincteric region are thicker than those of the rectal circular smooth muscle with discrete septa in between the muscle bundles. Similarly, the longitudinal muscles of the rectum extend into the anal canal and end up as thin septa that penetrate into the puborectalis and external anal sphincter muscles (EAS). Longitudinal muscle of the anal canal is also referred to as the conjoined tendon (muscle) because some authors believe that skeletal muscles of the pelvic floor (puboanalis) join the smooth muscles of the rectum to form a conjoint tendon. However, immuno-staining for the smooth and skeletal muscles in this region show that the smooth muscles make up the entire longitudinal muscle layer of the anal canal1, 2.
The autonomic nerves, sympathetic (spinal nerves) and parasympathetic (pelvic nerves) supply the internal anal sphincter3. Sympathetic fibers originate from the lower thoracic ganglia to form the superior hypogastric plexus. Parasympathetic fibers originate from the 2nd, 3rd and 4th sacral nerves to form the inferior hypogastric plexus, which in turn gives rise to superior, middle and inferior rectal nerves that ultimately supply the rectum and anal canal. These nerves synapse with the myenteric plexus of the rectum and anal canal. The majority of tone of the internal anal sphincter is myogenic, i.e., due to unique properties of the smooth muscle itself. Angiotensin 2 and prostaglandin F2α play modulatory roles. Sympathetic nerves mediate IAS contraction through the stimulation of α and relaxation through β1, β2 and β3 adrenergic receptors. Recent studies show a predominance of low affinity β3 receptors in the IAS. Stimulation of parasympathetic or pelvic nerves causes internal anal sphincter relaxation through nitric oxide containing neurons located in the myenteric plexus4. Vasointestinal intestinal peptide (VIP) and carbon monoxide (CO) are other potential inhibitory neurotransmitters of the inhibitory motor neurons but most likely play limited roles. There are also excitatory motor neurons in the myenteric plexus of IAS and the effects of these neurons are mediated through acetylcholine and substance P. Some investigators believe that the excitatory and inhibitory effects of myenteric neurons on the smooth muscles of IAS are mediate through the ICC but other investigators do not necessarily confirm these findings 4 . Degeneration of myenteric neurons resulting in impaired IAS relaxation is the hallmark of Hirschsprung’s disease5.
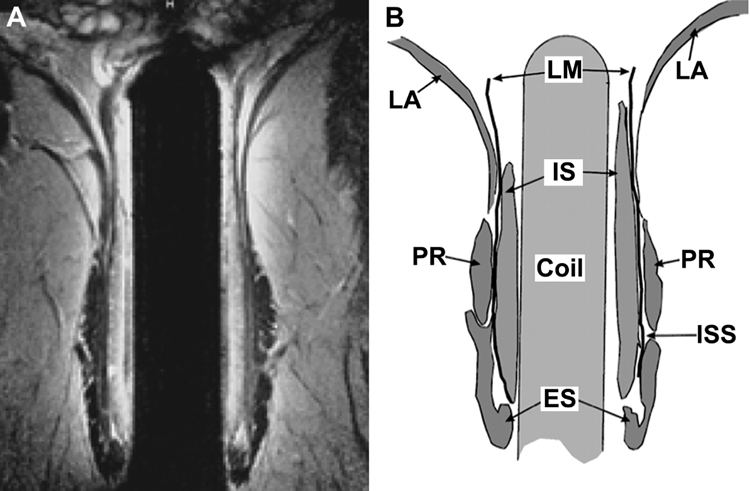
EXTERNAL ANAL SPHINCTER
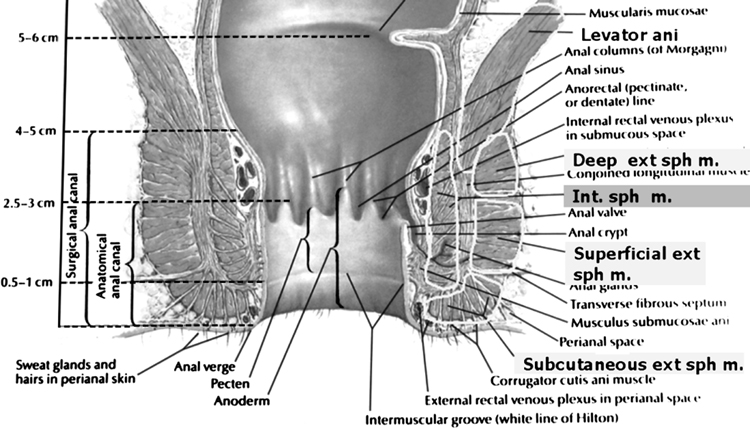
In his original description Santorini (1769) stated that EAS has three separate muscles bundles - subcutaneous, superficial and deep6. Large numbers of publication continue to show external anal sphincter to be made up of these 3 components. However, several investigators have found that the subcutaneous and superficial muscle bundles only constitute the EAS7–10. The subcutaneous portion of the EAS is located caudal to the IAS and the superficial portion surrounds the distal part of IAS. The deep portion of the EAS is either very small and merges imperceptibly with the puborectalis muscle, or in authors opinion has been confused with the puborectalis muscle. In several schematics published in the literature11, including the one by Netter (Figure 2), the EAS is made of three components. A close inspection of these schematics reveals that the puborectalis muscle is entirely missing from these drawings. Based on the 3 dimensional ultrasound and magnetic resonance imaging, we feel that the puborectalis muscle is actually the deepest part of the EAS. Shafik described that the EAS consists of 3 loops; in fact the puborectalis muscle forms the top loop in his drawing9 (figure 3). Histological studies by Fritsch1 and MR imaging study of Stoker et al12 (figure 4) are quite convincing that the EAS muscle is composed of only the subcutaneous and superficial portions1. Anteriorly, the EAS is attached to the perineal body and transverse perinei muscle, and posteriorly to the anococcygeal raphae. In fact, EAS is not a circular muscle in its entirety; rather it is attached to the transverse perinei (also called as puboperineal) muscle on either side8. The posterior wall of the EAS is shorter in its cranio-caudal extent than the anterior wall. This should not be misconstrued as a muscle defect in the axial US and MR images of the lower anal canal. Another implication of this peculiar anatomy is when the anal canal pressure is measured using circumferential side holes; the posterior side holes exit first from the anal canal13 first thereby causing apparent circumferential asymmetry of the anal canal pressures. The muscle fibers of EAS are composed of fast and slow twitch types, which allow it to maintain sustained tonic contraction at rest and also allow it to contract rapidly with voluntary squeeze. Motor neurons in Onuf’s nucleus (located in the sacral spinal cord) innervate EAS muscle through the inferior rectal branches of the right and left pudendal nerves11
Figure 2.
This schematic shows that the external anal sphincter is made up of subcutaneous, superficial and deep part. We believe that deep external anal sphincter is actually the puborectalis muscle (see text for explanation) Adapted from Frank.H.Netter, Atlas of Human Anatomy. Plate 393, 4th ed, Philadelphia, PA : Saunders/Elsevier, c2006 with permission
Figure 3.
A sketch of the external anal sphincter from a lateral view, as described by Shafik: External anal sphincter is described as made of 3 loops, basal loop (BL), intermediate loop (IL) and deep loop (DP). Note the relationship between the puborectalis muscle (PR) and DP. We believe that DP is actually the posterior part of the puborectalis muscle (see text for explanation). Adapted from Bogduk N. Issues in Anatomy: the external anal sphincter revisited. Aust N Z J Surg. Sep 1996;66(9):626–629, with permission.
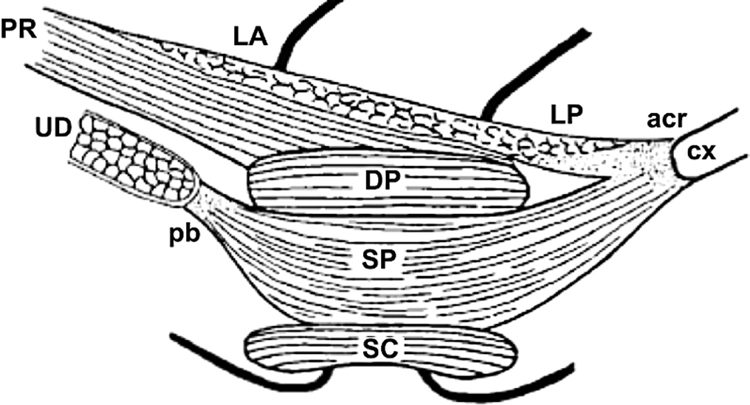
Figure 4.
Anatomy based on the MRI images: A: Coronal mid anal T2-weighted fast spin-echo (2,500/100) MR image obtained with an endoanal coil. B Corresponding drawing demonstrates the internal sphincter (IS), intersphincteric space (ISS), longitudinal muscle(LM), external sphincter (ES),puborectalis muscle (PR), and levator ani muscle (LA). These MRI images show that a part of the external anal sphincter is located below and a small portion surrounds the internal anal sphincter. Puborectalis muscle surrounds the upper part of the internal anal sphincter. Based on MR images it is quite clear that external anal sphincter consists of only 2 parts, subcutaneous (below the internal anal sphincter) and superficial (around the internal anal sphincter) (See text for explanation). Adapted from Stoker J, Halligan S, Bartram CI. Pelvic floor imaging. Radiology. Mar 2001;218(3):621–641, with permission.
PUBORECTALIS AND DEEP PELVIC FLOOR MUSCLES
In 1555, Andreas Vesalius wrote an account of the pelvic floor muscles, which he named “Musculus sedem attollens”14. This was later replaced by the more definitive name of “levator ani” by Von-Behr15. The pelvic diaphragm, first so named by Meyer16 (1861) included primitive flexors and abductors of the caudal part of the vertebral column. These muscles included coccygeus (also referred to as ischiococcygeuys), ileococcygeus and pubococcygeus and these three muscles were felt to constitute the levator ani muscle. They originate from the pectinate line of the pubic bone and the fascia of the obturator internus muscle and are inserted into the coccyx. Holl (1897), a German anatomist described that some of the pubococcygeus muscle fibers, instead of inserting into the coccyx, looped around the rectum and to these fibers he assigned the name “puborectalis” or “sphincter recti”17. It appears that the puborectalis muscle originates from the middle of inferior pubic rami rather than from the pubic symphysis. The puborectalis muscle is now included in the levator ani muscle group and the term “Levator ani” is used synonymously with pelvic diaphragm muscles. Peter Thompson18 in a classic text on this subject, “The MYOLOGY of the PELVIC FLOOR” wrote, according to Sappey (1869), the levator ani is one of those muscle which has been studied the most, and at the same time one about which we know the least”. Sappey also stated that the “The doctrine of continuity of fibers between two or more muscles of independent actions has been applied to the levator ani at various scientific epochs, and this ancient error, renewed without ceasing, has singularly contributed to complicate its study”19 It is interesting that to this date; the nomenclature, anatomy, neural innervation and functions of the levator ani / pelvic diaphragm are still veiled in deep mystery. Based on anatomical dissection studies, the pubococcygeus, puborectalis and puboperineal muscles originate from the pubic bone and are difficult to differentiate from each other. These muscles have also been collectively called as the pubovisceralis muscle; a concept originally championed by Lawson20 and currently supported by Delancey21 22 in majority of his writings. The term pubovisceral muscle is well accepted in the urogynecological texts, however it is rarely mentioned in the anatomical textbooks or gastroenterology literature. Lawson felt that the portions of the pubovisceral muscle are inserted into the urethra, vagina, perineal body and anal canal and to those portions he assigned the names pubouretheralis, pubovaginalis, puboperinealis and puboanalis muscles respectively. According to Lawson, the major function of these muscles is to provide physical support to the visceral organs.
Branches from the sacral nerve roots of S2, S3 and S4 innervate the pelvic floor muscles. However, there is considerable controversy as to whether the pudendal nerves actually innervate the levator-ani muscles. An electrophysiological study by Percy and colleagues found the electrical stimulation of the pudendal nerve did not activate the puborectalis muscle23. However, it is possible that in their study the electrodes may not have been precisely located in the puborectalis portion of the levator ani muscle. Our opinion is that the puborectalis muscle (middle layer of pelvic floor muscle) is actually innervated by the pudendal nerve24 (from below) and the deep muscles (pubococcygeus, ileococcygeus and coccygeus) are innervated by the direct branches of sacral nerve roots S3 & S43. The significance is that pudendal nerve damage may cause dysfunction of puborectalis muscle and external anal sphincter muscles (both constrictor muscles) and this in turn may cause fecal incontinence.
PELVIC FLOOR IMAGING
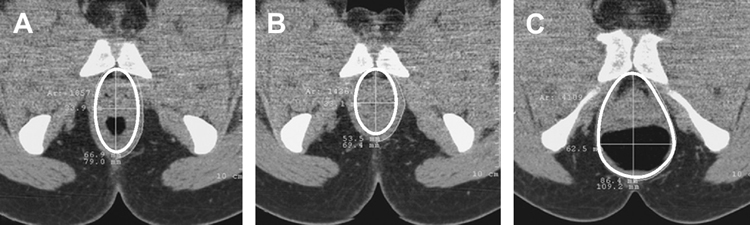
Advances in MRI, CT scanning and three dimensional (3D) ultrasound imaging have provided novel insights into anatomy and function of the pelvic floor muscles. Ultrafast CT scanning can image dynamic changes in the pelvic floor muscle during contraction and defecation25. These studies reveal that the levator hiatus becomes smaller during pelvic floor contraction and larger during the act of defecation (figure 5). The changes in the pelvic floor hiatus size are predominantly related to the puborectalis muscle and they reflect the constrictor function of pelvic floor. On the other hand, the ascent (elevation) and descent of the pelvic floor, including the levator plate, is mostly likely related to the contraction and relaxation of the pubococcygeus, ileococcygeus and ischiococcygeus muscles.
Figure 5.
Seated CT defecography, axial images of Puborectalis at rest (A), squeeze (B) and defecation (C). Note that the pelvic floor hiatus becomes smaller during squeeze and larger during defection. Adapted from Li D, Guo M. Morphology of the levator ani muscle. Dis Colon Rectum. Nov 2007;50(11):1831–1839, with permission.
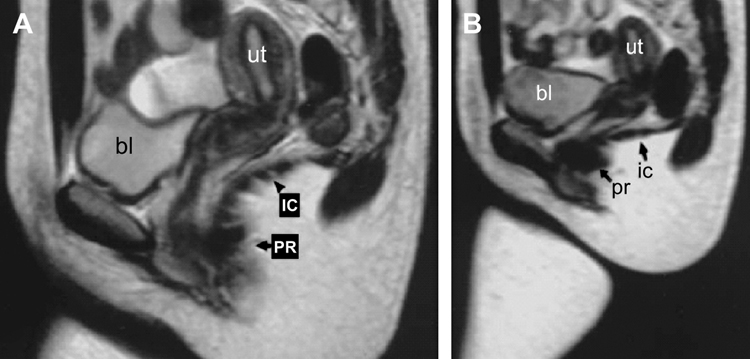
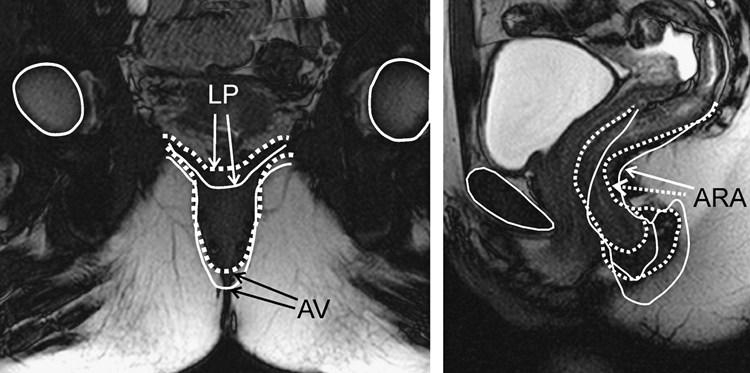
MRI studies have outlined the anatomy of pelvic floor muscles much more clearly than was possible with anatomical dissection studies. Hyott and colleagues developed imaging programs to outline the details of pelvic floor muscle. Their studies reveal physiological gaps in the ileococcygeus muscle, that one may perceive as defects in the pelvic floor muscles26. Elegant studies by Bharucha and colleagues have demonstrated, using dynamic MR imaging technique, changes in the anorectal angle during squeeze and during the act of defecation27–29. Changes in the anorectal angle reflect the constrictor function of pelvic diaphragm muscle, and it is felt that these changes in the anorectal angle are caused by the contraction and relaxation of the puborectalis muscle (figure 6, 7). On the other hand, it is likely that cranio-caudal movements of the anorectal angle are predominantly related to the pubococcygeus, ileococcygeus and ischiococcygeus muscles. During pelvic floor contraction, the anorectal angle becomes acute and it moves cephalad. On the other hand, during relaxation and defecation, the anorectal angle becomes obtuse and moves caudad.
Figure 6.
MRI images at rest and squeeze in the mid sagittal plane: These images show movements of the anorectal angle and levator plate (formed by the ileococcygeus muscle): Sagittal at rest (A) and straining (B) showing the changes in the different components of the levator ani (bl = bladder; ut = uterus; IC = Ileococcygeus; PR = puborectalis). On straining, the resting convex shape of the IC becomes flattened, and the genital hiatus reduces in size because of ventral movement of the puborectalis. Adapted from Singh K, Jakab M, Reid WM, Berger LA, Hoyte L. Three-dimensional magnetic resonance imaging assessment of levator ani morphologic features in different grades of prolapse. Am J Obstet Gynecol. Apr 2003;188(4):910–915, with permission.
Figure 7.
Magnetic resonance images (MRI) in the mid sagittal and coronal planes: these images were obtained at rest (Solid) and squeeze (dotted) and then the images were overlapped to show the movement of various anatomical structures during squeeze. Note the cranial and ventral movements of the anal canal and change in the anorectal angle with squeeze. In the coronal images, note the vertical movement of the anus, and flattening of the levator plate with squeeze. Obtained from author
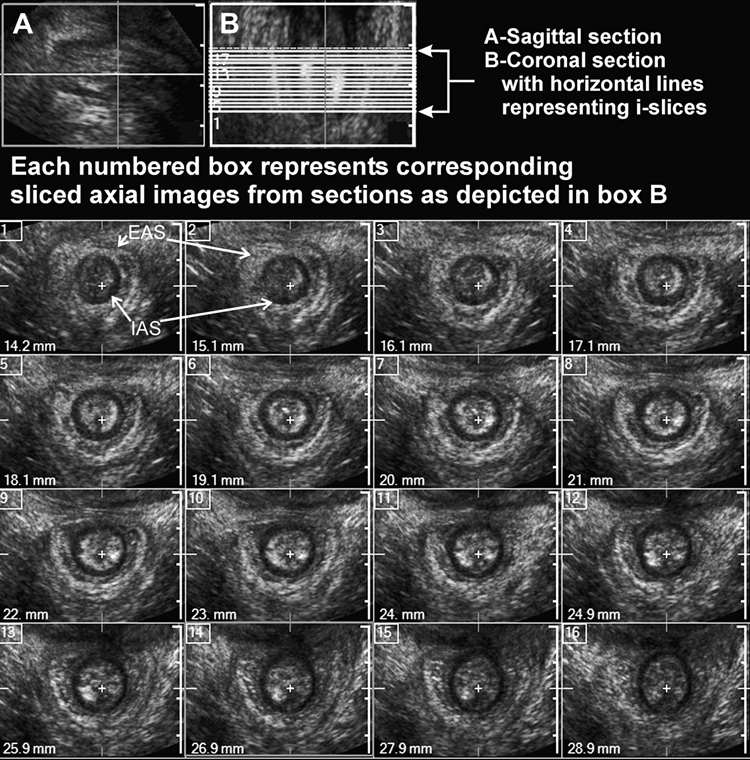
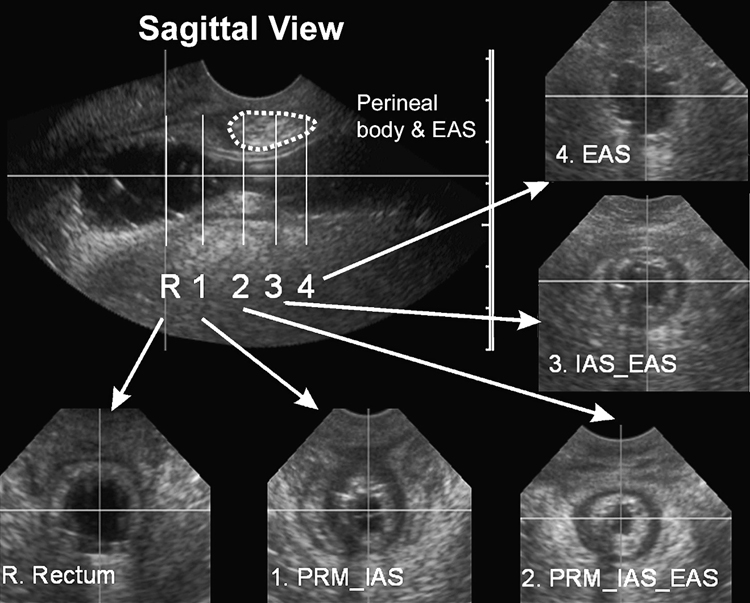
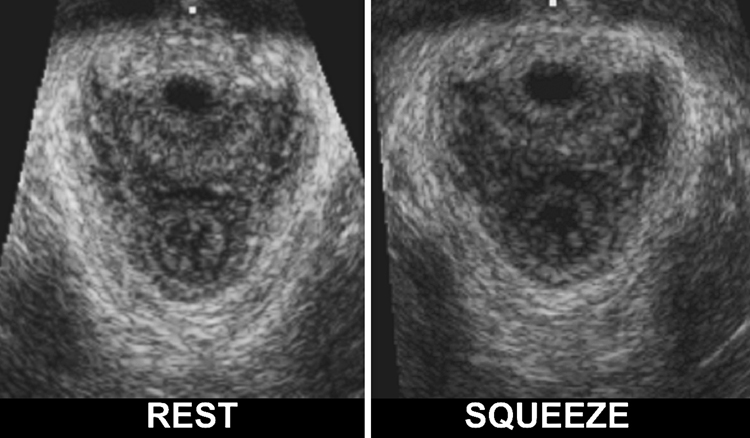
Two dimensional and 3D endoanal US imaging are used widely to detect defects in the anal sphincter complex. More recently, 3D ultrasound imaging (3D-US) using cutaneous (transperineal) approach has provided novel insights into the anatomy and function of the anal sphincter muscles and pelvic floor muscles. The major advantages of 3D transperineal US imaging are that, 1; it is subject friendly (no insertion of the transducer into the anal canal is required), 2; it can be performed in the physician’s office and, 3; it is relatively inexpensive. Dietz has used this technique quite effectively to study the physiology and pathophysiology of pelvic floor muscles under various conditions30–32. This technique is relatively simple, it requires placement of the US transducer on the skin of the perineum. A 3D-US volume is acquired over a period of 6–8 seconds and US images can be analyzed off line in the coronal, sagittal, transverse or for that matter in any other plane. This technique also allows capturing of dynamic or cine- images in 2 or 3 planes and therefore makes it possible to study the motion of various pelvic floor structures in real time. In addition, the software program can slice these image volumes at every 1mm or any desired distance to provide the 2D tomographic images at close distances (figure 8). We have extended the use of 3D-US imaging to study the anal canal closure mechanism33, vaginal high-pressure zone34 and the role of puborectalis muscle in the genesis of anal canal and vaginal canal pressures. Defects in the anal sphincter and puborectalis muscles can be detected relatively easily using the 3D-US imaging technique35.
Figure 8.
Ultrasound images of the anal canal obtained from the 3D-US volume: cross-sectional (axial) images along the length of anal canal in a nulliparous subject. In this example the anal sphincter complex is shown at every 1 mm distance using I-Slice function of HD-11 (Philips). Marked in the figure are the IAS (black circle) and the EAS (white outer ring) are smooth, uniform and symmetrical. Obtained from author
SENSORY FUNCTION OF THE RECTUM AND ANAL CANAL
Similar to other viscera, colonic distention results in non-descript discomfort and at higher degrees of distension one feels pain that is poorly localized. On the other hand, rectal distention is perceived as rectal fullness that is more localized and somewhat defined, i.e., as a desire to defecate. In addition to mucosal nerve endings, there are also low threshold, slowly adapting mechanoreceptors in the muscularis propria of the rectum. These intraganglionic laminar endings detect mechanical deformation of the myenteric ganglia and are most likely involved in detecting tension in the circular and longitudinal muscles of the rectum. The anal canal responds to distention as well as mechanical shearing stimuli, it is lined by numerous free and organized nerve endings (i.e. Meissner’s corpuscles, Krause end-bulbs, Golgi-Mazzoni bodies and genital corpuscles). The nerve ending are exquisitely sensitive to light touch, pain and temperature. Sensory traffic from the rectum and anal canal is conveyed to the spinal cord by unmyelinated small C fibers and larger A fibers11.
APPLIED PHYSIOLOGY
Ideally speaking, one should describe the function of each component of the pelvic floor muscle individually; however no such information is available. Broadly, the pelvic floor muscles can be considered to have 2 important functions. They provide, 1; support or “floor” to the pelvic viscera and 2; constrictor functions to the urethra, vagina and anal canal. We will describe the role of the pelvic floor muscles on the rectum and anal canal in detail and will touch on their role in the closure function of the vagina. Furthermore, it is quite likely that the puborectalis muscle plays an important role in the urethral closure mechanism, however more studies are needed in this area. In cadavers, the pelvic floor is shaped like a basin but in living individuals it is shaped like a dome36, 37. Why is that the case? Muscles in general have relatively simple function; they shorten as they contract. Generally, the insertion point of the muscle moves towards the point of the origin (sphincter muscles being an exception). In the case of pubococcygeus, ileococcygeus and ischiococcygeus, such an action results in the movement of coccyx anteriorly (ventrally) toward the pubic bone38. In fact, during pelvic floor contraction the coccyx moves ventrally and cranially. The change in the shape of the pelvic floor during contraction, from a basin to dome, is due to the shortening of the pubococcygeus, ileococcygeus and ischiococcygeus muscles. At the same time, conversion from “basin” to the “dome” lifts the pelvic viscera (including the rectum) in the cranial direction and provides mechanical support or “ floor” to the rectum and other pelvic floor viscera. Therefore, it is likely that the weakness of these muscles result in perineal descent. Decent of the pelvic visceral organs (including rectum) can be measured in the radiological studies (MRI or barium defecography) by determining the location of the anorectal angle in relationship with the pubococcygeus line39, 40. The latter is an imaginary line connecting the lower edge of pubic symphysis and the tip of coccyx. In normal individuals, the anorectal angle is located either cranial or very close to the pubococcygeal line and it moves below the pubococcygeal line with the descending perineal syndrome or weakness of the pelvic floor muscle. There is general consensus that the IAS and EAS are the major constrictors of anal canal. The puborectalis muscle is generally felt to be important in maintenance of the anorectal angle27, 41. Contraction of puborectalis muscle results in an acute anorectal angle and relaxation (during defecation) causes this angle to become obtuse. The anorectal angle can be measured with (barium defecography)42 or MR imaging27. However, as described in the following paragraphs, recent studies show that the puborectalis muscle is actually involved in the anal canal closure mechanism, i.e., in the genesis of anal canal pressure33, 43.
ANAL CANAL PRESSURE
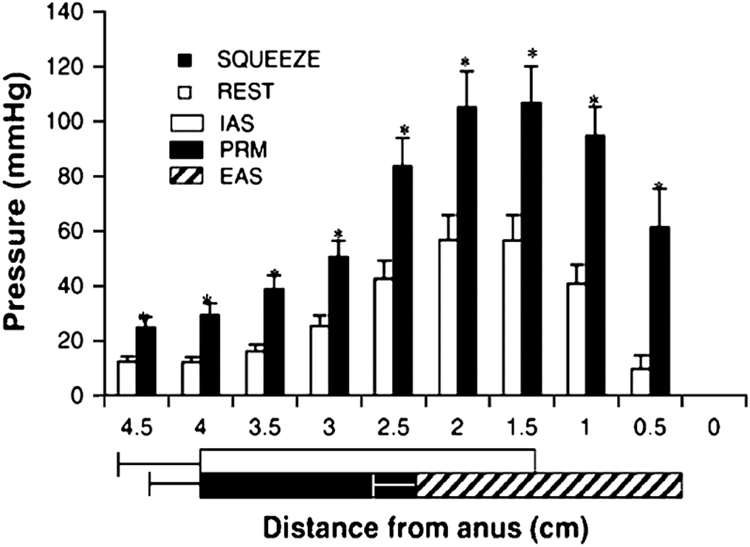
Anal canal pressure is a major determinant of the strength of anal continence mechanism and therefore its brief discussion is extremely relevant. Anal canal pressure can be measured with perfusion manometry (using either side hole or sleeve sensor), solid-state transducers or more recently with large number of closely spaced array of pressure sensors (high resolution manometry)29. Furthermore, the pressures can be displayed in the form of colored topographical (contour) plots, which are convenient to visualize. Classical studies by Duthie have shown that the majority of the resting pressure (70–80%) in the anal canal is related to the IAS and the remainder due to the EAS44. With voluntary anal squeeze, the increase in the anal canal pressure is mostly due to the external anal sphincter. Anatomical and functional studies, using simultaneous 3 D ultrasound imaging and side hole perfusion manometry have provided novel insights into the genesis of anal canal pressure43. Based on the 3D-US images one can determine the precise length and the anatomical relationship of the IAS, EAS and puborectalis muscle and then locate the anal canal pressures in relationship with these anatomical structures. These studies reveal that in the proximal part of the anal canal the closure pressures are related to the contraction of IAS and puborectalis muscle, in the middle, to the contraction of the EAS and in the distal part to the contraction of the EAS only (figure 9, 10).
Figure 9.
Anal canal pressures along the length of the canal and its relationship with anatomical structures: Anal canal pressure was measured using the station pull through technique. Each bar represents mean+SE from the 17 subjects. Note the baseline pressure and the squeeze pressures at each station. The pressures during squeeze at all stations are significantly higher than at rest (p<0.005). Also note, the location of Internal anal sphincter (IAS), puborectalis (PRM) and external anal sphincter (EAS) along the length of the anal canal. Obtained from author
Figure 10.
Ultrasound images of the anal canal in the sagittal and axial planes with a water filled bag placed in the anal canal: the sagittal image shows the anal canal along its entire length. Axial images at various locations along the length of anal canal allow visualization of various components of the anal closure mechanism. Axial images at R=rectum, 1=Puborectalis (PRM) & Internal sphincter (IAS), 2 = PRM, IAS, and external anal sphincter (EAS), 3 = IAS & EAS, 4 = EAS only. Obtained from author
VAGINAL HIGH-PRESSURE ZONE
How does puborectalis, a “U” shaped muscle increases, the anal canal pressure? The 2 anterior limbs of puborectalis muscle are attached to the 2 pubic rami and posteriorly they join each other behind the anal canal. Contraction of the puborectalis muscle lifts up the anal canal in the ventral or anterior direction and in so doing causes compression of the anal canal, vagina and urethra against the back of pubic symphsis (figure 11). If the above were true, there would be a high-pressure zone in the vagina, which is indeed true45. Pressure characteristics of the vaginal high pressure zone reveal that the anterior and posterior pressure in the vagina are higher than the lateral pressure, which suggest that vagina is compressed in the anterior - posterior direction by the puborectalis muscle. Three-dimensional US images show that the pelvic floor hiatus becomes smaller and larger with the contraction and relaxation of the puborectalis muscle, respectively24, 46. Pudendal nerve block increases dimensions of the pelvic floor hiatus and decreases vaginal pressure24. Distension of the vagina increases the anterior-posterior length of the puborectalis muscle and allows it to contract stronger (based on the length tension principle). Anal canal pressure in the proximal part of the anal canal (part surrounded by the puborectalis muscle) and not the distal part (surrounded by the EAS) increases with vaginal distension47.
Figure 11.
Pelvic Floor Hiatus Captured from the 3D ultrasound images at rest and during a pelvic floor contraction: Note that with contraction the hiatus becomes smaller and the puborectalis muscle moves towards the pubic symphsis. The anterior motion of the puborectalis muscle compresses, anal canal, vagina and urethra against the back of pubic symphsis, which constitutes the constrictor function of pelvic diaphragm. Obtained from author
Since vagina does not possess any intrinsic sphincter mechanism, the vaginal high-pressure zone is entirely related to the puborectalis muscle. The significance of the latter finding is that one can easily assess the puborectalis muscle function using vaginal manometry. It is likely that future studies will use this important understanding to further define the role of puborectalis muscle in fecal continence, incontinence, and other pelvic floor disorders.
Pelvic Floor Muscles and Fecal Incontinence
The etiology of fecal incontinence is multi-factorial and can be broadly divided into problems related to, 1; diarrhea or excessive amount of liquid stools, 2; reservoir or rectal dysfunction and 3; anal canal closure dysfunction. As discussed in the previous paragraphs, it is quite clear that the three separate and distinct anatomical structures, IAS, EAS and puborectalis muscle, guard the anal canal opening (triple security). Why three? Does this represent redundancy or is it that a fine orchestration of these three structures is crucial in keeping continence under different circumstances and for different rectal contents (air, liquid and solids)? Further studies are needed to prove or disprove these points. Read and colleagues in 1980’s, based on the anal canal pressure studies, found that the dysfunction of EAS is the most common cause of fecal incontinence48. A small subset of patients were found to have a defective IAS as well49. Endoanal ultrasound imaging studies of Sultan and colleagues found anatomical defects in the EAS muscle of 35% of women, following vaginal delivery50. The latter also suggests that anatomical defects of the EAS are one of the most common causes of fecal incontinence. However, more recent studies suggest a “multi hit hypothesis” in the genesis of fecal incontinence. Fernandez-Fraga used a novel instrument “perineal dynamometer” to study the pelvic floor function in patients with fecal incontinence51. They found that patients have functional defect in more than one muscle of anal continence and the severity of fecal incontinence was related to the composite effect of damage to the 3 continence muscles. Biofeedback therapy resulted in improvement of fecal incontinence symptoms and the improvement correlated best with the improvement in levator ani function, rather than with the improvement in the IAS, EAS pressure. A study by Bharucha et al28 confirmed findings of Fernandez Fraga and their study lends further credence to the “multi-hit hypothesis” of fecal incontinence.
Studies by Delancey52 and Dietz 53 show that anatomical disruptions of the puborectalis muscle are quite common following childbirth (20–35%). However, it is clear that all these subjects do not have symptoms of fecal incontinence. Our studies in asymptomatic multiparous women confirm findings of Delancey and Dietz33. We believe that further studies are required to determine the relationship between anatomical disruptions as seen on the imaging studies and functional impairment of puborectalis muscle function. However, it is clear that patients with fecal incontinence have defects in more than one muscle of continence and the symptoms are more severe in patients with defects in the multiple muscles.
Pelvic Floor Muscles and Constipation
Constipation affects 20–30% of the adult population in the United States54 and it’s etiology, similar to that of fecal incontinence, is multi-factorial. Broadly, there are 2 major types of constipation, 1; slow transit type in which the movement of fecal material through the colon is slow and 2; outlet obstruction type, in which patient has trouble evacuating rectal contents. Hirschprung’s disease, characterized by failure if caudal migration of myenteric plexus and may be considered as a cause of outlet obstruction type of constipation. However, Hirschsprung’s disease is uncommon in adults. Outlet obstruction, secondary to pelvic floor dysfunction accounts for 50% or more cases of constipation in adults55. Originally described by Preston and Lennard-Jones in 1985 as anismus56, the entity has received several names, i.e., pelvic floor dyssynergia, paradoxical puborectalis muscle contraction, paradoxical sphincter contraction and dyssynergic defecation55. Normally, during the act of defecation or Valsalva maneuver the respiratory diaphragm and abdominal wall contract together, which results in an increase in the intra-abdominal and rectal pressure. Simultaneously, there is relaxation of the pelvic floor muscles and anal sphincter muscles during defecation. Based on the rectal and anal sphincter pressure recordings, Rao categorized dyssynergic defecation disorders into 3 different types. Type 1 – increase in the rectal pressure and anal sphincter contraction, Type 2 – no increase in the rectal pressure and sphincter contraction and Type 3 – increase in the rectal pressure but either absent or incomplete sphincter relaxation55. Dyssynergic defecation usually acquired but in some cases the symptoms are present from childhood, which suggests that the individual never “learned the defecation process” correctly.
Paradoxical pelvic floor contraction can be recognized on the anal sphincter recording, electromyographic recordings (using anal plug electrodes or cutaneous electrodes) and imaging studies. The latter can be performed using X ray fluoroscopy (barium defecography), CT fluoroscopy and magnetic resonance imaging (MRI). During the act of defecation two events occur in the pelvic floor muscles, 1; pelvic floor descends and, 2; pelvic floor hiatus becomes larger. The descent of pelvic floor muscles is seen as a drop in the anorectal angle to below the pubo-coccygeal line (an imaginary line connecting the lower end of pubic symphsis and coccyx) and widening of the pelvic floor hiatus (also seen as an increase in the anorectal angle). With pelvic floor contraction, the anorectal angle moves cranially and ventrally. The reverse occurs during defecation. In patients with constipation, MRI defecography studies show heterogeneity of abnormalities of the abdominal wall contraction, pelvic floor descent and puborectalis muscle relaxation40. The most important finding in these studies is that the puborectalis muscle either does not relax or it does so incompletely. The latter results in either no change or a slight decrease in the anorectal angle. The advantage of MRI defecography is that it allows clear visualization of the pelvic viscera and various other anatomical abnormalities associated with pelvic floor disorders, e.g., rectocele, cystocele, rectal intussusception and prolapse. Recent studies show that biofeedback treatment for constipation is quite effective in treating constipation related to the pelvic floor muscle dysfunction and results in amelioration of the physiological muscle abnormalities54, 57.
Summary and Conclusions
Pelvic floor muscles have two important functions; they provide, 1; physical support to the pelvic viscera and, 2; constrictor mechanism to the anal canal, vagina and urethra. Newer imaging and physiological studies strongly suggest that these two functions of the pelvic floor are quite distinct and are likely related to different components of the pelvic floor muscles. The pubococcygeus, ileococcygeus and ischiococcygeus most likely provide the physical support or act as a “floor” for the pelvic viscera. On the other hand, the puborectalis muscle provides the constrictor function to the anal canal, vagina and urethra.
The urethra and anal canal, each has two constrictors or sphincters of their own. In the case of anal canal these are the IAS and EAS, and in the case of urethra they are the smooth muscle sphincter (located at the bladder neck) and rhabdo-sphincter (external urethral sphincter). Based on the physiologic studies, it appears that the puborectalis muscle is the 3rd constrictor or the sphincter of anal canal. Future studies are likely to reveal that puborectalis muscle serves as a constrictor for the urethra as well. Vagina, on the other hand, has only one constrictor mechanism, which is solely provided by the puborectalis portion or the pelvic floor muscle. We believe that puborectalis muscle is the common link between gastroenterologist, colorectal surgeon, urologist and urogynecologist, the specialties of medicine taking care of patients with pelvic floor disorders.
Pelvic floor disorders are many and are generally lumped together. However, it may be possible to broadly sub-classify them into disorders of pelvic floor support (prolapse, descending perineal syndrome) and constrictor function (urinary and fecal incontinence). Furthermore, these disorders may be further divided into dysfunctions of pelvic floor contraction (fecal and urinary incontinence) and relaxation (constipation and urinary retention). As the clear picture of functional anatomy of pelvic floor muscles emerges, it is imminent that different components of the pelvic floor muscles will be implicated in different pelvic floor disorders. With such a functional classification “splitter approach” our hope is that it may be possible to target specific therapeutic strategies to treat specific pelvic floor muscle disorders more effectively.
Acknowledgments
Financial supported by: NIH RO1 - DK60733
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Varuna Raizada, Address: VA Health Care Center (111D), 3350, La Jolla Village Dr, San Diego, California, 92161, Tel: (858) 552-7556, Fax: (858) 552-4327, Email: drvarunaraizada@yahoo.com
Ravinder K. Mittal, Address: VA Health Care Center (111D), 3350, La Jolla Village Dr, San Diego, California, 92161, Tel: (858) 552-7556, Fax: (858) 552-4327, Email: rmittal@ucsd.edu
Bibliography
- 1.Fritsch H, Brenner E, Lienemann A, Ludwikowski B. Anal sphincter complex: reinterpreted morphology and its clinical relevance. Dis Colon Rectum. 2002;45(2):188–194. doi: 10.1007/s10350-004-6144-x. [DOI] [PubMed] [Google Scholar]
- 2.Fritsch H, Aigner F, Ludwikowski B, et al. Epithelial and muscular regionalization of the human developing anorectum. Anat Rec (Hoboken) 2007;290(11):1449–1458. doi: 10.1002/ar.20589. [DOI] [PubMed] [Google Scholar]
- 3.Dyck PJ, Thomas PK. Autonomic and somatic systems to the anorectum and pelvic floor. 4th ed. Philadelphia PA: Elsvier Saunders; 2005. [Google Scholar]
- 4.Rattan S. The internal anal sphincter: regulation of smooth muscle tone and relaxation. Neurogastroenterol Motil. 2005;17 Suppl 1:50–59. doi: 10.1111/j.1365-2982.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 5.Goyal RK, Hirano I. The enteric nervous system. N Engl J Med. 1996;334:1106–1115. doi: 10.1056/NEJM199604253341707. [DOI] [PubMed] [Google Scholar]
- 6.Santorini J. Septemdecim tabulae. 1715 [Google Scholar]
- 7.Bogduk N. Issues in anatomy: the external anal sphincter revisited. Aust N Z J Surg. 1996 Sep;66:626–629. doi: 10.1111/j.1445-2197.1996.tb00834.x. [DOI] [PubMed] [Google Scholar]
- 8.Ayoub SF. Anatomy of the external anal sphincter in man. Acta Anat (Basel) 1979;105:25–36. doi: 10.1159/000145103. [DOI] [PubMed] [Google Scholar]
- 9.Shafik A. A new concept of the anatomy of the anal sphincter mechanism and the physiology of defecation. The external anal sphincter: a triple-loop system. Invest Urol. 1975;12:412–419. [PubMed] [Google Scholar]
- 10.Peschers UM, DeLancey JO, Fritsch H, Quint LE, Prince MR. Cross-sectional imaging anatomy of the anal sphincters. Obstet Gynecol. 1997;90(5):839–844. doi: 10.1016/S0029-7844(97)00406-7. [DOI] [PubMed] [Google Scholar]
- 11.Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterol Motil. 2006;18(7):507–519. doi: 10.1111/j.1365-2982.2006.00803.x. [DOI] [PubMed] [Google Scholar]
- 12.Stoker J, Halligan S, Bartram CI. Pelvic floor imaging. Radiology. 2001;218:621–641. doi: 10.1148/radiology.218.3.r01mr26621. [DOI] [PubMed] [Google Scholar]
- 13.Taylor BM, Beart RW, Jr., Phillips SF. Longitudinal and radial variations of pressure in the human anal sphincter. Gastroenterology. 1984;86:693–697. [PubMed] [Google Scholar]
- 14.Vesalius A. De humnai corporis fabrica libri septum. 2 ed. 1555. [PubMed] [Google Scholar]
- 15.Von Behr A. Handbook of Human Anatomy. Philadephia: Lindsay & Blakiston; 1847. [Google Scholar]
- 16.Meyer G. Lehrbuch der Anatomie des Menschem. 1861 [Google Scholar]
- 17.Holl M. Handbuch des Anatomie. Jena: Fischer; 1897. [Google Scholar]
- 18.Thompson P. The Myology of the Pelvic Floor. Newton: McCorquoddale; 1899. [Google Scholar]
- 19.Sappey P. Traite d, Anatomie Descriptive. (2nd ed) 1739 [Google Scholar]
- 20.Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Ann R Coll Surg Engl. 1974;54:244–252. [PMC free article] [PubMed] [Google Scholar]
- 21.DeLancey JO, Delmas V. Groos Anatomy and Functional Anatomy of the Pelvic Floor. Philadelphia: Elsevier Saunders; 2004. [Google Scholar]
- 22.Kearney R, Sawhney R, DeLancey JO. Levator ani muscle anatomy evaluated by origin-insertion pairs. Obstet Gynecol. 2004;104:168–173. doi: 10.1097/01.AOG.0000128906.61529.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Percy JP, Neill ME, Swash M, Parks AG. Electrophysiological study of motor nerve supply of pelvic floor. Lancet. 1981;1:16–17. doi: 10.1016/s0140-6736(81)90117-3. [DOI] [PubMed] [Google Scholar]
- 24.Guaderrama NM, Liu J, Nager CW, et al. Evidence for the innervation of pelvic floor muscles by the pudendal nerve. Obstet Gynecol. 2005 Oct;106:774–781. doi: 10.1097/01.AOG.0000175165.46481.a8. [DOI] [PubMed] [Google Scholar]
- 25.Li D, Guo M. Morphology of the levator ani muscle. Dis Colon Rectum. 2007;50:1831–1839. doi: 10.1007/s10350-007-0265-y. [DOI] [PubMed] [Google Scholar]
- 26.Hoyte L, Jakab M, Warfield SK, Shott S, Flesh G, Fielding JR. Levator ani thickness variations in symptomatic and asymptomatic women using magnetic resonance-based 3-dimensional color mapping. Am J Obstet Gynecol. 2004;191:856–861. doi: 10.1016/j.ajog.2004.06.067. [DOI] [PubMed] [Google Scholar]
- 27.Fletcher JG, Busse RF, Riederer SJ, et al. Magnetic resonance imaging of anatomic and dynamic defects of the pelvic floor in defecatory disorders. Am J Gastroenterol. 2003;98:399–411. doi: 10.1111/j.1572-0241.2003.07235.x. [DOI] [PubMed] [Google Scholar]
- 28.Bharucha AE, Fletcher JG, Harper CM, et al. Relationship between symptoms and disordered continence mechanisms in women with idiopathic faecal incontinence. Gut. 2005;54:546–555. doi: 10.1136/gut.2004.047696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bharucha AE, Fletcher JG. Recent advances in assessing anorectal structure and functions. Gastroenterology. 2007;133:1069–1074. doi: 10.1053/j.gastro.2007.08.051. [DOI] [PubMed] [Google Scholar]
- 30.Dietz HP. Ultrasound imaging of the pelvic floor. Part II: three-dimensional or volume imaging. Ultrasound Obstet Gynecol. 2004;23:615–625. doi: 10.1002/uog.1072. [DOI] [PubMed] [Google Scholar]
- 31.Dietz HP. Ultrasound imaging of the pelvic floor. Part I: two-dimensional aspects. Ultrasound Obstet Gynecol. 2004 Jan;23:80–92. doi: 10.1002/uog.939. [DOI] [PubMed] [Google Scholar]
- 32.Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–585. doi: 10.1002/uog.1899. [DOI] [PubMed] [Google Scholar]
- 33.Jung SA, Pretorius DH, Weinstein M, Nager CW, Den-Boer D, Mittal RK. Closure Mechanism of the Anal Canal in Women: Assessed by Three-Dimensional Ultrasound Imaging. Dis Colon Rectum. 2008;51:932–939. doi: 10.1007/s10350-008-9221-8. [DOI] [PubMed] [Google Scholar]
- 34.Jung SA, Pretorius DH, Padda BS, et al. Vaginal high-pressure zone assessed by dynamic 3-dimensional ultrasound images of the pelvic floor. Am J Obstet Gynecol. 2007;197:52, e51–e57. doi: 10.1016/j.ajog.2007.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinstein MM, Pretorius DH, Jung S-A, Nager C, Mittal RK. Transcutaneous 3-Dimensional Ultrasound Imaging: A Novel Technique to Detect Anatomical Defects in the Muscles of Anal Sphincter Complex. Clinical Gastroenterology and Hepatology. doi: 10.1016/j.cgh.2008.08.019. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo M, Li D. Pelvic floor images: anatomy of the levator ani muscle. Dis Colon Rectum. 2007;50:1647–1655. doi: 10.1007/s10350-007-0262-1. [DOI] [PubMed] [Google Scholar]
- 37.Hjartardottir S, Nilsson J, Petersen C, Lingman G. The female pelvic floor: a dome--not a basin. Acta Obstet Gynecol Scand. 1997;76:567–571. doi: 10.3109/00016349709024586. [DOI] [PubMed] [Google Scholar]
- 38.Bo K, Lilleas F, Talseth T, Hedland H. Dynamic MRI of the pelvic floor muscles in an upright sitting position. Neurourol Urodyn. 2001;20:167–174. doi: 10.1002/1520-6777(2001)20:2<167::aid-nau19>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 39.Singh K, Jakab M, Reid WM, Berger LA, Hoyte L. Three-dimensional magnetic resonance imaging assessment of levator ani morphologic features in different grades of prolapse. Am J Obstet Gynecol. 2003;188:910–915. doi: 10.1067/mob.2003.254. [DOI] [PubMed] [Google Scholar]
- 40.Bharucha AE, Fletcher JG, Seide B, Riederer SJ, Zinsmeister AR. Phenotypic variation in functional disorders of defecation. Gastroenterology. 2005;128:1199–1210. doi: 10.1053/j.gastro.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 41.Locke GR, 3rd, Pemberton JH, Phillips SF. AGA technical review on constipation. American Gastroenterological Association. Gastroenterology. 2000;119:1766–1778. doi: 10.1053/gast.2000.20392. [DOI] [PubMed] [Google Scholar]
- 42.Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW. Defecography in normal volunteers: results and implications. Gut. 1989;30:1737–1749. doi: 10.1136/gut.30.12.1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu J, Guaderrama N, Nager CW, Pretorius DH, Master S, Mittal RK. Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am J Gastroenterol. 2006;101:1092–1097. doi: 10.1111/j.1572-0241.2006.00596.x. [DOI] [PubMed] [Google Scholar]
- 44.Duthie HL, Watts JM. Contribution of the External Anal Sphincter to the Pressure Zone in the Anal Canal. Gut. 1965;6:64–68. doi: 10.1136/gut.6.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guaderrama NM, Nager CW, Liu J, Pretorius DH, Mittal RK. The vaginal pressure profile. Neurourol Urodyn. 2005;24:243–247. doi: 10.1002/nau.20112. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein MM, Jung SA, Pretorius DH, Nager CW, den Boer DJ, Mittal RK. The reliability of puborectalis muscle measurements with 3-dimensional ultrasound imaging. Am J Obstet Gynecol. 2007;197:68, e61–e66. doi: 10.1016/j.ajog.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 47.Padda BS, Jung SA, Pretorius D, Nager CW, Den-Boer D, Mittal RK. Effects of pelvic floor muscle contraction on anal canal pressure. Am J Physiol Gastrointest Liver Physiol. 2007;292:G565–G571. doi: 10.1152/ajpgi.00250.2006. [DOI] [PubMed] [Google Scholar]
- 48.Read NW, Haynes WG, Bartolo DC, et al. Use of anorectal manometry during rectal infusion of saline to investigate sphincter function in incontinent patients. Gastroenterology. 1983;85:105–113. [PubMed] [Google Scholar]
- 49.Sun WM, Read NW, Donnelly TC. Impaired internal anal sphincter in a subgroup of patients with idiopathic fecal incontinence. Gastroenterology. 1989;97:130–135. doi: 10.1016/0016-5085(89)91425-x. [DOI] [PubMed] [Google Scholar]
- 50.Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 23. 1993;329:1905–1911. doi: 10.1056/NEJM199312233292601. [DOI] [PubMed] [Google Scholar]
- 51.Fernandez-Fraga X, Azpiroz F, Malagelada JR. Significance of pelvic floor muscles in anal incontinence. Gastroenterology. 2002;123:1441–1450. doi: 10.1053/gast.2002.36586. [DOI] [PubMed] [Google Scholar]
- 52.DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46–53. doi: 10.1016/s0029-7844(02)02465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–712. doi: 10.1097/01.AOG.0000178779.62181.01. [DOI] [PubMed] [Google Scholar]
- 54.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–664. doi: 10.1053/j.gastro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 55.Olsen AL, Rao SS. Clinical neurophysiology and electrodiagnostic testing of the pelvic floor. Gastroenterol Clin North Am. 2001;30:33–54. doi: 10.1016/s0889-8553(05)70166-7. v-vi. [DOI] [PubMed] [Google Scholar]
- 56.Preston DM, Lennard-Jones JE. Anismus in chronic constipation. Dig Dis Sci. 1985;30:413–418. doi: 10.1007/BF01318172. [DOI] [PubMed] [Google Scholar]
- 57.Chiarioni G, Salandini L, Whitehead WE. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology. 2005;129:86–97. doi: 10.1053/j.gastro.2005.05.015. [DOI] [PubMed] [Google Scholar]