Abstract
The human herpes simplex virus (HSV) is highly pathogenic, with infections caused by two distinct antigenic types, HSV-1 and HSV-2. Differentiation of antibodies to these specific antigens can provide useful information for the diagnosis of subclinical or undiagnosed HSV-2 infections, as well as for reducing the risk of maternal transfer of HSV to the neonate. In this study, a multiplex assay capable of concurrent detection of HSV-1 and -2 immunoglobulin G (IgG) antibodies was compared to immunoblot, Western blot, and enzyme-linked immunosorbent assays. Agreement of the multiplex assay was 95% or greater (n = 332) for both HSV-1 and -2 compared to the three assays. Sensitivities for HSV-1 ranged from 94.9 to 97.9%, with specificities of 93 to 97%. For HSV-2, the sensitivity and specificity ranges were 92.6 to 98.9% and 98.3 to 98.7%, respectively. Our studies show that the multiplexed microsphere-based assay offers a sensitive and specific alternative method for the detection HSV-1 and -2 type-specific antibodies. Advantages of the multiplex assay include multiple results per assay, the inclusion of internal controls for each specimen, and higher throughput of results.
Herpes simplex virus (HSV) occurs worldwide and is one of the most common human pathogens. Infection with HSV produces a variety of clinical manifestations, ranging from mild stomatitis to potentially fatal viral encephalitis. There are two well-recognized species of HSV classified as HSV type 1 (HSV-1) and HSV type 2 (HSV-2). HSV-1 is most often associated with orofacial (mouth, lips, tongue, pharynx, and eyes) transmission and infection, with 70 to 80% seropositivity in U.S. adults (17). HSV-2 has classically been associated with neonatal infections and genital herpes. Genital infections with HSV-1, however, are increasing and now exceed 50% in certain populations (4, 8, 11, 14). Seropositivity for HSV-2 has been reported in 10 to 40% of U.S. adults (17).
Primary infections with either type of HSV give rise to both cell-mediated and humoral immune responses capable of neutralizing the virus and killing virus-infected cells. The immune response, however, cannot completely eliminate the virus, allowing recurrent outbreaks or persistent disease. Following primary infection, the virus colonizes the sensory neurons, where it remains latent and may reactivate at a later time (6).
Antibodies are produced against structural components of the virus, as well as the viral envelope, capsid, and internal proteins. Many of these antigens share common epitopes resulting in high cross-reactivity between HSV-1 and -2. Type-specific glycoproteins (gG-1 and gG-2) have been identified which allow for the discrimination of immunoglobulin G (IgG) antibodies to either HSV-1 or -2. Immunoassays based on these purified glycoproteins have been available for over 10 years and have now become the standard of use for HSV type-specific serology (3, 10, 12, 13, 15, 16). These type-specific assays allow accurate identification of asymptomatic HSV-2 infection in patients who pose a risk of transmission to their sexual partners, as many individuals are unaware that they are infected or do not recognize subtle or atypical symptoms. Type-specific assays can also aid in diagnosis and, hence, prevention of maternal transfer of HSV to the neonate. Mortality rates in untreated infants who develop disseminated infections can exceed 80% (7), with at least half of those who do survive developing permanent neurological impairment.
In this study, we evaluate the performance of a recently FDA-cleared multiplexed assay capable of identifying HSV-1 and -2 type-specific IgG antibodies in a single reaction. Results of the multiplexed assay were compared to commercially available enzyme-linked immunosorbent assay (ELISA) and immunoblotting. Discrepant results were resolved by additional testing by Western blotting (1).
MATERIALS AND METHODS
Clinical samples.
Three-hundred thirty-two serum samples originally sent to ARUP Laboratories for HSV type-specific testing by immunoblot IgG assay were included in this study. These samples were divided into five categories based on the initial immunoblot result. The first category consisted of 140 samples that were HSV-1 positive and HSV-2 negative. The second category comprised 34 samples that were HSV-1 negative and HSV-2 positive. The third category contained 56 samples that were positive for HSV-1 and HSV-2. The fourth category consisted of 88 samples that were negative for both HSV-1 and HSV-2. The fifth group included 14 samples that were considered either untyped or atypical by the immunoblot. Samples from the fifth group either had a positive herpesvirus common band with no positive HSV-1 or HSV-2 band (untyped) or a negative herpesvirus common band with either a positive HSV-1 or HSV-2 band (atypical). Samples were stored at 2 to 8°C until completion of the study. All patient samples included in this study were deidentified according to the University of Utah Institutional Review Board approved protocol (no. 7275) to meet Health Information Portability and Accountability Act patient confidentiality guidelines.
Commercial immunoassays.
All commercial assays included in this study were performed with strict adherence to the manufacturers’ instructions as detailed in the product inserts. All incubations were at room temperature (20 to 25°C). Pertinent details of the assays are described below.
Immunoblot testing.
HerpeSelect 1 and 2 immunoblot IgG assays were purchased from Focus Diagnostics (Cypress, CA). Nitrocellulose strips were spotted with four antigen bands: an anti-human serum control band, a herpesvirus common antigen band which is a blend of HSV-1 and HSV-2 viral antigens, a recombinant gG-1 (molecular mass, 35 to 40 kDa) antigen band, and a recombinant gG-2 antigen (molecular mass, 80 to 110 kDa) band. Patient samples and controls were diluted 1:101 and required 20 μl of each sample. The total time required to perform the assay and interpret the results was approximately 200 min. A band was considered positive or present if its intensity was equal to or greater than that of the gG-2 band on the positive control strip. Each strip must show a visible anti-human serum control band in order for that strip's results to be considered valid. Interpretation of the strips is given in Table 1.
TABLE 1.
Interpretation of the immunoblot HSV-1 and -2 IgG assaya
| Anti-human serum band | Herpesvirus common antigen band | gG-1 antigen band | gG-2 antigen band | Interpretation |
|---|---|---|---|---|
| − | +/− | +/− | +/− | Test not valid, sample repeated |
| + | + | + | − | Positive for HSV-1 |
| + | + | − | + | Positive for HSV-2 |
| + | + | + | + | Positive for HSV-1 and HSV-2 |
| + | + | − | − | Untyped |
| + | − | + | +/− | Atypical |
| + | − | +/− | + | Atypical |
+, positive antibody response; −, negative antibody response; +/-, positive or negative antibody response.
ELISA testing.
HerpeSelect IgG ELISAs were purchased from Focus Diagnostics. The microwells were coated with recombinant gG-1 (molecular mass, 35 to 40 kDa) and gG-2 (molecular mass, 80 to 110 kDa) antigens. Each patient sample, positive control, negative control, and calibrator was diluted 1:101 and required 5 μl of sample. The time required to perform the assay and interpret the results was approximately 140 min. The index value (IV) result for each specimen was determined by dividing the optical density (OD) by the mean OD of the calibrator. Samples with an IV of <0.90 were considered negative for HSV IgG antibodies, and samples with an IV of >1.10 were considered positive for HSV IgG antibodies, while samples with an IV ranging from 0.90 to 1.10 were considered equivocal.
The HSV 1&2 IgM assay was purchased from Diamedix Corporation (Miami, FL) and utilizes a combination of partially purified HSV-1 (MacIntyre strain) and HSV-2 (G-strain) antigens. This assay was used to test 11 discrepant samples to determine the possibility of an acute infection.
Multiplex testing.
The multiplex AtheNA Multi-Lyte HSV type-specific test system was provided by Inverness Medical-Clinical Product Group (Princeton, NJ). The assay employed recombinant gG-1 (molecular mass, 55 kDa) and gG-2 (molecular mass, 55 kDa) antigen-coupled microspheres, an additional microsphere to detect nonspecific binding, as well as four microspheres used as internal calibrators. Patient samples and controls had a final dilution of 1:105 and required 10 μl of sample. The assay took approximately 120 min to obtain the final result. Using Intra-Well Calibration Technology, internal calibration microsphere sets are used to convert raw fluorescence into arbitrary units. Reference ranges for the multiplex assay were as follows: <100 arbitrary units (AU)/ml, negative, indicating no detectable IgG antibody; 100 to 120 AU/ml, inconclusive, with the recommendation of testing of a second sample at a later date; >120 AU/ml, positive, indicating that the specimen is positive for IgG antibody.
Western blot testing.
To reconcile any results that were discrepant between the immunoblot, ELISA, and multiplex assay, 50 samples were sent to the University of Washington Medical Center (UWMC), Seattle, to be run on their HSV Western blot test (1). The Western blot assay is based on HSV-1 and -2-infected human fibroblasts which are then lysed, denatured, and electrophoresed on polyacrylamide gels. The antigens are then transferred onto nitrocellulose membranes, where they are reacted with patient sera which have been previously absorbed with HSV-1 and -2 antigens to increase specificity (1). The Western blot, therefore, measures antibody patterns to all of the HSV viral proteins, whereas the ELISA and multiplex assay are based on the two recombinant gG-1 and -2 proteins. The immunoblot assay is essentially the same with the recombinant glycoproteins spotted onto nitrocellulose, but it also contains an additional spotted common HSV antigen. The UWMC Western blot results were reported as positive for HSV-1, HSV-2, or both.
Statistical analysis.
Overall agreement, sensitivity, specificity, and 95% confidence intervals (CIs) were calculated using two-by-two contingency table analysis (5). Results from the ELISA and multiplex assay were compared to the immunoblot results. Samples with discrepant results were repeated in duplicate on the ELISA and multiplex assay and once on the immunoblot assay. The mean value of duplicate results was used for the final result for the ELISA and multiplexed assay if it was in agreement between replicates and differed from the original result. The repeated immunoblot result was interpreted by two medical technologists and the medical director of the laboratory. The consensus result of the three interpreters was used for the final result. Results that were still not in total agreement between the three assays were sent out for Western blot analysis, with this result used in calculations as the “WB Resolved” result. Samples with inconclusive results were not included in the calculations of clinical agreement, sensitivity, and specificity.
RESULTS
Comparison of multiplex assay to ELISA, immunoblot, and the Western blot resolved results.
The multiplex assay was initially analyzed by comparing it to the ELISA and immunoblot assays for antibodies to HSV-1 and -2. Agreement for HSV-1 between the multiplex assay and ELISA was 94.8%. Sensitivity and specificity were 95.8% and 93.4%, respectively (Table 2). Discrepant results were fairly evenly split, with the multiplex assay having nine positive results that were negative by ELISA and eight negative results that were positive by ELISA. The ELISA had a higher frequency of equivocal results, 1.5% (5 of 332) compared to the multiplex assay, which did not have any. For HSV-2, the multiplex assay had slightly higher agreement (96.9%) and specificity (98.7%) but lower sensitivity (92.6%) compared to the ELISA. The majority of the discrepant results (7) were positive by ELISA and negative by the multiplex assay. The multiplex assay reported 6 of 332 results as equivocal (1.8%), compared to the ELISA, which only had 1 equivocal result.
TABLE 2.
Correlation of the multiplex assay with ELISA
| Multiplex result | No. of samples with ELISA resulta:
|
||
|---|---|---|---|
| Positive | Negative | Equivocal | |
| HSV-1 | |||
| Positive | 182 | 9 | 1 |
| Negative | 8 | 128 | 4 |
| Equivocal | 0 | 0 | |
| HSV-2 | |||
| Positive | 88 | 3 | 0 |
| Negative | 7 | 227 | 1 |
| Equivocal | 2 | 4 | |
The respective agreement, sensitivity, and specificity were as follows: HSV-1, 94.8% (CI, 91.8 to 96.7%), 95.8% (CI, 93.2 to 97.4%), and 93.4% (CI, 89.9 to 95.7%); HSV-2, 96.9% (CI, 94.5 to 98.1%), 92.6% (88.5 to 94.6%), and 98.7% (97.0 to 99.5%).
When the multiplex assay was compared to the immunoblot assay, the sensitivity (97.9%) for HSV-1 improved compared to ELISA but the specificity (92.9%) was lower. (Table 3). Most of the discrepant results (10) were positive by the multiplex assay and negative by the immunoblot assay. For HSV-2, agreement (97.9%), sensitivity (96.7%), and specificity (98.3%) were all excellent for the multiplex assay compared to the immunoblot assay.
TABLE 3.
Correlation of the multiplex assay with the immunoblot assaya
| Multiplex result | No. of samples with immunoblot assay resulta:
|
||
|---|---|---|---|
| Positive | Negative | Equivocal | |
| HSV-1 | |||
| Positive | 188 | 10 | 0 |
| Negative | 4 | 130 | 0 |
| Equivocal | 0 | 0 | |
| HSV-2 | |||
| Positive | 87 | 4 | 0 |
| Negative | 3 | 232 | 0 |
| Equivocal | 2 | 4 | |
The respective agreement, sensitivity, and specificity were as follows: HSV-1, 95.8% (CI, 93.2 to 97.2% ), 97.9% (CI, 95.6 to 99.1%), and 92.9% (CI, 89.7 to 94.5%); HSV-2, 97.9% (CI, 95.7 to 98.9%), 96.7% (CI, 92.7 to 98.6%), and 98.3% (CI, 96.8 to 99.0%).
Of the 332 samples included in this study, there were 50 samples (15.1%) that were not in total agreement between multiplex assay, ELISA, and immunoblot assay. These 50 discrepant samples were sent to the UWMC for HSV-1 and -2 Western blot testing. The Western blot result was then used as the resolved result for the discrepant samples. The multiplex assay compared well to the Western blot resolved results for both HSV-1 and -2 (Table 4). For HSV-1, overall agreement was 95.8%, with a sensitivity of 94.9% and a specificity of 97.0%. Concordance between the multiplex assay and Western blot for HSV-2 was excellent, with an agreement of 98.8%, sensitivity of 98.9%, and specificity of 98.7%.
TABLE 4.
Correlation of the multiplex assay with the Western blot resolved result
| Multiplex result | No. of samples with Western blot resolved resulta:
|
||
|---|---|---|---|
| Positive | Negative | Equivocal | |
| HSV-1 | |||
| Positive | 188 | 4 | 0 |
| Negative | 10 | 130 | 0 |
| Equivocal | 0 | 0 | |
| HSV-2 | |||
| Positive | 88 | 3 | 0 |
| Negative | 1 | 234 | 0 |
| Equivocal | 2 | 4 | |
The respective agreement, sensitivity, and specificity were as follows: HSV-1, 95.8% (CI, 93.2 to 97.2%), 94.9% (CI, 92.8 to 96.1%), and 97.0% (CI, 93.8 to 98.7%); HSV-2, 98.8% (CI, 97.0 to 99.3%), 98.9% (CI, 95.5 to 99.8%), and 98.7% (CI, 97.5 to 99.1%).
Comparison of the multiplex assay, ELISA, and immunoblot assay to the Western blot resolved results.
A second analysis of the samples was conducted to determine how the three different commercial assays performed based on presumptive HSV-1 and -2 single infections or coinfections, as determined by the Western blot resolved result. Category 1 samples (n = 140) were HSV-1 positive and HSV-2 negative. The immunoblot assay had a concordance of 97.9%, with 137 of the 140 samples correctly reported as type 1 positive and type 2 negative (Fig. 1). Of the three immunoblot assay discrepant samples, one was reported as HSV-1 and -2 positive, while the other two were negative for both HSV-1 and -2. Concordance of the multiplexed assay for the category 1 samples was 94.3% (132 of 140), with 1 discrepant sample being HSV-1 and -2 positive and the remaining 7 samples having HSV-1- and -2-negative results. The ELISA had the lowest concordance for this category (92.1%), with three discrepant samples positive for HSV-1 and -2 and eight samples negative for both HSV-1 and -2.
FIG. 1.
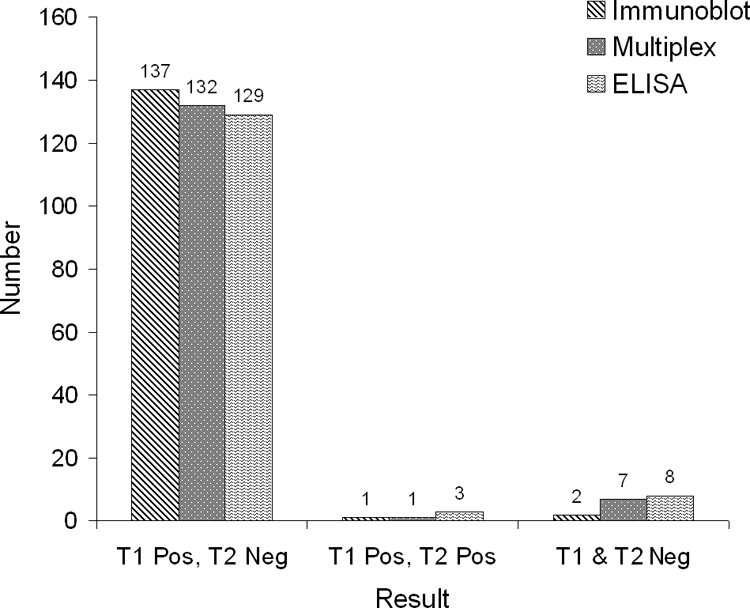
Analysis of category 1 Western blot resolved results (HSV-1 positive, HSV-2 negative) by the immunoblot assay, multiplex assay, and ELISA. n = 140. T1, HSV-1; T2, HSV-2; Pos, positive; Neg, negative.
The second category (n = 34) consisted of samples which were HSV-1 negative and HSV-2 positive. The immunoblot assay had a concordance of 97.1% (33 of 34), with one discrepant sample positive for both HSV-1 and -2 (Fig. 2). The multiplex assay correctly identified all 34 samples as HSV-1 negative and HSV-2 positive for a concordance of 100%. Concordance for the ELISA was only 91.2%, with three discrepant samples having positive results for both HSV-1 and -2.
FIG. 2.
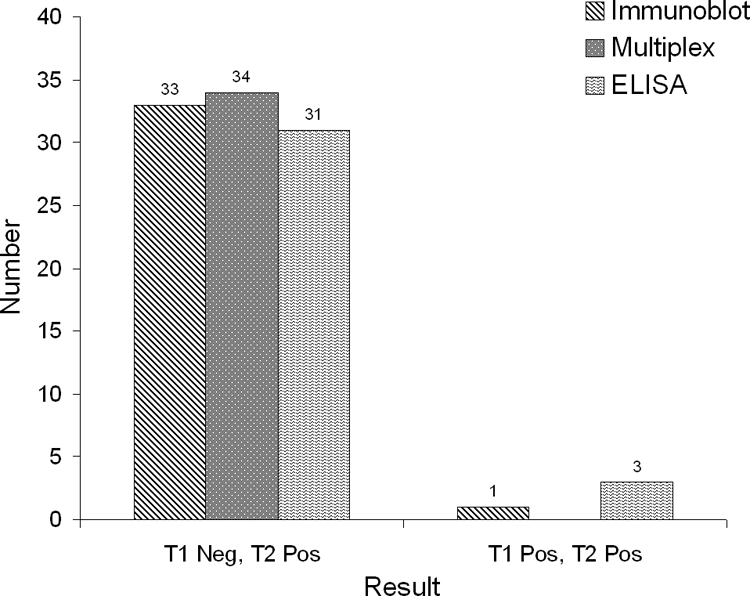
Analysis of category 2 Western blot resolved results (HSV-1 negative, HSV-2 positive) by the immunoblot assay, multiplex assay, and ELISA. n = 34. T1, HSV-1; T2, HSV-2; Pos, positive; Neg, negative.
Category 3 samples (n = 56) all had dual antibody responses to both HSV-1 and -2, once again according to the resolved Western blot results. Concordance of the immunoblot assay was 96.4%, with two discrepant samples that were HSV-1 positive but HSV-2 negative (Fig. 3). The multiplex assay had a total of three discrepant results: one HSV-1 positive and HSV-2 negative and two that were HSV-1 negative and HSV-2 positive, for a concordance of 94.6%. The ELISA had the best concordance for this subset at 100%.
FIG. 3.
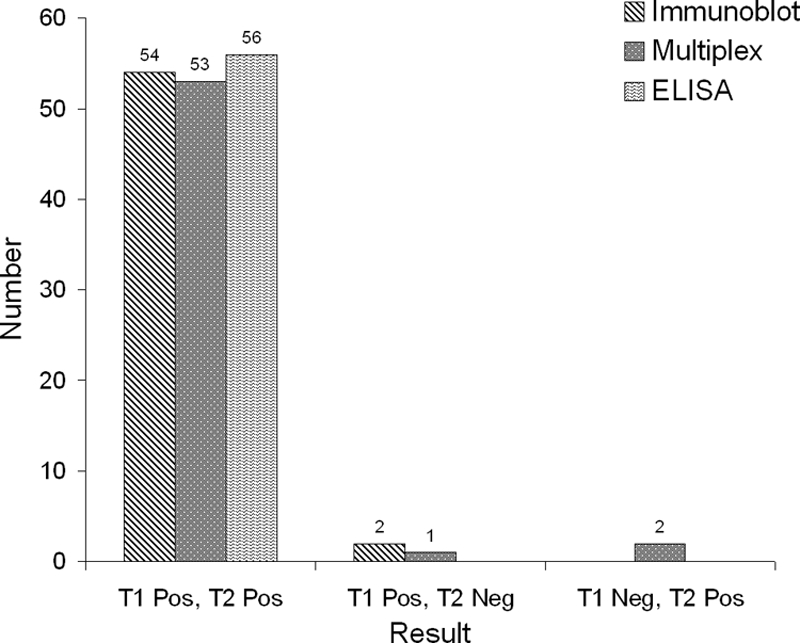
Analysis of category 3 Western blot resolved results (HSV-1 and HSV-2 positive) by the immunoblot assay, multiplex assay, and ELISA. n = 56. T1, HSV-1; T2, HSV-2; Pos, positive; Neg, negative.
The fourth category contained 88 samples that were negative for antibodies to both HSV-1 and -2. Both the immunoblot and multiplex assays had concordances of 95.5%, each having three HSV-1-positive, HSV-2-negative discrepant samples and one HSV-1-negative, HSV-2-positive discrepant sample. Only two of these four discrepant results were the same sample, however. The ELISA only had two discrepant results: one HSV-1 positive, HSV-2 negative and one HSV-1 negative, HSV-2 positive, for a concordance of 97.7%. There was one common discrepant sample between the three commercial assays that was HSV-1 negative and HSV-2 positive but negative for both HSV species by Western blotting.
A fifth subset of discrepant samples was identified which was unique to the immunoblot assay due to the inclusion of a common HSV (not type specific) antigen band. This category consisted of 11 “untyped” samples and three “atypical” samples (Table 1). A number of samples with untyped results (HSV common band positive but negative for the type-specific bands) would be expected as the common HSV antigen consists of a mixture of whole-virus lysates with components of the virus known to cross-react with other herpesviruses. Three of these untyped samples, however, did have reactivity to the type-specific glycoproteins (two were gG-1 positive by multiplex assay, and one was gG-2 positive by the ELISA). Of the two gG-1-positive samples by the multiplex assay, one was also HSV-1 positive by Western blotting, and the other was HSV-1 and -2 negative. The sample that was gG-2 positive by ELISA had an “atypical” result by Western blotting. To determine if these patients with untyped immunoblot assay results had an acute or early infection, to which antibodies to the gG-1 and -2 antigens had not yet developed (2), HSV IgM serology was performed. Results from an HSV-1 and -2 IgM combined ELISA found 3 of the 11 untyped samples to be IgM positive. Two of these IgM-positive samples had IVs just above the positive cutoff value, while the third was well above the cutoff value.
The three samples classified as atypical (common band negative, HSV-1 or -2 positive) by the immunoblot assay all showed reactivity to either gG-1 or gG-2 by the ELISA, but only one had reactivity (gG-2) in the multiplex assay. The Western blot results for these three samples were as follows: (i) HSV-1 negative, HSV-2 atypical; (ii) HSV-1 positive, HSV-2 negative; and (iii) HSV-1 and -2 negative.
DISCUSSION
While the Western blot is still considered the “gold standard” for type-specific serological diagnosis of HSV, the cumbersome nature of the assay, along with the unavailability of a commercial assay, make it impractical for routine clinical laboratory use. It is for this reason that Western blot type-specific HSV serology has been widely replaced by ELISA and immunoblot assays based on the recombinant gG-1 and gG-2 proteins, allowing cost-effective and high-throughput testing. The greatest advantage of these type-specific assays is in their aid with the differentiation of HSV-1 and -2 infections, and therefore the testing of antibodies to both HSV species is commonly requested by the physician. The immunoblot assay allows for the determination of antibody responses to both antigens in a single reaction but suffers from some of the same limitations as the Western blot assay. These include being labor intensive with low throughput, as well as manual and subjective interpretation of the presence or absence of bands according to their relative intensity. The ELISA eliminates many of these limitations, allowing for higher throughput and automation, along with objective result interpretation based on index values determined by the ODs of the patient sample compared to a known calibrator value. The remaining disadvantage of ELISAs is that HSV-1 and -2 antibody analysis must be performed on separate assays. The HSV multiplex assay offers the same advantages as ELISA, but now results for both HSV-1 and -2 can be accomplished in a single reaction. In this study, we evaluated a recently FDA-cleared HSV multiplex assay in comparison to well-established immunoblot and ELISA methods with Western blot analysis employed for discrepant resolution.
Based on the CIs calculated for the agreement, sensitivity, and specificity of the multiplex assay compared to the ELISA and immunoblot assay, it can be concluded that all three assays performed equally well. Concordance of the three commercial assays to the Western blot resolved results was also very good. Performance of the multiplex assay compared to the Western blot resolved result provided a less-biased analysis as the ELISA and immunblot assay were from the same manufacturer who employed the same recombinant antigen for both assays. It was somewhat surprising than that there was not a greater concordance between the ELISA and immunoblot assay. For single HSV infections (either type 1 or 2 positive), the immunoblot assay compared better to the Western blot resolved result than the ELISA (Fig. 1 and 2). For the samples with dual HSV-1 and -2 infections and seronegative samples, the ELISA compared better to the Western blot assay than the immunoblot assay (Fig. 3 and 4). The concordance of the multiplex assay to the Western blot mostly fell between the ELISA and immunoblot assay.
FIG. 4.
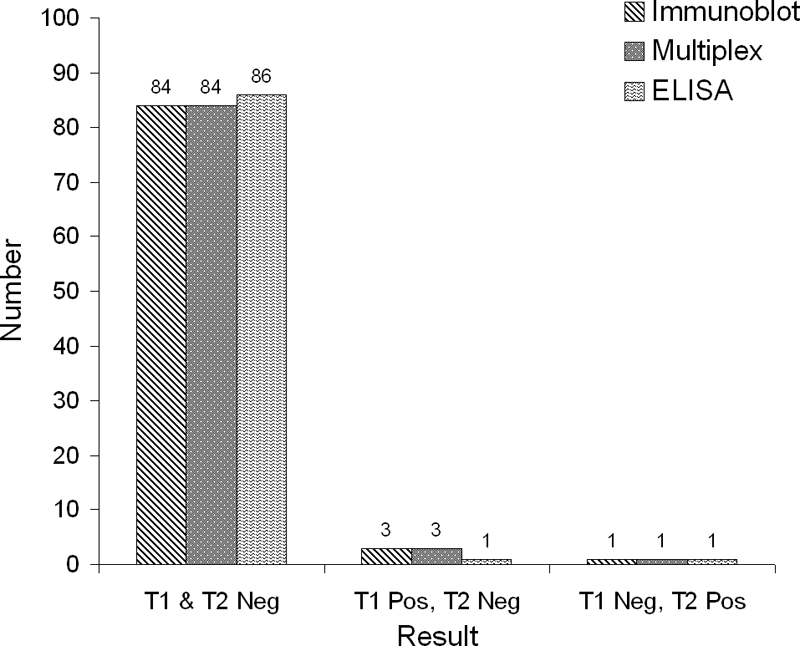
Analysis of category 4 Western blot resolved results (HSV-1 and HSV-2 negative) by the immunoblot assay, multiplex assay, and ELISA. n = 88. T1, HSV-1; T2, HSV-2; Pos, positive; Neg, negative.
In theory, the inclusion of the common antigen band in the immunoblot assay would provide advantages over the ELISA and multiplex assay, which are based on the recombinant gG proteins alone. Glycoprotein G is not an essential protein for HSV replication, and infections may occur with glycoprotein G-deficient virus. Liljeqvist et al. reported about 0.2% (5/2,400) of HSV isolates were gG deficient (9). Additionally, individuals infected with HSV may not exhibit detectable IgG antibody to the glycoprotein 1 and 2 type-specific HSV antigens in the early stages of infection. Western blot studies have shown that antibody to glycoprotein G first appears 2 to 3 months after initial infection in 60% to 70% of patients, while the remaining patients may require up to 6 months to seroconvert (2). In our study, there were 11 samples tested by immunoblotting that had positive results for the common HSV antigen band but were negative for both of the type-specific gG antigen bands. To determine whether these were early infections in which antibodies to the glycoproteins have yet to appear, HSV IgM serology was performed. Of the 11 samples, only 3 (27%) were IgM positive, indicating that the majority of these were probably not acute infections. Additionally, three of these untyped samples had reactivity to the type-specific multiplex assay, ELISA, and Western blot assay.
There were an additional three samples that were HSV common antigen band negative and gG-1 or -2 positive. According to interpretive data from the immunoblot assay package insert, these samples should be reported as “HSV Negative, No evidence of HSV exposure detected.” These were likely false-negative results by the immunoblot assay, as the multiplex assay, ELISA, and Western blot assay showed reactivity to either HSV-1 or -2 in all three samples. While the HSV common antigen band included in the immunoblot assay has some additional benefits over the ELISA and multiplex assay, it can also lead to some confusion in the interpretation of a small percentage of results.
The multiplex assay evaluated in this study performed statistically equal to the ELISA, immunoblot assay, and Western blot assay based on overlapping CIs. Advantages of the multiplex assay included the reporting of both HSV-1 and -2 IgG results from a single reaction, resulting in reagent, labor, sample volume, and storage space savings. The lower cost of the multiplex assay, as well as the labor savings of performing only one assay to obtain results for both HSV-1 and -2, resulted in a 20% cost savings compared to ELISA and 60% savings compared to the immunoblot assay. There are also several options available for automating the entire multiplex procedure, but these were not evaluated in the present study. Additional benefits of the multiplex test system are the inclusion of an internal control microsphere that detects nonspecific binding of the patient sample to the microsphere. Four additional microsphere sets contained within the bead mix are utilized for intrawell calibration. This technology generates a four-point standard curve to internally calibrate each well of the assay, converting the raw median fluorescent intensity value into semiquantitative units. Regression analysis of the internal standards is performed, allowing the software to adjust the calculated unit values based upon the unique characteristics of the patient serum. The software also minimizes front-to-back intra-assay variation by utilizing these internal controls. The multiplex system provided an accurate and cost-effective system for the detection of HSV-1 and -2 type-specific antibodies.
Footnotes
Published ahead of print on 19 November 2008.
REFERENCES
- 1.Ashley, R. L., J. Militoni, F. Lee, A. Nahmias, and L. Corey. 1988. Comparison of Western blot (immunoblot) and glycoprotein G-specific immunodot enzyme assay for detecting antibodies to herpes simplex virus types 1 and 2 in human sera. J. Clin. Microbiol. 26662-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashley, R. L., and A. Wald. 1999. Genital herpes: review of the epidemic and potential use of type-specific serology. Clin. Microbiol. Rev. 121-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashley, R. L., L. Wu, J. W. Pickering, M.-C. Tu, and L. Schnorenberg. 1998. Premarket evaluation of a commercial glycoprotein G-based enzyme immunoassay for herpes simplex virus type-specific antibodies. J. Clin. Microbiol. 36294-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coyle, P. V., H. J. O'Neill, D. E. Wyatt, C. McCaughey, S. Quah, and M. O. McBride. 2003. Emergence of herpes simplex type 1 as the main cause of recurrent genital ulcerative disease in women in Northern Ireland. J. Clin. Virol. 2722-29. [DOI] [PubMed] [Google Scholar]
- 5.Fleiss, J. L. 1981. Statistical methods for rates and proportions, 2nd ed. John Wiley & Sons, New York, NY.
- 6.Gupta, R., T. Warren, and A. Wald. 2007. Genital herpes. Lancet 3702127-2137. [DOI] [PubMed] [Google Scholar]
- 7.Kimberlin, D. 2004. Herpes simplex virus, meningitis and encephalitis in neonates. Herpes 11(Suppl. 2)65A-76A. [PubMed] [Google Scholar]
- 8.Lafferty, W. E., L. Downey, C. Celum, and A. Wald. 2000. Herpes simplex virus type 1 as a cause of genital herpes: impact on surveillance and prevention. J. Infect. Dis. 1811454-1457. [DOI] [PubMed] [Google Scholar]
- 9.Liljeqvist, J.-Å., B. Svennerholm, and T. Bergström. 1999. Typing of clinical herpes simplex virus type 1 and type 2 isolates with monoclonal antibodies. J. Clin. Microbiol. 372717-2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martins, T. B., R. D. Woolstenhulme, T. D. Jaskowski, H. R. Hill, and C. M. Litwin. 2001. Comparison of four enzyme immunoassays with a Western blot assay for the determination of type-specific antibodies to herpes simplex virus. Am. J. Clin. Pathol. 115272-277. [DOI] [PubMed] [Google Scholar]
- 11.Mertz, G. J., S. L. Rosenthal, and L. R. Stanberry. 2003. Is herpes simplex virus type 1 (HSV-1) now more common than HSV-2 in first episodes of genital herpes? Sex. Transm. Dis. 30801-802. [DOI] [PubMed] [Google Scholar]
- 12.Morrow, R., and D. Friedrich. 2006. Performance of a novel test for IgM and IgG antibodies in subjects with culture-documented genital herpes simplex virus-1 or -2 infection. Clin. Microbiol. Infect. 12463-469. [DOI] [PubMed] [Google Scholar]
- 13.Nascimento, M. C., S. Ferreira, E. Sabino, I. Hamilton, J. Parry, C. S. Pannuti, and P. Mayaud. 2007. Performance of the HerpeSelect (Focus) and Kalon enzyme-linked immunosorbent assays for detection of antibodies against herpes simplex virus type 2 by use of monoclonal antibody-blocking enzyme immunoassay and clinicovirological reference standards in Brazil. J. Clin. Microbiol. 452309-2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ribes, J. A., A. D. Steele, J. P. Seabolt, and D. J. Baker. 2001. Six-year study of the incidence of herpes in genital and nongenital cultures in a central Kentucky medical center patient population. J. Clin. Microbiol. 393321-3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sauerbrei, A., and P. Wutzler. 2007. Novel recombinant ELISA assays for determination of type-specific IgG antibodies against HSV-1 and HSV-2. J. Virol. Methods 144138-142. [DOI] [PubMed] [Google Scholar]
- 16.Whittington, W. L., C. L. Celum, A. Cent, and R. L. Ashley. 2001. Use of a glycoprotein G-based type-specific assay to detect antibodies to herpes simplex virus type 2 among persons attending sexually transmitted disease clinics. Sex. Transm. Dis. 2899-104. [DOI] [PubMed] [Google Scholar]
- 17.Xu, F., M. R. Sternberg, B. J. Kottiri, G. M. McQuillan, F. K. Lee, A. J. Nahmias, S. M. Berman, and L. E. Markowitz. 2006. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA 296964-973. [DOI] [PubMed] [Google Scholar]


