Abstract
Aim
To identify whether intensive treatment and aftercare telephone contacts influence long-term abstinence and well-being of patients with alcohol dependency.
Methods
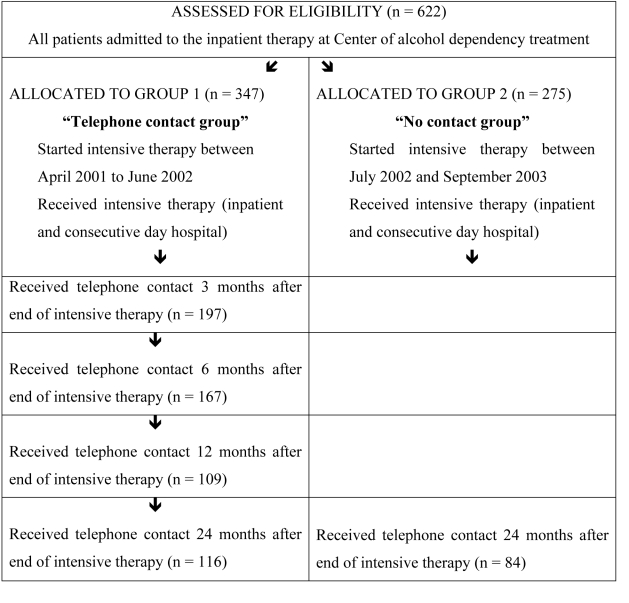
Six hundred and twenty two patients were evaluated at the beginning and end of intensive in-patient treatment. At the end of the treatment, the patients were divided into two recruitment cohorts – telephone contact group (n = 347), in whom basic outcome criteria (abstinence, marital and employment status, self-evaluation of well-being) were evaluated 3, 6, 12, and 24 months after intensive treatment and no contact group (n = 275) in whom the basic outcome criteria were checked only at 24 months after the intensive treatment. At 24 months, response rate was 33.4% in telephone contact group (n = 116) and 30.5% (n = 84) in no contact group.
Results
Positive indicators of therapy success (abstinence or decrease in drinking, stabile social relations, and more positive self-evaluation of well-being) were found in 53.0% of patients at 3 months, 44.3% at 6 months, and 30.6% at 12 months in telephone contact group. Overall abstinence 24 months after the end of intensive treatment was reported in 25.7% of all patients, including non-respondents. Both groups achieved significant improvement in subjective well-being during intensive treatment. At 24 months, 3 attributes of subjective well-being (subjective psychological health, evaluation of financial status, general quality of life) were significantly higher in telephone contact group. However, groups did not significantly differ in the abstinence level (telephone contact group = 27.7%, no contact group = 24.4%).
Conclusion
Significant differences in well-being variables between telephone contact group and no contact group at 24 months after the end of intensive treatment are at least partially due to phone contact/informative checking 3, 6, and 12 months after the end of intensive therapy. Telephone or any short and easy accessible communication checking is a promising as supportive and research tool in aftercare alcohol addiction treatment, especially because of its cost-benefit advantages.
Outcome expectations about alcohol dependency treatment should not be limited only to the reduction of alcohol use, but to a broader definition of “rehabilitation” (1). Successful outcomes of alcohol dependency treatment are usually considered to be reduction in alcohol and other drugs use, increase in personal health, and improvements in social functioning (2). In non-preselected cases, half of patients relapse within 6 months after treatment (2). Alcohol relapse rates are estimated to be the highest immediately after treatment and the first year is considered to be pivotal in establishing positive behavior changes necessary for sustaining a long-term recovery for alcohol problems (3).
In the study evaluating the impact of different psychiatric disorders on life satisfaction, the lowest life satisfaction was found in patients with dysthymia, posttraumatic stress disorder (PTSD), social phobia, and alcohol dependence, all with a large effect size (4). The subjective perception of well-being or quality of life of treated alcoholics can be a criterion for therapy success, but it is frequently overlooked in alcohol dependency treatment evaluation (5). Alcoholics have lower levels of quality of life compared with general population norms or with other chronic health conditions (6). Alcohol-dependent individuals are supposed to experience improvements in quality of life after treatment with both short-term and long-term abstinence (7). Abstinence does still seem to be one of most important factors in well-being improvement. A study of subjects with long-term excessive alcohol consumption showed that individuals who reduced their alcohol consumption by 60% did not differ in levels of mental well-being from subjects without alcohol intake reduction (8).
The role of telephone calls in the monitoring and treatment of chronic disorders may play an important role. For example, telephone monitoring and support was feasible and acceptable for 85% of clients discharged from residential PTSD treatments; clients receiving telephone support were twice as likely to complete an outpatient visit and report higher satisfaction with care (9). A program combining telephone care management and brief, structured psychotherapy significantly improved outcomes in primary care patients initiating antidepressant treatment (10). Telephone-based continuing care appears to be an efficient approach of step-down treatment in most patients with particular dependency treatment (11). McKay et al (12) combined weekly telephone-based monitoring and brief counseling contacts with weekly supportive group sessions over the first four weeks, cognitive behavioral relapse prevention twice a week, and standard group counseling twice a week. Participants under telephone monitoring had higher rates of total abstinence than those in standard counseling. Finally, for most substance-dependent patients who went through the phase of outpatient treatment, telephone-based monitoring and brief counseling appeared to be as effective as more intensive face-to-face treatments (12).
Slovenia has 6 alcoholism inpatient treatment centers within the public health system. They have had a similar treatment philosophy, based on social-ecological approach of Vladimir Hudolin, ever since 1971 (13). The basic principle of their approach is that no change in behavior or addictive lifestyle can be achieved outside the patient’s bio-social system. In Slovenia, the inpatient treatment system has gradually changed over time, adding more intense psychotherapy program, but the basic approach has remained the same. The Center for Alcohol Addiction Treatment of the University Psychiatric Hospital Ljubljana has a capacity of 33 inpatients and 30 outpatients. The treatment program is abstinence-based. Active participation of patients’ significant others is emphasized as an essential part of the program and aftercare recovery. Treatment orientation has been based on the synthesis of different therapeutic approaches; mainly psychodynamically-oriented group therapy combined with a behavioral-cognitive approach, including the principles of motivational enhancement therapy and family therapy. However, although there are many easily accessible comprehensive treatment programs for alcohol dependency in Slovenia, basic indicators about outcomes are quite unknown. Therefore, the main aim of our study was to evaluate basic outcomes after intensive treatment in a different time intervals up to 24 months after intensive therapy, to evaluate short- and long-term changes in patient well-being, and to identify the association between aftercare telephone checking and two-year outcomes.
Participants and methods
Participants
This study was designed as a prospective observational study. We collected data on two patient cohorts that participated in the same treatment program but differed in recruitment period and aftercare telephone contacts (Figure 1). All patients entering the program from April 2001 to June 2002 were allocated to telephone contact group (n = 249), whereas the patients entering the program from July 2002 and September 2003 were allocated to no contact group (n = 170). Telephone contact group was checked by telephone at 3, 6, 12, and 24 months after intensive treatment; no contact group was checked only once 24 months after intensive treatment.
Figure 1.
Patients' inclusion and dropout from the study.
Method
Patients with alcohol dependency syndrome, diagnosed according to the 10th Revision of International Classification of Diseases (14), were referred from Psychiatric Intensive Care, the Crisis Intervention Unit of the hospital, and other psychiatric' outpatient clinics and general practices. Indications for admission to intensive inpatient treatment are severe psychosocial or psychiatric consequences of alcohol addiction or difficulties/inability to stop drinking despite previous attempts. Patients with severe impairment in neuropsychological functioning and acutely suicidal or psychotic patients without a long-term stable remission usually are unable to follow the program and are admitted to another type of psychiatric treatment. The intensive treatment program (intensive therapy) has 2 parts. The first is inpatient treatment, which lasts 4-5 weeks, depending on the patient’s health status on admission. In the first week after admission, detoxification process takes place if not already provided at intensive psychiatric department. The second part of intensive therapy is provided in a day hospital (6-8 weeks), where patients are trained to cope with daily challenges in real life. On the second day of admission to inpatient therapy, each patient is allocated to a “basic” small group of 10-12 patients with two group therapists. There are 5 small groups with identical program, but with different therapists and different group climates. Group session lasts 75 minutes; there are 2 sessions on Mondays with significant others and a group therapy on working days. Once a week, there is a great group meeting of all patients and therapists from 5 small groups. Each evening, patients from the basic group have a self-help group session without therapists with an educational topic. All patients are included in additional therapeutic activities such as kinesiotherapy (twice a week), occupational therapy (four times a week), and psycho-educational sessions (twice a week). Patients also choose 1 or 2 of once-a-week therapies, such as relaxation techniques, psychodrama, training of the social skills, music therapy, and art therapy. During treatment, patients receive individual interventions at least three times (at the beginning, at the transition from inpatient treatment to day hospital, and at the end of whole intensive treatment). Individual short intervention can vary a lot, because a psychiatrist is at patients' disposal from 8:15 to 9:00 am. Patients were asked to sign permission that they accept receiving telephone calls. Approval for the study was obtained from the Ethics Committee of the Ministry of Health.
Instruments
A set of questionnaires was prepared for the purpose of this study for patients (in the beginning, at the end, and after the intensive treatment – web extra material) and therapists; data were also collected from medical records. The first questionnaire, administered to patients within the first 10 days after admission (after withdrawal), collected demographic data and contained five self-evaluation questions on well-being. Five variables were treated as central dependent variables, each of them on a five-point scale. These included evaluation of subjective psychological and subjective physical health, financial status, social relations with significant others, and general quality of life (from 1 – very poor to 5 – very good). The five evaluations were supposed to cover subjective perception of physical and psychosocial health and yet to be easy detectable by phone intervention later in the follow-up. At the end of the intensive treatment program, the patients completed the same self-evaluation questionnaire. Group therapists, having the most frequent interactions with patients, were asked to estimate patient compliance with the treatment program from 1 – very poor to 5 – very good. For every patient, the week of follow-up was determined in advance and patients were contacted by telephone always on Wednesday, because this was a less busy day for the staff. Four trained nurses from department made phone calls as part of their afternoon duty. The phone calls followed the same questionnaire at every time point. The telephone contact group was checked at 3, 6, and 12 months after the end of the intensive treatment program and both groups were checked at 24 months. Each time, patients were asked the same questions about abstinence/relapse, participation in after-care recovery, participation of significant others in after-care settings, quantity and quality of relapse, the type of help they received in coping with relapse, changes in marital status/partnership (status of partnership unchanged, better/finding a partner, worse/end of partnership), employment status (status of employment unchanged, better/getting a job, worse/losing a job), and the same 5 self-evaluation questions as at the beginning and at the end of intensive treatment. The accuracy of yes/no answers about abstinence (sobriety) was controlled by two opposite questions in different parts of the questionnaire (“Are you still abstinent?” and “Have you ever relapsed since the end of the treatment?”).
Statistical analysis
Comparisons of characteristics of two groups were tested with t test for 2 independent samples and with χ2 test. Kolmogorov-Smirnov nonparametric one-sample test showed that distribution of each central dependent variable (self-evaluations) significantly differed from normal. This is why nonparametric tests were mostly applied. Comparisons between self-evaluations at the beginning and at the end of intensive treatment were tested with Wilcoxon nonparametric test for 2 related samples. For comparing telephone contact group and no contact group at different time intervals, Mann-Whitney nonparametric test for 2 independent samples was applied. Proportions of abstinent and non-abstinent patients 24 months after the end of intensive therapy with regard to telephone contact were tested by the χ2 test. Statistical Package for the Social Sciences, version 13 (SPSS Inc., Chicago, IL, USA) was used for the analyses. The level of significance was set at P < 0.05.
Results
There was no significant difference between telephone contact group and no contact group in the length of inpatient treatment, the length of day hospital treatment, and the number of all treatments including the one during the study. The only significant difference found was that patients in no contact group were two years younger than those in telephone contact group (Table 1). Also no significant difference between groups was found at the end of intensive treatment, when group therapists evaluated patient compliance with therapy in both the telephone contact group and no contact group, (3.1 ± 1.1 vs 3.2 ± 1.0, respectively; P = 0.191, t test). There were no significant differences between telephone contact and no contact group with regard to sex, marital, educational, and employment status, and whether significant others were included in therapy (Table 2).
Table 1.
Characteristics of patients in telephone contact and no contact groups
| Mean ± standard deviation |
P* | ||
|---|---|---|---|
| telephone contact (n = 347) | no contact (n = 275) | ||
| Age (years) | 46.2 ± 9.1 | 44.7 ± 9.1 | 0.035 |
| Inpatient treatment (days) | 35.3 ± 17.7 | 34.7 ± 14.2 | 0.683 |
| Day hospital treatment (days) | 28.1 ± 18.3 | 27.9 ± 19.8 | 0.869 |
| Number of inpatient treatments, including the one during study | 1.4 ± 0.7 | 1.5 ± 0.8 | 0.191 |
*t test for two independent samples.
Table 2.
Demographic characteristics of patients with regard to their initial group allocation
| No (%) of patients |
P* | ||
|---|---|---|---|
| telephone contact (n = 347) | no contact (n = 275) | ||
| Sex: | |||
| male | 268 (77.2) | 198 (72.0) | 0.135 |
| female | 79 (28.8) | 77 (28.0) | |
| Marital status: | |||
| married | 163 (55.3) | 123 (54.9) | 0.992 |
| divorced | 51 (17.3) | 39 (17.4) | |
| single | 65 (22.0) | 51 (22.8) | |
| widowed | 16 (5.4) | 11 (4.9) | |
| Education (years): | |||
| ≤8 | 73 (24.6) | 55 (24.5) | 0.819 |
| 10-12 | 182 (61.3) | 131 (58.3) | |
| 14 | 28 (9.4) | 23 (10.2) | |
| ≥16 | 14 (4.7) | 16 (7.1) | |
| Employment status: | |||
| employed | 180 (61.0) | 147 (65.6) | 0.142 |
| retired | 46 (15.6) | 22 (9.8) | |
| unemployed | 69 (23.4) | 55 (24.6) | |
*χ2 test.
No significant difference was found between telephone contact and no contact groups at 24 months in abstinence, alcohol use in relapsed respondents, inclusion in after-care, inclusion of significant others in after-care, and changes in marital status (Table 3). Abstinence or drinking less was reported 24 months after the end of intensive therapy in 29.2% of all patients from both groups including non-respondents (continuous abstinence, 25.7%). More than 93% of all respondents reported stable or improved social functioning at 24 months. The control question about abstinence showed good accuracy regarding drinking status. If the patients answered that their marital and employment status remained unchanged, it was also considered as a positive outcome, because addiction has destructive consequences for all important social relations. Most relapses were estimated as “drinking less than before admission to treatment.” In no contact group, there were less stable conditions, with less unchanged conditions of employment and more improved and worsened employment situations.
Table 3.
Drinking status, after-care participation, change in marital and employment status of telephone contact group (n=347) at 3, 6, 12, and 24 mo after the end of intensive treatment and no contact group (n=84) at 24 mo after end of intensive treatment
| Telephone contact group |
No contact group |
||||
|---|---|---|---|---|---|
| 3 mo |
6 mo |
12 mo |
24 mo |
24 mo |
|
| Drinking status with regard to initial cohort, including non-respondents | n = 197 | n = 167 | n = 109 | n = 116 | n = 84 |
| Response rate from the initial cohort (n = 347): | 56.8 | 48.1 | 31.4 | 33.4 | 30.5 |
| No alcohol use – question 1 (%)* | 48.4 | 40.3 | 27.1 | 27.7† | 24.4† |
| No alcohol use – question 2 (%)‡ | 49.3 | 42.1 | 27.7 | 30.3§ | 24.4§ |
| Alcohol use in respondents who relapsed in comparison with baseline: | n = 29 | n = 27 | n = 15 | n = 20 | n = 17 |
| equal (%) | 23.8 | 16.7 | 28.6II | 14.3II | |
| lower (%) | 76.2 | 77.8 | 100.0 | 64.3 | 71.4 |
| greater (%) | 5.6 | 7.1 | 14.3 | ||
| After-care participation of respondents (%): | |||||
| group membership | 47.0 | 48.2 | 45.9 | 45.5¶ | 40.9¶ |
| psychotherapy or psychiatric treatment | 11.9 | 13.1 | 13.8 | 12.4 | 15.9 |
| none | 40.1 | 38.7 | 40.4 | 42.1 | 43.2 |
| Change in marital status of respondents (%): | |||||
| unchanged | 81.8 | 85.3 | 84.8 | 81.0** | 82.8** |
| finding a partner | 14.6 | 14.1 | 11.4 | 14.9 | 13.8 |
| losing a partner | 3.6 | 0.6 | 3.8 | 4.1 | 3.4 |
| Change in employment status of respondents (%) | |||||
| Unchanged | 84.4 | 83.3 | 85.3 | 82.7†† | 68.2†† |
| Better – getting job or promotion | 13.1 | 13.0 | 12.7 | 12.7 | 21.2 |
| Worse – losing job or lower status | 2.5 | 3.7 | 2.0 | 4.5 | 10.6 |
*Are you still completely abstaining?
†χ21 = 0.29, P = 0.590.
‡Have you ever relapsed since the end of the intensive treatment?
§χ21 = 8.79, P = 0.118.
IIχ22 = 1.05, P = 0.591.
¶χ22 = 0.71, P = 0.702.
**χ22 = 0.12, P = 0.941.
††χ22 = 5.84, P = 0.054.
Comparison between self-evaluations at the beginning and at the end of intensive therapy showed that patients in telephone contact group improved significantly in all of the five domains of subjective well-being. At the end of intensive therapy, these patients had significantly more positive subjective psychological and psychical health, evaluations of financial status, social relations, and general life quality. Patients in no contact group improved significantly in four domains of subjective well-being at the end of intensive therapy (significantly more positive subjective psychological and psychical health, evaluations of social relations, and general life quality), but there was no significant difference in the perception of financial status. Short-term therapeutic outcome seemed to be a bit more positive in the telephone contact group (Table 4).
Table 4.
Comparison between self-evaluations at the beginning and at the end of intensive therapy*
| Variable | Telephone contact group |
No contact group |
||||
|---|---|---|---|---|---|---|
| n | mean ± standard deviation | P* | n | mean ± standard deviation | P† | |
| Subjective psychological health: | ||||||
| beginning | 257 | 3.0 ± 1.0 | <0.001 | 164 | 2.9 ± 1.1 | <0.001 |
| end | 3.8 ± 1.0 | 3.9 ± 0.9 | ||||
| Subjective physical health: | ||||||
| beginning | 257 | 3.4 ± 1.1 | <0.001 | 163 | 3.2 ± 1.1 | <0.001 |
| end | 3.8 ± 1.0 | 3.9 ± 1.0 | ||||
| Evaluation of financial status: | ||||||
| beginning | 258 | 2.7 ± 1.0 | 0.002 | 162 | 2.6 ± 1.1 | 0.098 |
| end | 2.9 ± 1.0 | 2.8 ± 1.1 | ||||
| Evaluation of social relations: | ||||||
| beginning | 258 | 3.6 ± 1.1 | <0.001 | 163 | 3.4 ± 1.2 | <0.001 |
| end | 4.0 ± 2.1 | 3.8 ± 1.0 | ||||
| General quality of life: | ||||||
| beginning | 260 | 2.8 ± 0.9 | <0.001 | 163 | 2.6 ± 1.1 | <0.001 |
| end | 3.5 ± 0.9 | 3.4 ± 1.0 | ||||
*Evaluation on a 5-point scale (1 – very poor to 5 – very good).
†Wilcoxon test for two related samples.
Comparison between telephone contact group and no contact group showed no significant difference in any of five subjective domains of well-being at the end of intensive therapy (Table 5). At 24 months after intensive therapy, telephone contact group evaluated subjective psychological health, financial status, and general life quality significantly higher than no contact group, as well as subjective physical health (P = 0.070). There was no significant difference in the evaluation of social relations. In the long-term period, less positive self-evaluations were found in no contact group than in telephone contact group (Table 5).
Table 5.
Comparison between telephone contact group and no contact group at the end of intensive treatment and 24 mo after the end of intensive therapy in different self-evaluations*
| Variable | n | Mean ± standard deviation |
P† | |
|---|---|---|---|---|
| telephone contact | no contact | |||
| End of intensive therapy: |
||||
| subjective psychological health |
427 |
3.8 ± 1.0 |
3.9 ± 0.9 |
0.492 |
| subjective physical health |
424 |
3.8 ± 1.0 |
3.9 ± 11.0 |
0.109 |
| evaluation of financial status |
426 |
2.9 ± 1.0 |
2.8 ± 1.1 |
0.466 |
| evaluation of social relations |
425 |
4.0 ± 2.1 |
3.8 ± 1.0 |
0.621 |
| general quality of life |
427 |
3.5 ± 0.9 |
3.5 ± 1.0 |
0.946 |
| 24 mo after end of intensive therapy: |
||||
| subjective psychological health |
209 |
3.8 ± 1.1 |
3.4 ± 1.3 |
0.036 |
| subjective physical health |
209 |
3.7 ± 1.0 |
3.4 ± 1.2 |
0.077 |
| evaluation of financial status |
209 |
3.2 ± 1.0 |
2.8 ± 1.2 |
0.034 |
| evaluation of social relations |
209 |
3.9 ± 1.0 |
3.6 ± 1.1 |
0.145 |
| general quality of life | 211 | 3.6 ± 0.9 | 3.2 ± 1.3 | 0.040 |
*Evaluation on a 5-point single scale (1 – very poor to 5 – very good).
†Mann-Whitney test for independent samples.
Discussion
Substantial part of patients who participated in our study not only established stable abstinence, but also maintained short-term and long-term positive changes in their psychosocial functioning; these changes were more prominent in the telephone contact group.
Although there is no special research team available in our center, we wanted to identify some clinically important aspects of patient capacity for therapeutic change over time intervals. Basic alcohol use treatment outcomes in our study relied only on self-reporting, basically because of lack of funds for research, but the answers about abstinence – controlled by two types of questions – were almost always identical. There is also evidence that carefully collected self-report alcohol and drug use data can be as accurate as data obtained by means of alternative measures that are often assumed to be more objective (ie, laboratory tests) (15). Data from MATCH trial (16) show that about one-third of the aftercare patients, who had previously received inpatient treatment, remained continuously abstinent, compared with 20% of the outpatient sample at one-year follow-up. In our sample, 1-year abstinence outcome of the first cohort was somewhere in-between the two previously mentioned results. However, our study could not measure up to the outstanding methodology of MATCH study (16), and the drop-out because of our method of follow-up was very high. It is very possible that outcomes from our study would have shown better outcomes if the drop-out rate had been smaller. For the sake of reliable presentation of results, it is assumed that all non-respondents relapsed, which is not certain. Our outcomes are analogous with the 12-month outcomes of the US alcoholism treatment data; 24% of treated alcoholics were found continuously abstinent, among those not totally abstinent there was 87% reduction in alcohol consumption and 60% reduction in alcohol-related problems (17). Both cohorts of our study at month 24 of aftercare reported similar abstinence rate with 12-month outcomes from the US study (17).
If alcohol addiction treatment is to be presented to the professional community and to the public as successful, it has to be realistic. It is appropriate to compare alcohol addiction treatment with the treatment of other chronic conditions, such as hypertension, diabetes, and asthma: in all patients who were prescribed medication for the treatment of chronic illnesses, less than half of patients took the medication as prescribed; less than 30% of patients accepted the prescribed behavioral changes, such as weight loss and diet; each year 40%-60% of patients with hypertension, diabetes, or asthma relapsed (18). However, it was argued that that intensive treatment of dependency is also cost beneficial in a strict economic sense, if the patient’s condition improves before the end of treatment and lasts 6-12 months (2). Our study showed a long-term improvement in-between one quarter to one third of treated patients.
Our expectations from aftercare informational checking were as follows: 1) to obtain concurrent information about patient functioning during different stages of rehabilitation and 2) to improve patient long-term outcomes with several more aftercare contacts (19). More beneficial outcomes in 24 months well-being of telephone contact group could be influenced by many factors. Treatment process is affected by patient, provider, and treatment program characteristics, the therapist-patient relationship, patient involvement in treatment, characteristics of patient social context and life events (20). For example, even therapists’ tone has been found to predict how their patients will fare (19). We did not control a whole range of variables, but the most striking difference between the two cohorts was found in three domains of well-being 24 months after the end of intensive treatment. Comparison between the groups in demographic variables, well-being at the end of intensive treatment, and therapists' evaluation of patient compliance showed no significant difference. The only significant difference was that patients in the no contact group were two years younger, however, two years of difference in participants with mean age of 46 could not be critical, because both groups belong to the same generation. We did not find differences in the abstinence rate, as it was found in another study (12) where participants in the telephone contact group had higher rates of total abstinence than those in standard group counseling. Our results, indicating the beneficial influence of telephone checking on well-being, can be regarded as only preliminary, but we believe that it is worth trying to examine the influence of aftercare telephone checking in more detail. Other data report telephone checking as a promising and supportive research tool (11). Its use in “concurrent treatment monitoring” in alcoholism treatment (21) should be taken into account as a routine, especially because of its cost-benefit advantages. It seems that telephone contacts have some influence on patient well-being at the end and 24 months after intensive therapy, indicating that maintaining even a short contact with former patients can strengthen the short-term positive outcomes.
There are several limitations of our study. First, there was the sampling problem. The patients were not allocated to the groups simultaneously. Also, the latter group was smaller. However, although it would be better if patients were enrolled simultaneously, the patients from both groups had very similar demographic, socioeconomic, and socio-cultural characteristics.
Second, the design of our study did not permit us to identify other possible influences on patients except for telephone checking. There are also problems with generalizations of results because of the missing cases at different time points. One of the limitations was also the method of obtaining follow-up data. It was done by four callers (nurses at the Center) as a part of their routine work once a week in the afternoon. They were instructed to follow the protocol and to make as little as possible additional conversations, but supportive tone of communication was advisable. Their calls were not supposed to have an intervening or counseling role, but their way of communication was not controlled. Also, were not able to control the callers’ persistence to reach former patients, which might have affected the dropout rate.
There is a discrepancy between very comprehensive treatment programs and insufficient funds for research in Slovenia. In future, we will try to form a research team that would be able to conduct more methodologically appropriate studies. However, by conducting the present study, we showed that it is possible to perform primary research (22) within the framework of routine clinical work and without the need for large financial support.
References
- 1.McLellan AT, Weisner C. Achieving the public health potential of substance abuse treatment: implications for patient referral, treatment “matching” and outcome evaluation. In: Bickel W, DeGrandpre R, editors. Drug policy and human nature. Philadelphia (PA): Williams & Wilkins; 1996. p. 127-54. [Google Scholar]
- 2.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the drug abuse treatment outcome study (DATOS). Psychol Addict Behav. 1997;11:294–301. doi: 10.1037/0893-164X.11.4.294. [DOI] [Google Scholar]
- 3.Maisto SA, Clifford PR, Longabaugh R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. J Stud Alcohol. 2002;63:397–403. doi: 10.15288/jsa.2002.63.397. [DOI] [PubMed] [Google Scholar]
- 4.Meyer C, Rumpf HJ, Hapke U, John U. Impact of psychiatric disorders in the general population: satisfaction with life and the influence of comorbidity and disorder duration. Soc Psychiatry Psychiatr Epidemiol. 2004;39:435–41. doi: 10.1007/s00127-004-0755-3. [DOI] [PubMed] [Google Scholar]
- 5.Rudolf H, Watts J. Quality of life in substance abuse and dependency. Int Rev Psychiatry. 2002;14:190–7. doi: 10.1080/09540260220144975. [DOI] [Google Scholar]
- 6.Donovan D, Mattson ME, Cisler RA, Longabaugh R, Zweben A. Quality of life as an outcome measure in alcoholism treatment research. J Stud Alcohol Suppl. 2005;(15):119–39. doi: 10.15288/jsas.2005.s15.119. [DOI] [PubMed] [Google Scholar]
- 7.Foster JH, Powell JE, Marshall EJ, Peters TJ. Quality of life in alcohol-dependent subjects – a review. Qual Life Res. 1999;8:255–61. doi: 10.1023/A:1008802711478. [DOI] [PubMed] [Google Scholar]
- 8.Eriksson M, Berggren U, Fahlke C, Hard E, Balldin J. Mental well-being in subjects with long-term excessive alcohol consumption: an experimental study. Alcohol. 2002;27:99–105. doi: 10.1016/S0741-8329(02)00218-5. [DOI] [PubMed] [Google Scholar]
- 9.Rosen CS, DiLandro C, Corwin KN, Drescher KD, Cooney JH, Gusman F. Telephone monitoring and support for veterans with chronic posttraumatic stress disorder: a pilot study. Community Ment Health J. 2006;42:501–8. doi: 10.1007/s10597-006-9047-6. [DOI] [PubMed] [Google Scholar]
- 10.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 11.Breslin C, Sobell LC, Sobell MB, Buchan G, Kwan E. Aftercare telephone contacts with problem drinkers can serve a clinical and research function. Addiction. 1996;91:1359–64. doi: 10.1111/j.1360-0443.1996.tb03621.x. [DOI] [PubMed] [Google Scholar]
- 12.McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Arch Gen Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- 13.Wolf D. Vladimir Hudolin and his work. Proceedings of the meeting held at 1st Croatian High School in Sušak 1999. Rijeka: Regional center for Alcoholism; 2007. [Google Scholar]
- 14.World Health Organization. The ICD-10 classifications of mental and behavioral disorders. Diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 15.Perl HI, Dennis ML, Huebner RB. State-of-the-art methodologies in alcohol-related health services research. Addiction. 2000;95(Suppl 3):S275–80. doi: 10.1080/09652140020004232. [DOI] [PubMed] [Google Scholar]
- 16.Matching alcoholism treatments to client heterogeneity: project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 17.Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62:211–20. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- 18.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 19.Miller WR. Why do people change addictive behavior? The 1996 H. David Archibald Lecture. Addiction. 1998;93:163–72. doi: 10.1046/j.1360-0443.1998.9321632.x. [DOI] [PubMed] [Google Scholar]
- 20.Finney JW. Assessing treatment and treatment processes. In: Allen JP, Wilson VB, editors. Assessing alcohol problems: a guide for clinicians and researchers. NIH Publication No 03-3745. Bethesda (MD): National Institute on Alcohol Abuse and Alcoholism; 2003. p. 189-217. [Google Scholar]
- 21.McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100:447–58. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- 22.Wilson DB. Meta-analyses in alcohol and other drug abuse treatment research. Addiction. 2000;95(Suppl 3):S419–38. doi: 10.1080/09652140020004313. [DOI] [PubMed] [Google Scholar]