Abstract
Objectives. We investigated the relationship between childbirth and 5-year incidence of obesity.
Methods. We performed a prospective analysis of data on 2923 nonobese, nonpregnant women aged 14 to 22 years from the 1979 National Longitudinal Survey of Youth Cohort, which was followed from 1980 to 1990. We used multivariable logistic regression analyses to determine the adjusted relative risk of obesity for mothers 5 years after childbirth compared with women who did not have children.
Results. The 5-year incidence of obesity was 11.3 per 100 parous women, compared with 4.5 per 100 nulliparous women (relative risk [RR] = 3.5; 95% confidence interval [CI] = 2.4, 4.9; P < .001). The 5-year incidence of obesity was 8.6 for primiparous women (RR = 2.8; 95% CI = 1.5, 5.0) and 12.2 for multiparous women (RR = 3.8; 95% CI = 2.6, 5.6). Among parous women, White women had the lowest obesity incidence (9.1 per 100 vs 15.1 per 100 for African Americans and 12.5 per 100 for Hispanics).
Conclusions. Parous women have a higher incidence of obesity than do nulliparous women, and minority women have a higher incidence of parity-related obesity than do White women. Thus, efforts to reduce obesity should target postpartum women and minority women who give birth.
Women in the United States are disproportionately overweight, particularly minority and socioeconomically disadvantaged women.1,2 Approximately two thirds of adult women are overweight, and of this group, one third are obese.1 Among racial/ethnic groups, African American and Hispanic women have the highest prevalences of obesity, at 50% and 40%, respectively.1 Women who are socioeconomically disadvantaged have higher obesity rates than do women of higher socioeconomic standing.3 In addition, emerging evidence links perinatal factors such as parity (number of births) to obesity in later life,4–9 although researchers investigating the relationship between parity and major weight gain or obesity have found mixed results.7,10–17
Several studies have reported that multiparous women (those who have had 2 or more live births) were more likely to be overweight than were nulliparous women (those who have never had a live birth).10–13,15 Another study found that primiparous women (those who have had at least 1 live birth) were more likely to be overweight and to have major long-term weight gain than were multiparous and nulliparous women.17 Other studies have found little or no relationship between parity and weight gain or obesity.7,12,14,16 The inconsistencies in these findings may stem from differences in definitions of the main outcomes, the use of cross-sectional study designs versus prospective designs, or the exclusion of prevalent cases of obesity at baseline. The majority of these studies focused on the outcomes of mean body mass index (BMI), mean weight gain, weight change, major weight gain, or prevalence of obesity, but not on the incidence of parity-related obesity. Additionally, these studies did not establish that births occurred before the outcome measured.10,12,13,16 Nor have these studies investigated whether racial/ethnic or socioeconomic differences exist in the incidence of parity-related obesity. Thus, we used prospective data to determine the 5-year incidence of parity-related obesity among our sample and to investigate whether this incidence varied by race/ethnicity or socioeconomic status.
METHODS
Study Design
We analyzed data on 2923 women from the 1979 National Longitudinal Survey of Youth (NLSY), an ongoing prospective study of a nationally representative sample of 12 686 US residents aged 14 to 22 years in 1979. Details of recruitment, sampling methods, and study procedures have been published previously.18 Briefly, the US Department of Labor sponsored the NLSY cohort study to examine participants’ labor-force experiences, education, and training. Additional funding from the National Institute for Child Health and Human Development allowed for the inclusion of perinatal and health-related variables.
The NLSY study was constructed from 3 independent, multistage, stratified area probability samples: (1) a cross-sectional sample that represented noninstitutionalized civilian youths aged 14 to 22 years in 1979; (2) a supplemental sample that oversampled Hispanics, African Americans, and respondents who were not African American or Hispanic and who were economically disadvantaged in 1979; and (3) a military sample that represented youths aged 17 to 21 years who were enlisted in the armed services in 1979. The cohort was statistically powered to analyze historically underrepresented groups such as women and minorities.
The study duration for the NLSY is 1979 to the present; our study period encompassed 1980 to 1990. We chose this period because, although key perinatal and anthropometric variables were available for the entire NLSY study duration, the supplemental sample was not followed beyond 1990.
Sample Characteristics
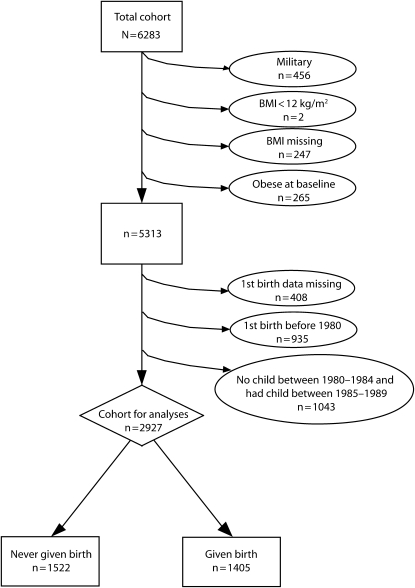
A total of 6283 women were enrolled in NLSY. We included the NSLY's adolescent respondents in our study sample because the data on the relationship of parity to incidence of obesity among adolescents are extremely limited. Moreover, excluding adolescents and limiting our sample to adults would result in an underestimation of the impact of parity on the incidence of obesity. We excluded women meeting any of the following conditions: those in the military sample (n = 456), because it was not followed beyond 1985; those for whom BMI (weight in kilograms divided by height in meters squared) data were missing (n = 247); obese women (n = 265); and those with a BMI of less than 12 kg/m2 (n = 2), because they do not represent healthy individuals in the community. However, we included underweight women (BMI < 18.5 kg/m2), who may gain weight over time with repeated births. This left a cohort of 5313 (Figure 1).
FIGURE 1.
Flow chart of study sample selection.
Note. BMI = body mass index.
We also excluded women missing information on their first childbirth (n = 408), women who first gave birth before 1980 (n = 935), and women who had no children between 1980 and 1984 but who had children between 1985 and 1990 (n = 1043). This left a final cohort of 2927. We further divided this cohort into 2 groups: the nulliparous group (n = 1522) were women who did not give birth between 1980 and 1990, and the parous group (n = 1405) were women who had at least their first child between 1980 and 1984.
Measures
Demographic variables.
We used maternal education level as a proxy for socioeconomic status. Participant education level was not an appropriate proxy because the majority of the respondents were still in school. Also, maternal education is correlated strongly with health-risk behaviors among adolescents.19,20 We defined maternal education level as the highest education level attained by the participant's mother, categorized into 3 levels: high (1 year or more of college), medium (high school diploma), and low (less than a high school diploma). We defined participant education level as the highest education level attained by the participant, with the results categorized in the same 3 levels as those used for maternal education. Place of residence at age 14 was dichotomized into urban and rural areas. Marital status was dichotomized into married versus unmarried, with the latter category including participants who were single, divorced, widowed, separated, or other. Smoking status was defined as “smoker” if the woman gave an age in answer to the question, “At what age did you start to smoke daily?” A participant was defined as a nonsmoker if she reported no age in answer to the question about smoking. All demographic variables were measured at baseline.
Parity variables.
The participant's age at the birth of her first child, age at first birth, was dichotomously categorized into 11 to 17 years and 18 to 33 years. Women 17 years and younger are considered children and thus are evaluated according to different weight classifications.21 We defined parity as the total number of live births between 1980 and 1990. We defined the nulliparous group as women who had no children between 1980 and 1990. The primiparous group had 1 child, their first, from 1980 to 1984, and they had no children within the 1985 to 1990 follow-up interval.
Initially, we created 2 multiparous groups (women who had more than 1 child). The first multiparous group consisted of women who had 2 or more biological children between 1980 and 1984 and no children during the follow-up period in which obesity was determined (1985–1990). This definition ensured that all births occurred before the obesity outcome. The second group included women who had at least their first biological child between 1980 and 1984 and other children between 1985 and 1990. For this group, it was possible for births to have occurred after the obesity outcome. We analyzed the incidences of obesity for these 2 multiparous groups separately, and we found the incidences to be similar. Therefore, to ensure a more stable estimate of obesity incidence, we combined the 2 multiparous groups for the analyses.
Definition of main outcome.
Our main outcome variable was 5-year incidence of obesity. We used self-reported weight (collected annually in 1980–1983 and in 1985, 1986, and 1988) and height (collected in 1981, 1982, 1983, and 1985) to calculate BMI. We used the 1985 height to calculate BMI for years 1985 and later, because by 1985 all the women in the sample had reached their adult height. Obesity for women 18 years or older was defined according to the standard World Health Organization (WHO) criterion of BMI at or above 30 kg/m2.22 Because the WHO criterion does not apply to those younger than 18 years, we used age- and gender-specific BMI percentiles from the Centers for Disease Control and Prevention for girls aged 14 to 17 years. Girls in this age category with a BMI greater than the 95th percentile for their age were classified as obese, and those with a BMI greater than the 85th percentile were classified as overweight.21
In our calculation of the 5-year incidence of obesity for women who gave birth between 1980 and 1984, the numerator contained the number of obese cases within the 5-year interval, starting with the birth year of the first child born, and the denominator contained the number of total births within that year. For example, for women who had a child in 1982, the 5-year incidence of obesity was calculated as follows: number of these women who became obese between 1982 and 1986 divided by the total number of women who gave birth in 1982. The overall 5-year incidence for the women who gave birth between 1980 and 1984 was calculated by summing all of the incidence rates for the individual years.
Eight women gave birth in the year when their weight was measured. We excluded 4 of these women from the analyses because they were pregnant when their weight was measured. We included the other 4 women because they met 1 of 2 criteria: (1) their weight was measured 6 months to 1 year after they delivered (n = 1), or (2) they remained obese in the years following the birth of their child (n = 3).
The 5-year incidence of obesity for women in the nulliparous group was calculated as follows: number of obese women in the nulliparous group between 1980 and 1985 divided by the number of women who did not give birth between 1980 and 1990. We used the obesity incidence rate for the first 5-year interval (1980–1985) as a proxy for the overall obesity incidence rate for the nulliparous group. This decision was based on a comparison of obesity incidence rates from successive 5-year intervals, incremented by 1 year each, from 1980 to 1989 for this group. These comparisons revealed only small increases in the incidence of obesity from each 5-year interval to the next. We believe these increases in obesity incidence were the result of increasing age, which we accounted for in the multivariate model.
Statistical Analyses
In our bivariate analyses, we used Pearson's χ2 to compare categorical variables and Student's t test or analysis of variance for continuous variables to aid in identifying potential confounding variables for the multivariable models. We used 4 multiple logistic regression models to determine the relative risk of developing obesity over a 5-year interval. Model A determined the relative risk of developing obesity over a 5-year interval, comparing parous women to nulliparous women. Model B compared primiparous women to nulliparous women, model C compared multiparous women to nulliparous women, and model D compared multiparous women to primiparous women. We controlled for chronological age, smoking, residence, maternal education level, marital status, and race/ethnicity. We used Stata software version 8 for all analyses (Stata Corp LP, College Station, TX). Our analyses tested for effects of the following interactions on the incidence of obesity: race/ethnicity × parity, race/ethnicity × maternal education, and race/ethnicity × age.
RESULTS
In comparisons of the group with missing data to the remaining cohort, women missing BMI at baseline (n = 247) were similar to the remaining cohort with respect to educational level, age at first birth, and parity; women missing BMI at baseline differed in that more were Hispanic, they were older, and more were married women who had a mother with low educational attainment. Women missing information on the birth of their first biological child (n = 408) were similar to the remaining cohort with regard to race/ethnicity, education, maternal education, baseline mean age, and BMI; they differed in that more of them were married, and they were slightly older.
Table 1 displays the demographic and clinical characteristics of the sample at baseline (1979–1980), stratified by race/ethnicity. Compared with African American and Hispanic women, White women were slightly older, they were more likely to be married and to live in a rural location, and they had higher personal and maternal education levels. African American women were heavier and more likely to be primiparous than the 2 other racial groups. Hispanic and African American women had a younger age at first birth than did White women.
TABLE 1.
Demographic and Clinical Characteristics: National Longitudinal Survey of Youth, 1980–1990
| Characteristic | Total (N = 2923) | White (n = 1789) | African American (n = 665) | Hispanic (n = 469) | P |
| Age, y, mean (SD) | 17.3 (2.2) | 17.5 (2.2) | 17.0 (2.1) | 17.1 (2.2) | .04 |
| Baseline chronological age, y, mean (SD) | .001 | ||||
| 14–17 | 1635 (56) | 930 (52) | 421 (63) | 284 (61) | |
| 18–22 | 1288 (44) | 859 (48) | 244 (37) | 185 (39) | |
| Highest education completed, no. (%) | .001 | ||||
| Less than high school diploma | 1894 (65) | 1075 (60) | 477 (72) | 342 (73) | |
| High school diploma | 619 (21) | 420 (24) | 115 (17) | 84 (18) | |
| 1 or more years of college | 410 (14) | 294 (16) | 73 (11) | 43 (9.0) | |
| Married, no. (%) | 154 (5.0) | 122 (7.0) | 9 (1.0) | 23 (5.0) | .001 |
| Maternal education level, no. (%) | .001 | ||||
| Less than high school diploma | 1153 (41) | 527 (31) | 314 (51) | 312 (70) | |
| High school diploma | 1132 (41) | 814 (47) | 215 (35) | 103 (23) | |
| 1 or more years of college | 498 (18) | 376 (22) | 89 (14) | 33 (7.0) | |
| Area residence, no. (%) | .001 | ||||
| Urban/suburban | 2319 (80) | 1355 (76) | 540 (81) | 424 (91) | |
| Rural | 597 (20) | 430 (24) | 123 (19) | 44 (9) | |
| Body mass index in 1981, kg/m2, mean (SD) | 21.5 (2.8) | 21.2 (2.7) | 22.1 (2.9) | 21.8 (2.7) | .001 |
| Body mass index category,a no. (%) | .001 | ||||
| Underweight | 234 (8.0) | 169 (9) | 29 (4) | 36 (8) | |
| Normal weight | 2352 (80) | 1450 (81) | 528 (79) | 374 (80) | |
| Overweight | 337 (12) | 170 (10) | 108 (16) | 59 (12) | |
| Age at first birth, no. (%) | .09 | ||||
| 11–17 years | 143 (10) | 66 (9.0) | 44 (12) | 33 (13) | |
| 18–33 years | 1261 (90) | 701 (91) | 330 (88) | 230 (87) | |
| Parity, no. (%) | .001 | ||||
| Nulliparous | 1522 (52) | 1023 (57) | 293 (44) | 206 (44) | |
| Primiparous | 327 (11) | 168 (9.0) | 108 (16) | 51 (11) | |
| Multiparous | 1074 (37) | 598 (33) | 264 (39) | 212 (45) |
Note. Some data were not collected in 1979 and became available in later years. Weight data became available in 1981; age at first birth and parity were retrospectively collected in 1983 and prospectively collected from that time onward.
For women 18 years of age or older, underweight is defined as BMI < 18.5 kg/m2, normal weight as BMI = 18.5 kg/m2 to 24.9 kg/m2, and overweight as BMI = 25 kg/m2 to 29.9 kg/m2. For girls under 18 years of age, underweight is defined as BMI < 15th percentile for age, normal weight as BMI = 15th to 85th percentiles for age, and overweight as BMI > 85th percentile for age.
Table 2 displays the unadjusted 5-year incidence and relative risk of obesity for parous women compared with nulliparous women. The number of women who gave birth in each year was as follows: 304 in 1980, 296 in 1981, 283 in 1982, 272 in 1983, and 246 in 1984. Compared with nulliparous women evaluated over 5-year intervals as described above, parous women were 2.5 times more likely to develop obesity in the 5 years after childbirth. The relative risks of developing obesity after childbearing were similar across racial/ethnic groups.
TABLE 2.
Five-Year Incidence (per 100 Women) and Unadjusted Relative Risk of Obesity Among Parous and Nulliparous Women: National Longitudinal Survey of Youth, 1980–1990
| Nulliparous, % (No./Total) | Parous, % (No./Total) | Relative Risk (95% CI) | |
| Overall | 4.5 (69/1522) | 11.3 (159/1401) | 2.5 (2.1, 3.2) |
| Race/ethnicity | |||
| White | 3.6 (37/1023) | 9.1 (70/766) | 2.5 (1.9, 3.3) |
| African American | 6.5 (19/293) | 15.1 (56/372) | 2.3 (1.5, 3.4) |
| Hispanic | 6.3 (13/206) | 12.5 (33/263) | 2.0 (1.3, 3.2) |
| Maternal education level | |||
| Less than high school diploma | 7.5 (34/456) | 12.6 (88/697) | 1.7 (1.3, 2.3) |
| High school diploma | 4.3 (27/632) | 9.6 (48/500) | 2.2 (1.6, 3.0) |
| 1 or more years of college | 1.1 (4/376) | 11.5 (14/122) | 10.5 (4.4, 24.9) |
| Age at first birth, y | |||
| 11–17 | … | 5.6 (8/142) | 2.1 (1.1, 4.2) |
| 18–33 | … | 12.0 (151/1259) | |
| Parity | |||
| Nulliparous (Ref) | 4.5 (69/1522) | … | 1.00 |
| Primiparous | … | 8.6 (28/327) | 1.9 (1.7, 2.2) |
| Multiparous | … | 12.2 (131/1074) | 2.7 (2.2, 3.3) |
Note. CI = confidence interval.
Among the nulliparous group, the incidence of obesity was higher for minority women than for White women. For minority women who had given birth, the incidence of obesity was 37% to 66% higher than the incidence of obesity in White women who had given birth. Among nulliparous women, incidence of obesity covaried inversely with maternal education. The effect of the interaction between maternal education and childbirth on the incidence of obesity was statistically significant (P < .001), although this relationship was not present among parous women.
All of the childbearing women who became obese in their 5-year follow-up intervals (n = 159) developed obesity within 2 years of giving birth. Of these women, 89% (n = 142) remained at least significantly overweight (BMI ≥ 28 kg/m2) throughout the remainder of their follow-up periods.
Table 3 shows 5-year obesity incidences by race/ethnicity and parity. The lowest obesity incidence occurred in the nulliparous White group, with the highest incidence occurring among the African American and Hispanic multiparous groups. For White and African American women, nulliparous women had lower incidences of obesity than did primiparous and multiparous women. The obesity incidences of White and African American women increased with the birth of a single child and increased further for women with multiple births. For Hispanic women, the incidences of obesity were similar between nulliparous and primiparous women; however, the sample size of Hispanic primiparous women was small. Among all 3 racial/ethnic groups, the obesity incidence was highest for multiparous women. The race/ethnicity × parity interaction had an effect on the incidence of obesity, but the race/ethnicity × maternal education interaction and race/ethnicity × age interaction had no effect on obesity incidence.
TABLE 3.
Five-Year Incidence of Obesity per 100 Women, by Parity and Race/Ethnicity: National Longitudinal Survey of Youth, 1980–1990
| Nulliparous (n = 1522), % (No./Total) | Primiparous (n = 327) , % (No./Total) | Multiparous (n = 1074) , % (No./Total) | |
| White | 3.6 (37/1023) | 7.1 (12/168) | 9.7 (58/598) |
| African American | 6.5 (19/293) | 12.0 (13/108) | 16.3 (43/264) |
| Hispanic | 6.3 (13/206) | 5.9 (3/51) | 16.7 (30/212) |
Finally, Table 4 displays results from multivariable logistic regression models for the relative risk of developing obesity. Women with 1 or more births had 3.5 times the obesity risk of women who never gave birth. The relative risks of obesity for primiparous and multiparous women were almost 3 times and 4 times (respectively) that of nulliparous women, although the difference between the obesity risks of primiparous and nulliparous women was not statistically significant.
TABLE 4.
Multivariate Models for 5-Year Risk of Parity-Related Obesity: National Longitudinal Survey of Youth, 1980–1990
| Models | Unadjusted RRa (95% CI) | Adjusted RR (95% CI) |
| Given birth vs never given birth | 2.7 (2.0, 3.6) | 3.5 (2.4, 4.9) |
| Primiparous vs nulliparous | 2.0 (1.2, 3.1) | 2.8 (1.5, 5.0) |
| Multiparous vs nulliparous | 3.0 (2.2, 4.0) | 3.8 (2.6, 5.6) |
| Multiparous vs primiparous | 1.5 (0.97, 2.3) | 1.4 (0.89, 2.4) |
Note. RR = relative risk; CI = confidence interval. All models adjusted for chronological age, race/ethnicity, marital status, residence, baseline height and weight, smoking, and maternal education status.
Given the prospective nature of the data, RRs were approximated with odds ratios from logistic regression.
DISCUSSION
Our main findings show that the 5-year risk of developing obesity was 3.5 times greater among women who had given birth than among women who had never given birth. This parity-related risk of developing obesity was similar across racial groups. Although nulliparous African American and Hispanic women had a higher obesity incidence than did nulliparous Whites, the obesity incidence of African American and Hispanic women increased greatly with childbearing. For women who never had children, maternal education covaried inversely with the incidence of obesity. Interestingly, we found that the relative risk of obesity was similar between primiparous and multiparous women; however, primiparous and multiparous women had 3 to 4 times the obesity risk of nulliparous women. Finally, of the childbearing women who became obese in the 2 years following childbirth, only 11% returned to a normal BMI in the remainder of the 5 years following childbirth.
These findings provide important prospective evidence that childbirth contributes to the development of obesity. Childbirth (either primiparous or multiparous) appeared to increase a woman's risk of developing obesity relatively soon after delivery. This finding is troubling because most women who become obese subsequent to childbirth remain overweight or obese in the years following the perinatal period. Our findings also showed that childbirth contributed to the racial disparities demonstrated in obesity levels. The incidence of parity-related obesity was higher among African American and Hispanic women than among White women. This finding may be caused by racial differences in the influence of perinatal factors on the development of obesity. For example, White women are more likely to have excessive pregnancy weight gain than are minority women, but minority women tend to have greater postpartum weight retention than do White women.6,23 Additionally, maternal education appears to be protective only for women who have never had children, raising the question of whether this finding is a function of biology, social environment, or an interaction of the two.
In addition, primiparous and multiparous women had greater risk of obesity than did nulliparous women but similar risk to each other. This finding suggests that parity-related weight gain or retention has the greatest impact on obesity risk with the first childbirth; the contribution of subsequent births to obesity appears to be nominal. Future research should further investigate this finding by examining whether the interpregnancy intervals of multiparous women contribute to this phenomenon.
Our findings concur with those of Williamson et al., who found that primiparous adult women were more likely to develop major weight gain over a 10-year period than were nulliparous and multiparous women.17 They found no evidence that multiparous women gained more weight than did primiparous women.17 Similarly, a prospective study by Rosenberg et al. concluded that BMI was higher among primiparous women than among nulliparous women.24 They also determined that weight gain was greater among primiparous women than among multiparous women.24 Our findings also agree with those of Wolfe et al., which showed that parity-associated weight gain was considerable for White women and even greater for African American women. Specifically, African American women with increased parity were 5 times more likely to experience major weight gain than were those with no parity increase.9
Our findings differ from a prospective study by Brown et al., which found mean BMI to be lower for women with 1 or 2 births than for nulliparous women or for women with 3 or more births.12 The study also found that BMI increased as parity increased from 3 to 8 live births.12 However, the Brown sample was predominantly White, limiting its generalizability, and the authors did not establish that the birth of the child always preceded the occurrence of obesity.12
Strengths and Limitations
Several study limitations deserve comment. Although this data set was rich in perinatal and sociodemographic variables, it was limited because the parent study was originally designed to investigate labor-force issues and health. Our results may have underestimated the incidence and risk of obesity because weights were not measured annually, and because parity only reflected live births, excluding stillbirths and late-term miscarriages. The prevalence of obesity among young adults is greater today than it was in our study period of 1980 to 1990, which could affect incidence.1,25–27 We did not have information on family history of obesity to account for predisposition to obesity. Finally, there may be residual confounding of other factors that may explain the effect of pregnancy on obesity, such as excessive pregnancy weight gain and postpartum weight retention.
Despite these limitations, the strengths of our study are its prospective, community-based design and its large, diverse sample of young women of childbearing age followed over a 10-year period. The large sample of minority women strengthened the race/ethnicity-specific analyses, an especially important factor given that minority women are disproportionately affected by obesity and tend to be underrepresented in research studies. Finally, we allowed each woman to serve as her own control in the follow-up period.
Conclusions
Our findings demonstrate that childbirth increases the risk of becoming obese. The effects of parity on the risk of obesity are greater among minority women. Based on these findings, obesity-prevention efforts should target women during the postpartum period. One recommendation would be to identify the women at greatest risk—normal-weight women who become overweight, overweight women, and women who are obese at the 6-week postpartum visit—and encourage them to lose weight, giving them the target of returning to their pre-pregnancy weight by 1 year postpartum. Until more clinical and community-based weight-management interventions are developed, these women should be given access to extant weight-management resources, and their weight should be closely monitored within the first year postpartum.
The contribution of specific perinatal factors such as interpregnancy interval, excessive pregnancy weight gain, postpartum weight retention, and postpartum change in lifestyle need to be further examined. Future prospective studies or surveillance databases should include time-dependent perinatal variables that will allow for scrutiny of these variables’ relationships with obesity development.
Acknowledgments
This research was supported by a Harold Amos Medical Faculty grant from the Robert Wood Johnson Foundation, a Faculty Development Award from University Hospital Case Medical Center, a Clinical Research Professorship from the American Cancer Society, and a Family Medicine Research Center grant from the American Academy of Family Physicians.
Note. All funding sources had no role in data interpretation or in preparation, review, or approval of the article.
Human Participant Protection
No protocol approval was needed for this study because it relied on a publicly available data set that did not contain personal identifying information.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288:1723–1727 [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289:76–79 [DOI] [PubMed] [Google Scholar]
- 3.The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. Washington, DC: Public Health Service; 2001 [Google Scholar]
- 4.Linne Y, Barkeling B, Rossner S. Long-term weight development after pregnancy. Obes Rev 2002;3:75–83 [DOI] [PubMed] [Google Scholar]
- 5.Olson CM, Strawderman MS, Hinton PS, Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 year postpartum. Int J Obes Relat Metab Disord 2003;27:117–127 [DOI] [PubMed] [Google Scholar]
- 6.Parker JD, Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol 1993;81(5 (pt 1)):768–774 [PubMed] [Google Scholar]
- 7.Rookus MA, Rokebrand P, Burema J, Deurenberg P. The effect of pregnancy on the body mass index 9 months postpartum in 49 women. Int J Obes 1987;11:609–618 [PubMed] [Google Scholar]
- 8.Rooney BL, Schauberger CW. Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol 2002;100:245–252 [DOI] [PubMed] [Google Scholar]
- 9.Wolfe WS, Sobal J, Olson CM, Frongillo EA., Jr Parity-associated body weight: modification by sociodemographic and behavioral factors. Obes Res 1997;5:131–141 [DOI] [PubMed] [Google Scholar]
- 10.Arroyo P, Avila-Rosas H, Fernandez V, Casanueva E, Galvan D. Parity and the prevalence of overweight. Int J Gynaecol Obstet 1995;48:269–272 [DOI] [PubMed] [Google Scholar]
- 11.Billewicz WZ. Body weight in parous women. Br J Prev Soc Med 1970;24:97–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown JE, Kaye SA, Folsom AR. Parity-related weight change in women. Int J Obes Relat Metab Disord 1992;16:627–631 [PubMed] [Google Scholar]
- 13.Burke GL, Savage PJ, Manolio TA, et al. Correlates of obesity in young black and white women: the CARDIA Study. Am J Public Health 1992;82:1621–1625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coitinho DC, Sichieri R, D'Aquino Benicio MH. Obesity and weight change related to parity and breast-feeding among parous women in Brazil. Public Health Nutr 2001;4:865–870 [DOI] [PubMed] [Google Scholar]
- 15.Heliovaara M, Aromaa A. Parity and obesity. J Epidemiol Community Health 1981;35:197–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SK, Sobal J, Frongillo EA, Olson CM, Wolfe WS. Parity and body weight in the United States: differences by race and size of place of residence. Obes Res 2005;13:1263–1269 [DOI] [PubMed] [Google Scholar]
- 17.Williamson DF, Madans J, Pamuk E, Flegal KM, Kendrick JS, Serdula MK. A prospective study of childbearing and 10-year weight gain in US white women 25 to 45 years of age. Int J Obes Relat Metab Disord 1994;18:561–569 [PubMed] [Google Scholar]
- 18.NLSY79 User's Guide. Columbus, OH: Center for Human Resource Research; 2006. Available at: ftp://www.nlsinfo.org/pub/usersvc/NLSY79/NLSY79%202004%20User%20Guide/79text/front.htm. Accessed June 2006 [Google Scholar]
- 19.Basu AM, Stephenson R. Low levels of maternal education and the proximate determinants of childhood mortality: a little learning is not a dangerous thing. Soc Sci Med 2005;60:2011–2023 [DOI] [PubMed] [Google Scholar]
- 20.Miech R, Chilcoat H. Maternal education and adolescent drug use: a longitudinal analysis of causation and selection over a generation. Soc Sci Med 2005;60:725–735 [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics Clinical growth charts. Available at: http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/clinical_charts.htm. Accessed June 3, 2008 [DOI] [PubMed]
- 22.Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 1997 [Google Scholar]
- 23.Keppel KG, Taffel SM. Pregnancy-related weight gain and retention: implications of the 1990 Institute of Medicine guidelines. Am J Public Health 1993;83:1100–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Kumanyika SK, Adams-Campbell LL. A prospective study of the effect of childbearing on weight gain in African-American women. Obes Res 2003;11:1526–1535 [DOI] [PubMed] [Google Scholar]
- 25.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord 1998;22:39–47 [DOI] [PubMed] [Google Scholar]
- 26.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 2002;288:1728–1732 [DOI] [PubMed] [Google Scholar]
- 27.Ogden CL, Troiano RP, Briefel RR, Kuczmarski RJ, Flegal KM, Johnson CL. Prevalence of overweight among preschool children in the United States, 1971 through 1994. Pediatrics 1997;99(4):E1. [DOI] [PubMed] [Google Scholar]