Abstract
Objectives. We used community-partnered participatory research (CPPR) to measure collective efficacy and its role as a precursor of community engagement to improve depression care in the African American community of South Los Angeles.
Methods. We collected survey data from participants at arts events sponsored by a CPPR workgroup. Both exploratory (photography exhibit; n = 747) and confirmatory (spoken word presentations; n = 104) structural equation models were developed to examine how knowledge and attitudes toward depression influenced community engagement.
Results. In all models, collective efficacy to improve depression care independently predicted community engagement in terms of addressing depression (B = 0.64–0.97; P < .001). Social stigma was not significantly associated with collective efficacy or community engagement. In confirmatory analyses, exposure to spoken word presentations and previous exposure to CPPR initiatives increased perceived collective efficacy to improve depression care (B = 0.19–0.24; P < .05).
Conclusions. Enhancing collective efficacy to improve depression care may be a key component of increasing community engagement to address depression. CPPR events may also increase collective efficacy. Both collective efficacy and community engagement are relevant constructs in the South Los Angeles African American community.
Although depressive disorders are treatable, many people with such disorders, especially members of underserved minority groups, do not receive treatment.1–7 Access to high-quality depression care can be improved through evidence-based programs,8,9 but such programs are not widely disseminated in underserved communities.10 Collective action through cooperative efforts among service agencies and community members may be necessary to increase their implementation.11–16 However, little is known about how to engage underserved groups in efforts to improve depression care.
Perceived racism in health care, the stigma of mental illness, and lack of knowledge about depression may result in individuals in the African American community deciding not to seek help for depression.17,18 However, as noted by one of the members of the minority community that was the focus of study, “Depression is a silent killer. We need to get the word out to the community that we can do something about it.” In addition, distrust in services and research engendered by travesties such as Tuskegee and experiments on slaves in the antebellum period is a barrier to participation in research among African Americans.18–22 According to another study participant, “People in our community … have been involved with research before—the problem is universities never come back … and tell us what they did in our community.”
Community-based participatory research is recommended as one means of engaging members of minority groups in addressing health issues.12,15,23,24 In public health, community-based research focuses on social, structural, and physical environmental inequities through active involvement of community members, organizational representatives, and researchers in all aspects of the research process. Partners contribute their expertise to enhance understanding of a given phenomenon and integrate the knowledge gained with action to benefit the community involved.23
Both sides can gain from such an approach, as noted by another participating community member:
To participate with academics, the community can develop expertise in research—like [institutional review boards], data collection, and methods… . The academics get to learn about how to work in [the] community … being transparent, gaining trust, and planning with community instead of on community.
Community-partnered participatory research (CPPR), a variant of community-based participatory research, emphasizes equal power sharing among community and academic participants while engaging stakeholders and community members in planning, action, and research that have a mutual benefit.24–26 For example, as noted by one of the participants in our study: “Allowing the community to participate in the hypothesis, data collection, analysis, and interpretation gave the community partnership over every aspect of the project.”
Our study represented one component of a CPPR initiative called Witness for Wellness (http://www.witness4wellness.org), initiated in 2003 to reduce the burden of depression in underserved communities of color in South Los Angeles.26–29 In Witness for Wellness, a multi-agency council was developed under the leadership of Healthy African American Families (HAAF), the University of California at Los Angeles, the RAND Corporation, and Charles Drew University.26 The council developed a written agreement to reinforce CPPR principles and initiated 3 working groups including Talking Wellness, the group we studied.17,25,27,28
The Talking Wellness group focused on improving the capacity of the community to discuss depression and reduce stigma; community members suggested the approach of presenting community-generated arts events.27 The Talking Wellness group had 74 participants during January 2004 through November 2007, the period of work leading to this article: 10 academic members (7 White, 2 Asian American, 1 African American) and 64 members of the South Los Angeles African American community. We evaluated 2 events for this study: spoken word and comedy presentations and a photography exhibit. (Spoken word is a form of artistic performance in which poetry or stories are recited aloud.)
Our study involved several goals. The first was to explore whether concepts of collective efficacy and community engagement concerning depression care were important in the African American community of South Los Angeles and determine how they were related through causal modeling. Collective efficacy is a group's shared belief in its conjoint capabilities to improve a problem in the community (in this case, depression care). Community engagement refers to the perception that individual problems (in this case, depression and mental wellness) are problems of the community as a whole.
The second goal was to determine whether and how exposure to Talking Wellness arts events and other CPPR initiatives influenced community engagement. The third goal was to determine the feasibility of applying a CPPR paradigm of equal power sharing for community and academic partners through all phases of a rigorous research process, as evidenced through maintaining group membership across phases and completing products such as research protocols, data collection instruments, grant submissions, and research papers.
We expected that low levels of knowledge and high levels of stigma about depression would predict lower levels of community engagement or perceived collective efficacy around depression than would high levels of knowledge and low levels of stigma. In addition, we expected that exposure to Talking Wellness events and CPPR initiatives would increase community engagement.
We are not aware of other studies identifying pathways to community engagement as a means of addressing depression in minority communities.15,24 The attitudinal constructs we used in this study were derived from the Health Belief Model (i.e., in terms of perceived importance of a problem and stigma as a barrier),23,29 the theory of reasoned action and planned behavior (i.e., in terms of perceived norms and attitudes concerning a behavior),30 Bandura's social cognitive theory of collective efficacy as measured through individual perceptions,31–38 and the concept of community engagement from the CPPR model.25 Previous studies have shown that measures of collective efficacy are associated with health outcomes.39–42
METHODS
The Talking Wellness group staged 2 types of arts events during the Pan African Film Festival (as part of Black History Month in February 2005) at the Baldwin Hills Mall in South Los Angeles. Self-report surveys were distributed to attendees by academic and community members of Witness for Wellness. The events, venues, survey items, and study design were developed and pilot tested by The Talking Wellness group in monthly meetings conducted over the course of a year.17
Arts Events
Photo exhibit.
This exhibit featured 12 photos taken by community photographers depicting locations in South Los Angeles that they believed represented both positive (e.g., local historical landmarks) and negative (e.g., garbage dumps) environmental influences on mood. The exhibit was displayed at the Baldwin Hills Mall during the film festival; 8464 passersby were approached by trained community and academic staff and asked to view the exhibit and complete a survey after the viewing. Of the 793 (9.4%) individuals who agreed to do so, 746 (8.8%) were eligible for the study (i.e., they were 18 years or older) and provided legible responses.
Spoken word and comedy events.
The Talking Wellness group hosted 2 spoken word sessions during the festival, advertised via the festival brochure, circulated fliers, and verbal recruiting at the local mall. The events included a discussion of depression, an introduction to the Talking Wellness mission, and readings of poems by community members concerning their experiences with depression, sources of stress, and other personal experiences. Comedy routines were performed with similar themes. Each event was approximately 90 minutes in duration.
Audience members were asked to complete surveys including both preevent and postevent components. Data on sociodemographic characteristics were obtained from all participants before the event; knowledge and attitude items were completed after the event so as to avoid priming effects or sensitization to outcomes via preevent exposure. To improve the causal inference of our proposed model, we included preevent knowledge and attitude items for a random half of the participants. The 2 survey formats were ordered through a random number table before distribution. Of the 140 audience members, 107 (76.4%) returned surveys; 87 (62.1%) of these individuals were eligible (older than 18 years) and provided legible responses. Forty-three had available data for both preevent and postevent attitude items, and 44 had available data for postevent attitude items only.
Knowledge and stigma items were derived from an earlier survey, Partners in Care,43,44 and attitude items were developed that represented the community's sense of collective identity. During exploratory data analyses, we empirically identified item clusters post hoc, theorizing their relationship with each other and with constructs they represented (community engagement, collective efficacy, knowledge about depression) according to the community's lived experience and theory. (The collaborative process of measure construction and construct interpretation is illustrated later in the sections on collective efficacy and knowledge.)
Variables
Community engagement.
As mentioned earlier, we defined community engagement in the context of this study as the perception that depression and mental wellness are community problems. Four items were conceptualized a priori as measures of community engagement. Two applied to both the spoken word events and the photo exhibit: “Overcoming depression and wellness in the community requires planning and action” and “Depression and wellness are important issues for my community.” Two applied to the photo exhibit only: “I would recommend this photo exhibit to others in my community” and “This photo exhibit reinforced how people in my community are connected by shared experiences and cultural history.” Participants rated all items on a 5-point scale ranging from “strongly agree” to “strongly disagree”; a “don't know” option was also available. We formed scale scores by averaging pairs in each of these clusters.
Collective efficacy.
One item was used as a direct measure of collective efficacy: “I feel hopeful that our community can make progress on improving access to care for clinical depression.” Again, participants rated this item on a 5-point scale ranging from “strongly agree” to “strongly disagree,” with a “don't know” option also available. Surprisingly, preliminary factor analyses consistently paired this item with a second item: “Depression is a medical illness” (initially conceptualized as a depression knowledge item). When the Talking Wellness community members reflected on the pairing of these 2 items, they suggested the concept of “collectivistic orientation.” Individual community members' responses to the medical illness item may have reflected their belief that there is hope that depression can be helped through medical treatments, even though it is often viewed as intractable within the community.
Social stigma.
Six items were used to assess social stigma.43,44 Three items concerned personal attitudes: “I have no patience with a person who is always feeling blue,” “I would be embarrassed if people thought I was depressed,” and “I feel helpless to make a difference with someone who is always feeling blue.” Three items reflected perceived norms: “Most people think less of a person who has been depressed,” “Most people in the community would treat someone who has depression just as they would anyone,” and “Most people would be willing to accept someone who has had depression as a friend.” Respondents rated these items on the same 5-point scale used with community engagement and collective efficacy. Exploratory factor analyses identified distinct constructs for personal attitudes and perceived norms, so we formed 2 scales by averaging items.
Depression knowledge.
Six items identified by the Talking Wellness group as measuring “depression knowledge” were included. There was one global item: “How much do you think you know about depression?” Participants rated this item on a 4-point scale ranging from “a lot” to “almost nothing”; a “don't know” option was also available. Personal experiences with depression were assessed with 2 of the other 5 items: “Someone I know is depressed enough to need treatment” (rated on the same 5-point scale) and “Do you know someone who has received treatment for depression?” (with response options of “yes,” “no,” and “don't know”).
Although members of the Talking Wellness group assumed that these depression knowledge items (including the medical illness item transferred to the collective efficacy category) defined a single construct, bivariate correlations among the individual items were low (0.08–0.28), failing to identify any item clusters. Furthermore, none of the items displayed meaningful patterns with the other variables in our models. Thus, the depression knowledge items were omitted from the analyses described here.
Event exposure.
The spoken word surveys included 2 items assessing individuals' previous participation in Witness for Wellness and other partnered initiatives sponsored by HAAF. Item scores were summed. Event exposure was measured according to whether the first assessed attitude scores were preevent or postevent scores.
Sociodemographic factors.
The survey included items assessing participants' age in years, gender, self-reported ethnicity and race, education, and zip code of residence.
Data Analyses
We developed structural equation models (SEMs) including 3 latent variables (stigma, collective efficacy, and community engagement) identified in the exploratory factor analyses. A latent variable (similar to a factor in factor analysis) is a conceptual construct that is not directly measured; rather, it is mathematically inferred from 2 or more directly measured variables such as survey items.
In the first step of our modeling, we assigned individual variables as indicators (measures) of one of our 3 latent variables (constructs). In the second and third steps, we used regression procedures to link the latent variables in an effort to highlight the causal implications of our model. These SEMs summarized and reproduced the information in the correlation matrix among all variables.
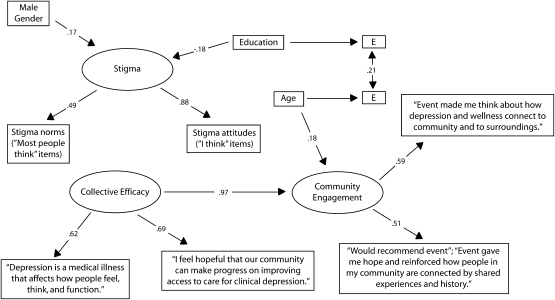
In the second step, we developed exploratory SEMs based on the photo exhibit data (n = 704; Figure 1). In this exploratory modeling, we used a combination of theory and trial and error to develop a model that reasonably fit the covariance structure among the individual items. We used a comparative fit index value above 0.90 as the criterion for goodness of fit.
FIGURE 1.
Post hoc model for the photography exhibit data set illustrating an analysis of 3 latent variables (stigma, collective efficacy, community engagement) and 3 single-item measured variables: Talking Wellness, South Los Angeles, CA, 2005.
Note. All pathways are standardized parameter estimates.
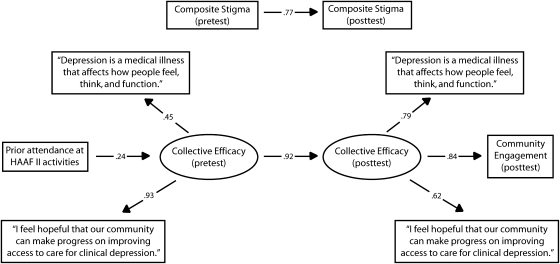
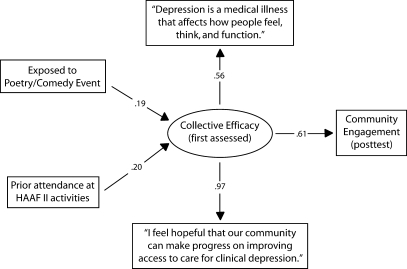
In the third step, we tested the model derived from this post hoc process in confirmatory analyses with 2 new data sets, the spoken word preevent and postevent (within participant) data illustrated in Figure 2 (n = 44) and the postevent-only (between participants) data illustrated in Figure 3 (n = 87). The analyses shown in Figures 2 and 3 fit the same model shown in Figure 1 in this new data set. Replication of a model in a new data set eliminated the possibility that the exploratory model was achieved through capitalization on chance.
FIGURE 2.
Confirmatory model focusing on within-participant (preevent–postevent) spoken word and comedy event data: Talking Wellness, South Los Angeles, CA, 2005.
Note. HAAF = Healthy African American Families. All causal pathway values are standardized parameter estimates. The composite stigma and community engagement variables were formed by averaging the 2 corresponding variables in Figure 1.
FIGURE 3.
Confirmatory model focusing on between-participant (first assessed or postevent only) spoken word and comedy event data: Talking Wellness, South Los Angeles, CA, 2005.
Note. HAAF = Healthy African American Families. All causal pathway values are standardized parameter estimates. The community engagement variable was formed by averaging the corresponding variables in Figure 1.
We used EQS (Multivariate Software Corporation, Encino, CA) to calculate preliminary models (spoken word events and photo exhibit) and the final model for spoken word data. We used Mplus (Muthén and Muthén, Los Angeles, CA) for the model shown in Figure 1 to combine the 20 imputations used to account for missing data at the item level. In all models, we made an a priori decision to model community engagement, the main outcome and an effect caused by other variables in the model.
The confirmatory models shown in Figure 2 (within participant) and Figure 3 (between participants) also modeled community engagement as a consequence of the other variables. These 2 models included as well a measure of CPPR event exposure (previous participation in Witness for Wellness or other HAAF initiatives). Given the small amount of data, we simplified the Figure 2 and Figure 3 models by removing sociodemographic variables and replacing the stigma latent constructs identified in the first modeling step with measured scale scores.
Missing Data
Nonresponses and “don't know” responses were defined as missing data. Missing data rates for items in the samples retained for analysis ranged from 0% to 28%. In the case of the photo data, we used a multiple imputation technique to account for item-level nonresponse and uncertainty in imputed values. Predictive mean matching methods were used to create 20 imputed data sets.45,46 We then used standard complete data methods to analyze each of the 20 complete data sets. The results across 20 imputed data sets were averaged via Mplus. We replaced missing values for spoken word data with means.
RESULTS
Sample Demographic Characteristics
Table 1 summarizes the demographic characteristics of the respondents. The majority of respondents were African Americans from Los Angeles County. Ethnic diversity was somewhat greater among the spoken word audience, and educational levels were higher among these individuals. Few respondents were without a high school education, and most (more than 70%) were employed.
TABLE 1.
Demographic Characteristics of Arts Event Respondents: Talking Wellness, South Los Angeles, CA, 2005
| Characteristic | Total, No. (%) | Attended Spoken Word and Comedy Events, No. (%) | Attended Photography Exhibit, No. (%) |
| Women Age, y | 485 (61.7) | 75 (68.8) | 410 (60.6) |
| 18–30 | 140 (18.6) | 10 (9.7) | 130 (20) |
| 31–40 | 153 (20.3) | 34 (33.0) | 119 (18.3) |
| 41–50 | 218 (29.0) | 26 (25.2) | 192 (29.5) |
| 51–65 | 206 (27.4) | 27 (26.2) | 179 (27.5) |
| > 65 Race/ethnicity | 31 (4.1) | 4 (3.9) | 27 (4.2) |
| African American or Black or African descent | 745 (94.9) | 97 (88.9) | 638 (95.3) |
| European American, non-Hispanic | 26 (5.6) | 9 (8.3) | 17 (2.5) |
| Hispanic | 43 (5.4) | 3 (2.8) | 40 (6.0) |
| Asian American/Pacific Islander | 8 (1.6) | 3 (2.8) | 5 (0.7) |
| American Indian | 7 (1.0) | 0 (0.0) | 7 (1.0) |
| Other | 25 (4.2) | 5 (4.6) | 20 (3) |
| Currently employed | 553 (72.5) | 80 (74.1) | 473 (71.0) |
| Educational level | |||
| Less than high school | 48 (6.1) | 4 (3.7) | 44 (6.6) |
| High school diploma or equivalent | 288 (35.9) | 24 (22.2) | 264 (39.5) |
| Associate degree | 145 (18.6) | 24 (22.2) | 121 (18.1) |
| Undergraduate degree | 166 (25.3) | 30 (27.8) | 136 (20.4) |
| Master's degree | 99 (17.7) | 22 (20.4) | 77 (11.5) |
| Doctoral degree | 23 (5.3) | 4 (3.7) | 19 (2.8) |
| Los Angeles City resident | 529 (68.4) | 65 (63.1) | 464 (70.9) |
| Los Angeles County resident | 712 (93.3) | 97 (94.2) | 615 (94.0) |
Structural Models
Exploratory analysis of photography exhibit data.
Figure 1 shows the results of the post hoc SEM focusing on (1) the relationships between measured variables (rectangles) and the latent variables (ovals) to which they had been assigned and (2) the relationships among the latent variable SEMs. The arrows emanating out to measured variables are analogous to factor loadings (i.e., the correlation between an item and a mathematical construct representing the variance shared by all indicators). Paths connecting latent variables are analogous to regressing one latent variable on another, although all parameters are estimated simultaneously in an SEM. All of the parameters illustrated in Figure 1 were statistically significant (P < .05).
In the upper left corner of Figure 1, the latent construct of stigma is identified according to 2 measured constructs (norms and attitudes). This latent construct was influenced by gender (perceived stigma was higher among men; B = 0.17) and education (higher educational levels led to lower perceived stigma; B = −0.18); education accounted for 3.2% and gender for 2.9% of the variance in stigma. The fact that the stigma construct was split into distinct subcomponents (norms and personal attitudes) was of little practical significance given the lack of relations between the stigma latent variable and the other key latent constructs (collective efficacy and community engagement). Collective efficacy, defined according to 2 measured items, was unrelated to stigma but strongly influenced community engagement (B = 0.97).
Confirmatory analyses of spoken word data.
This a priori model fit the data extremely well (comparative fit index = 0.96, root mean squared residual = 0.03; χ222 = 27.47; P = .19; Figure 2). The model confirmed that (preevent and postevent) stigma measures were not related to either collective efficacy or community engagement. There was a strong causal link from preevent collective efficacy to postevent collective efficacy (B = 0.92). As with the previous model, postevent collective efficacy was a strong precursor of postevent community engagement (B = 0.84). Consistent with our expectations, previous attendance at Witness for Wellness and HAAF initiatives (not measured in the photo data set) was associated with preevent collective efficacy (B = 0.24; z = 5.57; P < .001) and thus was indirectly related to both postevent collective efficacy and community engagement. It is highly unusual for a model to fit so well when applied to a new data set.
Figure 3 shows the alternative preevent–postevent analysis that allowed a between-participants evaluation of exposure to the spoken word event. Because the preevent data were common to both models, this analysis was not independent of that shown in Figure 2. Again, the a priori model provided an excellent fit to the data (comparative fit index = 0.96; root mean squared residual = 0.03; χ222 = 27.47; P = .19; Figure 3). The expected path from collective efficacy (as initially assessed) to postexposure community engagement was strong and significant (B = 0.61). Furthermore, both event exposure (B = 0.19) and previous attendance at Witness for Wellness and HAAF initiatives (B = 0.24; z = 5.57; P < .001) were independently associated with collective efficacy and thus indirectly related to community engagement.
Feasibility of Community-Partnered Participatory Research
Community participants took responsibility for designing and implementing the arts events. Survey constructs and items were collaboratively developed. Research participants were recruited and data were collected by community and academic members. Hypotheses and analysis plans were developed in joint meetings. Estimation of SEMs relied on academic expertise, but interpretation and modifications benefited from the input of all participants. Thus, CPPR principles can be used to support a rigorous if exploratory research effort.
DISCUSSION
Our exploratory factor analyses, exploratory SEMs, and confirmatory SEMs showed that perceived collective efficacy for improving depression care led to community engagement and the view of depression as a community concern. The models for which measures were available and appropriate revealed that previous exposure to partnered research initiatives and exposure to the spoken word event increased collective efficacy to improve depression care, thereby indirectly increasing community engagement.
Thus, initiatives and events designed to increase community engagement in mental health may do so through instilling a sense of collective efficacy. The arts events described here represented collaboration in action and, moreover, may have received attention because they were implemented through a research partnership, an unusual context for the sponsoring festival. They offered direct role modeling of commitment to discussing depression, which may have enhanced collective efficacy.33–37
In a surprise to the academic members of the Talking Wellness working group, stigma constructs were not significantly associated with community engagement or collective efficacy, despite the good reliability of these constructs (i.e., they loaded strongly on the stigma latent variable and had strong test–retest reliability). Community members of the Talking Wellness group were not surprised that stigma was unrelated to other variables, believing that this result may have reflected the broader community's interest in advocating for increases in availability of and access to quality health care for depression in South Los Angeles.
The failure of stigma to relate to other variables could also have been related to lower stigma levels among our educated sample. Alternatively, social stigma may be more salient to personal help-seeking outcome measures than to our community engagement outcome measure. Furthermore, we did not find an effect of partnered research initiatives or spoken word on stigma constructs. It may be important to initially build collective efficacy and engage the community in addressing depression and then lower social stigma with respect to care through targeted stigma-reduction interventions.47,48 Approaches designed to address collective efficacy may be especially important given the “collectivist” mind-set in most African American communities.40,49,50 Because reducing stigma was a goal of Talking Wellness, this was a difficult but important lesson.
Limitations
We relied on self-reported data from a convenience sample recruited from festival attendees in a single geographic area. We may have found different relationships among constructs outside the context of arts events or with African Americans of lower socioeconomic status. We defined several latent constructs post hoc but replicated them in an independent sample. As a result of the small samples for the spoken word and comedy events, we had low power to detect a link between other attitude constructs and stigma measures; thus, the absence of a link may have been a type 2 error. The individuals agreeing to complete the survey may have been more “engaged” members of the community, and our results may have overestimated the link between event attendance, collective efficacy, and community engagement.
Summary and Implications
In the context of CPPR, perceived collective efficacy may be an important precursor to community engagement. This article makes an important, if preliminary, contribution to the CPPR literature. We have shown that such interventions may require additional features to address the stigma of mental illness.
Furthermore, this study illustrates the promise of CPPR to support community and academic collaboration across the full range of rigorous research activities and community program development. “It was a breakthrough and a milestone. You got to see and know academia on a personal level. That was important for trust,” said one community member. “I saw this as validating my experience. And we got to show that the community has scholars as well,” said another.
Acknowledgments
Support for this project was provided by the Robert Wood Johnson Foundation (grant 038293); the RAND Corporation; the National Institute of Mental Health Research Center (grant P30 MH068639); Healthy African American Families II; Charles R. Drew University; Drew/University of California at Los Angeles (UCLA) Project EXPORT (grant MD00148/MD00182); the Research Center for Minority Institutions (grant 1U54RR022762-01A1); the National Institute of Mental Health (grant T32 MH19126-17 to the American Psychiatric Association Program for Minority Research Training in Psychiatry); the Klingenstein Third Generation Foundation Fellowship in Childhood and Adolescent Depression; the Magic Johnson Foundation; and the Black Hollywood Education and Resource Center.
This article is dedicated to the memories of Marlene Nishimoto-Horowitz and Andy Gardner.
We thank the Talking Wellness partners for their expert advice: Robert Brook, Paul Koegel, Naihua Duan, Deborah Glik, Gery Ryan, Bonnie Zima, Kavita Patel, Tanika Spates, Ruth Klap, Lingqi Tang, Lily Zhang, Susan Stockdale, Ricky Bluthenthal, Katy Minnium, Rachel Pearson, Brittany Butler, Keith Norris, Patrick Manalastas. We also thank the RAND Survey group, the staff at the UCLA Health Services Research Center and Healthy African-American Families, Gail Yeaple, Harry Yoon, Dale Chung, Janet Cummings, Patrick Link, Sequoia Mercier, Eric Mercier, V. Kali, Sharon McDaniel, Barbara Boulet, Martha Tucker, S. Pearl Sharp, Moza Cooper, and Ayuko Babu. Finally, we acknowledge the Pan African Film Festival, the poets and comedians who performed at the festival, the community staff who gave their time and effort, and the Talking Wellness and Witness for Wellness participants.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Mental Health: Culture, Race, and Ethnicity. Rockville, MD: US Public Health Service; 2001 [Google Scholar]
- 2.Brown C, Battista DR, Bruehlman R, Sereika SS, Thase ME, Dunbar-Jacob J. Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Med Care 2005;43:1203–1207 [DOI] [PubMed] [Google Scholar]
- 3.Brown DR, Ahmed F, Gary LE, Milburn NG. Major depression in a community sample of African Americans. Am J Psychiatry 1995;152:373–378 [DOI] [PubMed] [Google Scholar]
- 4.Cooper LA, Brown C, Vu HT, et al. Primary care patients' opinions regarding the importance of various aspects of care for depression. Gen Hosp Psychiatry 2000;22:163–173 [DOI] [PubMed] [Google Scholar]
- 5.Snowden LR, Pingitore D. Frequency and scope of mental health services delivery to African Americans in primary care. Ment Health Serv Res 2002;4:123–130 [DOI] [PubMed] [Google Scholar]
- 6.Wang PS, Bergland P, Kessler RC. Recent care for common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. J Gen Intern Med 2000;15:284–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Achieving the Promise: Transforming Mental Health Care in America. Rockville, MD: President's New Freedom Commission on Mental Health; 2003 [Google Scholar]
- 8.Miranda J, Schoenbaum M, Sherbourne C, Duan N, Wells K. Effects of primary care depression treatment on minority patients' clinical status and employment. Arch Gen Psychiatry 2004;61:827–834 [DOI] [PubMed] [Google Scholar]
- 9.Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA 2003;290:57–65 [DOI] [PubMed] [Google Scholar]
- 10.Frank RG, Huskamp HA, Pincus HA. Aligning incentives in the treatment of depression in primary care with evidence-based practice. Psychiatr Serv 2003;54:682–687 [DOI] [PubMed] [Google Scholar]
- 11.Wells KB, Miranda J. Reducing the burden of depression. JAMA 2007;298:1451–1452 [DOI] [PubMed] [Google Scholar]
- 12.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173–202 [DOI] [PubMed] [Google Scholar]
- 13.Israel BA, Eng E, Schulz AJ, Parker EA, eds. Methods in Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass Publishers; 2005 [Google Scholar]
- 14.Minkler M, Wallerstein N. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass Publishers; 2002 [Google Scholar]
- 15.Wallerstein N. Commentary: challenges for the field in overcoming disparities through a CBPR approach. Ethn Dis 2006;16(suppl 1):S146–S148 [PubMed] [Google Scholar]
- 16.Wells KB, Miranda J, Bruce ML, Alegria M, Wallerstein N. Bridging community intervention and mental health services research. Am J Psychiatry 2004;161:955–963 [DOI] [PubMed] [Google Scholar]
- 17.Chung B, Corbett CE, Boulet B, et al. Talking Wellness: a description of a community-academic partnered project to engage an African-American community around depression through the use of poetry, film, and photography. Ethn Dis 2006;16(suppl 1):S67–S78 [PubMed] [Google Scholar]
- 18.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 19.LaVeist T, ed. Race, Ethnicity, and Health: A Public Health Reader. San Francisco, CA: John Wiley & Sons Inc; 2002 [Google Scholar]
- 20.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health 1997;87:1773–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Randall V. Dying While Black. Dayton, OH: Seven Principles Press; 2006 [Google Scholar]
- 22.Thomas SB, Quinn SC. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health 1991;81:1498–1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed.San Francisco, CA: John Wiley & Sons Inc; 2002 [Google Scholar]
- 24.Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA 2007;297:407–410 [DOI] [PubMed] [Google Scholar]
- 25.Bluthenthal R, Jones L, Fackler-Lowrie N, et al. Witness for Wellness: preliminary findings from a community-academic participatory research mental health initiative. Ethn Dis 2006;16(suppl 1):S18–S34 [PubMed] [Google Scholar]
- 26.Wells KB, Staunton AA, Norris K. Building an academic-community partnered network for clinical services research: the Community Health Improvement Collaborative (CHIC). Ethn Dis 2006;16(suppl 1):S3–S17 [PubMed] [Google Scholar]
- 27.Jones A, Charla F, Butler BT, Williams P, Wells KB, Rodriguez M. The Building Wellness Project: a case history of partnership, power sharing, and compromise. Ethn Dis 2006;16(suppl 1):S54–S66 [PubMed] [Google Scholar]
- 28.Stockdale S, Patel K, Gray R, Hill DA, Franklin C, Madyun N. Supporting wellness through policy and advocacy: a case history of a working group in a community partnership initiative to address depression. Ethn Dis 2006;16(suppl 1):S43–S53 [PubMed] [Google Scholar]
- 29.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Behav 1984;11:1–47 [DOI] [PubMed] [Google Scholar]
- 30.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980 [Google Scholar]
- 31.Simons LG, Simons RL, Conger RD, Brody GH. Collective socialization and child conduct problems: a multi-level analysis with an African American sample. Youth Soc 2004;35:267–292 [Google Scholar]
- 32.Crocker J, Luhtanen R, Blaine B, Broadnax S. Collective self-esteem and psychological well-being among White, Black, and Asian college students. Pers Soc Psychol Bull 1994;20:s504–s513 [Google Scholar]
- 33.Bandura A. Social Foundations of Thought and Action: Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986 [Google Scholar]
- 34.Bandura A, ed. Self-Efficacy in Changing Societies. New York, NY: Cambridge University Press; 1995 [Google Scholar]
- 35.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997 [Google Scholar]
- 36.Bandura A. Exercise of human agency through collective efficacy. Curr Dir Psychol Sci 2000;9:75–78 [Google Scholar]
- 37.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1–26 [DOI] [PubMed] [Google Scholar]
- 38.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science 1997;277:918. [DOI] [PubMed] [Google Scholar]
- 39.Goddard RD, Hoy WK, Hoy AW. Collective efficacy beliefs: theoretical developments, empirical evidence, and future directions. Educ Researcher 2004;33:3–13 [Google Scholar]
- 40.Belgrave FZ, Townsend TG, Cherry VR, Cunningham DM. The influence of an afrocentric worldview and demographic variables on drug knowledge, attitudes, and use among African American youth. J Community Psychol 1997;25:421–433 [Google Scholar]
- 41.Utsey SO, Bolden MA, Williams O, III, Lee A, Lanier Y, Newsome C. Spiritual well-being as a mediator of the relation between culture-specific coping and quality of life in a community sample of African Americans. J Cross Cult Psychol 2007;38:123–136 [Google Scholar]
- 42.Cohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health 2000;90:230–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roeloffs C, Sherbourne C, Unutzer J, Fink A, Tang L, Wells KB. Perceived stigma among depressed primary care patients: predictors and utilization of services. Gen Hosp Psychiatry 2003;25:311–315 [DOI] [PubMed] [Google Scholar]
- 44.Dwight-Johnson M, Unutzer J, Sherbourne CD, Tang L, Wells KB. Can QI programs for depression in primary care address patient preferences for treatment? Med Care 2001;39:934–944 [DOI] [PubMed] [Google Scholar]
- 45.Tang L, Song J, Belin TR, Unutzer J. A comparison of imputation methods in a longitudinal randomized clinical trial. Stat Med 2005;24:2111–2128 [DOI] [PubMed] [Google Scholar]
- 46.Lavori PW, Dawson R, Shera D. A multiple imputation strategy for clinical trials with truncation of patient data. Stat Med 1995;14:1913–1925 [DOI] [PubMed] [Google Scholar]
- 47.Corrigan PW, Bodenhausen G, Markowitz F, Newman L, Rasinski K, Watson A. Demonstrating translational research for mental health services: an example from stigma research. Ment Health Serv Res 2003;5:79–88 [DOI] [PubMed] [Google Scholar]
- 48.Pinfold V, Huxley P, Thornicroft G, Farmer P, Toulmin H, Graham T. Reducing psychiatric stigma and discrimination: evaluating an education intervention with the police force in England. Soc Psychiatry Psychiatr Epidemiol 2003;38:337–344 [DOI] [PubMed] [Google Scholar]
- 49.Hunter CD. Cultural Orientation, Perceptions of Racial Discrimination, and Collective Self-Esteem Among African Americans and West Indian Americans. [dissertation] New York, NY: Columbia University; 2006 [Google Scholar]
- 50.Ogbonnaya AO. Person as community: an African understanding of the person as an intrapsychic community. J Black Psychol 1994;20:75–87 [Google Scholar]