Abstract
Objectives.We explored the oral health knowledge, attitudes, and activities of Early Head Start (EHS) staff members, parents, and pregnant women, along with their suggestions related to future oral health educational interventions targeting EHS children.
Methods. Nine focus groups were conducted with EHS staff, parents, and pregnant women. Audiotapes of sessions were transcribed and entered into ATLAS.ti 5.0 for coding and analysis.
Results. Attitudes about the importance of children's oral health among parents and pregnant women were mixed. Staff members voiced responsibility for children's oral health but frustration in their inability to communicate effectively with parents. Parents in turn perceived staff criticism regarding how they cared for their children's oral health. Gaps were noted in the oral health activities of EHS programs. Participants expressed confusion regarding the application of Head Start oral health performance standards to EHS. The need for culturally sensitive, hands-on oral health education was highlighted.
Conclusions. Tailored, theory-based interventions are needed to improve communication between EHS staff and families. Clear policies on the application of Head Start oral health performance standards to EHS are warranted. Educational activities should address the needs and suggestions of EHS participants.
Early childhood caries has emerged as a concern over the past few years because of its widespread and increasing prevalence, its inequitable distribution among preschool-aged children, and its negative consequences for children, their families, and public health programs.1–4 Many barriers to obtaining dental care exist for young children in most parts of the United States, particularly children in low-income families, and treatment failure rates can be high for those with elevated risk factors.5,6 Recent initiatives have explored innovative approaches to providing preventive and treatment services for these high-risk young children.7,8
The Head Start and Early Head Start (EHS) programs provide an excellent setting in which to develop and test oral health interventions for young children who are at high risk for early childhood caries.9–11 Built on 30 years of Head Start experience, the EHS program began in 1995 and now consists of approximately 650 local programs serving more than 60 000 children.12 Although EHS programs reach only about 10% of eligible children, they can play an important role in promoting the oral health of young children and families.
EHS programs operate under a set of performance standards adopted from the long-standing Head Start program requiring that the oral health needs of children and their families be addressed.5,13 Several of these standards relate to oral health activities and components such as oral examinations, access to oral health care, and preventive services provided directly to children.5,14 Because EHS programs offer services for pregnant women and infants soon after birth, they can intervene at an opportune time to help reduce risk factors for oral disease and promote good oral health practices before the onset of disease. By the time children are old enough to enroll in Head Start, many are already on a trajectory of poor oral health that is difficult to change.5
Creating a foundation for a lifetime of good oral health among EHS children requires a number of strategies.11,15 Among others, these strategies include (1) delivering effective oral health promotion services in the classroom to instill healthy habits, (2) educating and motivating parents to take an active role in their children's oral health, and (3) developing collaborative relationships within communities to ensure that EHS children have access to oral health care.
Although EHS is well positioned to have an impact on the oral health of young children and families, little is known about the oral health activities of EHS staff. Most of the small number of dental studies that have been conducted have focused on Head Start, which targets children 3 to 5 years of age (EHS includes children up to the age of 3 years). Even in the case of the Head Start program, however, relatively little is known about program effectiveness.
For example, the Task Force on Community Preventive Services, in an evaluation of the impact of early childhood development programs on health, concluded that there was insufficient evidence to determine the effectiveness of these programs in improving dental outcomes.16 Therefore, a large gap exists in our understanding of the oral health activities of EHS staff and the barriers that affect these activities, including characteristics of parents of enrolled children and pregnant women. We explored the oral health knowledge, attitudes, and activities of EHS staff members, parents, and pregnant women in relation to the oral health of EHS children, as well as their suggestions regarding future oral health educational interventions targeting EHS children.
METHODS
Study Design and Setting
We conducted a qualitative study using focus groups to gather information on the oral health of children enrolled in EHS programs. To our knowledge, qualitative research has not been used to study this topic, and such studies have been used only rarely to explore oral health issues related to preschool-aged children.17 We selected this approach because we were in the initial stages of designing oral health interventions for EHS programs in North Carolina and believed that it was an appropriate research design to provide an in-depth understanding of the determinants of children's oral health. We believed that the results derived from our research, coupled with other sources, would enable us to plan a comprehensive educational intervention.18
North Carolina has 18 EHS programs with a total of 1440 funded slots for pregnant women and children younger than 3 years. The 18 programs include 51 centers in 28 of the state's 100 counties. Approximately 420 staff members working directly with children or families are employed in these programs. All but 1 of the programs offer services for pregnant women and enroll newborns soon after birth. Because our long-term objective was to gain insights that could be used to develop an intervention aimed at improving children's oral health, we sought perspectives from participants representative of the state's programs.
Sample Selection
In establishing our focus groups, we selected a nonprobabilistic, purposive sample of 4 EHS programs geographically dispersed across the state. Programs were chosen to include the major racial/ethnic groups (White, African American, American Indian, and Latino) represented in the state's population. The health coordinator for each program arranged the focus group sessions and recruited all participants. Coordinators were instructed to select participants they believed would have opinions and views representative of their staff and parent enrollees.
We chose to conduct 9 focus group sessions in the 4 selected EHS programs. Four sessions were conducted with EHS program staff, 3 were conducted with parents of EHS children, and 2 were conducted with pregnant women enrolled in EHS.
Discussion Guide and Data Collection
We developed a discussion guide based on the activities and responsibilities identified in EHS performance standards and input from an advisory committee of EHS staff. The guide included 4 general areas of interest: opinions about and values placed on the oral health of young children and pregnant women, current practices related to the oral health of children, recommended oral health activities for young children and pregnant women, and suggestions for potential education and training activities.
The focus group sessions were conducted from October through December of 2004. Each session was between 45 minutes and 2 hours in duration and was tape recorded to ensure transcription accuracy. As a means of ensuring consistency across the focus groups, sessions were facilitated by one of a pair of project personnel with experience in focus group research. In addition, notes were taken during each session by an independent observer to aid in the analysis of the transcriptions. One session was conducted in Spanish with Latina parents of enrolled EHS children. As a means of assessing data accuracy, participants reviewed and commented on a summary of the discussions (provided by the interviewer) at the end of each focus group.
Participating parents and pregnant women were provided with lunch before each session as well as an incentive of $20 after the conclusion of the session. In addition, snacks were provided for all EHS staff participants.
Data Transcription, Coding, and Analysis
Session recordings were transcribed verbatim by a commercial company specializing in this work (Franklin Square Services Inc, Chapel Hill, NC). Research staff verified and corrected all transcripts while simultaneously listening to the recordings and reading the written transcriptions. A summary of each of the 9 sessions was prepared according to the major areas discussed. A separate summary for each type of participant (i.e., program staff, parents, and pregnant women), organized according to discussion topical area, was then prepared. From these documents an executive summary was prepared for discussion and input from all of the EHS health coordinators in the state.
Transcriptions from the 9 focus groups were imported into ATLAS.ti, a software package that allows qualitative analysis of textual data.19 One of the investigators who had been trained in the use of ATLAS.ti for qualitative data processing and analysis conducted a systematic examination of the text to identify, group, and code primary themes, along with subcategories that further explained the primary themes.20 Patterns of text were identified and labels (codes) assigned to each group through an iterative, comparative process of searching and reviewing the text.21 This content analysis in which codes were developed and refined continued until we were certain that all common and important themes and subcategories had been identified.
The results of the content analysis are presented according to the primary themes we identified in the text. Field notes and feedback from the health coordinators who reviewed the summaries of the focus groups were used to aid in interpretation of data. We also analyzed the frequency of occurrence of the primary and secondary codes, both overall and by type of focus group, to assess similarities and differences among staff, parents, and pregnant women. These frequencies were used to guide our choice of results to present and discuss as well, but they are not included here because of the large number of codes (49 in all).
RESULTS
The 9 focus group sessions included 31 staff members, 22 parents, and 13 pregnant women. All of the participants were female with the exception of one father in a parent session. The staff sessions included program directors, teachers, and family service, health, and education coordinators. One group of pregnant women was composed entirely of first-time expectant mothers; the other group was a mix of first-time mothers and women with other children, some of whom were already enrolled in EHS. Each of the selected EHS programs included a large proportion of parents from one of the major racial/ethnic groups represented in EHS. The racial/ethnic makeup of the staff in each focus group largely reflected that of parents from the program in question, with the exception of the group with Latino parents, in which most of the staff members were African American or White. Pregnant women were African American and White.
Table 1 displays selected characteristics of each of the EHS programs from which focus group participants were selected, as well as characteristics of all 18 programs in the state. The 4 selected programs were larger in terms of number of staff, children, and pregnant women than the average program in the state and included more minority staff members and parents, a result of our goal to adequately represent each of the 4 major racial/ethnic groups in the study. With respect to other characteristics, these programs were generally representative of the state's 18 programs as a whole (Table 1).
TABLE 1.
Comparison of the 4 EHS Programs From Which Focus Group Participants Were Selected and the State's 18 EHS Programs as a Whole: North Carolina, 2004
| Programs Participating in Focus Groups |
||||
| Characteristic | Focus Groups With Staff (n = 4) | Focus Groups With Parents (n = 3) | Focus Groups With Pregnant Women (n = 2) | All Programs (n = 18) |
| Mean no.a | ||||
| Staff | 49.5 | 52.3 | 55.5 | 26.4 |
| Children | 113.0 | 115.3 | 128.0 | 77.2 |
| Pregnant women | 18.5 | 20.0 | 30.0 | 9.0 |
| Staff | ||||
| Mean age, y Educational level, % | 38.2 | 37.0 | 38.1 | 38.3 |
| Some high school | 0.0 | 0.0 | 0.0 | 0.8 |
| High school diploma | 9.5 | 12.1 | 3.2 | 9.3 |
| Some college | 44.2 | 40.0 | 33.7 | 49.3 |
| Undergraduate degree | 39.0 | 39.3 | 52.6 | 31.8 |
| Graduate degree Race/ethnicity, % | 7.3 | 8.6 | 10.5 | 8.8 |
| White | 25.6 | 20.1 | 26.6 | 48.1 |
| African American | 55.6 | 56.1 | 70.2 | 37.9 |
| Latino | 2.2 | 2.9 | 0.0 | 4.0 |
| American Indian | 15.0 | 19.4 | 0.0 | 7.9 |
| Other | 1.6 | 1.4 | 3.2 | 2.1 |
| Parents | ||||
| Mean age, y Educational level, % | 28.0 | 26.6 | 26.9 | 28.0 |
| Some high school | 16.1 | 15.5 | 18.1 | 18.3 |
| High school diploma | 29.0 | 29.7 | 27.5 | 32.6 |
| Some college | 47.8 | 44.5 | 49.7 | 42.2 |
| Undergraduate degree Race/ethnicity, % | 7.1 | 10.3 | 4.7 | 6.9 |
| White | 14.4 | 11.8 | 16.8 | 35.7 |
| African American | 69.0 | 65.8 | 78.5 | 40.1 |
| Latino | 4.8 | 6.8 | 2.7 | 17.9 |
| American Indian | 11.4 | 15.5 | 1.3 | 5.7 |
Note. EHS = Early Head Start.
Average number of staff, children, and pregnant women in the 4 selected programs and the 18 programs in the state as a whole.
Six major themes emerged from the content analysis: (1) the importance of oral health for young children and pregnant women, (2) the consequences of tooth decay for children and families, (3) communication between parents and staff about oral health, (4) oral health practices in EHS programs and at home, (5) provision of professional dental services for EHS children, and (6) recommended educational activities for EHS programs. Results related to each theme are presented in the sections to follow.
Importance of Oral Health
A common subtheme was that staff acknowledged the importance of oral health for young children, particularly the importance of early dental care; however, the reasons why it is important were not consistently well understood. According to one staff member,
I think it's very important to start 'em real little… . I know we've started in these classrooms of Early Head Start when they're just real little. Once they get that first tooth broke through, even before then we use the little thing you slip on your finger and go across their gums and clean that for them.
Many staff members reported that EHS parents do not seem to place enough importance on their children's oral health. One staff member noted, “I really don't think it . . . crosses [parents'] minds that it is really, really important.” Another staff member expressed the belief that parents do not take their children to the dentist because they think “their children's teeth are going to fall out anyway.”
By contrast, many parents understood the importance of caring for children's teeth and developing good oral habits early in life. For example:
You should start caring for [teeth] early. Even my son, he's very young, but he has a couple of teeth. I believe you should brush them twice a day at least. Start early to get a routine of them brushing at least twice a day.
Comments from other parents, however, indicated that some did not recognize the importance of oral health care in young children. One noted that “baby teeth fall out anyway and don't have nerve endings, so why care for them?”
Pregnant women generally did not understand the importance of dental care during pregnancy. A number of misconceptions were expressed about the effects of pregnancy on teeth, as evidenced by statements such as the following: “Pregnancy sucks the calcium out of your teeth.” Most first-time expectant mothers lacked an understanding of the importance of primary teeth and how they should care for the oral health of their child after birth.
Consequences of Tooth Decay
A variety of perceived effects of tooth decay in children were discussed by both staff and parents. The consequences for children observed by staff included lack of participation in the classroom, pain, inability to eat properly, speech problems, and fear of going to the dentist. Staff also believed that diseased primary teeth could have negative consequences later in life and that parents' lives would be affected as well because of the financial implications of dental treatment. Health coordinators in particular expressed frustration in finding treatment for children affected by tooth decay.
Many parents also discussed their perceptions of the consequences of tooth decay for children, including pain, trouble sleeping, poor nutrition, crying, bad moods, and fear of dentists. The costs of dental treatment and missed work were mentioned as consequences for parents themselves. Parents voiced strong opinions regarding the negative emotional effects of childhood dental disease on both themselves and their children. For example, some parents mentioned feelings of guilt and the emotional toll of not being able to care better for their children's teeth:
And the parent feels bad when the child does have a cavity, and feels like, “Well, what did I do, and what didn't I do, why [does] the child [have] that?”
I think the emotional pain they go through with their teeth having to be done that way, and having to be put to sleep and have their teeth worked on, that's an ordeal.
Communication Between Parents and Staff
Staff and parents both expressed frustration in regard to their efforts to communicate with each other about oral health, the most common theme in the study. Many staff members struggled in achieving effective communication with parents and felt unable to persuade them that oral health is important and should be a priority at home. One staff member commented: “Some are going to take it a lot easier, some are going to be ‘Oh, okay,’ nod their head and go out the door.”
In turn, parents at times believed that they were not well understood by EHS staff, even perceiving criticism and unfair judgment. Parents expressed difficulties in managing their demanding lives and stated that staff members sometimes did not understand what parents go through from day to day. In the words of 2 parents:
They can give us advice, but this is our child so we're going to still do it the way that we believe is right. I mean, I'll listen to the advice that they give me, but I'm still going to have my own opinions about it, and deal with that in my manner.
I would take friendly advice, but not like criticism, like you're doing it wrong. Like maybe suggestions or something.
Oral Health Practices
The oral health practices of EHS children as described by staff were generally age appropriate and often creative but also reflected a need for continuing education of staff to update dental knowledge and practices. Teachers engage in various activities to teach children how to care for their teeth and attempt to transmit educational messages to children through songs and other classroom activities. In accordance with Head Start oral health standards, staff reported that children's teeth were brushed after meals and that infants' gums were wiped after feedings. All of the programs reported serving healthy foods, not allowing “sippy cups” or pacifiers, and using bottles only at mealtimes.
However, other Head Start standards related to prevention, such as educational activities for parents, varied among the programs. American Indian program staff reported that they had offered workshops on oral health for parents. By contrast, staff from the other 3 programs had not offered oral health educational workshops for parents. In addition, staff use of toothpaste to brush children's teeth in the centers was not consistent across programs.
Parents expressed frustration in their attempts to care for their child's teeth because of their busy schedules, conflicting life demands, a lack of cooperation from their child, or a lack of knowledge about how to brush a young child's teeth. Parents mentioned a variety of reasons for not practicing good oral hygiene for their children, including “I'm too tired at bedtime to struggle with my child” and “It's just not a priority for me.”
Although some parents understood the importance of children's oral health, they reported that they were unable to determine how to incorporate oral health practices into their daily routines. Many parents also expressed great frustration at the pervasive availability of sweets and did not have confidence in their ability to keep them out of their children's diet.
Most parents were unaware of the importance of fluoride among high-risk children. One of the biggest problems in maintaining oral health mentioned by parents was weaning their children from the bottle, which they found difficult to do by the recommended age. Many expressed the opinion that use of a bottle was the only way they could get their child to sleep at night.
Provision of Professional Dental Services
Staff members reported that dental screenings are a routine part of all EHS programs. Each program arranges for a dental screening and assists families in obtaining treatment when needed. However, considerable differences in the interpretation of the Head Start performance standards as they apply to dental screening of EHS children were observed among programs. Some interpreted the standards to mean that EHS children must receive an examination by a dentist just as Head Start children do, and others interpreted them to mean that dental screenings in the EHS center or a medical setting may be counted toward meeting the performance standards outlined for EHS children. Staff also demonstrated awareness of area medical providers who perform dental screenings of young children as part of a Medicaid statewide program.22
Some EHS staff, particularly health coordinators, believed that they were effective in locating dentists to provide for the oral health treatment needs of their children, often under challenging conditions. When needed to ensure that care is received, transportation, financing, and translation services are provided to EHS families. However, most staff expressed concern and frustration that, as a result of the shortage of dental providers who treat young children, parents often must travel long distances, wait long periods for an available appointment, or have their child go without treatment.
Most parents were unsure of the recommended age for the first dental visit, and few had taken their child for a dental checkup, generally only visiting the dentist when a problem arose. Pregnant women reported varying experiences in obtaining dental care during pregnancy. Some had no trouble scheduling an appointment for a checkup, whereas others were unable to find a provider who would see them.
Recommended Educational Activities
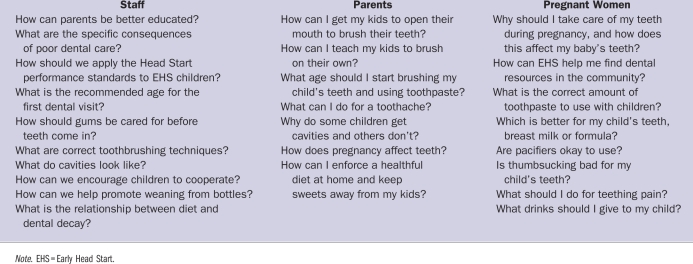
A common theme was the frustration expressed by participants regarding the lack of oral health information and misinformation on a number of preventive dentistry activities. They offered thoughts on the kinds of information they would like included in oral health–related interventions for EHS programs (see the box on this page). For example, parents wanted to know the age to start tooth brushing and to start using fluoridated toothpaste, and staff wanted to know when children should visit the dentist for the first time.
Oral Health Information Sought by Focus Group Participants: North Carolina, 2004
Focus group participants also discussed the need to gain skills to care for children's oral health needs. For instance, staff noted that skills training would increase their confidence in educating children and communicating with parents in an effective manner. Also, some staff members wanted to know how to integrate oral health information into their existing curriculum and how to better communicate with parents about the importance of oral health. Other staff mentioned the need to know how to work effectively with children who are uncooperative while their teeth are being brushed. Parents also expressed a desire to know how to manage an uncooperative child during oral hygiene care.
Participants had numerous suggestions on how training should be conducted. They emphasized that training should be “participatory” and “hands on.” To meet these goals, some participants suggested having demonstration activities that would include role playing between parents and children.
Finally, a number of staff and parents discussed cultural sensitivity. They mentioned that parents come from diverse cultural backgrounds and that health education messages might be better received if they were culturally and linguistically appropriate.
DISCUSSION
Valuable information and insights were gleaned from the participants in our focus groups regarding their oral health knowledge, attitudes, and activities as well as their suggestions on oral health education interventions targeting EHS children. Overall, we did not find any major differences in participants' comments according to race or ethnicity.
Staff and parents were generally knowledgeable about oral health in young children, although gaps were noted. We also received a number of mixed messages from parents and pregnant women about their attitudes and practices associated with their children's oral health. Despite the sentiment expressed that children's oral health is important, few parents discussed taking appropriate oral health preventive measures for their children other than tooth brushing. Comments revealed that parents and pregnant women had a range of attitudes, both positive and negative, toward oral health in young children. Studies have shown that one's culture, experiences, and beliefs strongly influence one's oral health attitudes.23 The ways in which oral health education messages can address divergent beliefs and attitudes that adversely affect the oral health of young children need to be considered in planning any educational intervention for this population.
Our results provide justification for designing intervention programs to help reduce the burden of early childhood caries and its impact on the quality of life of children and their families.24 Comments from our focus group participants provide a vivid account of the importance of oral health and how it affects the lives of children and the parents and staff who care for them. Parents reported effects of dental disease in a number of areas and particularly conveyed its emotional consequences, for example their feelings of guilt about not being able to prevent tooth decay or extensive dental treatment in their children.
The functional and psychological effects of oral diseases among EHS children, parents, and staff members should be considered as an outcome in intervention studies conducted with the EHS child population. Such an approach would involve recognition of the importance of parents' perspectives on how dental disease in their children influences their lives, complementing the biological perspective prevalent in the literature.
A strongly expressed theme that emerged from both staff and parent focus group sessions was the need for more effective ways to communicate about oral health. Staff believed that they were responsible for the oral health of enrolled children but were at times frustrated by their inability to communicate effectively with parents. Parents expressed frustration with what they sometimes perceived as criticism from staff members regarding how they cared for their children's dental needs. This lack of communication was exacerbated by the discrepancy between the value many parents placed on their children's oral health and staff members' beliefs that parents had a low regard for their children's oral health. Staff may have misinterpreted parents' lack of time and inability to incorporate oral health habits into their daily lives as their placing a low value on oral health.
A study in which Ohio Head Start staff and parents were surveyed produced similar findings. Most staff (67%) surveyed in that study believed that parents did not value oral health care for their children, whereas parents reported that they valued oral health care.25
This discordance between staff members and parents raises important practice implications. For example, with the understanding that parents value their children's oral health, staff members could devote less time and energy to persuading parents about the importance of oral health and more to providing useful and practical information building on parents' knowledge, experience, and readiness to change. Furthermore, by repeatedly stressing the point that oral health is important to parents who already possess this belief, staff may appear to be putting parents down. This approach can in turn decrease the likelihood that health education messages are heard and accepted.26
Because of the communication problems uncovered in this study, we are in the process of investigating approaches to communicating health information that may be particularly suited to helping EHS staff assist parents in improving the oral health of their children.27 A number of well-developed approaches to health behavior change focus on identifying an individual's stage of change (or readiness to change) and providing skills to facilitate the individual's progression along different stages.
Motivational interviewing,28 an individualized, semidirective approach that recognizes that people who need to make behavioral changes are at different levels of readiness, may be one approach to help move parents toward adopting desirable oral health behaviors. According to the basic principles of motivational interviewing, the person providing advice must express empathy toward the person being counseled, as well as exploring discrepancies between deeply held values and day-to-day behaviors, accepting the person's reluctance to change, presenting options, and supporting the person's self-efficacy. Motivational interviewing has not been applied widely in dentistry, but results in other settings show promise.29,30 We are currently using this approach to test interventions designed to support appropriate parental oral health behaviors and simple communication techniques.
This study produced a number of positive findings with respect to current activities related to children's oral health. Staff members confirmed that children in the 4 EHS programs receive some of the oral health preventive activities called for in the Head Start performance standards. EHS programs appear well equipped to care for children's oral health through the provision of balanced, noncariogenic diets; tooth brushing; and creative play for educational purposes. Also, when local resources permit, staff effectively network with local providers to obtain needed treatment.
However, insights gained in the focus group sessions also raised several concerns about current activities. For example, many of the pregnant women in the focus groups had not visited a dentist during their pregnancy. This finding is consistent with results from other studies suggesting that economically disadvantaged women are less likely than are other women to visit a dentist during pregnancy.31 Also, despite the fact that Head Start and EHS standards require meaningful involvement of parents in promoting the oral health of their children, few parent education activities were reported by staff members. Accordingly, effective strategies to prevent dental caries in EHS children should include the education of prospective and new parents as a means of instilling positive parenting behaviors.32
Our results suggest that clearly defined policy guidance is needed for EHS programs. Historically, Head Start performance standards have been applied to EHS programs without consideration of the differences in developmental stages of the children enrolled in the 2 programs. We found that staff and parents were confused about the age at which children should have their first oral health clinical assessment, whether it should be a screening or examination, and who should provide that service.
At the time of this study, most programs actively practiced oral hygiene in the centers, but staff members were confused about the use of fluoridated toothpaste. The Head Start Bureau has recently provided clarification on some of these policies.14 Our hope is that through continued research on educational interventions in the early childhood education setting, further evidence-based program policy guidelines can be developed and training provided so that guidelines are adopted and understood in EHS settings.
Participants' suggestions generated useful information regarding future dental health education interventions targeting EHS staff, parents, and pregnant women, including the importance of primary teeth and professional visits to dental and medical clinics for preventive dental services. A number of issues cut across focus groups, such as the need for culturally sensitive materials; hands-on, participatory educational activities; and simple, clear educational messages. Pregnant women in particular need to be informed given that often they do not have a clear understanding of the importance of caring for their oral health during pregnancy and that they have varying degrees of knowledge regarding how to care for young children's dental needs.
Limitations
The qualitative nature of this study may limit the conclusions that can be drawn from the findings. Participants made up a convenience sample recruited by EHS health coordinators. Although all of the state's major racial/ethnic population groups were represented in the sample, responses from participants may not have been representative of the larger population of EHS staff, parents, and pregnant women. Another limitation involved the differences between the cultural backgrounds of focus group facilitators and participants, which may have limited the focus group discussions. However, the extensive amount of information collected, coupled with repetition of themes, minimizes the significance of this limitation.
Conclusions
This study is one of the few to examine issues related to the oral health of EHS children. It contributes to the literature by helping to identify the knowledge, attitudes, practices, and suggestions of a diverse group of EHS staff members, parents, and pregnant women relevant to the oral health of EHS children. Such experiential knowledge not only has implications for the design of oral health interventions in North Carolina EHS programs; it also has broader implications for EHS programs elsewhere and for other early education and child-care programs that enroll low-income children. Further research is required in EHS programs in other regions of the country to validate and build on the findings of this investigation.
Acknowledgments
Funding for this project was provided by the Centers for Medicare and Medicaid Services, Health Resources and Services Administration, and the Centers for Disease Control and Prevention (grant 11-P-91251/5).
Human Participant Protection
This study was approved by the institutional review board of the University of North Carolina, Chapel Hill. Participants provided informed consent.
References
- 1.Edelstein BL, Douglass CW. Dispelling the myth that 50 percent of US schoolchildren have never had a cavity. Public Health Rep 1995;110:522–530 [PMC free article] [PubMed] [Google Scholar]
- 2.Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000 [Google Scholar]
- 3.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11 2007;(248):1–92 [PubMed] [Google Scholar]
- 4.Inglehart MR, Filstrup SL, Wandera A. Oral health-related quality of life in children. In: Inglehart MR, Bagramian RA, eds. Oral Health-Related Quality of Life. Chicago, IL: Quintessence Publishing Co Inc; 2002:79–88 [Google Scholar]
- 5.Edelstein BL. Access to dental care for Head Start enrollees. J Public Health Dent 2000;60:221–229 [DOI] [PubMed] [Google Scholar]
- 6.Berkowitz RJ, Moss M, Billings RJ, Weinstein P. Clinical outcomes for nursing caries treated using general anesthesia. ASDC J Dent Child 1997;64:210–211, 228 [PubMed] [Google Scholar]
- 7.Brown A, Lowe E, Zimmerman B, Crall J, Foley M, Nehring M. Preventing early childhood caries: lessons from the field. Pediatr Dent 2006;28:553–560 [PubMed] [Google Scholar]
- 8.American Dental Association State and community models for improving access to dental care for the underserved—a white paper. Available at: http://www.ada.org/prof/resources/topics/topics_access_whitepaper.pdf. Accessed July 15, 2008
- 9.Zigler E, Piotrkowski CS, Collins R. Health services in Head Start. Annu Rev Public Health 1994;15:511–534 [DOI] [PubMed] [Google Scholar]
- 10.Karoly LA, Kilburn MR, Cannon JS. Early Childhood Interventions: Proven Results, Future Promise. Santa Monica, CA: RAND Corporation; 2005 [Google Scholar]
- 11.Early Head Start National Resource Center A holistic approach to health and safety. Available at: http://www.headstartinfo.org/pdf/holistic_health_safe_TA7.pdf Accessed July 18, 2008
- 12.Head Start Bureau Head Start fact sheet. Available at: http://www.acf.hhs.gov/programs/ohs/about/fy2007.html Accessed July 18, 2008 [Google Scholar]
- 13.US Department of Health and Human Services, Administration for Children and Families Head Start performance standards. Available at: http://www.access.gpo.gov/nara/cfr/waisidx_06/45cfr1304_06.html. Accessed July 18, 2008
- 14.US Department of Health and Human Services, Administration for Children and Families Oral health—revision. Available at: http://eclkc.ohs.acf.hhs.gov/hslc/Program%20Design%20and%20Management/Head%20Start%20Requirements/PIs/2006/resour_pri_00109_122006.html. Accessed July 18, 2008
- 15.Crall J. Policy and program considerations for improving oral health in EHS/Head Start. Available at: http://www.hsnrc.org/HSB-MCHB.cfm. Accessed July 18, 2008
- 16.Anderson LM, Shinn C, Fullilove MT, et al. The effectiveness of early childhood development programs: a systematic review. Am J Prev Med 2003;24:32–46 [DOI] [PubMed] [Google Scholar]
- 17.Gussy MG, Waters E, Kilpatrick NM. A qualitative study exploring barriers to a model of shared care for pre-school children's oral health. Br Dent J 2006;201:165–170 [DOI] [PubMed] [Google Scholar]
- 18.Green LW, Kreuter MW. Health Promotion Planning: An Educational and Ecological Approach. 3rd ed.Mountain View, CA: Mayfield Publishing Co; 1999 [Google Scholar]
- 19.Muhr T. User's Manual for ATLAS.ti 5.0. Berlin, Germany: ATLAS.ti Scientific Software Development GmbH; 2004 [Google Scholar]
- 20.Krueger RA. Focus Groups: A Practical Guide for Applied Research. Thousands Oaks, CA: Sage Publications; 1994 [Google Scholar]
- 21.Ryan G, Bernard H. Data management and analysis methods. In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: Sage Publications; 1994:769–802 [Google Scholar]
- 22.Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ 2003;67:876–885 [PubMed] [Google Scholar]
- 23.Sisson KL. Theoretical explanations for social inequalities in oral health. Community Dent Oral Epidemiol 2007;35:81–88 [DOI] [PubMed] [Google Scholar]
- 24.Slade GD, Resine ST. The Child Oral Health Impact Profile: current status and future directions. Community Dent Oral Epidemiol 2007;35(suppl 1):50–53 [DOI] [PubMed] [Google Scholar]
- 25.Siegal MD, Marx ML, Cole SL. Parent or caregiver, staff, and dentist perspectives on access to dental care issues for Head Start children in Ohio. Am J Public Health 2005;95:1352–1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson LS, Story M. Perceptions of overweight and obesity in their community: findings from focus groups with urban, African-American caretakers of preschool children. J Natl Black Nurses Assoc 2003;14:28–37 [PubMed] [Google Scholar]
- 27.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed.New York, NY: Guilford Press; 2002 [Google Scholar]
- 28.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract 2005;55:305–312 [PMC free article] [PubMed] [Google Scholar]
- 29.Weinstein P, Harrison R, Benton T. Motivating mothers to prevent caries: confirming the beneficial effect of counseling. J Am Dent Assoc 2006;137:789–793 [DOI] [PubMed] [Google Scholar]
- 30.Harrison R, Benton T, Everson-Stewart S, Weinstein P. Effect of motivational interviewing on rates of early childhood caries: a randomized trial. Pediatr Dent 2007;29:16–22 [PubMed] [Google Scholar]
- 31.Lydon-Rochelle MT, Krakowiak P, Hujoel PP, Peters RM. Dental care use and self-reported dental problems in relation to pregnancy. Am J Public Health 2004;94:765–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boggess KA, Edelstein BL. Oral health in women during preconception and pregnancy: implications for birth outcomes and infant oral health. Matern Child Health J 2006;10:S169–S174 [DOI] [PMC free article] [PubMed] [Google Scholar]


