Abstract
Background
Operation for MEN1 related hyperparathyroidism includes a neck exploration with resection of 3.5 or 4 parathyroid glands and transcervical thymectomy (TCT). We reviewed our experience with initial operation for MEN1 HPT to determine the outcome and utility of routine TCT.
Methods
All patients with MEN1 who underwent initial neck exploration from 1993 – 2007 under an IRB-approved protocol were reviewed.
Results
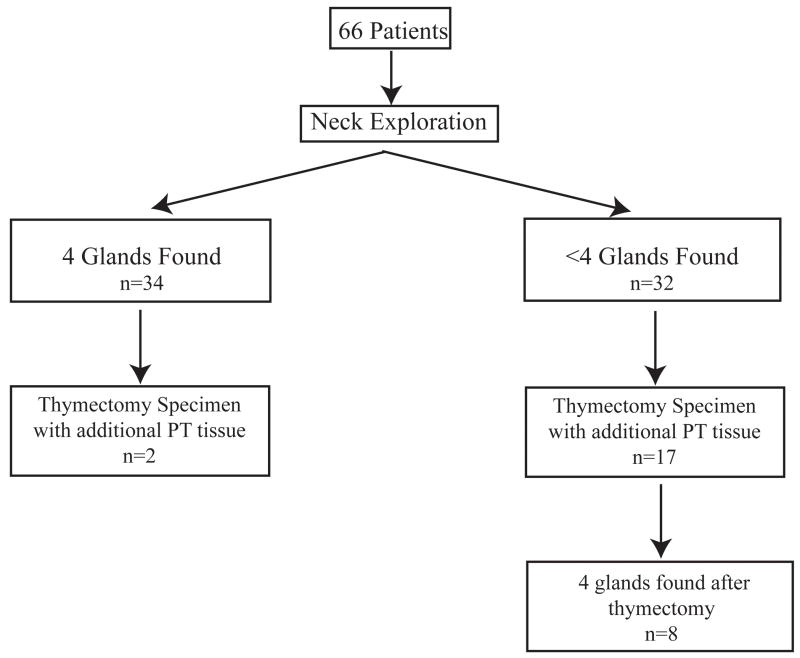
We identified 66 patients with initial surgery for HPT in MEN1. In 34 patients, four glands were found and in 32 patients, less than four glands were found. In two of the 34 (6%) and 17 of the 32 (53%), intra-thymic parathyroid tissue was found on permanent pathology. No thymic carcinoid tissue was found in any specimen.
Conclusions
These data highlight the importance of performing TCT when less than four entopic parathyroid glands are found at first operation.
INTRODUCTION
Multiple endocrine neoplasia type 1 is an autosomal dominant familial cancer syndrome with a prevalence of 1 in 10,000 to 1 in 100,000.1 Endocrine manifestations include pituitary, parathyroid, and enteropancreatic endocrine tumors, as well as other rarer tumors.1,2 The MEN1 gene, and its protein product menin, were identified in 1997; most of the mutations predicted a truncated protein product and thus suggest a loss of function role for MEN1 in tumorigenesis.1 Primary hyperparathyroidism (HPT) due to parathyroid tumor(s) is usually the earliest and most frequent manifestation of MEN1 with a penetrance of almost 100% by age 50.2 Parathyroid disease in MEN1 patients is multiglandular in nature due to its hereditary basis, and all parathyroid tissue is generally considered abnormal or at high risk for tumors.3
The recurrence rate for hyperparathyroidism in sporadic patients has been reported to be approximately two percent.4 Recurrence rates in MEN1 patients are much higher, ranging from 14 to 69 percent depending on the operation performed, time after operation, and series.5–8 The high recurrence rates and understanding of the underlying genetic mechanisms have led to efforts to clear as much abnormal parathyroid tissue as possible without causing permanent hypoparathyroidism.
Transcervical thymectomy (TCT) has often been performed with neck exploration in MEN1 patients and mainly at initial parathyroidectomy.7–10 The rationale for this has been concern that there may be ectopic or missing parathyroid tissues in the thymus.11 An association between highly aggressive thymic carcinoid tumors and MEN1 has also been described.12–14 However, no study has systematically studied the yield of these tissues in thymectomy specimens performed with parathyroid resection in MEN1 patients. We reviewed our experience with initial parathyroid resection and TCT for all MEN1 patients over a 14 year period to determine the utility of performing routine TCT.
METHODS
Sixty six patients with MEN1-related HPT who underwent initial neck exploration with TCT from 1993 to 2007 were identified and their charts retrospectively reviewed. These patients were admitted to the NIH under an IRB approved clinical protocol and all gave informed consent. We defined MEN1 HPT as occurring within a known MEN1 kindred or in a patient with pancreatic and/or pituitary lesions.
Demographic information, signs and symptoms at presentation or screening, and duration of symptoms when present were collected. Information regarding kindred, mutational status, and other manifestations of MEN1 were collected as were pre- and post-operative serum and ionized calcium values, pre-, intra-(when available), and postoperative parathormone values. Data regarding the types and results of pre-operative tumor localization studies were also collected.
All peri-operative data, operative notes, and pathology reports were reviewed for the number of glands the surgeon found in the neck exploration and the thymectomy specimen. The current NIH preference at an initial operation for these patients is a transcervical incision and subtotal (3.5 gland if four glands are found) resection without fresh parathyroid autotransplantation.15 All patients underwent transcervical thymectomy. Thymic tissue is identified on both sides of the neck and dissected in a substernal manner in order to resect as much thymic tissue as possible down to the inominate and below if it can safely be removed via the collar incision. This typically results in removal of an estimated 30–40% of the thymus. Pathology reports were also reviewed for the presence of any carcinoid tissue in thymectomy specimens. Follow-up data were obtained when available.
For the purpose of analysis, we divided the patients into two groups. The first group consisted of patients in whom four glands were found during the neck exploration and before TCT was performed, and the second group consisted of those patients in whom gland(s) were still unaccounted for prior to TCT. The yield of additional parathyroid and any carcinoid tissues as well as recurrence data were compared between these groups.
These groups were also compared with respect to pre-operative data. A chi-squared test or Fisher’s exact test, as appropriate, was used to compare dichotomous characteristics. Counts of signs, symptoms, or signs plus symptoms were compared between the groups using an exact Cochran-Armitage test for trend.16 The distribution of kindred vs. lesion vs. both was compared between groups using Mehta’s modification to Fisher’s exact test.17 Continuously distributed parameters were compared between groups using a Wilcoxon rank sum test since many parameters were not normally distributed. All p-values are two-tailed and have not been adjusted for multiple comparisons.
RESULTS
Features of HPT and MEN1
Demographic information for all patients is presented in Table 1. There were eight kindreds with multiple family members in the patient cohort. All but two patients underwent one or more pre-operative non-invasive parathyroid tumor localization studies; no patients were found to have images suggestive of mediastinal masses. All patients underwent neck exploration and TCT.
Table 1.
Patient Characteristics (n=66)
| Demographics | ||
|---|---|---|
| n | % | |
| Males | 31 | 47 |
| Females | 35 | 53 |
| Mean age at operation (yrs) ± SEM | 33.5 ± 1.6 | |
| Range of age at operation (yrs) | 12.8 – 62 | |
| MEN1 Status | n | % |
| Part of a known kindred | 53 | 80 |
| Mutation identified in patient or family member | 53 | 80 |
| Other Lesion (all) | 49 | 74 |
| Pituitary | 33 | 50 |
| Pancreatic | 24 | 36 |
| Part of known Kindred Only | 18 | 27 |
| Other Lesion Only | 13 | 20 |
| Known Kindred and Other Lesion | 35 | 53 |
| Presentation | n | % |
| Asymptomatic Patients | 6 | 9 |
| Patients with ≥1 sign or symptom | 60 | 91 |
| Symptoms | ||
| Total patients with ≥1 symptom(s) | 32 | 48 |
| Bone Pain | 12 | 18 |
| Fatigue | 12 | 18 |
| Anxiety or Depression | 7 | 11 |
| Abdominal Pain* | 7 | 11 |
| Constipation | 4 | 6 |
| Nausea/vomiting | 1 | 1.5 |
| Signs | ||
| Total patients with ≥1 Sign(s) | 54 | 82 |
| Osteopenia and/or Osteoporosis | 37 | 56 |
| Nephrolithiasis | 29 | 44 |
| Hypertension | 2 | 3 |
| Nephrocalcinosis | 1 | 1.5 |
| Renal Insufficiency | 1 | 1.5 |
| Arrythmia | 1 | 1.5 |
| Mean number of signs and symptoms ± SEM | 3.8 ± 1.9 | |
| Range of number of signs and symptoms | 0 – 5 | |
Of the 7 patients with abdominal pain, only 1 patient did not have concomitant Zollinger-Ellison Syndrome or Peptic Ulcer Disease
Number of Parathyroid Tumors
In 40 cases, four glands were found and a 3.5 gland resection was performed. In 18 cases, three glands were found and a 2.5 gland resection was performed; in 4 cases, three glands were found and all were resected. In four cases, two or fewer glands were found and all of these glands were resected.
Patients in whom the surgeon identified all four glands in the neck exploration prior to beginning TCT are shown on the left of Figure 1. This group included three patients in whom a lesion was identified in cervical thymic tissue during neck exploration before beginning the transcervical thymectomy. Of the 34 patients in this group, additional parathyroid tissue was found in only two permanent thymic specimens (2/34, 6%). Pathology described the tissue within the thymectomy specimen as a full gland in one patient and clusters of thyroid and parathyroid tissue in the second patient.
Figure 1.
Analysis of Patients by Number of Glands Found in Neck Exploration. PT = parathyroid
Of the 32 patients in the group in which less than four entopic parathyroid glands were found during the neck exploration, additional parathyroid tissue was found by the surgeon or the pathologist in the thymic specimen in 17 patients (17/32, 53%). A lesion was identified in cervical thymic tissue during neck exploration before beginning the transcervical thymectomy in one patient in this group. Pathology reported the tissue within the thymectomy specimens as hypercellular parathyroid tissue in seven patients, full glands in nine patients, and parathyroid tissue in one patient. Following thymectomy, four glands were accounted for in eight of these 32 patients.
Overall, thymic parathyroid tissue was found in two of the 34 patients (6%) in whom four entopic glands were identified during neck exploration and 17 of the 32 (53%) patients in whom four glands were not (p<0.0001 by Chi-square test). No carcinoid tissue was seen in any specimen. Demographic characteristics, MEN status, signs and symptoms at presentation, and serum calcium and parathormone values were compared between these two groups; no characteristic was found to be significantly different (Table 2).
Table 2.
Comparison Among Patients Based on Glands Found During Neck Exploration and Before Thymectomy
| Four Glands Found n=34 | <4 Glands Found n=32 | p | |
|---|---|---|---|
| Sex | |||
| Male | 12 | 19 | 0.05 |
| Female | 22 | 33 | |
| Age at operation (yrs) | 35.3±2.3 | 31.4±2.1 | 0.19 |
| MEN1 definition | |||
| Part of Kindred Alone | 9 | 9 | 0.88 |
| Other MEN1 Lesion Alone | 7 | 6 | 0.85 |
| Kindred and Other MEN1 Lesion | 18 | 17 | 0.98 |
| Kindred vs. Lesion vs. Both | 1.00 | ||
| Symptoms | |||
| Bone Pain | 6 | 6 | 0.86 |
| Fatigue | 5 | 7 | 0.45 |
| Anxiety or Depression | 3 | 4 | 0.63 |
| Constipation | 3 | 1 | 0.61 |
| Number of symptoms | 0.65±0.1 | 0.66±0.2 | 1.00 |
| Signs | |||
| Nephrolithiasis | 13 | 16 | 0.34 |
| Osteopenia | 13 | 12 | 0.95 |
| Osteoporosis | 7 | 5 | 0.6 |
| Number of signs | 1.3±0.2 | 1.2±0.1 | 0.76 |
| Symptoms and Signs | 1.9±0.2 | 1.9±0.2 | 0.83 |
| Pre-Operative | |||
| Serum Calcium (mmol/L) | 2.68±0.02 | 2.67±0.03 | 0.94 |
| Venous Ionized Calcium (mmol/L) | 1.53±0.02 | 1.54±0.02 | 0.52 |
| Intra-operative | |||
| % change Intact Parathormone (pg/mL) | −85±3 | −86±3 | 0.67 |
Post-operative Status
The mean percent of the maximum changes in serum calcium, venous ionized calcium, and intact parathormone values after operation were −18.4% ± 0.99 (n=61), −20.4% ± 1.1 (n=64), and −84.6% ± 2.3 (n=52). Serum calcium values were normal or low post-operatively in all patients except for two patients who had persistent hyperaparathyroidism. All four glands were not found in either patient at the end of neck exploration and TCT. Six patients had postoperative complications (9%). There were five cases of infection requiring antibiotics (sinus infection, two urinary tract infections, otitis media, and leg cellulitis). The patient with leg cellulitis also developed transient rhabdomyolosis which resolved with hydration. There was one case of post-operative seizure which was associated with transient elevation of creatine kinase.
Transient post-operative hypocalcemia was seen in most patients.. The mean post-operative serum calcium (normal range: 2.05–2.50 mmol/L) and venous ionized calcium (normal range: 1.12–1.32 mmol/L) nadirs were 1.90 ± 0.02 mmol/L (n=51) and 1.07 ± 0.01 mmol/L (n=53) respectively. 43 patients (65%) were discharged home with oral calcium supplements.
Follow-up data were available for 59 patients (89%) and are presented in Table 3. The mean follow-up time was 6.4 ± 0.5 yrs, range 0.42 – 14 years. Sixteen of these patients had recurrent primary HPT. Eight recurrences occurred in patients who had four glands seen at the conclusion of neck exploration; the mean time to recurrence in these patients was 2.4±0.4 years. Four of these patients were re-explored at the NIH; three were found to have hyperplasia of the remnant gland and one patient was found to have a fifth gland. Eight recurrences occurred in those who had less than four glands seen at the conclusion of neck exploration; the mean time to recurrence in these patients was 3.8±0.8. Two of these eight patients had four glands found after thymectomy. Two of these patients were re-explored at the NIH and both were found to have hyperplasia of the remnant gland.
Table 3.
Follow-Up Data*
| Incidence of | Four Glands Found | <4 Glands Found |
|---|---|---|
| Supernumary Glands | 0/34 (0%) | 1/32 (3%) |
| Persistent Disease | 0/34 (0%) | 2/32 (6%) |
| Recurrence (Hypercalcemia) | 8/31 (26%) | 8/28 (29%) |
| Persistent Hypocalcemia | 10/31 (32%) | 5/28 (18%) |
| Autografts performed+ | 3 | 3 |
| Success | 1 | 1 |
| Partial Success | 1 | 1 |
| Failure | 1 | 1 |
59 patients had follow-up; 31 patients in the four glands found group and 28 in the <4 glands found group.
Success defined as normocalcemia without supplementation; partial success defined as normocalcemia with Calcium supplementation only, failure as requiring both Calcium and Vitamin D supplementation.18
One patient was re-explored for persistent disease and was found to have an undescended gland.
Fifteen of the 59 patients had persistent hypocalcemia despite oral supplementation (25%). Five of these patients had less than four glands seen during neck exploration. Mean serum calcium, venous ionized calcium, and intact parathormone values at the last recorded visit or prior to autograft for these patients were 2.19 ± 0.04 mmol/L (n=10), 1.18 ± 0.03 mmol/L (n=7), and 31.3 ± 7.5 pg/mL (n=9) respectively. Six cryopreserved parathyroid autografts were performed for hypocalcemic symptoms in these patients using our previously described techniques.18
There were no other long-term complications and no cases of thymic carcinoid.
DISCUSSION
Prophylactic thymectomy
Current initial operations for primary HPT in MEN1 patients include either subtotal parathyroidectomy (in which 3.5 glands or less are removed) or total parathyroidectomy (in which 4 or more glands are removed) with autotransplantation.7 Subtotal resections have been associated with higher recurrence rates than complete resections with autotransplantation, however, sub-total resections have a lower incidence of prolonged post-operative hypocalcemia. Among 92 MEN1 patients seen at the NIH, subtotal resection resulted in 33% (19/58) recurrence with median follow-up of 5.7 years, while total resection resulted in 23% (3/13) recurrence with median follow-up of 10.9 years.7
TCT is commonly performed with parathyroid resection in MEN1 patients.7,15 A review of 503 unselected autopsy cases found 24 (5%) with at least five parathyroid glands in separate locations. The most common location for the fifth gland was in or near the thymus. Twenty-six percent of the inferior glands were also found in or near the thymus, but only 2.2% of glands were found in the mediastinal thymus or the anterior mediastinum. Of note, true intrathyroidal glands were found only in three cases (0.2%) [11]. Thymic carcinoid tumors have been described in several series of MEN1 patients.12–14 Besides these reports, the data regarding the utility of TCT to remove additional parathyroid tissue or carcinoid tumors during parathyroid resection in MEN1 patients are limited. TCT adds time to the operation and increases the possibility of injury to adjacent structures (nerves and vessels) and also does not clear all of the mediastinal thymic tissue.
In the prior NIH study of initial operation for 92 MEN1 patients, TCT was performed in 86% of cases but data are not reported regarding pathology analysis of thymic specimens.7 In another series of 50 MEN1 patients from Sweden, thymectomy data are reported for 15 patients who underwent total parathyroidectomy with TCT at reoperation for recurrence. A fifth parathyroid gland was found in six of 15 thymus specimens (40%).5 A third series of 37 MEN1 patients from The University of Texas MD Anderson Cancer Center undergoing both initial and re-operation reported the thymus to be the location for additional glands in six of eight patients (75%) with ectopic glands. Twenty TCTs were performed and six specimens contained parathyroid tissue (30%).8
Finally, a series of 256 MEN1 cases collected from the GENEM registry in France and Belgium reviewed trends in operative strategy for HPT. TCT was performed with parathyroid resection in 32% of operations before 1986, 54% between 1986 and 1990, and 62% after 1990. Univariate analysis of factors associated with post-operative normocalcemia found less than subtotal parathyroidectomy vs. subtotal (54 % cure vs. 93%, p=0.0001), and no thymectomy vs thymectomy (58% cure vs. 84%, p=0.0001) to be significant. However, on multivariate analysis only the extent of resection remained significant.10
Thymic carcinoid in MEN1
Approximately 100 cases of thymic carcinoids in the setting of MEN1 series have been reported.12,13,17 In a prospective study of 85 MEN1 patients at the NIH, investigators found seven patients (8%) with thymic carcinoid. All patients were male and four were smokers. One patient underwent TCT with parathyroidectomy prior to development of thymic carcinoid, four patients did not, and this information was unknown for two patients. The mean time of onset of thymic carcinoid was 19 years after MEN1 diagnosis and 16 years after presentation with hyperparathyroidism.12 In two retrospective studies of seven patients each with MEN1 and thymic carcinoid, all patients in both studies were male and most were smokers. Data regarding previous neck operations are not available in these studies.13,14
Thymic carcinoid has been reported to occur despite previous TCT. This occurred in one patient in the prior NIH study.12 Occurrence was also described in an MEN1 patient who presented with left shoulder pain and a large intrathoracic mass on CT nine months after parathyroid resection and TCT.19 The natural history of thymic carcinoid is not well described, but it is thought to demonstrate aggressive growth.12,13,17
From these data, the yield of supernumerary or ectopic parathyroid glands for all MEN1 patients undergoing TCT is unclear, and no recent study has commented on the presence of carcinoid tumors within thymic specimens. Additionally, data from cadaveric review of sporadic patients revealed that 26% of missing inferior glands were found in or associated with the thymus, but that only 24 cases (5%) had more than 4 glands.11 Cadaveric data are not available for MEN1 patients alone and it is unknown how many, if any, of the patients in this series were MEN1. However, these data raise the question of the utility of routine TCT when all four glands are identified during neck exploration.
In our study, persistent hyperparathyroidism following resection occurred in two of the 66 patients (3%) and recurrent hyperparathyroidism was seen in 16 of the 59 patients (27%). These rates are within the range of other published series.7–10 All 66 patients in our study underwent TCT. No carcinoid tissue was found in any of the 66 thymectomy specimens. There was low yield of parathyroid tissue within the permanent thymectomy specimens in patients when four entopic glands were identified (2/34, 6%) during neck exploration, whereas the yield was much higher in patients when less than four glands were identified during exploration (17/32, 53%), p<0.0001. Pre-operative data and the results of the intra-operative parathormone assay were not found to be statistically different between the groups.
These data suggest that the results of the neck exploration should guide the decision to undertake TCT. If four glands are found during the neck exploration, the risks of a TCT appear to outweigh any benefit. In contrast, if four glands are not found during the neck exploration, there is a much higher probability that the thymus will contain ectopic parathyroid tissue and TCT remains indicated. In light of these data, we recommend reserving TCT in MEN1 patients for those patients in which four glands are not found during the neck exploration.
Acknowledgments
This was supported by the intramural NIH programs of NCI and NIDDK.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chandrasekharappa SC, Guru SC, Manickam P, Olufemi SE, Collins FS, Emmert-Buck MR, et al. Positional Cloning of the gene for multiple endocrine neoplasia – type 1. Science. 1997;276:404–408. doi: 10.1126/science.276.5311.404. [DOI] [PubMed] [Google Scholar]
- 2.Brandi ML, Gagel RF, Angeli A, Bilezikian JP, Beck-Peccoz P, Bordi C, et al. Guidelines for Diagnosis and Therapy of MEN Type 1 and Type 2. J Clin Endocrinol Met. 2001;86(12):5658–5671. doi: 10.1210/jcem.86.12.8070. [DOI] [PubMed] [Google Scholar]
- 3.Rizzoli R, Green J, Marx SJ. Primary Hyperparathyroidism in Familial Multiple Endocrine Neoplasia Type I. Am J Med. 1985;78:467–474. doi: 10.1016/0002-9343(85)90340-7. [DOI] [PubMed] [Google Scholar]
- 4.Niederle B, Roka R, Brennan MF. The transplantation of parathyroid tissue in man: development, indications, technique and results. Endocr Rev. 1982;3:245–279. doi: 10.1210/edrv-3-3-245. [DOI] [PubMed] [Google Scholar]
- 5.Hellman P, Skogseid B, Oberg K, Juhlin C, Akerstom G, Rastad J, et al. Primary and reoperative parathyroid operations in hyperparathyroidism of multiple endocrine neoplasia type 1. Surgery. 1998;124:993–999. [PubMed] [Google Scholar]
- 6.Burgess JR, David R, Parameswaran V, Greenaway TM, Shepherd JJ. The outcome of subtotal parathyroidectomy for the treatment of hyperparathyroidism in multiple endocrine neoplasia type 1. Arch Surg. 1998;133(2):126–129. doi: 10.1001/archsurg.133.2.126. [DOI] [PubMed] [Google Scholar]
- 7.Elaraj DM, Skarulis MC, Libutti SK, Norton JA, Bartlett DL, Pingpank JF, et al. Results of initial operation for hyperparathyroidism in patients with multiple endocrine neoplasia Type 1. Surgery. 2003;134(6):858–864. doi: 10.1016/s0039-6060(03)00406-9. [DOI] [PubMed] [Google Scholar]
- 8.Lambert LA, Shapiro SE, Lee JE, Perrier ND, Truong M, Wallace MJ, et al. Surgical treatment of hyperparathyroidism in patients with multiple endocrine neoplasia Type 1. Arch Surg. 2005;140(4):374–382. doi: 10.1001/archsurg.140.4.374. [DOI] [PubMed] [Google Scholar]
- 9.Thompson NW. The surgical management of hyperparathyroidism and endocrine disease of the pancreas in the multiple endocrine neoplasia type 1 patient. J Int Med. 1995;238:269–280. doi: 10.1111/j.1365-2796.1995.tb00934.x. [DOI] [PubMed] [Google Scholar]
- 10.Goudet P, Cougard P, Verges B, Murat A, Carnaille B, Calender A, et al. Hyperparathyroidism in Multiple Endocrine Neoplasia Type I. World J Surg. 2001;25:886–890. doi: 10.1007/s00268-001-0046-z. [DOI] [PubMed] [Google Scholar]
- 11.Akerstrom G, Malmaeus J, Bergstrom R. Surgical anatomy of human parathyroid glands. Surgery. 1984;95(1):14–21. [PubMed] [Google Scholar]
- 12.Gibril F, Chen Y-J, Schrump DS, Vortmeyer A, Zhuang Z, Lubensky IA, et al. Prospective study of thymic carcinoids in patients with multiple endocrine neoplasia type I. J Clin Endocrinol Met. 2003;88(3):1066–1081. doi: 10.1210/jc.2002-021314. [DOI] [PubMed] [Google Scholar]
- 13.Ferolla P, Falchetti A, Filosso P, Tomassetti P, Tamburrano G, Avenia N, et al. Thymic neuroendocrine carcinoma (carcinoid) in multiple endocrine neoplasia type I: The italian series. J Clin Endocrinol Met. 2005;90(5):2603–2609. doi: 10.1210/jc.2004-1155. [DOI] [PubMed] [Google Scholar]
- 14.Kivlen MH, Bartlett DL, Libutti SK, Skarulis MC, Marx SJ, Simonds WF, et al. Reoperation for hyperparathyroidism in multiple endocrine Neoplasia type 1. Surgery. 2001;130(6):991–998. doi: 10.1067/msy.2001.118379. [DOI] [PubMed] [Google Scholar]
- 15.Agresti A. Categorical Data Analysis. New York: John Wiley and Sons, Inc; 1990. pp. 79–129. [Google Scholar]
- 16.Mehta CR, Patel NR. A network algorithm for performing Fisher’s exact test in r x c contingency tables. J Am Stat Assoc. 1983;78:427–434. [Google Scholar]
- 17.Teh BT, Zedenius J, Kytola S, Skogseid B, Trotter J, Choplin H, et al. Thymic carcinoids in multiple endocrine neoplasia type I. Ann Surg. 1998;228(1):99–105. doi: 10.1097/00000658-199807000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldman AL, Sharaf RN, Skarulis MC, Bartlett DL, Libutti SK, Weinstein LS, et al. Results of heterotopic parathyroid autotransplantation: a 13 year experience. Surgery. 1999;126(6):1042–1048. doi: 10.1067/msy.2099.101580. [DOI] [PubMed] [Google Scholar]
- 19.Burgess JR, Giles N, Shepherd JJ. Malignant thymic carcinoid is not prevented by transcervical thymectomy in multiple endocrine neoplasia type I. Clin Endocrinol. 2001;55:689–693. doi: 10.1046/j.1365-2265.2001.01348.x. [DOI] [PubMed] [Google Scholar]