Abstract
Background and Purpose:
Insomnia is a highly prevalent problem that is associated with increased use of health care services and products, as well as functional impairments. This study estimated from a societal perspective the direct and indirect costs of insomnia.
Participants and Methods:
A randomly selected sample of 948 adults (mean age = 43.7 years old; 60% female) from the province of Québec, Canada completed questionnaires on sleep, health, use of health-care services and products, accidents, work absences, and reduced productivity. Data were also obtained from the Quebec government administered health insurance board regarding consultations and hospitalizations. Participants were categorized as having insomnia syndrome, insomnia symptoms or as being good sleepers using a standard algorithm. Frequencies of target cost variables were obtained and multiplied by unit costs to generate estimates of total costs for the adult population of the province of Quebec.
Results:
The total annual cost of insomnia in the province of Quebec was estimated at $6.6 billion (Cdn$). This includes direct costs associated with insomnia-motivated health-care consultations ($191.2 million) and transportation for these consultations ($36.6 million), prescription medications ($16.5 million), over the-counter products ($1.8 million) and alcohol used as a sleep aid ($339.8 million). Annual indirect costs associated with insomnia-related absenteeism were estimated at $970.6 million, with insomnia-related productivity losses estimated at $5.0 billion. The average annual per-person costs (direct and indirect combined) were $5,010 for individuals with insomnia syndrome, $1,431 for individuals presenting with symptoms, and $421 for good sleepers.
Conclusions:
This study suggests that the economic burden of insomnia is very high, with the largest proportion of all expenses (76%) attributable to insomnia-related work absences and reduced productivity. As the economic burden of untreated insomnia is much higher than that of treating insomnia, future clinical trials should evaluate the cost-benefits, cost-utility, and cost-effectiveness of insomnia therapies.
Citation:
Daley M; Morin CM; LeBlanc M; Grégoire JP; Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. SLEEP 2009;32(1):55-64.
Keywords: Insomnia, epidemiology, health economics
INSOMNIA IS A PREVALENT PUBLIC HEALTH PROBLEM, WITH BETWEEN 6% AND 10% OF THE POPULATION MEETING DIAGNOSTIC CRITERIA FOR INSOMNIA syndrome1–3 and about a third of the population experiencing insomnia symptoms at any given moment.2 Despite its high prevalence, there is little information on the economic burden of insomnia. Information on the costs of illnesses, an indicator of their burden to society, is increasingly driving policy decisions about the funding and development of health care and research programs and priorities. Insurance companies are also concerned with the costs of illnesses and the impact that interventions may have in reducing symptoms and health care system utilization.
Economic evaluations of the cost of illnesses or the cost effectiveness of treatments consider 2 broad categories of costs. These include direct costs associated with the consumption of resources (e.g., consultations, products, and testing), and indirect costs associated with the loss of resources (e.g., absenteeism, reduced productivity).4 While studies show a relationship between insomnia severity and the use of health-care service and product utilization,5–9 quantification of the associated costs is scarce. Similarly, some studies have reported a relationship between insomnia, increased absenteeism, and decreased productivity,10–13 yet the economic burden of this has been less frequently measured.
The National Commission on Sleep Disorders Research estimated the direct costs of insomnia in the United States at $13.9 billion for the year 1995,14 whereas Leger et al.15 estimated the total cost of insomnia in France at about 10 million francs (or $2 billion US). The indirect costs associated with insomnia have received less attention in the literature, primarily because these costs are more difficult to estimate and quantify, there is no single database from which to draw, and measurement of these variables is more subject to interpretation and memory bias. Stoller16 attempted to quantify work-related deficits by combining data obtained in a study of workplace performance in Navy servicemen17 with her own insomnia prevalence estimate of 33% and a performance decrement estimate of 4%. The monetary value of absenteeism and lost productivity was estimated at $41.1 billion annually (1995 US$). A per person estimate was attempted by Chilcott and Shapiro,5 who suggest a decrease in work productivity due to insomnia of 10%. This amounts to $3,000 per insomnia sufferer per year. Stoller16 also looked at a number of other indirect costs, including insomnia-related accidents, alcoholism, and depression, estimating their costs at between $77.05 and $92.13 billion. Although these estimates have been criticized because they are based on liberal prevalence rates and relied on some questionable assumptions,9 they are still frequently used to describe the indirect economic consequences of insomnia.
A French study18 concluded that insomnia is associated with increased absenteeism and reduced productivity, with associated costs about twice as high for insomnia patients as for good sleepers. The methods of costing did not allow, however, for an analysis of the proportional contribution of insomnia. There was also a methodological problem associated with double-counting costs that may have inflated cost estimates. Using existing data banks, Hillman et al.19 estimated the financial costs of all sleep disorders combined (e.g., insomnia, sleep apnea, periodic limb movements) for Australia at about $1,524 million, or 0.8% of the Australian gross domestic product. While an innovative approach was used to estimate fractions of other health impacts attributable to sleep disorders, this study did not permit the identification of costs associated with individual sleep disorders.
A recent study by Ozminkowski et al.20 used medical claims data for health-care services, and absenteeism and short-term disability records to assess costs of insomnia occurring in adults in the US. After matching adult (aged 18–64) subsamples on variables determined by propensity score analysis, indirect costs combined were $1,253 higher in individuals with insomnia as compared to those without insomnia. The matching procedure and use of objective data lend strength to this study. However, costs related to reduced productivity, transportation, use of alcohol, and use of over-the-counter products were excluded from the analysis, suggesting that the results may underestimate the real cost of insomnia.
Despite recent progress in documenting the economic burden of insomnia, some methodological weaknesses limit the current state of knowledge on this topic. The use of large administrative databases precludes analysis of potential confounding variables such as the reasons for consultations, use of OTC products, actual consumption of prescribed medications and, for some medications, the target ailment for which it was prescribed. When workplace records are used to obtain absenteeism data, reasons for absences are rarely provided and productivity data are not available. Similarly, the use of official accident records precludes identification of the contributing role of insomnia to these events. Studies typically use 2 groups—individuals with and without insomnia; the inclusion of an intermediate category would allow analysis of a linear relationship between costs and insomnia severity.
The purpose of this study was to estimate, from the societal perspective, direct and indirect costs of insomnia. Costs were compared across three groups of participants classified as being good sleepers, having insomnia symptoms or having insomnia syndrome. The proportional contribution of insomnia to overall consultation costs and three indirect dependent cost variables, absenteeism, productivity and accidents, was also calculated.
METHOD
Participants
This research was part of a larger epidemiological study documenting the natural history of insomnia. It was approved by Laval University's research ethics committee. Participants were randomly selected from the province of Quebec for an initial telephone sleep survey. They were chosen using a stratified probabilistic selection procedure, based on the last Canadian census, combined with a random digit selection method and the Kish method to identify which household member was interviewed.21 The only inclusion criteria for the telephone interview were to be over 18 years of age and to speak French (for more information, see Morin et al.2). Of 2001 respondents who completed the initial survey, 1467 accepted to continue with a longitudinal extension of the study (73% participation rate), which entailed completing questionnaires sent out by mail. In order to obtain as representative a sample of the population as possible, only people having previously received a diagnosis for a sleep disorder other than insomnia (7.2%) were excluded from the next phase, leaving a potential sample of 1,362. Of the 1,362 questionnaires sent out, 997 (73%) were returned, and 44 additional respondents were excluded due to sleep disorders other than insomnia that were not reported at the initial interview. Five participants could not be classified in any of the 3 groups because of missing data. The final sample consisted of 948 participants. Participants were paid $25.00 Cdn for completing the questionnaires.
Procedure
Sleep status groups.
Participants were classified in 3 groups based on an algorithm derived from a combination of criteria from the Diagnostic and Statistical Manual of Mental Disorders,22 the International Classification of Diseases, 10th Edition,23 and the use of sleep-promoting products (prescribed and over-the-counter). Responses from the Insomnia Severity Index24 and the Pittsburgh Sleep Quality Index25 and from questions on sleep-promoting medication utilization were used to evaluate the presence or absence of each criterion.
The 3 sleep status groups were defined as follows: Insomnia syndrome (SYND). Participants in this group met all diagnostic criteria for insomnia. They were dissatisfied with their sleep (i.e., dissatisfied [3] or very dissatisfied [4] on a 0–4 scale) and presented symptoms of initial, maintenance or late insomnia ≥ 3 nights per week for a minimum duration of one month. Psychological distress or daytime impairment related to sleep difficulties was also reported by those individuals (i.e., much [3] or very much [4] on 0–4 scales). Finally, if prescribed medication was used as a sleep-promoting agent ≥ 3 nights per week, participants were automatically classified in the insomnia syndrome group whether or not they presented symptoms of initial, maintenance, or late insomnia.
Insomnia symptoms (SYMP).
Participants in this group presented symptoms of initial, maintenance or late insomnia ≥ 3 nights per week, without fulfilling all criteria of an insomnia syndrome (i.e., they could be satisfied with their sleep, not report distress or daytime consequences, or their insomnia could have been present for < one month). Also included in this group were individuals dissatisfied with their sleep quality, but without symptoms of initial, maintenance, or late insomnia. Last, participants using prescribed medication to promote sleep < 3 nights per week, or over-the-counter medication at least one night per week were automatically classified in this group.
Good sleepers (GS).
These participants were satisfied with their sleep (i.e., very satisfied [0], satisfied [1], or neutral [2] on a 0–4 scale), did not report insomnia symptoms, and did not use sleep-promoting medication.
Of the 948 participants, 493 (51.7%) were classified as good sleepers, 308 (32.3%) as having insomnia symptoms, and 147 (15.4%) as having an insomnia syndrome. Of the last group, 20 individuals did not fulfill all of the insomnia diagnostic criteria but used prescribed sleep medication ≥ 3 nights per week.
Assessment and Measures
Of the questionnaires used in the larger study, only those directly relevant to the present paper are described here. The first 2 are questionnaires used to classify participants in one of the 3 groups.
The Insomnia Severity Index24 is a 7-item questionnaire used to provide a subjective index of sleep impairment probing severity of sleep onset, sleep maintenance, and early awakening problems; satisfaction with the current sleep pattern; perceived interference of sleeping difficulties with daily functioning; noticeability of impairment attributed to the sleep problem; and degree of distress caused by the sleep problem. Items are evaluated according to a 5-point Likert scale (0 = not at all, 4 = extremely) with total scores ranging from 0 to 28. This tool has been shown to have adequate psychometric properties.26
The Pittsburgh Sleep Quality Index25 is a 19-item questionnaire that assesses sleep quality and disturbances over a one-month interval. Four open-ended questions are followed by closed questions that are rated on a 4-point Likert scale. Seven component scores are derived (e.g., subjective sleep quality, duration, efficiency) and the total score (range from 0 to 21) is obtained by adding up the 7 component scores. The PSQI has been shown to have a diagnostic sensitivity of 89.6% and a specificity of 86.5% for diagnosing primary insomnia.
Health Care Service Use and Insomnia Impact Questionnaire.
A questionnaire was developed to obtain information on costs associated with health-care service and product utilization, use of alcohol as a sleep aid, hospitalizations, productivity, absenteeism, and accidents. Although this instrument has not been formally validated, key questions are similar to those used in the NIMH Epidemiological Catchment Area Survey1 and other research.8 Participants were asked to report on the past 3-month frequency of consultations with all types of health-care practitioners as well as on whether insomnia was a reason for consulting (main reason, secondary reason, not a reason). Only a fraction of costs associated with visits where insomnia was not the main consultation motive was considered in the cost-of-illness calculations. In the absence of formal guidelines, and to remain conservative, a fraction of 0.20 was chosen as an estimate of the proportion of the time (and cost) involved in discussing insomnia in the context of a consultation for another health problem. The total cost of these consultations was therefore multiplied by 0.2 to estimate their cost.
Participants were asked to provide detailed information on the number and types of all products consumed (prescription, over-the-counter, herbal/natural, alcohol) in the previous 3 months, the dosage (where appropriate), the frequency in the last 3 months, and the health problem for which the product was used. Information was also requested regarding hospitalizations occurring in the previous 6 months (number, reason, duration, diagnoses, interventions). Prescription medication names provided by participants were coded according to the 23 major categories identified in the American Hospital Formulary Service27 and, where necessary, using the self-report specification regarding the particular ailment being treated. Over-the-counter medications were coded according to categories identified by the Nonprescription Drug Manufacturers Association of Canada28 as being the most frequently used products. Self-reported health problems were coded using the 18 major diagnostic categories of the ICD-9 and used by the Régie de l'assurance maladie de Québec (RAMQ).
Participants were asked to report on the number of hours absent from work in the past 3 months and to indicate whether they had experienced reduced productivity (remunerated work or other activities) during the same period and if so, for a total of how many hours. Rather than rely on a dichotomous response that could inflate productivity loss estimates, we tried to provide nuanced information by asking participants to estimate by what proportion they thought their productivity had diminished (e.g., 10%, 50%, 90%). For questions related to absences and productivity, participants reported on the cause that was perceived to have most strongly motivated these events (e.g., illness, fatigue, stress, insomnia), along with the perceived strength of the link with insomnia and its consequences (such as fatigue, reduced concentration). This was evaluated using a scale of 0 to 10, which was later used as a multiplier for calculating insomnia-related costs.
Motor vehicle and other accidents (e.g., work-related, falls) that occurred in the past 6 months were also reported, along with a subjective assessment of the link between insomnia or its consequences (such as fatigue, reduced concentration) and the event.
Except for hospitalizations and accidents, for which a longer recall period of 6 months was used, the recall period was the 3 months prior to questionnaire completion. These recall periods were chosen to minimize recall bias and maximize accuracy when extrapolating one-year estimates (see Drummond et al.29 for a discussion of optimal reference periods).
Régie de l'assurance maladie du Québec and MedEcho.
Data were obtained from 2 provincial government health care databases. The RAMQ is the Quebec government-administered provider of health-care services. All residents receive coverage for visits to certain health-care professionals (i.e., primary care physicians, medical specialists), with some individuals receiving additional assistance if they meet certain conditions (e.g., invalidity, economic hardship, senior citizens). This database provided information as to RAMQ-covered consultations for the study participants (type of professional consulted, diagnosis received). A separate database (MedEcho) maintained by the Ministry of Health and Social Services provided hospitalization data (date, length of stay, principal and secondary diagnoses).
Cost measures and calculations.
The procedures for the costing process were based on guidelines from the Canadian Coordinating Office for Health Technology Assessment. Consultation unit costs for survey data were calculated by taking the average cost in 2002 of a consultation with each type of health-care professional and multiplying it by the frequency of visits to that same professional. Unit costs were obtained either from professional associations (modal charge) or by calling a sample of 5 service providers (e.g., acupuncture) and calculating the mean. Costs associated with consultations with general practitioners and specialists were provided directly by the RAMQ.
Transportation costs were calculated according to distance estimates provided by participants for each consultation. The standard cost for running a mid-sized vehicle in 2002 was $0.53 per kilometer. Public transportation costs were based on individual ticket price of $1.95 and taxi rates included a base rate of $2.50, plus the standard $1.20 per-kilometer fee.
Medication costs were obtained from a publication of IMS Health CompuScript database for 2002 that identifies the unit costs of the 1,000 most frequently used prescription and OTC products and their variants in Canada. These costs include mark-up and pharmacists' fees. Products reported by participants that were not identified on the list were costed in one of 3 ways: first, we used a price catalogue (2002) published annually by the RAMQ that is used for their reimbursements and to which was added to unit costs the minimum pharmacist's fee; second, a wholesaler's pharmaceutical catalogue for the year 2002 was used to find list costs. To this was added the pharmacist's minimal fee and an average mark-up for the province of Quebec provided in the RAMQ cost catalogue. Alternatively, we obtained shelf prices directly from a sample of pharmacies, averaging across them to obtain a mean. In every case of doubt (e.g., the dosage or variant of a prescription medication was not indicated by the participant), the lowest identifiable price was chosen in order to produce the most conservative estimate possible.
Unit costs for alcohol were provided by the Société des alcools du Québec and were based on means of sales of various types of alcohol in the province in 2002. A distinction was made between beer, wine, hard liquor and “cooler” type beverages with unit prices as follows: $2.27, $3.10, $1.50, and $2.79, respectively.
The human capital approach, an accepted labor costing technique, was used to calculate the cost of absenteeism and lost productivity (see Drummond – McGuire,4 for further discussion). More precisely, time was valued using Statistics Canada Labour Force Survey data for 2002 on mean salaries according to age group and gender. Final calculations were weighted to take into consideration work force participation rates reported by the Labour Force Survey (also stratified by age and gender). As the time period for this study did not exceed one year, no adjustments for inflation or other factors were necessary.
In order to estimate the cost of absences, total hours reported absent in the 3-month reference period were multiplied by the age- and gender-appropriate hourly wage. To estimate costs associated with lost productivity, the reported hours of reduced productivity were multiplied by the reported estimate of the percentage drop in productivity indicated by the participants (e.g., 8 hours at 50% reduced productivity = 8 × 0.5 = 4 hours). The resulting numbers were totalled across the various reduced productivity periods for each person, and then multiplied by the age- and gender-appropriate hourly wage. A further distinction was made between total costs and costs attributable to insomnia. For each reported absence or period of lost productivity, participants indicated on a scale of 0 to 10 the extent to which they felt insomnia and/or its consequences had been responsible for their absence or reduced productivity. The proportional contribution of insomnia in monetary terms to absenteeism and productivity loss was estimated by multiplying total costs by the percentage indicated by participants on the scale. Participants had the option to report on productivity issues both at work and in other situations (e.g., household chores). A daily task approach is more inclusive and allows reports by homemakers, unemployed, and retired participants to be included.4
Annual insomnia-related consultation costs for the province of Quebec were estimated via extrapolation by multiplying per person costs determined for each sleep status category by the number of adults estimated to be in each of these categories in the province. Prevalence rates used were those obtained in the initial epidemiological mother study based on survey data (see Morin et al.2): 9.5% for insomnia syndrome, 29.9% for insomnia symptoms, and 60.6% for good sleepers. The estimated number of adults 18 years or older living in Quebec at the time of the study was 5,679,702 (Statistics Canada, 2002). It is therefore estimated that 3,441,899 (60.6%) of those individuals are good sleepers, that 1,698,230 (29.9%) have some insomnia symptoms, and that 539,571 (9.5%) meet criteria for an insomnia syndrome.
Statistical Analyses
To estimate costs, the dependent variables were costs accrued due to: (a) insomnia-related consultations (with insomnia as both a primary and a secondary motive); (b) transportation to and from these same consultations; (c) prescription medications, OTC products and alcohol consumed as a sleep aid; (d) insomnia-related hospitalizations and accidents; and (e) insomnia-motivated absences and reduced productivity.
One-way analysis of variance (ANOVA) was used to compare group means with Games-Howell post hoc tests used (unequal variances assumed). With a sample of 948 participants and group sizes much greater than 50, we felt justified in using analysis of variance techniques using non-log-transformed data.30
RESULTS
Sociodemographic and Clinical Characteristics of Sample
The mean age of participants was 43.7 years (SD = 14.0, range = 18–83) with no significant group differences. Females comprised 60.0% of the sample; there were significantly more women in the SYND group (70.1%) than in the SYMPT (59.1%) or GS (58%) groups, Chi square = 7.98, P < 0.05. Most participants were married (58.1%), and worked day shifts (76.4%) at full-time jobs (55.9%). A third (33.7%) had junior college or professional diplomas, while 27.3% held a university degree. No group differences were found for measures of marital status, education, income, work type, or work schedule.
Consultations
Mean 3-month costs for consultations with different health-care professionals are presented in Table 1 for the 3 subgroups. The cost of health-care visits was calculated separately for RAMQ-reimbursed and non RAMQ-reimbursed consultations because these data come from different sources. Analysis of the RAMQ database was undertaken by looking at general practitioners and psychiatrists separately, and by collapsing all specialists into one group. These data indicate that participants in the SYND group had significantly higher costs associated with visits to general practitioners, to psychiatrists, and to other specialists combined than SYND and GS groups.
Table 1.
Mean Global 3-Month Health-Care Costs (Cdn$) by Professional and Diagnostic Categories (n = 948)
| Health-care professional | Good Sleepers (n = 508) Mean (SD) | Symptoms (n = 295) Mean (SD) | Syndrome (n = 153) Mean (SD) | F | P |
|---|---|---|---|---|---|
| RAMQ-reimbursed professionals | |||||
| General practitioners | 44.86 (49.41)a | 49.08 (65.61)a | 77.85 (123.31)b | 5.92 | 0.003 |
| Psychiatrists | 0.27 (3.78)a | 1.49 (17.38)a | 10.24 (52.8)b | 6.15 | 0.002 |
| Other specialists | 47.46 (138.08)a | 54.35 (112.96)a | 87.88 (113.52)c | 4.78 | 0.002 |
| Non-RAMQ reimbursed professionals (survey) | |||||
| Overall | 94.28 (196.1)a | 108.4 (182.5)b | 228. 5 (357.6)c | 52.08 | 0.000 |
| Psychologists | 9.65 (71.32)a | 15.05 (87.38)a | 59.28 (179.49)b | 13.71 | 0.000 |
| Pharmacists | 6.09 (16.21)a | 9.04 (18.05)a | 13.26 (27.07)b | 8.41 | 0.000 |
| Physiotherapists | 13.01 (117.92) | 7.13 (55.86) | 51.37 (284.79) | 4.94 | 0.007 |
| Acupuncturists | 0.34 (7.46)a | 7.26 (59.10)b | 8.31 (45.35)b | 4.18 | 0.016 |
| Homeopaths | 0.66 (7.76) | 1.72 (12.84) | 3.27 (18.05) | 2.93 | 0.054 |
| Social Workers | 1.06 (15.53) | 1.93 (20.73) | 4.68 (23.00) | 2.05 | 0.130 |
| Massage Therapists | 8.10 (30.43) | 9.44 (58.45) | 14.24 (46.03) | 1.07 | 0.344 |
| Other | 8.10 (72.22) | 4.36 (21.76) | 1.73 (9.47) | 0.95 | 0.389 |
| Nurses | 1.35 (8.14) | 1.78 (9.25) | 2.30 (11.81) | 0.65 | 0.523 |
| Chiropractor | 6.71 (32.60) | 7.79 (42.16) | 8.35 (45.29) | 0.14 | 0.872 |
| Consultation reasons | |||||
| Insomnia | 2.52 (28.88)a | 2.54 (40.10)a | 15.45 (48.91)b | 7.49 | 0.001 |
| Insomnia secondary | 8.91 (50.11)a | 23.95 (103.70)b | 113.33 (288.95)c | 34.62 | 0.000 |
| Not insomnia | 75.47 (174.87)a | 83.97 (137.54)a | 117.57 (279.34)b | 2.84 | 0.044 |
Note. Means with different subscripts differ significantly from each other using Games Howell post hoc tests (P < 0.05). RAMQ = Réegie de l'assurance maladie du Quéebec.
Costs of all self-reported non-RAMQ consultations combined were significantly higher in the SYND group. Comparisons were also made for the 10 other health professional classes based on self-report data. Participants in the SYND groups had higher expenditures than participants in the other groups for visits to psychologists, pharmacists, physiotherapists, acupuncturists, and homeopathic specialists (Table 1).
Costs according to the three consultation motives are presented in Table 1 (insomnia as the primary reason for consulting, as a secondary motive, or not a motive). Mean per-person 3-month expenditures associated with visits for which insomnia was the primary motive were significantly higher in the SYND group than in both the SYMP and GS groups, as were the costs associated with visits where insomnia was discussed as a secondary problem, and costs of consultations unrelated to insomnia.
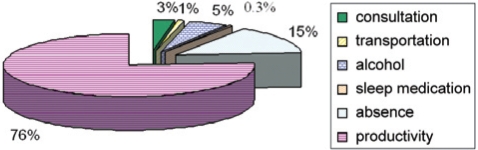
The annual cost of insomnia-related consultations was estimated at $85.3 million (see Table 2), or 32.6% of all direct costs measured and 2.9% of overall costs (Figure 1). Using the apportioning method described earlier, the estimated cost of visits to health-care professionals for which insomnia was treated as a secondary complaint was $106 million.
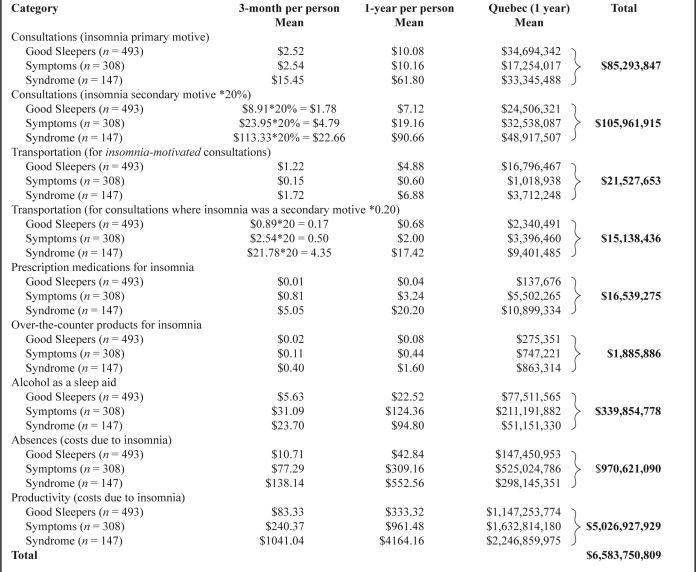
Table 2.
Three-Month and One-Year Estimates of Insomnia Costs Per Person and for Quebec per Insomnia Category (Cdn$; N = 948)
Note. Annual unit costs found in column 2 were multiplied by the estimated Quebec prevalence (adult) per category: Good Sleepers = 3,441,899; Symptoms = 1,698,230; Syndrome = 539,571. Only summary numbers in boldface (dollar figures in far right column) are included in total cost calculation.
Figure 1.
Estimated proportional contribution of direct and indirect costs to the overall economic burden of insomnia to society.
Transportation
Transportation costs related to travel to and from all health care appointments during a 3-month period were significantly higher for participants in the SYND group relative to those in the SYMP and GS groups, respectively), F(2,947) = 6.19, P < 0.002. The cost of consultations motivated solely by insomnia was $21.5 million (4.0% of all transportation costs). Costs for consultations where insomnia was a secondary motive—cost for such consultations was multiplied by 0.2—was estimated at $15.1 million (20% of the overall cost of consultations where insomnia was a secondary motive). Adding the 2, the total transportation cost associated with insomnia was estimated at $36.6 million, or 6% of all direct costs (and 0.6% of overall costs).
Medications
Prescription medications.
Table 3 presents average costs of prescription and OTC products as well as of alcohol used as a sleep aid. Participants in the SYND group spent significantly more money (out of pocket, before reimbursements) on all prescription drugs combined in the 3-month reference period, relative to both participants in the SYMP and in the GS groups, and there was no difference between the latter 2 groups.
Table 3.
ANOVA Analysis of Mean Costs Per Person of Prescription Medications, Over-the-Counter Products, and Alcohol Used as a Sleep Aid (Cdn$; N = 948)
| Category | Good Sleepers (n = 493) Mean (SD) | Symptoms (n = 308) Mean (SD) | Syndrome (n = 147) Mean (SD) | F | P |
|---|---|---|---|---|---|
| Prescription Medications ($) | |||||
| Overall | 64.69 (256.28)a | 77.14 (175.13)a | 133.61 (454.57)b | 3.43 | 0.033 |
| Insomnia | 0.01 (0.10)a | 0.81 (13.48)a | 5.05 (19.26)b | 12.07 | 0.000 |
| Mood | 2.17 (18.18)a | 3.45 (24.65)a | 11.15 (47.79)b | 6.18 | 0.002 |
| Anxiety | 2.09 (20.78)a | 2.78 (20.24)a | 11.13 (43.03)b | 7.08 | 0.001 |
| OTC products ($) | |||||
| Overall | 7.61 (31.86) | 11.54 (85.84) | 9.51 (25.88) | 3.42 | 0.620 |
| Insomnia | 0.02 (0.25)a | 0.11 (0.83)a | 0.40 (1.81)b | 10.70 | 0.000 |
| Anxiety | 0.01 (0.14)a | 0.03 (0.27)a | 0.47 (0.54)b | 5.82 | 0.003 |
| Alcohol used as a sleep aid ($) | |||||
| Overall | 5.63 (39.72) | 31.09 (76.95) | 23.70 (59.43) | 5.29 | 0.006 |
The highest per-person expenditures for prescription insomnia medication were observed in the SYND group (M = $5.05), although participants in the SYMP group also showed some expenses for insomnia medications (M = $0.81). Participants in the SYND group also spent significantly more on medications prescribed for depression and anxiety than participants in the other 2 groups. Overall, it was estimated that $16.5 million is spent annually on prescription medications for insomnia in the province of Quebec (Table 2), which represents 2.8% of all direct costs and 0.3% of overall costs. Such expenses are twice as high in the SYND as in the SYMP group.
Over-the-counter products.
No group differences were found in overall expenditures for OTC products. However, participants in the SYND group spent more on OTC products specifically for insomnia than participants in the 2 other groups. A similar pattern was identified for expenditures on OTC products for anxiety and stress. The annual estimate of expenditures for OTC products consumed for insomnia symptoms was $1.9 million, which represents less than 1% of direct and overall costs.
Alcohol
The total estimated annual cost of alcohol used for promoting sleep was $339.8 million, with $51.1 million (15%) spent by individuals with insomnia syndrome, $211.2 million (62%) by those with insomnia symptoms, and $77.5 million (23%) by good sleepers. Total expenditure on alcohol represents 60% of all direct costs and 5% of overall insomnia costs (see Figure 1). SYMP participants spent about 4 times as much on alcohol as SYND and almost 3 times as much as GS.
Hospitalizations
No hospitalizations were coded in the Med-Echo database as being due to insomnia (as indicated by the admission and hospital-stay diagnoses). Data were not obtained on possible treatments offered to participants for insomnia during hospitalizations for other ailments or interventions. Cost calculations were therefore not conducted.
Absenteeism
Because of divergent opinions regarding the optimal methodology for quantifying costs of absenteeism, data are presented in 2 ways: (a) in terms of time missed from work and (b) in terms of dollars associated with that time. Analyses of work function were conducted only for participants engaged in full- or part-time remunerated work (68.4% of sample). Table 4 shows that participants in the SYND group reported missing 19.9 hours of work over the previous 3 months, compared to 14.3 hours in the SYMP group and 5.9 hours in the GS group, F(2,933) = 3.46, P < 0.05. Participants with insomnia syndrome attributed a higher proportion of this time missed as due to their sleep difficulties (43.8%) than participants in the SYMP (22.0%) or the GS group (11.4%), F(2,141) = 10.00, P < 0.001.
Table 4.
Mean Hours Lost to Absences and Reduced Productivity: Three-Month Data and Extrapolated Annual Estimates (N = 948)
| Absenteeism |
Reduced Productivity |
|||||
|---|---|---|---|---|---|---|
| Good Sleepers (n = 493) | Symptoms (n = 308) | Syndrome (n = 147) | Good Sleepers (n = 493) | Symptoms (n = 308) | Syndrome (n = 147) | |
| 3-month | ||||||
| # of h (M; SD) | 5.94a (39.13) | 14.29b (65.62) | 19.94c (68.98) | 20.05a (96.31) | 32.66b (106.45) | 97.72c (241.87) |
| 95% CI | 2.46–9.41 | 6.19–22.38 | 9.47–26.92 | 11.47–28.62 | 20.60–44.71 | 56.23–139.20 |
| %loss due to insomnia | 11.58%a | 22.03%b | 43.75%c | 27.65%a | 37.93%b | 56.41%c |
| %h lost due to insomnia (M) | 0.69 | 3.14 | 8.72 | 5.36 | 13.18 | 54.15 |
| 1-year estimate | ||||||
| # of h (M) | 23.76 | 57.16 | 79.76 | 80.20 | 130.64 | 390.88 |
| h lost due to insomnia (M) | 2.75 | 12.59 | 34.89 | 22.17 | 49.55 | 220.49 |
| days lost due to insomnia (M) | 0.34 | 1.57 | 4.36 | 2.77 | 6.19 | 27.56 |
Note. Means with different subscripts differ significantly from each other using Games Howell post hoc tests (P < 0.05).
Total annual missed days of work are estimated at 2.97 for GS, 7.1 for people with insomnia SYMP, and 10.0 for those with insomnia SYND. Multiplying the total time absent by the percentages representing the contribution of insomnia to these absences produced an estimate of time absent due to insomnia. On an annual per person basis, good sleepers were absent 0.34 days because of insomnia, individuals with SYMP 1.57 days, and individuals with insomnia SYND 4.36 days. The latter group missed about 13 times as much work annually as good sleepers because of sleep problems.
Three-month average costs associated with absences were higher for individuals with an insomnia SYND, relative to those with SYMP and GS. After adjusting for the perceived proportional contribution of insomnia to these absences, average per-person 3-month costs were as follows: SYND = $138.14, SYMP = $77.29, and GS = $10.71. Extrapolating to the year it was estimated that $970.6 million is lost annually due to insomnia-related absences (see Table 2), with all 3 groups contributing significantly to this burden. Overall, this represents 16% of indirect costs and 14.7% of the total economic burden of insomnia to society.
Productivity
Table 4 shows that participants with insomnia syndrome reported significantly more hours (97.7) of lost productivity in the previous 3 months than participants in the SYMP group (32.7) or the GS group (20.0), F(2,921) = 18.03, P < 0.001. After adjusting for the estimated contribution of insomnia to productivity deficits, participants in the SYND group experienced 54.1 hours of insomnia-related reduced productivity in a 3-month period, compared to 13.2 hours for the SYMP group and 5.4 hours for the GS group. Extrapolating from these figures, the annual estimate of insomnia-related lost productivity was 27.6 days per year for individuals with insomnia syndrome, 6.2 days per year for those with symptoms, and 2.8 days for good sleepers. This translates into a ratio of about 10 days of reduced productivity to 1 for the SYND relative to GS group.
As with absenteeism, these hours can be expressed in terms of monetary losses. Good sleepers lost an average of $329 per 3-month period due to lost productivity, participants with insomnia symptoms lost $601, and those with an insomnia syndrome lost an average of $1,676. The 3-month per-person productivity costs obtained after adjusting for the proportional contribution of insomnia to productivity deficits were $83.33 for the GS group, $240.37 for the SYMP group, and $1,041.04 for the SYND group. The annual estimate of the indirect cost of insomnia in terms of productivity losses is thus $5.0 billion (Table 2), which represents 83.8% of direct costs or 76.2% of all insomnia costs.
Accidents
Motor vehicle accidents.
Thirty-four participants reported having experienced a motor vehicle accident in the previous 6 months. No significant group differences were detected. Of the 34 accidents, 17 insurance claims were filed and 16 received financial compensation ranging between $600 and $8,000. Eight participants (23.5%) reported that insomnia or its consequences had played a contributing role in the occurrence of the accident; there was no group difference on this variable. When asked to rate the strength of the link between insomnia and their accident (0–10 scale), all participants circled the number 5 or higher. Given the small number of accident cases and the heterogeneity of compensation amounts involved, no cost estimates were derived.
Other accidents.
Individuals in the SYND group were almost twice as likely to have experienced other types of accidents as good sleepers (OR: 2.43). Of the 75 accidents, 14 insurance claims were filed and 9 of those were awarded financial compensation. Compensation settlements ranged between $100 and $4,240. When asked whether they believed insomnia or its consequences had played a contributing role in the occurrence of the accident, 38.7% reported seeing a link. There was no group difference. When asked to rate the strength of the link between insomnia and their accident (0 to 10 scale), 79% of participants circled 5 or higher. Due to the small number of accident cases and the heterogeneity of compensation amounts involved, no cost estimates were produced.
DISCUSSION
This study indicates that the economic burden of insomnia to society is significant, with the total annual costs for this sleep disorder alone ($6.5 billion) representing about 1% (0.013) of the province of Quebec's $228.5 billion in gross domestic product for 2002. The annual per-person insomnia-related costs averaged $5,010 ($293 in direct costs and $4,717 in indirect costs) for individuals with an insomnia syndrome, $1,431 ($160 in direct costs and $1,271 in indirect costs) for those with insomnia symptoms, and even good sleepers cost an average of $422 annually ($45 in direct costs and $376 in indirect costs). Costs related to lost productivity comprised the largest proportion (76%) of all costs. The highest direct costs were for alcohol consumed as a sleep aid (58%) and consultations for insomnia (33%).
Comparisons of the present findings with results of previous studies are difficult because of different health-care systems and data collection methodologies. Nonetheless, the Ozminkowsi et al.20 study found that the combined direct and indirect costs of insomnia were $1,253 higher in individuals with insomnia relative to good sleepers. The cost difference in the present study between these 2 groups was $4,588; however, the present study included a third comparison group that also incurred significant insomnia-related costs falling between the good sleepers and insomnia syndrome groups. Furthermore, the present study included both alcohol and reduced productivity costs but these were not measured in the Ozminkowski study. Similarly, total costs for consultations constitute only 3% of all costs in the present study as compared to 18% in the Walsh and Engelhardt study.14 The difference is likely due to the higher proportions of costs attributed to decreased work function and alcohol use in the present study. In addition, direct costs for health services in Quebec represent predominantly administrative costs. Salaries and capital costs in the Quebec health care system are relatively low, given the centralization of the system. These comparisons highlight the importance of developing a standard methodology to conduct burden-of-illness research.
Prescription medication use for insomnia was reported by 3.7% of all participants and 17.8% of individuals with insomnia. The cost of these medications was estimated at $16.5 million annually, an amount representing a very small proportion of all direct costs ( < 1%). This is not surprising given that most medications prescribed for sleep in Canada (e.g., benzodiazepines, zopiclone) are generic and therefore very inexpensive. Higher rates of antidepressant and anxiolytic use were also observed in individuals with insomnia syndrome, but the proportion of those costs which may be associated with insomnia treatment were not factored into insomnia costs. This approach may have contributed to an underestimation of medication costs. Despite rates of OTC use similar to rates for prescription medication, expenditures on these products were considerably lower and represented the smallest proportion of all direct costs (0.03%). Many participants reported using products such as Tylenol, antihistamines, and herbal teas to aid sleep. The cost of these products is significantly lower than prescription medications and alcohol.
In the present study, 8% of the entire sample had used alcohol as a sleep aid, including 28% of participants with insomnia symptoms and syndrome. The reason for the higher rate of use in the SYMP group in this study is unclear. Perhaps individuals with insomnia syndrome are more likely to use prescription medications than other sleep aids due to the greater severity or chronicity of their symptoms. High comorbidity rates of alcohol abuse and mental disorders may also explain these elevated alcohol consumption rates.31
Costs associated with alcohol used as a sleep aid represent a higher proportion of overall costs in the present study (5%) than the 1% previously reported.5,14 Although these discrepancies may reflect different methodologies, alcohol use is a rather costly sleep aid that could substantially raise this expenditure. For example, an individual consuming 3 glasses of wine a week would spend about $9.30 (Cdn.), whereas someone taking a sleep medication 3 times a week would spend between $1.77 and $2.94 for zopiclone (5 mg and 7.5 mg, respectively), $1.17 and $1.35 for temazepam (15 mg and 30 mg, respectively), or under $1.00 for most dosages of lorazepam. Alcohol would thus result in expenditures between 3 and 14 times as high as the use of medication.
Expenses associated with insomnia-related absenteeism and reduced productivity ($6.0 billion) represent the largest portion of all direct and indirect costs combined, about 91%. Although Stoller's16 estimate of these indirect costs were lower (77%), probably because of the of a nonrepresentative Navy sample, both of these figures highlight the costly impact of insomnia for the individual and society, above and beyond direct health expenditures typically incurred for treating insomnia (i.e., medication and consultations). Each person with insomnia syndrome is estimated to cost society $552 a year in work-related absences and $4,154 in reduced productivity as a result of their sleep problems. This figure is close to the per-person annual lost productivity estimate of $3,000 of Chilcott and Shapiro. 5 People generally classified as good sleepers may nonetheless have episodes of poor sleep that have economic repercussions. While our figures should be considered conservative, as they have been adjusted downward to reflect the proportional role insomnia plays, they may reflect more accurately the real cost of insomnia than figures proposed elsewhere.14,16 Collectively, these findings indicate significant work-related costs associated with insomnia.
One of the limits of this study is the predominance of self-report methodology (although the RAMQ data confirmed certain self-report data). While accuracy of recall increases with shorter reference periods (e.g., one week), the benefits gained in terms of short-term accuracy are at the expense of accuracy when extrapolating to longer periods of time (e.g., one year). A 3-month reference period was adopted for most recall items to maximize the trade-off on these points.32,33 Another potential limiting factor of self-report measures is that individuals with insomnia have a tendency to overestimate sleep difficulties and daytime impairments relative to objective measures.34,35 Whether this tendency generalizes to the estimation of reduced productivity attributable to insomnia is unclear.
Another limitation is that the methods used to estimate productivity have not been validated. However, unless dealing with assembly-line style occupations where work productivity measures can be obtained by counting output units, quantifying productivity decreases will remain approximate. Also, while the sample size was sufficient to study costs of relatively frequently occurring events such as consultations or medication use, it was too small to draw valid conclusions about less frequent events such as accidents and hospitalizations. Finally, the higher proportion of women in the study may have increased some cost estimates, as women tend to use the health system more than men. This self-selection bias, which may simply reflect the fact that insomnia is more prevalent among women than men, may have been counterbalanced by higher alcohol and work function costs for men, as men were found to use alcohol as a sleep aid more frequently than women, and men's salaries still remain slightly higher for similar work than women's.
Despite these limitations, this study offers a number of contributions to the literature. Its use of standardized and conservative algorithms to define insomnia may have yielded more conservative and accurate cost estimates relative to studies using more liberal criteria to define insomnia. The differentiation between insomnia syndrome and subsyndromal levels allowed for determining if consumption and cost patterns varied as a function of insomnia severity. Also, burden-of-illness indicators (consultations, transportation, medication/OTC products, alcohol and work function) were measured to include only the costs specific to insomnia. Finally, an attempt was made to apportion the contribution of insomnia to absenteeism and productivity losses; this approach is likely to have yielded more conservative and realistic cost estimates than assuming that all of the lost income was a consequence of insomnia.16 This is an unlikely assumption, given our understanding of the high comorbidity levels that exist between insomnia, depression, anxiety, and physical illnesses.
Future research on the economic burden of insomnia should attempt to distinguish primary insomnia from insomnia comorbid with medical/psychiatric disorders and validate costing methods that would take into consideration the presence and contribution of comorbid disorders. Not adjusting for the contribution of coexisting physical and psychological disorder may inflate cost estimates specifically due to insomnia. Such improved methodology would allow for implementing the much-needed cost-effectiveness research.
Despite its high prevalence and economic burden, insomnia remains for the most part untreated. The present study indicates that the costs of untreated insomnia are significantly greater than the direct costs associated with its treatment. Increased awareness of the availability and effectiveness of insomnia treatments, both on the part of the public as well as health-care providers, could lead to significant reductions in the overall cost of this sleep disorder to society.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Morin has received research support from Sanofi-Aventis and Schering Plough; has participated in speaking engagements for Takeda and Sanofi-Aventis; and has consulted for Sepracor, Pfizer, Actelion, Lundbeck, and Sanofi-Aventis. Dr. Gregoire has received research support from Merck Frost Canada and Novartis Pharma AG. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research was supported by a grant from the Canadian Institutes of Health Research (MT42504).
REFERENCES
- 1.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention. JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 2.Morin CM, LeBlanc M, Daley M, Grégoire JP, Mérette C. Epidemiology of insomnia: Prevalence, self-help treatments and consultations initiated, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 4.Drummond MF, McGuire A. Economic evaluation in health care. Oxford: Oxford University Press; 2001. [Google Scholar]
- 5.Chilcott LA, Shapiro CM. The socioeconomic impact of insomnia. An overview. Pharmacoeconomics. 1996;10(Suppl 1):1–14. doi: 10.2165/00019053-199600101-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kapur VK, Redline S, Nieto FJ, Young TB, Newman AB, Henderson JA. The relationship between chronically disrupted sleep and healthcare use. Sleep. 2002;25:289–96. [PubMed] [Google Scholar]
- 7.Ohayon MM, Caulet M. Psychotropic medication and insomnia complaints in two epidemiological studies. Can J Psychiatry. 1996;41:457–64. doi: 10.1177/070674379604100711. [DOI] [PubMed] [Google Scholar]
- 8.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–23. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 9.Walsh JK. Clinical and socioeconomic correlates of insomnia. J Clin Psychiatry. 2004;65(suppl 8):13–19. [PubMed] [Google Scholar]
- 10.Leger D, Massuel M-A, Metlaine A. Professional correlates of insomnia. Sleep. 2006;29:171–8. [PubMed] [Google Scholar]
- 11.Linton SJ, Bryngelsson I. Insomnia and its relationship to work and health in a working-age population. J Occup Rehabil. 2000;10:169–83. [Google Scholar]
- 12.Sivertsen B, Overland S, Neckelmann D, et al . The long-term effect of insomnia on work disability: the HUNT-2 historical cohort study. Am J Epidemiol. 2006;163:1018–24. doi: 10.1093/aje/kwj145. [DOI] [PubMed] [Google Scholar]
- 13.Schweitzer PK, Engelhardt CL, Hilliker NA, Muehlbach MJ, Walsh JK. Consequences of reported poor sleep. J Sleep Res. 1992;21:260. [Google Scholar]
- 14.Walsh JK, Engelhardt CL. The direct economic costs of insomnia in the United States for 1995. Sleep. 1999;22(Suppl 2):S386–93. [PubMed] [Google Scholar]
- 15.Leger D, Levy E, Paillard M. The direct costs of insomnia in France. Sleep. 1999;22(Suppl 2):S394–401. [PubMed] [Google Scholar]
- 16.Stoller MK. Economic effects of insomnia. Clin Ther. 1994;16:873–97. [PubMed] [Google Scholar]
- 17.Johnson LC, Spinweber CL. Good and poor sleepers differ in Navy performance. Mil Med. 1983;148:727–31. [PubMed] [Google Scholar]
- 18.Godet-Cayre V, Pelletier-Fleury N, Le Vaillant M, Dinet J, Massuel MA, Leger D. Insomnia and absenteeism at work. Who pays the cost? Sleep. 2006;29:179–84. doi: 10.1093/sleep/29.2.179. [DOI] [PubMed] [Google Scholar]
- 19.Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep. 2006;29:299–305. doi: 10.1093/sleep/29.3.299. [DOI] [PubMed] [Google Scholar]
- 20.Ozminkowski RJ, Shaohung SW, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 21.Kish L. Survey sampling. New York: Wiley; 1965. [Google Scholar]
- 22.American Psychiatric Association. Washington, DC: American Psychiatric Association; 2000. Diagnostic and statistical manual of mental disorders – Text Revisions (DSM-IV-TR) [Google Scholar]
- 23.World Health Organization. Geneva: World Health Organization; 1992. The ICD-10 classification of mental and behavioral disorder: diagnostic criteria for research. (10th revision) [Google Scholar]
- 24.Morin CM. Insomnia: Psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- 25.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 26.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 27.American Hospital Formulary Service. American Society of Health-System Pharmacists; 2002. Retrieved from: http://www.ashp.org/ahfs/index.cfm. [Google Scholar]
- 28.Nonprescription Drug Manufacturers Association of Canada (NDMAC) Most frequently used over-the-counter products by Canadians. 2002 Retrieved from: http://www.ndmac.ca/
- 29.Drummond MF, Schulpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for economic evaluation of health care programmes. 3rd ed. New York: Oxford University Press; 2005. [Google Scholar]
- 30.Thompson SG, Barber JA. How should cost data in randomised controlled trials be analysed? BMJ. 2000;320:1197–200. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 1996 Jun;30(Suppl):17–30. [PubMed] [Google Scholar]
- 32.Conrad FG, Brown NR, Cashman ER. Strategies for estimating behavioural frequency in survey interviews. Memory. 1998;6:339–66. doi: 10.1080/741942603. [DOI] [PubMed] [Google Scholar]
- 33.Friedman WJ. Memory for the time of past events. Psychol Bull. 1993;35:44–66. [Google Scholar]
- 34.Edinger JD, Fins AI. The distribution and clinical significance of sleeptime misperceptions among insomniacs. Sleep. 1995;18:232–9. doi: 10.1093/sleep/18.4.232. [DOI] [PubMed] [Google Scholar]
- 35.Vignola A, Lamoureux C, Bastien CH, Morin CM. Effects of chronic insomnia and use of benzodiazepines on daytime performance in older adults. J Gerontol B: Psychol Sci Soc Sci. 2000;55B:54–62. doi: 10.1093/geronb/55.1.p54. [DOI] [PubMed] [Google Scholar]