Abstract
PURPOSE We wanted to explore the associations between intimate partner violence (IPV) and comorbid health conditions, which have received little attention in male patients.
METHODS Using a computer-based self-assessment health questionnaire, we screened sequential emergency department patients who were urban, male, and aged 18 to 55 years. We then examined associations between types of IPV disclosures, co-occurring mental health symptoms, and adverse health behaviors.
RESULTS Of 1,669 men seeking nonurgent health care, 1,122 (67.2%) consented to be screened, and 1,026 (91%) completed the screening; 712 (63%) were in a relationship in the past year. Of these men, 261 (37%) disclosed IPV: 20% (n = 144) disclosed victimization only, 6% (n = 40) disclosed perpetration only, and 11% (n= 77) disclosed bidirectional IPV (defined as both victimization and perpetration in their relationships). Men disclosing both victimization and perpetration had the highest frequencies and levels of adverse mental health symptoms. Rates of smoking, alcohol abuse, and drug use were likewise higher in IPV-involved men.
CONCLUSIONS A cumulative risk of poor mental health and adverse health behaviors was associated with IPV disclosures. Self-disclosure by men seeking acute health care provides the potential for developing tools to assess level of risk and to guide tailored interventions and referrals based on the sex of the patient.
Keywords: Male intimate partner violence, violence and mental health, behavioral health risks, preventive health screening, aggression, interpersonal relations, violence, health risk appraisal, health surveys
INTRODUCTION
Intimate partner violence (IPV), defined as a pattern of assaultive and coercive behaviors in intimate relationships, remains a major public health concern in the United States.1,2 The health care system advocates screening women for victimization and referring them to legal and community-based advocacy services. Both men and women, however, perpetrate a wide range of emotional and physical violence against their intimate partners, and3–5 bidirectional IPV may be more common than generally recognized in medical settings.6,7 Substance abuse and mental health problems have been found to be major cofactors in IPV,8–10 and there is reason to believe that interventions aimed at reducing violent behavior will be only marginally effective if co-occurring mental health and substance abuse problems are ignored.11–15 Recent research targeting substance use along with IPV behavior is promising.16–18
The US Preventative Service Task Forces ranked the evidence in favor of routine screening for family violence as inconclusive and raised concerns for possible harm from retaliatory IPV after disclosure. Although it is reasonable to consider whether IPV-involved men could benefit from treatment under a medical model, the topic requires more study. Numerous studies quantify the co-occurrence of IPV and adverse mental health symptoms and substance use in women patients,19–21 but fewer address these issues in IPV-involved men.22 In fact, there are few venues for IPV-involved men to receive help outside the criminal justice setting.23 The acute health care setting may be one such potential venue.24
A recent editorial citing the presence of IPV perpetrators in the emergency department setting called for research on their identification and potential for treatment,25 as the emergency department may be the only contact with a health care clinician for low-income and medically underinsured patients.26 Previous work suggests both male and female patients will disclose IPV perpetration and victimization on a computer-based health risk assessment in an emergency department setting, knowing the clinician will see the results.27 Likewise, MacMillan et al28 found patients preferred self-administered screening.
The larger investigation ascertained the safety and effectiveness of screening urban patients for IPV victimization and perpetration using a computer kiosk29 and assessed mental health symptoms in IPV-involved women.30 In this article, we focus on the mental health correlates of IPV in male patients. Our second objective was to identify the strength of the associations between types of abuse disclosed (emotional, physical, and sexual, as well as both unidirectional and bidirectional IPV) and the number of co-occurring mental and behavioral health problems in men. We predicted more IPV disclosure in men would be positively associated with an increase in adverse mental health symptoms and substance use.
METHODS
Study Design
Our cross-sectional study (with a small prospective follow-up) was made up of primarily African American men seeking care in emergency departments who self-reported being in a relationship in the past year and answered questions about IPV involvement (victimization, perpetration, or both) at a computer kiosk. Four groups of male patients were compared (those disclosing IPV victimization, perpetration, both victimization and perpetration, and those with no IPV disclosures) with respect to mental health symptoms, alcohol use, and use of tobacco and street drugs. All patients who reported IPV received brief counseling and referrals. To assess the safety of the screening process, we collected 1-week and 3-month follow-up information on all victims. At a follow-up interview, which took place in the emergency department, we asked about any adverse events related to screening and whether victims had acted on suggested referrals. Because emergency departments are notorious for poor follow-up rates, we also tracked 911 calls from the addresses of all screened patients living in the surrounding police district for 6 months before and 6 months after the screening visit as a measure of retaliatory violence.29
Selection of Participants and Setting
The study site was in a large southeastern city at a public hospital and trauma center that treats 105,000 patients a year. Sequential eligible patients between the ages of 18 and 55 years were approached in the emergency department waiting room during predetermined study times. Participants were excluded if they could not read English at a 5th-grade level or were intoxicated, acutely psychotic, or too ill to stand and complete a 20-minute health-assessment questionnaire. All participants were taken to a semiprivate booth in the waiting room, where they were invited and, if interested, consented to participate in a study using a computer-based health risk assessment. They received health information and tailored community referrals based on their disclosed health risks. The university institutional review board approved the study.
Data Collection
We collected standard demographic information and, when possible, used validated questions to measure IPV, depression, traumatic stress, suicidality, and substance use, as well as general health. Participants were free to stop the computer-screening process at any point for any reason, and they were encouraged to stop if they were called to see the physician or became too sick. Any patient who disclosed current suicidality was immediately referred to the attending physician for evaluation.
Methods of Measurement
IPV victimization and perpetration questions were only asked of patients who said they had been in a relationship in the past year. Victimization was assessed using The George Washington University Universal Violence Prevention Screening Protocol,24 which consists of 6 questions previously validated in our population.31 To assess perpetration, we used a modified version of a scale developed by the first author32,33 that consisted of 8 questions assessing controlling behavior, verbal aggression, attitudes toward physical and sexual aggression, and both physical and sexual abuse of a current partner. The questions and validation information for both IPV scales are available in the Supplemental Appendix, available online at http://www.annfammed.org/cgi/content/full/7/1/47/DC1.
We used the Beck Depression Inventory-II (BDI-II)34 to ascertain the presence and severity of depressive symptoms. Total BDI-II scores of 20 or higher, indicative of moderate or severe levels of depressive symptoms, were coded as presence of depressive symptoms.35 We used part 3 of the Posttraumatic Stress Diagnostic Scale36 to determine the presence and severity of symptoms of posttraumatic stress disorder (PTSD); consistent with recommendations, patients who had scores of 21 or higher, reflective of moderate or severe levels of PTSD symptoms, were coded as having PTSD symptoms. We used the Scale for Suicide Ideation37 to measure suicidal intent. Patients scoring 11or higher were considered positive for suicidal ideation38 and were referred for psychiatric evaluation.
Adverse health behaviors related to alcohol abuse were assessed using the CAGE screening test.39 One positive response is considered indicative of risky drinking and 2 or more are considered at risk for alcoholism.40,41 Because we were also interested in binge drinking, which has a strong association with IPV,8,16 2 questions were added about quantity and frequency (drinking 3 or more days a week and drinking 4 or more drinks on any single occasion), both of which had to be answered in the affirmative to prompt a concern for possible problem drinking. By contrast, health behaviors related to use of tobacco and street drugs were each assessed by single questions: “Do you smoke cigarettes?” and “Have you used any street drugs in the past 4 weeks?” Because use of tobacco and street drugs was not the focus of the study, these behaviors were not incorporated in the current analysis.
Data Analysis
We used SAS statistical software (version 8, SAS Institute, Cary, North Carolina) for data analyses. Proportions and a series of χ2 analyses (or exact distribution alternative) were computed to assess bivariate associations between IPV status (any/none) and demographic and health-related characteristics. We used the t test to compare age distributions by IPV status. We calculated prevalence and prevalence ratios of IPV victimization and perpetration status with 95% confidence intervals to assess bivariate associations between IPV status, mental health symptoms, and health behaviors.
The sample size was calculated from the number of IPV-positive individuals (both men and women) needed for follow-up to assess safety of the IPV screening, about 2 times the number of men needed to assess the association between IPV and mental health reports.
RESULTS
A total of 1,669 male patients were eligible for participation in the survey, and 1,122 (67.2%) consented to participate. No significant differences existed for race, age, or chief complaint between participants and non-participants. Of the men who consented to participate in the study, 1,026 (91%) participants completed all key elements of the questionnaire. Of the screened men, 712 (63%) participants had been in a relationship in the past year and answered questions about past year victimization or perpetration. This group made up our study population.
Table 1 ▶ displays the demographic information of the male participants by their IPV status. Most participants were single, African American, and uninsured. In general, IPV-involved men were less educated and less likely to be employed. They were more likely to be separated or divorced and more likely to report moderate to severe symptoms of depression, PTSD, and suicidality. IPV-involved men also were more likely to engage in other adverse health behaviors, including smoking, at-risk drinking, street drug use, nonuse of seatbelts, and risky sexual behavior.
Table 1.
Demographic Characteristics of Male Emergency Departments Patients in Relationships (N = 712)*
| Characteristic (No. Responding) | IPV Positive (n=261) | IPV Negative (n=451) | P Value | ||
| Age, mean (range), y (n = 708) | 35.4 (18–65) | 35.2 (18–66) | .835 | ||
| No. | % | No. | % | ||
| Race (n=712) | .693 | ||||
| White | 24/261 | 9.2 | 35/451 | 7.8 | |
| African American | 229/261 | 87.7 | 408/451 | 90.5 | |
| Hispanic | 1/261 | 0.4 | 2/451 | 0.4 | |
| Asian | 1/261 | 0.4 | 1/451 | 0.2 | |
| Other | 6/261 | 2.3 | 5/451 | 1.1 | |
| Education (n=705) | .004 | ||||
| No high school diploma | 52/255 | 20.4 | 60/450 | 13.3 | |
| High school diploma | 128/255 | 50.2 | 201/450 | 44.7 | |
| Some/completed college | 54/255 | 21.2 | 127/450 | 28.2 | |
| College graduate | 21/255 | 8.2 | 62/450 | 13.8 | |
| Health insurance (n = 694) | .126 | ||||
| None | 204/253 | 80.6 | 353/441 | 80.1 | |
| Medicaid/Medicare | 23/253 | 9.1 | 26/441 | 5.9 | |
| Private/employment/student | 26/253 | 10.3 | 62/441 | 14.1 | |
| Marital status (n = 708) | .017 | ||||
| Single (never married) | 176/258 | 68.2 | 325/450 | 72.2 | |
| Separated/divorced/widowed | 53/258 | 20.5 | 58/450 | 12.9 | |
| Married | 29/258 | 11.2 | 67/450 | 14.9 | |
| Reason for visit (n = 698) | .590 | ||||
| Medical | 215/255 | 84.3 | 365/443 | 82.4 | |
| Injury | 21/255 | 8.2 | 47/443 | 10.6 | |
| Other | 19/255 | 7.5 | 31/443 | 7.0 | |
| Employed (n=709) | 139/260 | 53.5 | 270/449 | 60.1 | .083 |
| Moderate/severe depressiona (n=712) | 48/261 | 18.4 | 15/451 | 3.3 | <.001 |
| Moderate/severe PTSDb (n=712) | 27/261 | 10.3 | 5/451 | 1.1 | <.001 |
| Suicidal ideationsc (n=712) | 24/261 | 9.2 | 3/451 | 0.7 | <.001 |
| Smoking (n=712) | 163/261 | 62.5 | 224/451 | 49.7 | .001 |
| Street drugsd (n=712) | 90/261 | 34.5 | 110/451 | 24.4 | .004 |
| High-risk sexual behaviore (n=698) | 95/252 | 37.7 | 118/437 | 27.0 | .003 |
| At-risk drinkingf (n=712) | 128/261 | 49.0 | 168/451 | 37.3 | .002 |
| Same-sex sexual partnerg (n=704) | 27/259 | 10.4 | 43/445 | 9.7 | .745 |
| Handgun accessh (n=706) | 49/260 | 18.9 | 68/446 | 15.3 | .215 |
| Seatbelt usei (n=703) | 151/258 | 58.5 | 338/445 | 76.0 | <.001 |
| Smoke detectorj (n=694) | 217/252 | 86.1 | 395/442 | 89.4 | .201 |
IPV = intimate partner violence; PTSD = posttraumatic stress disorder.
Note: data are reported for the number and percentage of participants answering the particular question or set of questions, (eg, age is missing for 4 participants (3 IPV positive, 1 IPV negative), so n = 708.
a Depression measured by the Beck Depression Index: scores ≥20 are indicative of moderate or severe levels of depressive symptoms.34,35
b Posttraumatic Stress Diagnostic Scale: scores >20 reflect moderate or severe levels of PTSD symptoms.36
c Scale for Suicide Ideation: scores >11 were considered suicidal and referred for psychiatric evaluation.37,38
d Use of street drugs in last 4 weeks, or a history of intravenous drug use.
e Nonuse of condoms and 1 of the following: history of a sexually transmitted disease in past 5 years, or more than 1 sexual partner in last year.
f At least 1 positive responses to CAGE questions or drinking at least 3 times week and 4 or more drinks per day on occasion.
g Had sex with a person of the same sex in past 10 years.
h Has handgun in home or car or someone close has a gun.
i Always uses a seatbelt in a car.
j Has a working smoke detector where they live.
Table 2 ▶ shows the number and percentages of men in relationships and who were positive for IPV victimization and perpetration by each question on the measures. Of the 712 men, 451 (63%) did not report any IPV, and 261 (37%) disclosed at least 1 type of IPV (emotional, physical, or sexual): 20% (n = 144) disclosed IPV victimization only, 5% (n = 40) disclosed IPV perpetration only, and 11% (n = 77) disclosed bidirectional IPV (both victimization and perpetration). Victimization was reported more often than perpetration, with emotional and physical victimization endorsed more frequently than sexual victimization.
Table 2.
Distribution of “Yes” Answers to Violence-Related Questions by All Men in Relationships Who Completed the IPV Questions on the Computer Survey (N = 712)
| IPV Questions | No. (%) |
| Victimization | |
| Within the past year has a partner slapped, kicked, pushed, choked, or punched you? | 119 (16.7) |
| Within the past year has a partner forced or coerced you to have sex? | 48 (6.7) |
| Within the past year has a partner threatened you with a knife/gun to scare/hurt you? | 40 (5.6) |
| Within the past year has a partner made you afraid you would be physically hurt? | 33 (4.6) |
| Within the past year has a partner used words/yelled/screamed in a way that frightened you? | 133 (18.7) |
| Total disclosing any IPV victimization | 221 (31.0) |
| Perpetration | |
| Do you feel like you always need to be in control of your partner? | 61 (8.5) |
| When you get angry, does it make your partner afraid? | 110 (15.5) |
| Have you hit/pushed/shoved your partner in the past year? | 86 (12.1) |
| Do you think there are times when it’s OK to physically hurt your partner? | 20 (2.8) |
| Have you physically hurt your partner in the past year? | 30 (4.2) |
| Are you worried you might physically hurt your partner? | 34 (4.8) |
| Do you think your partner should have sex when he/she doesn’t want to? | 119 (16.7) |
| Have you made your partner have sex when he/she didn’t want to? | 33 (4.6) |
| Total disclosing any IPV perpetration | 117 (16.4) |
| Total disclosing both victimization and perpetration | 77 (10.8) |
| Total with any IPV | 261 (36.7) |
IPV=intimate partner violence.
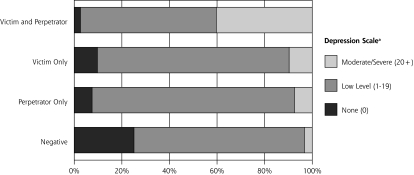
Figure 1 ▶ categorizes the mental health symptom scores by the extent of IPV-involvement. Mental health scores in the clinical range (moderate/severe) were more common for those who experienced any IPV and were highest among those reporting both victimization and perpetration; patient reports of any symptoms followed a similar pattern. Table 3 ▶ shows the prevalence ratios for both adverse mental health symptoms and unhealthy behaviors by IPV status. Those reporting perpetration only were more likely to report adverse mental health symptoms than those reporting victimization only, but those reporting both victimization and perpetration had the highest levels of adverse mental health symptoms. A similar gradient was identified for adverse health behaviors. The prevalence ratios of drug, tobacco and alcohol use increased as abuse and violence in the relationship increased, with bidirectional IPV having the greatest risks of poor mental health and unhealthy behaviors.
Figure 1.
Mental health symptom scores, by intimate partner violence status.
PTSD=posttraumatic stress disorder.
a Depression measured by the Beck Depression Inventory: ≥20 are indicative of moderate or severe levels of depressive symptoms.34,35
b Posttraumatic Stress Diagnostic Scale: scores of >20 reflect moderate or severe levels of PTSD symptoms.36
c Scale for Suicide Ideation: patients with scores of >11 were considered suicidal and referred for psychiatric evaluation37,38
Table 3.
Prevalence Ratios of Mental Health Symptoms and Adverse Health Behaviors by IPV Status for All Men in Relationships Who Completed the IPV Questions on the Computer Survey (n = 712)
| IPV Negative(n=451) | Any IPV (n=261) | Victim Only (n=144) | Perpetrator Only (n=40) | Victim and Perpetrator (n=77) | ||||||
| Symptoms and Adverse Behaviors | % | PRa | % | PR (95% CI) | % | PR (95% CI) | % | PR (95% CI) | % | PR (95% CI) |
| Depression | 3.3 | 1.00 | 18.4 | 5.53 (3.16–9.67) | 9.7 | 2.92 (1.45–5.91) | 7.5 | 2.26 (0.68–7.46) | 40.3 | 12.10 (6.87–21.34) |
| PTSD | 1.1 | 1.00 | 10.3 | 9.33 (3.64–23.93) | 6.9 | 6.26 (2.18–18.03) | 10.0 | 9.02 (2.52–32.26) | 16.9 | 15.23 (5.59–41.51) |
| Suicidality | 0.7 | 1.00 | 9.2 | 13.82 (4.20–45.46) | 3.5 | 5.22 (1.26–21.57) | 2.5 | 5.22 (1.26–21.57) | 23.4 | 35.14 (10.60–116.46) |
| Illegal drugs | 24.4 | 1.00 | 34.5 | 1.14 (1.12–1.79) | 27.1 | 1.11 (0.82–1.52) | 35.0 | 1.44 (0.91–2.26) | 48.1 | 1.97 (1.48–2.62) |
| Smoke cigarettes | 49.7 | 1.00 | 62.5 | 1.26 (1.10–1.44) | 64.6 | 1.30 (1.12–1.51) | 55.0 | 1.11 (0.82–1.49) | 62.3 | 1.26 (1.03–1.53) |
| Ethanol use in excess | 37.3 | 1.00 | 49.0 | 1.32 (1.11–1.56) | 38.9 | 1.04 (0.82–1.32) | 50.0 | 1.34 (0.96–1.87) | 67.5 | 1.81 (1.49–2.21) |
IPV = intimate partner violence; PR = prevalence ratio; PTSD = posttraumatic stress disorder.
a Reference group.
There were no detectable adverse events related to screening, either observed by the research assistants in the emergency department or reported by the 80 (56%) of male victims who returned for 1-week follow-up. Nor did we identify any increase in 911 calls to the addresses of screened men, regardless of IPV status (Table 4 ▶).
Table 4.
Rates of 911 Telephone Calls to Addresses of Male Study Participants 6 Months Before and After Screening
| Possible Violence | Total Telephone Calls | |||
| Participants | No. | % | No. | % |
| All participants (n = 531) | ||||
| 6 Months before | 67 | 13 | 124 | 23 |
| 6 Months after | 67 | 13 | 143 | 27 |
| Participant not a victim of IPV (n=439) | ||||
| 6 Months before | 54 | 12 | 99 | 23 |
| 6 Months after | 62 | 14 | 125 | 29 |
| All IPV victims (n = 92) | ||||
| 6 Months before | 13 | 14 | 25 | 27 |
| 6 Months after | 5 | 5 | 18 | 20 |
| IPV victim did not participate in 1-week follow-up (n = 51) | ||||
| 6 Months before | 7 | 14 | 13 | 25 |
| 6 Months after | 3 | 6 | 10 | 20 |
| IPV victim participated in 1-week follow-up (n = 41) | ||||
| 6 Months before | 6 | 15 | 12 | 30 |
| 6 Months after | 2 | 5 | 8 | 20 |
IPV=intimate partner violence.
Note: Data available only for those living in police districts in the county.
For the men disclosing victimization who returned to the emergency department for follow-up visits, Table 5 ▶ shows 1-week and 3-month use of referral resources. At 1 week, 55% said they had read the educational and referral information provided, and 13% had contacted IPV resources. Although only 47 male victims returned at 3 months, 15 (32%) reported they had contacted the referral resources; of those, 8 (17%) had sought mental health counseling, and 5 (11%) had sought alcohol counseling.
Table 5.
Most Frequently Reported Use of Resources and Safety Measures Taken by Male Patients Who Screened Positive for IPV Victimization
| Resources and Safety Measuresa | 1-Week Follow-Up Report (n=80) No. (%) | 3-Month Follow-Up Report (n=47) No. (%) |
| Used any of the resources | 8 (10) | 15 (32) |
| Hotline | 2 (2.5) | 7 (15) |
| IPV support groups | 5 (11) | |
| IPV shelter | 1 (1.3) | 2 (4.3) |
| Emergency housing | 1 (1.3) | |
| Alcohol treatment | 1 (1.3) | 5 (11) |
| Mental health counseling | 2 (2.5) | 8 (17) |
| Read information | 44 (55) | 24 (51) |
| Made a safety plan | 13 (16) | |
| Hid money in case you need to leave | 15 (19) | |
| Moved out | 11 (14) | 18 (38) |
| Called IPV hotlines or referrals | 10 (13) | |
| Changed or unlisted telephone number | 9 (19) |
IPV = intimate partner violence; WEB = Women’s Evidence of Battering Scale.
Note: a positive finding for male IPV victimization was any positive response on the IPV victimization scale and either lack of perpetration disclosure or evidence of battering (WEB >20) on a sex-neutral version of the battering scale.
a Results available only for men who returned to the emergency department for follow-up interviews at 1 week and/or 3 months after initial screening, counseling, and referral to resources.
DISCUSSION
We found that men coming to an urban emergency department for nonurgent complaints self-disclosed a substantial amount of IPV; 37% of men in an intimate relationship in the past year disclosed IPV victimization, perpetration, or both. Results regarding confounding factors, such as social disadvantage, support a general pattern of cumulative exposure leading to increased risk.42–44 The amount of IPV involvement was associated with increasing proportions of patients reporting moderate/severe mental health symptoms. Depression, PTSD, and suicidality scores all were higher, and those experiencing and/or perpetrating more types of abuse had the highest number of adverse mental health symptoms. Proportions of smoking, drinking and street drug use were also higher in IPV-involved men, providing further support that at least some of the adverse health effects associated with violence may be due to unhealthy behaviors.45 This finding is similar to that of other studies which found multiple comorbid health conditions in patients with high trauma exposure.45–49
There are studies on the psychological comorbidities of men in court-mandated batterer’s treatment.10,15 Our work lends support to studies that describe the co-occurrence of IPV with depression and substance abuse in IPV-involved individuals.50
El-Bassel et al described rates of IPV and substance abuse in women of ethnic minorities,51 and others have assessed the mental health impact of IPV in women,18,20,21 but less attention has focused on the mental health symptoms and substance abuse problems of IPV-involved men coming to health care settings.
Looking specifically at emergency department patients, Lipsky et al found 15% of male patients in a Los Angeles emergency department self-reported current IPV perpetration, including 17.1% of African American and 9.1% of Latino male patients.52 In our study, the cumulative amount of abuse disclosures (emotional, physical, sexual) and amount of unidirectional and bidirectional violence (victimization, perpetration, or both) were related in a dose-response manner to levels of depression, PTSD, and suicidal ideation.
Given the high degree of overlap, one could argue that identifying male partner violence should be a part of any mental health and substance abuse assessment. The literature on screening men in health care settings as part of comprehensive health risk assessments is scant, however. Several studies report that men screened in the emergency department for partner violence had rates of partner violence similar to that of women; between 13% and 30% of men in various emergency department samples report current physical IPV victimization.52–54 Others have concluded that many of these men were abusers.55–57 Among men in a batterer’s treatment program, 46% said they had seen a physician in the last 6 months; the emergency department was the most common site.58 Because the emergency department is likely to see a heterogeneous group of men with varying levels of IPV risk, it will be important to identify men’s IPV victimization as well as their perpetration, along with comorbid conditions that might lend themselves to intervention.
Most assessments and interventions with IPV-involved men have been through the criminal justice system, which uses a one-size-fits-all model of group didactics and cognitive restructuring.59 Only a small fraction of IPV-involved men engage in treatment, however, and less than one-half subsequently complete these programs.60,61 Not surprisingly, many interventions for IPV-involved men have been unable to show any effectiveness.62,63 In part, this lack of effectiveness may be because current interventions for IPV have often failed to address adequately the comorbid mental health and substance abuse problems that may exist for both victims and perpetrators. One central problem in the field of IPV batterer’s treatment is how to best match types of interventions to subpopulations of perpetrators.64 New methods for identification and risk stratification of IPV need to account for the severity and periodicity of occurrences, as well as comorbid conditions. If it can be determined that routine IPV screening with men in health care settings is safe, we can add additional tools to improve recognition of high-risk situations and make distinctions between broad categories of male partner violence. Improving our understanding of the interactions between mental health and violence as they relate to the complexities of human relationships will be important if we are to develop new tailored interventions that can be delivered outside of the criminal justice system.65
Limitations
This study has a number of important limitations. The patient population was a fairly homogeneous convenience sample of urban, primarily indigent, African American men seeking health care at 1 large county hospital emergency department, which limits generalizability. Only nonurgent patients were recruited; thus, we may have missed the more severe forms of IPV seen with major trauma. Although there was no indication of any safety concerns related to screening men for IPV based on observation during the emergency department visit self-report at 1 week or an increase in 911 telephone calls to their addresses, we were only able to follow up on 55% of male victims at 1 week. Also the study method of using 911 calls to their address can result in misclassification, because we did not track the 911 calls by individual, just by address. So there may have been undetected adverse events. IPV was self-reported and therefore subject to recall bias or unwillingness to disclose. There was no external validation of the actual levels and types of IPV, so the potential for classification error warrants caution when interpreting our results. Although we tried to use validated screening tools, IPV is best validated by partner report, and more work is needed to improve the sensitivity and specificity of screening tools for IPV in male patients in health care settings.
In conclusion, we found a cumulative risk of depressive and PTSD symptoms, suicidal ideation, and substance abuse to be associated with violence in the relationships of male urban emergency department patients. The identification of IPV risk in men as part of a health risk assessment provides opportunities for new targeted IPV interventions delivered outside the criminal justice setting. Such interventions must be guided by an understanding of the heterogeneity of male partner violence and co-occurring behavioral and mental health issues.
Acknowledgments
The authors wish to acknowledge Joanna Bisgaier, MSW, for help with manuscript preparation, James Wiley, PhD, for inspiration and conceptual clarity, and the many other people who have contributed to this project, particularly our research assistants, Robin Schultz Kemball, MPH, and Hadley Mintz, MPH, and the staff and patients of Grady Hospital Emergency Department.
Conflicts of interest: none reported
Funding support: The data used in this study was collected with support from Centers for Disease Control and Prevention, R49 423113. Karin Rhodes, MD, MS, was supported by a grant from the National Institute of Mental Health, K23 MH64572; Debra Houry, MD, MPH, was supported by a grant from the National Institute of Mental Health, K23069375.
REFERENCES
- 1.Tjaden P, Thoennes N. Prevalence, Incidence, and Consequences of Violence Against Women: Findings From the National Violence Against Women Survey. Washington, DC: National Institute of Justice and Centers for Disease Control and Prevention; 1998.
- 2.Saltzman LE, Green YT, Marks JS, Thacker SB. Violence against women as a public health issue. Am J Prev Med. 2000;19(4):325–329. [DOI] [PubMed] [Google Scholar]
- 3.Archer J. Sex differences in aggression between heterosexual partners: a meta-analytic review. Psychol Bull. 2000;126(5):651–680. [DOI] [PubMed] [Google Scholar]
- 4.Cascardi M, Langhinrichsen J, Vivian D. Marital aggression: impact, injury, and health correlates for husbands and wives. Arch Intern Med. 1992;152(6):1178–1184. [DOI] [PubMed] [Google Scholar]
- 5.Caetano R, Ramisetty-Mikler S, Field CA. Unidirectional and bi-directional intimate partner violence among White, Black, and Hispanic couples in the United States. Violence Vict. 2005;20(4):393–406. [PubMed] [Google Scholar]
- 6.Straus MA. The controversy over domestic violence by women: a methodological, theoretical, and sociology of science analysis. In: Arriaga XB, Oskamp S. Violence in Intimate Relationships. Thousand Oaks, CA: Sage Publications; 1999.
- 7.Vivian D, Langhinrichsen-Rohling J. Are bi-directionally violent couples mutually victimized? A gender-sensitive comparison. Violence Vict. 1994;9(2):107–124. [PubMed] [Google Scholar]
- 8.Cunradi CB, Caetano R, Clark CL, Schafer J. Alcohol-related problems and intimate partner violence among White, Black, and Hispanic couples in the US. Alcohol Clin Exp Res. 1999;23(9):1492–1501. [PubMed] [Google Scholar]
- 9.Lipsky S, Caetano R, Craig A. Larkin. GL: Psychosocial and substance-use risk factors for intimate partner violence. Drug Alcohol Depend. 2004;78(1):39–47. [DOI] [PubMed] [Google Scholar]
- 10.Bennett LW, Tolman RM, Rogalski CJ, Srinivasaraghavan J. Domestic abuse by male alcohol and drug addicts. Violence Vict. 1994;9(4):359–368. [PubMed] [Google Scholar]
- 11.Chase KA, O’Farrell TJ, Murphy CM, Fals-Stewart W, Murphy M. Factors associated with partner violence among female alcoholic patients and their male partners. J Stud Alcohol. 2003;64(1):137–149. [DOI] [PubMed] [Google Scholar]
- 12.Chermack ST, Taylor SP. Alcohol and human physical aggression: pharmacological versus expectancy effects. J Stud Alcohol. 1995;56(4):449–456. [DOI] [PubMed] [Google Scholar]
- 13.Collins JJ, Kroutil LA, Roland EJ, Moore-Gurrera M. Issues in the linkage of alcohol and domestic violence services. In: Galanter M, ed, Alcoholism and Violence. New York, NY: Plenum Press; 1997:387–405. [DOI] [PubMed]
- 14.Danielson KK, Moffitt TE, Caspi A, Silva PA. Comorbidity between abuse of an adult and DSM-III-R mental disorders: evidence from an epidemiological study. Am J Psychiatry. 1998;155(1):131–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones AS, Gondolf EW. Time-varying risk factors for reassault among batterer program participants. J Fam Violence. 2001;16(4):345–359. [Google Scholar]
- 16.Leonard KE. Drinking patters and intoxication in marital violence: review, critique and future directions for research. In: US Department of Health and Human Services, ed. Research Monograph 24: Alcohol and Interpersonal Violence: Fostering Multidisciplinary Perspectives. Rockville, MD: National Institutes of Health; 1993:253–280.
- 17.O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. J Subst Abuse Treat. 2000;18(1):51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Farrell TJ, Choquette KA, Cutter HS, et al. Cost-benefit and cost-effectiveness analyses of behavioral marital therapy as an addition to outpatient alcoholism treatment. J Subst Abuse. 1996;8(2):145–166. [DOI] [PubMed] [Google Scholar]
- 19.Campbell JC, Kub J, Belknap RA, Templin T. Predictors of depression in battered women. Violence Against Women. 1997;3(3):271–293. [Google Scholar]
- 20.Coid J, Petruckevitch A, Chung W, Richardson J, Morrey S, Feder G. Abusive experiences and psychiatric morbidity in women primary care attenders. Br J Psychiatry. 2003;183:332–339. [DOI] [PubMed] [Google Scholar]
- 21.Stein MB. Kennedy C. Major depressive and post-traumatic stress disorder comorbidity in female victims of intimate partner violence. J Affect Disord. 2001;66(2–3):133–138. [DOI] [PubMed] [Google Scholar]
- 22.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260–268. [DOI] [PubMed] [Google Scholar]
- 23.O’Leary KD. Conjoint therapy for partners who engage in physically abusive behavior. In: Geffner R, Rosenbaum A, eds. Domestic Violence Offenders: Current Interventions, Research, and Implications for Policies and Standards. New York, NY: Haworth; 2001:145–164.
- 24.Dutton MA, Mitchell B, Haywood Y. The emergency department as a violence prevention center. J Am Med Womens Assoc. 1996;51(3):92–95, 117. [PubMed] [Google Scholar]
- 25.Ernst AA. Intimate partner violence: steps for future generations. Ann Emerg Med. 2006;47(2):200–202. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Government Printing Office; 2000.
- 27.Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40(5):476–484. [DOI] [PubMed] [Google Scholar]
- 28.MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2006;296(5):530–536. [DOI] [PubMed] [Google Scholar]
- 29.Houry D, Kaslowe N, Kemball RS, et al. Does screening in the emergency department hurt or help victims of intimate partner violence? Ann Emerg Med. 2008;51(4):433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Houry D, Kemball R, Rhodes KV, Kaslow NJ. Intimate partner violence and mental health symptoms in African American female emergency department patients. Am J Emerg Med. 2006;24(4): 444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heron SL, Thompson MP, Jackson E. Kaslowe. NJ: Do responses to an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income black women? Ann Emerg Med. 2003;42(4):483–491. [DOI] [PubMed] [Google Scholar]
- 32.Rhodes KV, Khan Z. Validating a screen for IPV among male emergency department patients. Acad Emerg Med. 2005;12(5):46. [Google Scholar]
- 33.Rhodes KV, Lauderdale DS, Stocking CB, Howes DS, Roizen MF, Levinson W. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37(3):284–291. [DOI] [PubMed] [Google Scholar]
- 34.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
- 35.Dozois DJ, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory-II. Psychol Assess. 1998;10:83–89. [Google Scholar]
- 36.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 37.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behav Res Ther. 1997;35(11):1039–1046. [DOI] [PubMed] [Google Scholar]
- 39.Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905–1907. [DOI] [PubMed] [Google Scholar]
- 40.Nilssen O, Cone H. Screening patients for alcohol problems in primary health care setting. Alcohol Health Res World. 1994;18(2):136–139. [Google Scholar]
- 41.Soderstrom CA, Smith GS, Kufera J, et al. The accuracy of the CAGE, the Brief Michigan Alcoholism Screening Test, the Alcohol Use Disorders Identification Test in screening trauma center patients for alcoholism. J Trauma. 1997;43(6):962–969. [DOI] [PubMed] [Google Scholar]
- 42.Ernst AA, Nick TG, Weiss SJ, Houry D, Mills T. Domestic violence in an inner-city ED. Ann Emerg Med. 1997;30(2):190–197. [DOI] [PubMed] [Google Scholar]
- 43.Lemon SC, Verhoek-Oftedahl W, Donnelly EF. Preventive healthcare use, smoking, and alcohol use among Rhode Island women experiencing intimate partner violence. J Womens Health Gend Based Med. 2002;11(6):555–562. [DOI] [PubMed] [Google Scholar]
- 44.Guttman L. A new approach to factor analysis: the radex. In Lazars-feld PF, ed. Mathematical Thinking in the Social Sciences. New York, NY: Free Press; 1954.
- 45.Felitti VJ, Anda RF, Nordenberg D, et al. The relationship of adult health status to childhood abuse and household dysfunction. Am J Prev Med. 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 46.Grisso JA, Schwarz DF, Hirschinger N, et al. Violent injuries among women in an urban area. N Engl J Med. 1999;341(25):1899–1905. [DOI] [PubMed] [Google Scholar]
- 47.Hamberger KL, Potente T. Counseling Heterosexual Women Arrested for Domestic Violence: Implications for Theory and Practice in Domestic Partner Abuse. New York, NY: Springer; 1996. [PubMed]
- 48.Rosenberg HJ, Rosenberg SD, Wolford GL, Manganiello PD, Brunette MF, Boynton RA. The relationship between trauma, PTSD, and medical utilization in three high risk medical populations. Int J Psychiatry Med. 2000;30(3):247–259. [DOI] [PubMed] [Google Scholar]
- 49.Swan SC, Gambone LJ, Fields AM, Sullivan TP, Snow DL. Women who use violence in intimate relationships: the role of anger, victimization, and symptoms of posttraumatic stress and depression. Violence Vict. 2005;20(3):267–285. [DOI] [PubMed] [Google Scholar]
- 50.Dutton DG, Golant SK. The Batterer: A Psychological Profile. New York, NY: Basic Books; 1995.
- 51.El-Bassel N, Gilbert L, Witte S, et al. Intimate partner violence and substance abuse among minority women receiving care from an inner-city emergency department. Womens Health Issues. 2003;13(1):16–22. [DOI] [PubMed] [Google Scholar]
- 52.Lipsky S, Caetano R, Field CA, Bazargan S. The role of alcohol use and depression in intimate partner violence among Black and Hispanic patients in an urban emergency department. Am J Drug Alcohol Abuse. 2005;31(2):225–242. [PubMed] [Google Scholar]
- 53.Goldberg WG, Tomlanovich MC. Domestic violence victims in the emergency department: new findings. JAMA. 1984;251(24):3259–3264. [PubMed] [Google Scholar]
- 54.Mechem CC, Shofer FS, Reinhard SS, Horig S, Datner E. History of domestic violence among male patients presenting to an urban emergency department. Acad Emerg Med. 1999;6(8):786–791. [DOI] [PubMed] [Google Scholar]
- 55.Mills LD, Mills TJ, Taliaferro E, Zimbler A, Smith D. The prevalence of female-tomale intimate partner violence in an urban emergency department. J Emerg Med. 2003;25(2):215–218. [DOI] [PubMed] [Google Scholar]
- 56.Muelleman RL, Burgess P. Male victims of domestic violence and their history of perpetrating violence. Acad Emerg Med. 1998;5(9):869–870. [DOI] [PubMed] [Google Scholar]
- 57.Salber PR, Taliaferro E. Men and domestic violence. Acad Emerg Med. 1998;5(9):849–850. [DOI] [PubMed] [Google Scholar]
- 58.Coben JH, Friedman DI. Health care use by perpetrators of domestic violence. J Emerg Med. 2002;22(3):313–317. [DOI] [PubMed] [Google Scholar]
- 59.Pence E, Paymar M. Education Groups For Men Who Batter: The Duluth Model. New York, NY: Springer; 1993.
- 60.Gondolf E. Evaluating programs for men who batter: problems and prospects. J Fam Violence. 1987;2(1):95–108. [Google Scholar]
- 61.Gondolf E. A comparison of four batterer intervention systems: do court referral, program length, and services matter? J Interpers Violence. 1999;14(1):41–61. [Google Scholar]
- 62.Babcock JC, Green CE, Robie C. Does batterer’s treatment work? A meta-analytic review of domestic violence treatment. Clin Psychol Rev. 2004;23(8):1023–1053. [DOI] [PubMed] [Google Scholar]
- 63.Feder L, Wilson DB. A meta-analytic review of court-mandated batterer intervention programs: can the courts affect abuser’s behavior? J Exp Criminol. 2005;1:239–262. [Google Scholar]
- 64.Cavanaugh MM, Gelles RJ. The utility of male domestic violence offender typologies: new directions for research, policy and practice. J Interpers Violence. 2005;20(2):155–166. [DOI] [PubMed] [Google Scholar]
- 65.Miller SL. Expanding the boundaries: toward a more inclusive and integrated study of intimate violence. Violence Vict. 1994;9(2):183–194. [PubMed] [Google Scholar]