Abstract
This report describes the synthesis of two new cyclic RGD (Arg-Gly-Asp) dimers, 3 (E[G3-c(RGDfK)]2) and 4 (G3-E[G3-c(RGDfK)]2), and their corresponding conjugates 5 (HYNIC-E[G3-c(RGDfK)]2: HYNIC = 6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl) and 6 (HYNIC-G3-E[G3-c(RGDfK)]2). Integrin αvβ3 binding affinities of 5 and 6 were determined by displacement of 125I-echistatin bound to U87MG glioma cells. 99mTc complexes 7 ([99mTc(5)(tricine)(TPPTS)]: TPPTS = trisodium triphenylphosphine-3,3′,3″-trisulfonate) and 8 ([99mTc(6)(tricine)(TPPTS)]) were prepared in high yield and high specific activity. Biodistribution and imaging studies were performed in athymic nude mice bearing U87MG glioma and MDA-MB-435 breast cancer xenografts. It was found that G3 linkers are particularly useful for increasing integrin αvβ3 binding affinity of cyclic RGD dimers, and improving the tumor uptake and clearance kinetic of their 99mTc radiotracers. Complex 8 is a very promising radiotracer for the early detection of integrin αvβ3–positive tumors, and may have the potential for non-invasive monitoring of tumor growth or shrinkage during antiangiogenic treatment.
Keywords: integrin αvβ3, 99mTc-labeled cyclic RGD peptides, SPECT, tumor imaging
INTRODUCTION
Angiogenesis is a requirement for tumor growth and metastasis.1–10 Without the neovasculature to provide oxygen and nutrients, tumors cannot grow beyond 1 – 2 mm in size. Once vascularized, previously dormant tumors begin to grow rapidly and their volumes increase exponentially. The angiogenic process depends on vascular endothelial cell migration and invasion, and is regulated by cell adhesion receptors. Integrins are a family of proteins that facilitate cellular adhesion to and migration on extracellular matrix proteins found in intercellular spaces and basement membranes, and regulate cellular entry and withdraw from the tumor cell cycle.4–13 Integrin αvβ3 is a receptor for extracellular matrix proteins with the exposed arginine-glycine-aspartic (RGD) tripeptide sequence.5,6,9 Integrin αvβ3 is normally expressed at low levels on epithelial cells and mature endothelial cells; but it is highly expressed on the neovasculature of tumors, including osteosarcomas, glioblastomas, melanomas, lung carcinomas, and breast cancer.13–19 It has been demonstrated that integrin αvβ3 is overexpressed on both endothelial and tumor cells in human breast cancer xenografts,20 and the integrin αvβ3 expression correlates well with tumor progression and invasiveness of melanoma, glioma and breast cancers.13–20 The highly restricted expression of integrin αvβ3 during tumor growth, invasion and metastasis presents an interesting molecular target for early detection of rapidly growing and metastatic tumors.21–33 In addition, it would be highly advantageous to develop an integrin αvβ3-specific radiotracer that could be used to non-invasively visualize and quantify the integrin αvβ3 expression level before, during and/or after antiangiogenic therapy.
Over the last decade, many radiolabeled cyclic RGD peptides were evaluated as new integrin αvβ3-targeted radiotracers for imaging tumors by positron emission tomography (PET) or single photon emission computed tomography (SPECT).34–68 They have been reviewed extensively.21–33 Among the radiotracers evaluated in different pre-clinical tumor-bearing animal models, [18F]-AH111585, the core peptide sequence originally discovered from a phage display library (such as ACDRGDCFCG),69 and [18F]Galacto-RGD (2-[18F]fluoropropanamide c(RGDfK(SAA); SAA = 7-amino-L-glyero-L-galacto-2,6-anhydro-7-deoxyheptanamide) are under clinical investigations for noninvasive visualization of integrin αvβ3 expression in cancer patients.69–71 The imaging studies in cancer patients show that the 18F-labeled cyclic RGD peptides are able to target the integrin αvβ3–positive tumors. However, the low tumor uptake, high cost and lack of preparation modules for the 18F-labeled monomeric cyclic RGD peptides impose significant challenges to their continued clinical applications. To improve integrin αvβ3 binding affinity, we and others have been using multimeric cyclic RGD peptides, such as E[c(RGDfK)]2 (1) and E{E[c(RGDfK)]2}2 (2), to develop integrin αvβ3-targeted radiotracers.47–68 It was found that multimerization of cyclic RGD peptides enhances their integrin αvβ3 binding affinity and improves the radiotracer tumor uptake. However, the kidney and liver uptake of radiolabeled cyclic RGD peptides was also increased significantly as the peptide multiplicity increases.47,57–61
To solve the problem, we prepared two novel cyclic RGD peptide dimers, 3 (Figure 1: E[G3-c(RGDfK)]2) and 4 (Figure 1: G3-E[G3-c(RGDfK)]2), and their HYNIC (6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl) conjugates, 5 (HYNIC-E[G3-c(RGDfK)]2: and 6 (HYNICG3-E[G3-c(RGDfK)]2). The triglycine (G3) linkers were used for two main purposes: (1) to increase the distance between two cyclic RGD motifs from 6 bonds in 1 to 26 bonds in 3 and 4 (excluding side arms of K-residues) so that they can achieve simultaneous integrin αvβ3 binding; and (2) to improve radiotracer excretion kinetics from non-cancerous organs, such as kidneys, liver and lungs. We are particularly interested in 99mTc due to its optimal nuclear properties, easy availability and low cost.72–74 For 99mTc-labeling, HYNIC was used as a bifunctional coupling agent while tricine and TPPTS (trisodium triphenylphosphine-3,3′,3″-trisulfonate) were used as coligands to prepare 99mTc complexes 7 (Figure 1: [99mTc(5)(tricine)(TPPTS)]) and 8 (Figure 1: [99mTc(6)(tricine)(TPPTS)]). The integrin αvβ3 binding affinity of 5 and 6 was determined by competitive replacement of 125I-echistatin bound to U87MG human glioma cells. Biodistribution properties of 7 and 8 were evaluated in the athymic nude mice bearing U87MG human glioma and MDA-MB-435 breast cancer xenografts. For comparison purposes, we also evaluated cyclic RGD monomer conjugate 9 (HYNIC-G3-c(RGDfK)) and its ternary ligand 99mTc complex 10 ([99mTc(9)(tricine)(TPPTS)]) using the same in vitro and in vivo assays. Imaging studies were performed to evaluate 7 and 8 as new SPECT radiotracers for imaging integrin αvβ3-positive tumors. The main objective of this study is to demonstrate that G3 linkers are useful for enhancing integrin αvβ3 binding affinity of cyclic RGD peptide dimers, and improving the tumor uptake and excretion kinetics of their 99mTc radiotracers from non-cancerous organs. Improvement of radiotracer tumor uptake and excretion kinetics from kidneys, liver and lungs is critically important for early detection of the integrin αvβ3–positive tumors.
Figure 1.
Top: the schematic illustration of interactions between cyclic RGD peptide dimers and integrin αvβ3. A: The distance between two RGD motifs is long due to the presence of two linkers (L). As a result, the cyclic RGD dimer is able to bind integrin αvβ3 in a “bivalent” fashion. B: The distance between two RGD motifs is not long enough for simultaneous integrin αvβ3 binding. However, the RGD concentration is “locally enriched” in the vicinity of neighboring integrin αvβ3 once the first RGD motif is bound. In both cases, the end-result would be higher integrin αvβ3 binding affinity for the multimeric cyclic RGD peptides. Bottom: cyclic RGD dimers (3 and 4), their 99mTc complexes, [99mTc(5)(tricine)(TPPTS)] (7) and [99mTc(6)(tricine)(TPPTS)] (8) to be evaluated in this study.
EXPERIMENTAL SECTION
Materials and Methods
Chemicals were purchased from Sigma-Aldrich (St. Louis, MO), and were used without further purification. Cyclic RGD peptides, E[G3-c(RGDfK)]2, G3-E[G3-c(RGDfK)]2 and G3-c(RGDfK) were custom-made by the Peptides International, Inc. (Louisville, KY). Sodium succinimidyl 6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinate (HYNIC-NHS) was prepared according to literature method.75 Na99mTcO4 was obtained from a commercial DuPont Pharma 99Mo/99mTc generator (N. Billerica, MA). The ESI (electrospray ionization) mass spectral data were collected on a Finnigan LCQ classic mass spectrometer, School of Pharmacy, Purdue University. HPLC Method 1 used a LabAlliance HPLC system equipped with a UV/Vis detector (λ= 254 nm) and Zorbax C18 semi-prep column (9.4 mm × 250 mm, 100 Å pore size). The flow rate was 2.5 mL/min. The gradient mobile phase started with 95% solvent A (0.1% TFA in H2O) and 5% solvent B (0.1% TFA in CH3CN) to 60% solvent A and 40% solvent B at 25 min to 40% solvent A and 60% solvent B at 30 min. The radio-HPLC method (Method 2) used the LabAlliance HPLC system (State College, PA) equipped with a β-ram IN/US detector (IN/US System, Tampa, FL) and Zorbax C18 column (4.6 mm × 250 mm, 300 Å pore size; Agilent Technologies, Santa Clara, CA). The flow rate was 1 mL/min. The mobile phase was isocratic with 90% solvent A (25 mM NH4OAc buffer, pH = 5.0) and 10% solvent B (CH3CN) at 0 – 2 min, followed by a gradient mobile phase going from 10% solvent B at 2 min to 15% solvent B at 5 min, and 20% solvent B at 20 min.
Conjugate 5
HYNIC-NHS (10.2 mg, 24.4 μmol) and 3 (6.3 mg, 3.8 μmol) were dissolved in DMF (2 mL). After addition of triethylamine (10 mg, 10 μmol), the reaction mixture was stirred at room temperature overnight. The product was isolated from the reaction mixture by HPLC purification (Method 1). The fraction at 18.5 min was collected. Lyophilization of the collected fractions afforded 5 as a white powder. The yield was 4.0 mg (~54%) with >95% HPLC purity. ESI-MS (positive mode): m/z = 1964.43 for [M + H]+ (1962.80 calcd. for [C84H114N28O26S]+).
Conjugate 6
HYNIC-NHS (8.7 mg, 20.9 μmol) and 4 (8.1 mg, 4.4 μmol) were dissolved in anhydrous DMF (2 mL). After addition of triethylamine (10 mg, 10 μmol), the reaction mixture was stirred at room temperature overnight. The product was isolated by HPLC purification (Method 1). Fractions at 18.1 min were collected. Lyophilization of the combined collections afforded 6. The yield was 5.6 mg (~60%) with >95% HPLC purity. ESI-MS: m/z = 2136.60 for [M+H]+ (2134.89 calcd. For [C90H123N31O29S]+).
Conjugate 9
It was prepared according to the same procedure above using HYNIC-NHS (10.8 mg, 25.8 μmol) and G3-c(RGDfK) (5 mg, 6.45 μmol). Lyophilization of the collected fractions ~16.8 min (Method 1) afforded the expected conjugate 9. The yield was 3.1 mg (~45%) with HPLC purity >95%. ESI-MS: m/z = 1078.29 for [M+H]+ (1077.41 calcd. For [C46H59N15O14S]+)
99mTc-Labeling and Dose Preparation
To a lyophilized vial containing 5 mg of TPPTS, 6.5 mg of tricine, 38.5 mg of disodium succinate hexahydrate, and 12.7 mg of succinic acid, 20 μg of the cyclic RGD peptide conjugate (5, 6 and 9) was added 1.0 – 1.5 mL of Na[99mTcO4] solution (10 – 50 mCi) in saline. The vial was heated at 100 °C for 10 – 15 min in a lead-shielded water bath. After heating, the vial was placed back into the lead pig, and allowed to stand at room temperature for ~10 min. A sample of the resulting solution was analyzed by the radio-HPLC (Method 2) and ITLC. For biodistribution studies, all radiotracers were purified by HPLC (Method 2). Volatiles in the HPLC mobile phase were removed under vacuum. Doses were prepared by dissolving the purified radiotracer in saline to 20 – 30 μCi/mL. For imaging studies, doses were prepared by dissolving the radiotracer in saline to ~5 mCi/mL. For the blocking experiment, 1 was dissolved in the solution containing the radiotracer to give a concentration of 3.5 mg/mL. The resulting solution was filtered with a 0.20 micron Millex-LG filter unit before being injected into animals. Each tumor-bearing mouse was injected with 0.1 – 0.2 mL of the dose solution.
Partition Coefficient Determination
The radiotracer was purified by HPLC (Method 2). Volatiles were removed completely under vacuum. The residue was dissolved in a equal volume (3 mL:3 mL) mixture of n-octanol and 25 mM phosphate buffer (pH = 7.4). After stirring for ~20 min, the mixture was centrifuged at 8,000 rpm for 5 min. Samples (in triplets) from n-octanol and aqueous layers were counted in a Perkin Elmer Wizard – 1480 γ-counter (Shelton, CT). The log P value was reported as an average of three independent measurements plus the standard deviation.
In Vitro Whole-Cell Integrin αvβ3 Binding Assay
The in vitro integrin binding affinity and specificity of RGD peptides were assessed via a cellular competitive displacement assay using 125I-echistatin as the integrin-specific radioligand.50,52 Briefly, U87MG human glioma cells were grown in Gibco’s Dulbecco’s medium supplemented with 10% fetal bovine serum (FBS), 100 IU/ml penicillin and 100 μg/ml streptomycin (Invitrogen Co, Carlsbad, CA), at 37 °C in humidified atmosphere containing 5% CO2. Filter multiscreen DV plates were seeded with 105 glioma cells in binding buffer and incubated with 125I-echistatin in the presence of increasing concentrations of different cyclic RGD peptides. After removing the unbound 125I-echistatin, hydrophilic PVDF filters were collected and the radioactivity was determined using a gamma counter (Packard, Meriden, CT). The IC50 values were calculated by fitting the experimental data with the nonlinear regression using GraphPad Prism™ (GraphPad Software, Inc., San Diego, CA). Experiments were carried out twice with triplicate samples. The IC50 values are reported as an average of these samples plus the standard deviation.
Animal Model
Biodistribution and imaging studies were performed using the athymic nude mice bearing U87MG human glioma and MDA-MB-435 human breast cancer xenografts in compliance NIH animal experiment guidelines (Principles of Laboratory Animal Care, NIH Publication No. 86-23, revised 1985). The animal protocol for these studies has been approved by the Purdue University Animal Care and Use Committee (PACUC). U87MG glioma and MDA-MB-435 breast cancer cells were grown at 37 °C in Minimal Essential Medium (Alpha Modification) containing 3.7 g of sodium bicarbonate/L, 10% fetal bovine serum v/v, in a humidified atmosphere of 5% carbon dioxide. Female athymic nu/nu mice were purchased from Harlan (Indianapolis, IN) at 4 – 5 weeks of age. Each mouse was implanted subcutaneously with 5 × 106 tumor cells into the left and right upper flanks for the glioma model, or into the left and right mammary fat pads for the breast cancer model. In this way, one could access the impact of tumor size on the radiotracer imaging quality in a single tumor-bearing mouse. Two to four weeks after inoculation, animals with tumors in the range of 0.1 – 1.0 g were used for biodistribution and imaging studies.
Biodistribution Protocol
Twelve tumor-bearing mice (20 – 25 g) were anesthetized with intraperitoneal injection of a mixture containing Ketamine (40 – 100 mg/kg) and Xylazine (2 – 5 mg/kg). Once the animal was in surgical plane of anesthesia, the radiotracer (~2 μCi) in 0.1 mL saline was administered via tail vein. Four animals were sacrificed by sodium pentobarbital overdose (100 mg/kg) at 30, 60, and 120 min postinjection (p.i.). Blood samples were withdrawn from the heart. The tumor and normal organs (brain, eyes, spleen, lungs, liver, kidneys, muscle and intestine) were excised, washed with saline, dried with absorbent tissue, weighed, and counted on a Perkin Elmer Wizard – 1480 γ-counter (Shelton, CT). The organ uptake was calculated as a percentage of the injected dose per organ (%ID/organ) and a percentage of the injected dose per gram of organ tissue (%ID/g). For the blocking experiment, four tumor-bearing nude mice (20 – 25 g) were used, and each animal was administered with ~2 μCi of 7 along with ~350 μg (~14 mg/kg) of 1. At 1 h p.i., all four animals were sacrificed for organ biodistribution. The biodistribution data and target-to-background (T/B) ratios are reported as an average from four tumor-bearing mice at each time point plus the standard variation. Comparison between two different radiotracers was made using the two-way ANOVA test (GraphPad Prim 5.0, San Diego, CA). The level of significance was set at p < 0.05.
Scintigraphic Imaging
The athymic nude mice bearing the U87MG glioma or MDA-MB-435 breast cancer xenografts were used for scintigraphic imaging studies. Animals were anesthetized with intraperitoneal injection of sodium pentobarbital (45.0 mg/kg). Each animal was administered with 500 – 800 μCi of the radiotracer in 0.2 mL saline. Animals were placed prone on a single head mini γcamera (Diagnostic Services Inc., NJ) equipped with a parallel-hole, low-energy, and high-resolution collimator. Static images were acquired at 15, 30, 60 and 120 min p.i. and were stored digitally in a 128 × 128 matrix. The acquisition count limits were set at 500 K. After completion of the imaging study, the tumor-bearing mice were euthanized by sodium pentobarbital overdose (100 – 200 mg/kg).
Metabolism
Normal athymic nude mice were used for metabolism studies. Each mouse was administered with the 99mTc radiotracer (100 – 120 μCi). The urine samples were collected at 30 and 120 min p.i. by manual void, and were mixed with equal volume of 20% acetonitrile aqueous solution. The mixture was centrifuged at 8,000 rpm. The supernatant was collected and filtered through a 0.20 micron Millex-LG syringe-driven filter unit to remove any precipitate or particles. The filtrate was then analyzed by radio-HPLC (Method 2). The feces samples were collected at 120 min p.i. and suspended in a mixture of 20% acetonitrile aqueous solution (2 mL). The resulting mixture was vortexed for 10 min. After centrifuging at 8,000 rpm for 5 min, the supernatant was collected and passed through a 0.20 micron Millex-LG filter unit to remove any precipitate or particles. The filtrate was analyzed by radio-HPLC (Method 2).
RESULTS
Synthesis of Cyclic RGD Dimer Conjugates
Conjugates 5, 6 and 9 were prepared by direct conjugation of 3, 4 and G3-c(RGDfK), respectively, with excess HYNIC-NHS in DMF. All new conjugates were purified by HPLC (Method 1) and characterized by ESI-MS. The ESI-MS data were completely consistent with their proposed formula. Their HPLC purity of cyclic RGD dimer conjugates was >95% before being used for 99mTc-labeling and determination of their integrin αvβ3 binding affinity.
Integrin αvβ3 Binding Affinity
The integrin αvβ3 binding affinities of 5, 6 and 9 were determined by competitive displacement of 125I-echistatin on the integrin αvβ3-positive U87MG glioma cells (Figure 2). For comparison purposes, we also evaluated 11 (HYNIC-E[c(RGDfK)]2) and 12 (HYNIC-E{E[c(RGDfK)]2}2) using the same assay. IC50 values for 9, 11, 5, 6 and 12 were calculated to be 357.5 ± 8.3, 112.2 ± 20.8, 60.3 ± 4.4, 61.1 ± 2.1, and 7.2 ± 1.5 nM, respectively.
Figure 2.
In vitro competitive inhibition curves of 125I-echistatin bound to the integrin αvβ3–positive U87MG human glioma cells by 9 (■), 11 (▲), 5 (▼),6 (◆) and 12 (●). Their IC50 values were calculated to be 357.5 ± 8.3, 112.2 ± 20.8, 60.3 ± 4.4, 61.1 ± 2.1, and 7.2 ± 1.5 nM, respectively.
Radiochemistry
Complexes 7, 8 and 10 were prepared according to the literature methods.56,57 Their radiochemical purity (RCP) was >95% using the non-SnCl2 formulation.76 The specific activity was >10 Ci/μmol for all three radiotracers. They were analyzed by the reversed-phase HPLC method, and their HPLC retention times were 4.7, 9.2 and 10.5 min, respectively. All three new radiotracers were stable in the kit matrix for >12 h. It is interesting to note that complexes 7, 8 and 10 all showed a single radiometric peak in their radio-HPLC chromatograms. Since the Tc chelate is chiral, complexes [99mTc(HYNIC-BM)(tricine)(TPPTS)] (BM = biomolecule) are often formed as a 50%:50% mixture of two diastereomers if the BM moiety contains one or more chiral centers.74,77 Attempts to separate the two diastereomers in 7, 8 and 10 were not successful using the chromatographic conditions described in this study. Apparently, the presence of G3 groups makes separation of two diastereomers more difficult. We also determined the partition coefficients of 7, 8 and 10 in an equal volume mixture (3 mL:3 mL) of n-octanol and 25 mM phosphate buffer (pH = 7.4). Their Log P values were calculated to be −4.30 ± 0.03, −4.44 ± 0.05 and −4.40 ± 0.19, respectively.
Biodistribution Characteristics in Breast Cancer Model
The athymic nude mice bearing MDA-MB-435 human breast cancer xenografts were used to evaluate the biodistribution characteristics and excretion kinetics of 7 and 8. Figure 3 compares the tumor uptake and selected T/B ratios of complexes 7, 8, 13 ([99mTc(11)(tricine)(TPPTS)]) and 14 ([99mTc(12)(tricine)(TPPTS)]). The biodistribution data for 7 and 8 are listed in Tables SI and SII, and those for 13 and 14 in the same tumor-bearing animal model were obtained from our previous reports.32,58
Figure 3.
Comparison of tumor uptake and selected T/B ratios between 7, 8, 13 and 14 in athymic nude mice (n = 4) bearing MDA-MB-435 human breast cancer xenografts.
Complex 7 had the tumor uptake of 8.48 ± 0.59 %ID/g at 30 min p.i. and 9.11 ± 1.83 %ID/g at 120 min p.i. with very fast blood clearance (1.13 ± 0.21 %ID/g and 0.30 ± 0.06 %ID/g at 30 min and 120 min p.i., respectively). Its liver uptake was 4.20 ± 0.42 %ID/g at 30 min p.i. and 2.68 ± 0.46 %ID/g at 120 min p.i. As a result, the tumor/liver ratios increased steadily over the 2 h study period (1.56 ± 0.37 at 30 min p.i. and 3.09 ± 0.76 at 120 min p.i.). The kidney uptake of 7 was 20.90 ± 3.49 %ID/g and 10.74 ± 2.43 % ID/g at 30 and 120 min p.i., respectively. Its muscle uptake was 3.13 ± 1.04 %ID/g at 30 min p.i. and 1.60 ± 0.32 %ID/g at 120 min p.i. The tumor/muscle ratio for 7 was 2.84 ± 0.93 at 30 min p.i. and 5.57 ± 0.69 at 120 min p.i.
Complex 8 also had a high tumor uptake (8.34 ± 0.39 %ID/g, 7.85 ± 0.94 %ID/g and 7.60 ± 0.68 %ID/g at 30, 60, 120 min p.i., respectively) with very fast blood clearance (1.09 ± 0.20 %ID/g at 30 min p.i. and 0.38 ± 0.10 %ID/g at 120 min p.i.). The kidney uptake of 8 was 17.47 ± 2.00 %ID/g at 30 min p.i. and 8.01 ± 0.68 % ID/g at 120 min p.i. Its liver uptake was 3.28 ± 0.44 %ID/g and 2.47 ± 0.25 %ID/g at 30 and 120 min p.i., respectively. The muscle uptake of 8 was 2.33 ± 0.61 %ID/g at 30 min p.i. and 1.05 ± 0.42 %ID/g at 120 min p.i. The tumor/blood and tumor/liver ratios for 7 and 8 were almost identical within the experimental error; but the tumor/muscle ratios of 8 were better (p < 0.05) than those of 7 over the 2 h study period (Figure 3).
Blocking Experiment
The blocking experiment was used to demonstrate the integrin αvβ3 specificity. In this experiment, complex 7 was used as the radiotracer and 1 as the blocking agent at a dose of ~350 μg per mouse (or ~14 mg/kg). Figure 4 compares the selected organ uptake of 7 in the absence/presence of 1 at 60 min p.i. Co-injection of 1 resulted almost complete blockage of the tumor uptake for 7 (0.55 ± 0.04 %ID/g with 1 vs. 8.86 ± 2.23 %ID/g without 1). There was also a significant reduction in radioactivity accumulation in non-cancerous organs, such as the eyes, heart, intestine, kidneys, lungs, liver, muscle and spleen.
Figure 4.
Comparison of organ uptake for 7 at 60 min p.i. in the absence/presence of excess 1. Each data point represents an average of biodistribution data in four animals.
Biodistribution Characteristics in Glioma Model
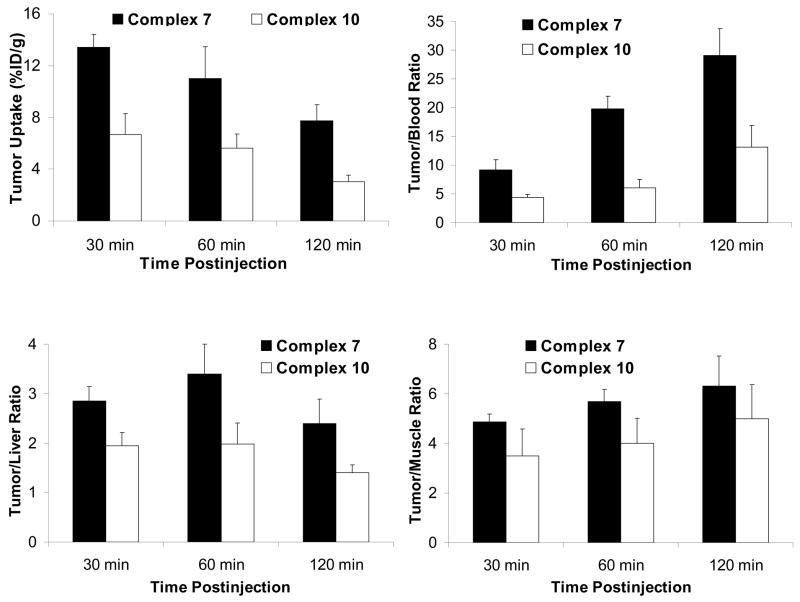
To further confirm our findings from the MDA-MB-435 breast cancer model, we also evaluated the biodistribution properties of 7 and 10 using athymic nude mice bearing U87MG glioma xenografts. The tumor size in these two tumor-bearing models was very close (0.1 – 0.5 g). Results from these studies will allow us to demonstrate the superiority of 7 over 10, and to compare the tumor uptake of 7 in two different tumor-bearing animal models. Figure 5 compares their tumor uptake and T/B ratios. Detailed biodistribution data for 7 and 10 are summarized in Tables SIII and SIV.
Figure 5.
Direct comparison of tumor uptake and selected T/B ratios between 7 and 10 in the athymic nude mice (n = 4) bearing U87MG human glioma xenografts.
In general, the normal organ uptake of 7 in the glioma-bearing mice was identical to that in those obtained in the breast cancer model. The tumor uptake of 7 was 13.43 ± 0.98 %ID/g, 11.02 ± 2.34 %ID/g and 7.74 ± 1.25 %ID/g at 30, 60, 120 min p.i., respectively, which were more than twice of that for 10 (6.70 ± 1.59 %ID/g, 5.62 ± 1.12 %ID/g and 3.03 ± 0.54 %ID/g at 30, 60, and 120 min p.i., respectively). As a result, 7 had the tumor/blood ratios (9.19 ± 1.79 at 30 min p.i. and 29.02 ± 4.68 at 120 min p.i.) and tumor/liver ratios (2.85 ± 0.29 at 30 min p.i. and 2.39 ± 0.50 at 120 min p.i.) that were significantly better (p < 0.01) than those of 10 (tumor/blood ratio = 4.42 ± 0.40 at 30 min p.i. and 13.08 ± 3.84 at 120 min p.i.; and tumor/liver ratio = 1.95 ± 0.62 at 30 min p.i. and 1.40 ± 0.16 at 120 min p.i.). The kidney uptake of 10 (10.88 ± 2.02 %ID/g at 30 min p.i. and 3.75 ± 0.48 % ID/g at 120 min p.i., respectively) was than half of that for 7 (23.33 ± 2.78 %ID/g at 30 min p.i. and 9.99 ± 0.61 %ID/g at 120 min p.i.). The muscle uptake of 10 (1.89 ± 0.42 %ID/g at 30 min p.i. and 0.64 ± 0.11 %ID/g at 120 min p.i.) was also significantly lower than that of 7 (2.72 ± 0.33 %ID/g at 30 min p.i. and 1.25 ± 0.10 %ID/g at 120 min p.i.).
Effect of Tumor Size
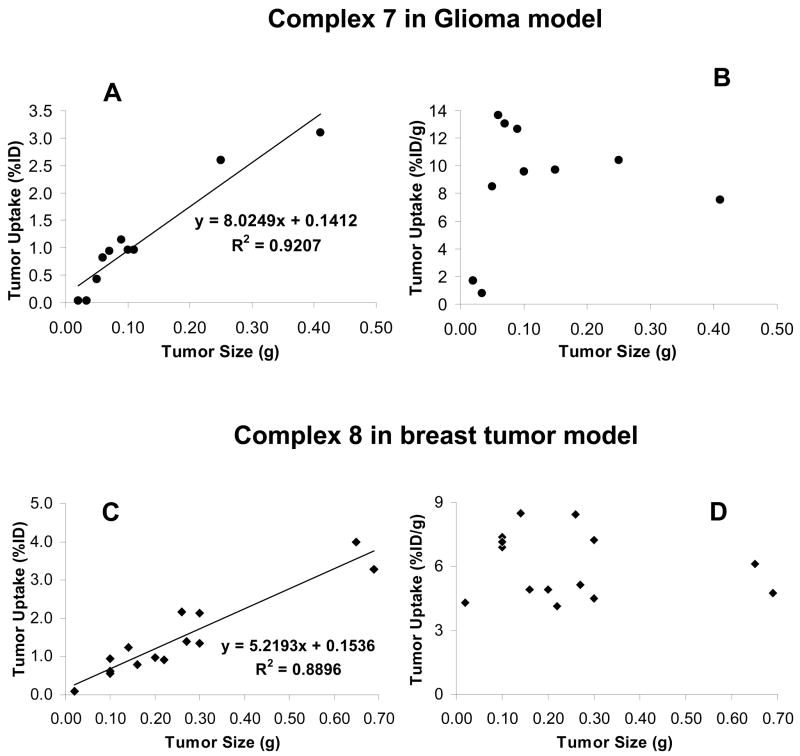
During biodistribution studies, we noticed that there is often a large variation in tumor size even if the same number of U87MG glioma cells were used for the same animal. Smaller tumors (< 0.5 g) tend to have higher radiotracer uptake than large tumors regardless of the identity of radiotracer. To clarify the relationship between the radiotracer tumor uptake and tumor size, we added extra glioma-bearing mice into the 120 min group for 7 and breast tumor-bearing mice for 8. Figure 6 shows the relationship between the tumor size and tumor uptake of 7 and 8. In the glioma model, there is a linear relationship between the tumor size (0.02 – 0.7 g; n = 10) and the %ID tumor uptake of 7 with R2 = 0.9207 (Figure 6A). As tumor size increases, the %ID tumor uptake also increases. If the tumor uptake is expressed as %/ID/g (Figure 6B), it seems that 7 has a narrow window to achieve the optimal %ID/g tumor uptake. When the tumor size is in the range of 0.1 g – 0.25 g, 7 has the tumor uptake between 8.0 %ID/g and 14 %ID/g. When the tumor size is too large (>0.4 g), its tumor uptake is <8.0 %ID/g. When the tumor size is too small (<0.05 g), its tumor uptake is less than 2.0 %ID/g. The linear relationship between tumor size (0.03 – 0.7 g; n = 14) and the radiotracer %ID tumor uptake was also observed for 8 with R2 = 0.8896 (Figure 6C) in the breast cancer model. However, the distribution pattern of the %ID/g tumor uptake relative to the tumor size was more scattered for 8 as compared to that for 7 in the glioma model (Figure 6D). Apparently, the radiotracer tumor uptake (expressed as %ID and %ID/g) is dependent not only on the tumor size but also on the tumor type.
Figure 6.
The relationship between tumor size and tumor uptake expressed as %ID (left) and %ID/g (right) for 7 at 120 min p.i. in the athymic nude mice bearing the U87MG glioma xenografts (n = 5 and tumor number = 10), and for 8 at 120 min p.i. in the athymic nude mice bearing the MDA-MB-435 xenografts (n = 7 and tumor number = 14).
Metabolic Properties
We studied the metabolic stability of 7, 8 and 10 using normal athymic nude mice. Two animals were used for each 99mTc radiotracer. Figure SI shows typical radio-HPLC chromatograms of 7 in saline, in urine at 30 and 120 min p.i., and in feces at 120 min p.i. There were no metabolites detectable for 7 in the urine and feces samples over 2 h study period. Similar metabolic stability was also observed for 8 (Figure SII) and 10 (Figure SIII).
Planar Imaging
Figure 7 shows static images of the athymic nude mice bearing U87MG glioma and MDA-MB435 breast cancer xenografts, respectively, at 15, 30, 60 and 120 min p.i. All tumors were clearly visualized as early as 15 min p.i. with excellent contrast. No significant activity accumulation was detected in the liver and lungs. We also examined tumor detectability using 8 as the radiotracer. Figure 8 compares the 60 min static images of the tumor-bearing mice (U87MG glioma xenografts with tumor size in the range 0.10 g – 0.80 g) administered with 8. It was found that the tumors of ~5 mm in diameter could be readily visualized as soon as 8 was injected. Larger tumors (>0.45 g) had much better visualization than smaller ones (~0.1 g).
Figure 7.
Top: static images of the tumor-bearing mice (U87MG glioma xenografts) administered with ~1 mCi of 7 at 15, 30, 60 and 120 min p.i. Bottom: static images of the tumor-bearing mice (MDA-MB435 breast cancer xenografts) administered with ~1 mCi of 8 at 15, 30, 60 and 120 min p.i. Arrows indicate the presence of tumors.
Figure 8.
The 60 min static images of 8 in the athymic nude mice with different tumor sizes (0.10 g – 0.80 g or 100 – 800 mm3).
DISCUSSION
For a new integrin αvβ3-targeted radiotracer to be successful, it must show clinical indications for high-incidence tumor types, such as breast, prostate, colorectal and lung cancers. The radiotracer should be able to have high tumor uptake with diagnostically useful T/B ratios in a short period of time (preferably <2 h p.i.). The radiotracer must be prepared in high yield and radiochemical purity with very high specific activity. In addition, it should be readily available at low cost for the radiotracer to assume a wide-spread clinical utility. Although PET imaging studies clearly show that the 18F-labeled cyclic RGD monomers are able to localize the integrin αvβ3–positive tumors in cancer patients,69–71 the relatively low tumor uptake, very high cost and lack of preparative modules for the 18F-labeled RGD peptides will severely limit their clinical utilities for non-invasive imaging of integrin αvβ3 expression in cancer patients. Therefore, there is a continuing need for the integrin αvβ3–targeted radiotracer that can be readily prepared in high radiochemical purity with high specific activity. The 99mTc-labeled cyclic RGD peptide dimers described in this study satisfy this need due to the optimal nuclear properties, easy availability and low cost of 99mTc,72–74 the non-SnCl2 formulation for routine clinical preparations of 99mTc-labeled cyclic RGD dimers, and their excellent biodistribution characteristics and excretion kinetics from non-cancerous organs, particularly liver and kidneys.
In this study, we have successfully prepared two cyclic RGD dimer conjugates (5 and 6). Their ternary ligand 99mTc complexes 7 and 8 were prepared in high yield (RCP >95%) and with high specific activity (> 10 Ci/μmol) using the non-SnCl2 kit formulation. They were stable in the kit matrix for more than 6 h. In this respect, 7 and 8 offer significant advantages over the 18F-labeled cyclic RGD peptide radiotracers, which often require several steps of radio-synthesis and tedious post-labeling chromatographic purification. Manual radio-synthesis and post-labeling chromatographic purification impose significant radiation exposure to radiopharmacists.
The integrin αvβ3 binding affinities against 125I-echistatin follow the order of 12 (IC50 = 7.2 ± 1.5 nM) ≫ 5 (IC50 = 60.3 ± 4.4 nM) ~ 6 (IC50 = 61.1 ± 2.1 nM) > 11 (IC50 = 112.2 ± 20.8 nM) ≫ 9 (IC50 = 357.5 ± 8.3 nM). The addition of G3 linkers between two cyclic RGD motifs is responsible for the improved integrin αvβ3 binding affinity of 5 and 6. However, the addition of an extra G3 linker between HYNIC and 3 had little impact on integrin αvβ3 binding affinity. It must be noted that the IC50 value depends largely on the radioligand (125I-echistatin vs. 125I-c(RGDyK)) and tumor cell lines (U87MG vs. MDA-MB-435) used in the in vitro competition assay. Caution should be taken when comparing the IC50 values of cyclic RGD peptides with those reported in the literature.
The distance between the two cyclic RGD motifs is 6 bonds in 11 and 26 bonds in 5 excluding side arms of K-residues. The higher integrin αvβ3 binding affinity of 5 (IC50 = 60.3 ± 4.4 nM) than that of 11 (IC50 = 112.2 ± 20.8 nM) suggests that 5 is bivalent in binding to the integrin αvβ3 (Figure 1A), and the distance between two cyclic RGD motifs in 11 is probably too short for simultaneous integrin αvβ3 binding (Figure 1B). This conclusion is supported by the higher tumor uptake of 7 (8.48 ± 0.59 %ID/g at 30 min p.i. and 9.11 ± 1.83 %ID/g at 120 min p.i.) than that of 13 (3.49 ± 0.62 %ID/g at 30 min p.i. and 3.82 ± 0.54 %ID/g at 120 min p.i.) in the same animal model.57,60 If they were bivalent in binding to integrin αvβ3, 5 and 11 would have had the same integrin αvβ3 binding affinity, whereas 7 and 13 would have had similar tumor uptake. Even though 11 is not bivalent, the binding of one RGD motif may significantly increase the local RGD concentration in the vicinity of neighboring integrin αvβ3 sites. This may explain why 11 (IC50 = 112.2 ± 20.8 nM) has higher integrin αvβ3 affinity than 9 (IC50 = 357.5 ± 8.3 nM), and the radiolabeled cyclic RGD dimers have better tumor uptake than their monomeric analogs.50–54,56–68 Therefore, 3 and 4 are better targeting biomolecules than 1 for the future development of integrin αvβ3-targeted radiotracers.
In 12, there are four identical cyclic RGD motifs. The longest distance between two adjacent RGD motifs is 16 bonds (excluding side arms of K-residues). The integrin αvβ3 binding affinity of 12 (IC50 = 7.2 ± 1.5 nM) is much higher than those of 11 (IC50 = 112.2 ± 20.8 nM) and 5 (IC50 = 60.3 ± 4.4 nM). On the basis of these results, one might suggest that the higher tumor uptake of 14 (5.78 ± 0.67 %ID/g at 30 min p.i. and 7.30 ± 1.32 %ID/g at 120 min p.i.) than that of 9 (3.49 ± 0.62 %ID/g at 30 min p.i. and 3.82 ± 0.54 %ID/g at 120 min p.i.) is most likely caused by a combination of the simultaneous integrin αvβ3 binding of two adjacent RGD motifs and the presence of four cyclic RGD motifs in 12.60 The lower tumor uptake for 14 (5.78 ± 0.67 %ID/g at 30 min p.i. and 7.30 ± 1.32 %ID/g at 120 min p.i.) than that of 7 (8.48 ± 0.59 %ID/g at 30 min p.i. and 9.11 ± 1.83 %ID/g at 120 min p.i.) is probably caused by the tumor size difference during biodistribution studies.
Complex 7 has significant advantages over 14 with respect to radioactivity accumulation in non-cancerous organs. For example, the liver uptake of 7 (2.68 ± 0.46 %ID/g at 120 min p.i.) was lower (p < 0.01) than that of 14 (4.09 ± 0.59 %ID/g at 120 min p.i.). Its tumor/liver ratios (2.85 ± 0.29 and 2.39 ± 0.50 at 30 and 120 min p.i., respectively) are better (p < 0.01) than those for 14 (1.25 ± 0.27 and 1.78 ± 0.27 at 30 and 120 min p.i., respectively). The tumor/muscle ratios of 7 (2.84 ± 0.93 at 30 min p.i. and 5.57 ± 0.69 at 120 min p.i.) are much better (p < 0.01) than those of 9 (1.44 ± 0.25 at 30 min p.i. and 3.28 ± 0.32 %ID/g at 120 min p.i.),32 and 14 (2.50 ± 0.70 %ID/g at 30 min p.i. and 3.69 ± 0.96 %ID/g at 120 min p.i.).58 The kidney uptake of 7 (10.74 ± 2.43 % ID/g at 120 min p.i.) is less than half of that of 10 (25.93 ± 2.52 %ID/g at 120 min p.i.). The higher kidney uptake of 14 is most likely caused by the presence of four R-residues in 14 as compared to two R-residues in 5. Thus, 3 and 4 are better targeting biomolecules than 2 for the future development of integrin αvβ3-targeted radiotracers.
Complex 8 has the tumor uptake (%ID/g), tumor/blood and tumor/liver ratios comparable to those of 7 (Figure 3); but its tumor/muscle ratios are significantly better (p < 0.01) than those of 7 over the 2 h period. Since the tumor uptake of 7 is almost completely blocked by co-injection of excess 1 (Figure 4), we believe that its tumor uptake is integrin αvβ3-mediated. The uptake blockage in eyes, heart, intestine, kidneys, lungs, liver and spleen suggests that the uptake of 7 in these organs is at least partially integrin αvβ3-mediated. This conclusion is supported by the immunohistopathological studies,53,54 which showed a strong positive staining of endothelial cells of the small glomeruli vessels in kidneys and weak staining in the branches of the hepatic portal vein.
The glioma uptake of 7 (13.43 ± 0.98 %ID/g at 30 min p.i. and 11.02 ± 2.34 %ID/g at 60 min p.i.) is significantly higher (p < 0.01) than its breast tumor uptake (8.48 ± 0.59 %ID/g at 30 min p.i. and 7.86 ± 2.23 %ID/g at 60 min p.i.). This seems consistent with the fact that the U87MG glioma cells have a higher level of integrin αvβ3 expression than MDA-MB-435 breast tumor cells.53,54 However, this difference disappears at 120 min p.i. (7.74 ± 1.25 %ID/g in glioma-bearing mice and 9.11 ± 1.83 %ID/g in breast tumor-bearing mice). At this moment, it is unclear why the uptake of 7 increases in the breast tumor while it decreases in the glioma.
Non-invasive imaging of molecular markers, such as integrin αvβ3, is highly desirable for patient selection before anti-angiogenic treatment and for more effective monitoring of therapeutic efficacy in the integrin αvβ3-positive cancer patients. The %ID tumor uptake reflects the integrin αvβ3 expression level on both tumor cells and endothelial cells of the tumor neovasculature. The %ID/g tumor uptake reflects the integrin αvβ3 density. When tumor is small (<0.05 g or 50 mm3), there is little angiogenesis with low blood flow and low integrin αvβ3 expression. As a result, the %ID and %ID/g tumor uptake values of 7 are low in the glioma model (Figure 6: A and B). When tumors are in their rapid growing stage (0.1 – 0.5 g or 100 – 500 mm3), the microvessel and integrin αvβ3 density is high. Its %ID/g tumor uptake is high (Figure 6B). As tumors grow, the total integrin αvβ3 level is increased, and the %ID tumor uptake increases (Figure 6A). In contrast, the microvessel density decreases due to maturity of blood vessels, and so is the integrin αvβ3 density due to larger interstitial space.78 In addition, parts of the tumor may become necrotic, leading to lower integrin αvβ3 density in larger tumors. As a result, the %ID/g tumor uptake of 7 in larger tumors (>0.5 g or 500 mm3) is lower than that of smaller ones (Figure 6B). In the breast tumor model, there is also a linear relationship between the tumor size and %ID tumor uptake of 8 (Figure 6C). However, its %ID/g tumor uptake values are more scattered as the tumor size changes (Figure 6D). The radiotracer tumor uptake depends not only on the tumor size but also on the tumor type. The linear relationship between the tumor size and the radiotracer %ID tumor uptake suggests that both 7 and 8 are useful for non-invasive monitoring of the tumor integrin αvβ3 expression.
Tumors must have sufficient radioactivity counts to be detectable. In this study, we found that tumors of >5 mm in diameter could be visualized with excellent contrast as early as 15 min postinjection of 7 and 8 (Figure 7). The most visible organs at 120 min p.i. are tumors, kidneys and bladder. Larger tumors have much better visualization than the smaller ones (Figure 8). The tumor detection limit is ~5 mm in diameter using a modified clinical SPECT camera. With the newer high resolution SPECT cameras or SPECT/CT, the tumor detection limit might be significantly lower using 7 and 8 as radiotracers. Both 7 and 8 are useful for early detection of integrin αvβ3–positive tumors.
Extensive metabolic degradation was observed for the 99mTc-labeled cyclic RGD monomer,35 dimer,57,58 tetramer,60,61 and the 64Cu-labeled RGD tetramer in kidneys and urine samples.54 However, the metabolism study shows that both 7 and 8 remain intact during their excretion from renal and hepatobiliary routes. It is unclear why 7 and 8 have such a high metabolic stability during excretion from renal and hepatobiliary routes (Figures SI and SIII) while 13 and 14 undergo extensive metabolism during excretion from the hepatobiliary route.
CONCLUSION
In summary, we have successfully prepared two new cyclic RGD peptide conjugates: 5 and 6, and evaluated complexes 7 and 8 as radiotracers for imaging integrin αvβ3 expression in athymic nude mice bearing U87MG glioma and MDA-MB-435 breast cancer xenografts. The results from this study clearly show that the G3 linkers between two cyclic RGD motifs in cyclic RGD dimers are useful for enhancing their integrin αvβ3 binding affinity, and for improving the tumor uptake and clearance kinetics of their corresponding 99mTc radiotracers from non-cancerous organs. In addition, 8 is readily prepared in high yield (RCP > 95%) and high specific activity (>10 Ci/μmol). Complex 8 offers significant advantages over the 18F-labeled RGD peptides with respect to cost, availability and easiness of routine preparation. Therefore, 8 is a very attractive radiotracer for the early detection of integrin αvβ3–positive tumors, and may have potential applications for non-invasive monitoring of tumor growth or shrinkage during antiangiogenic treatment.
Supplementary Material
Detailed biodistribution data and T/B ratios for 99mTc-labeled cyclic RGD peptides are listed in Tables SI – SVI. Figures SI – SIII illustrate typical radio-HPLC chromatograms of 7, 8 and 10, respectively, in saline before injection, in the urine at 30 min p.i., in the urine at 120 min p.i., and in the feces at 120 min p.i. This information is available free of charge via Internet at http://pubs.acs.org.
Acknowledgments
Authors would like to thank Dr. Sulma I. Mohammed, the Director of Purdue Cancer Center Drug Discovery Shared Resource, Purdue University, for her assistance with the tumor-bearing animal model. This work is supported, in part, by Purdue University and research grants: R01 CA115883 A2 (S.L.) from National Cancer Institute (NCI), R21 HL083961-01 from National Heart, Lung, and Blood Institute (NHLBI), and DE-FG02-08ER64684 from the Department of Energy.
ABBREVIATIONS
- E[c(RGDfK)]2
Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)-cyclo(Lys-Arg-Gly-Asp-D-Phe)]
- E[G3-c(RGDfK)]2
Glu{cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]-cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}
- G3-E[G3-c(RGDfK)]2
(Gly-Gly-Gly)-Glu{cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}-cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}
- E{E[c(RGDfK)]2}2
Glu{Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)]-cyclo(Lys-Arg-Gly-Asp-D-Phe)}-{Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)]-cyclo(Lys-Arg-Gly-Asp-D-Phe)}
- HYNIC
6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl
- HYNIC-E[c(RGDfK)]2
6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl-Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)-cyclo(Lys-Arg-Gly-Asp-D-Phe)]
- HYNIC-E[G3-c(RGDfK)]2
6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl-Glu{cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]-cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}
- HYNIC-G3-E[G3-c(RGDfK)]2
6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl-(Gly-Gly-Gly)-Glu{cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}-cyclo[Lys(Gly-Gly-Gly)-Arg-Gly-Asp-D-Phe]}
- HYNIC-E{E[c(RGDfK)]2}2
6-(2-(2-sulfonatobenzaldehyde)hydrazono)nicotinyl-Glu{Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)]-cyclo(Lys-Arg-Gly-Asp-D-Phe)}-{Glu[cyclo(Lys-Arg-Gly-Asp-D-Phe)]-cyclo(Lys-Arg-Gly-Asp-D-Phe)}
- TPPTS
trisodium triphenylphosphine-3,3′,3″-trisulfonate
References
- 1.Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995;1:27–31. doi: 10.1038/nm0195-27. [DOI] [PubMed] [Google Scholar]
- 2.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002;29:15–18. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 3.Mousa SA. Mechanisms of angiogenesis in vascular disorders: potential therapeutic targets. Drugs of the Future. 1998;23:51–60. [Google Scholar]
- 4.Mousa SA. Integrins as novel drug discovery targets: potential therapeutic and diagnostic implications. Emerging Therapeutic Targets. 2000;4:143–153. doi: 10.1016/s1367-5931(02)00350-2. [DOI] [PubMed] [Google Scholar]
- 5.Carmeliet P. Mechanism of angiogenesis and atheriogenesis. Nat Med. 2000;6:389–395. doi: 10.1038/74651. [DOI] [PubMed] [Google Scholar]
- 6.Bögler O, Mikkelsen T. Angiogenesis in Glioma: molecular mechanisms and roadblocks to translation. Cancer J. 2003;9:205–213. doi: 10.1097/00130404-200305000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Hwang R, Varner JV. The role of integrins in tumor angiogenesis. Hematol Oncol Clin North Am. 2004;18:991–1006. doi: 10.1016/j.hoc.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Jin H, Varner J. Integrins: roles in cancer development and as treatment targets. Br J Cancer. 2004;90:561–565. doi: 10.1038/sj.bjc.6601576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar CC. Integrin αvβ3 as a therapeutic target for blocking tumor-induced angiogenesis. Curr Drug Targets. 2003;4:123–131. doi: 10.2174/1389450033346830. [DOI] [PubMed] [Google Scholar]
- 10.Brooks PC, Clark RAF, Cheresh DA. Requirement of vascular integrin αvβ3 for angiogenesis. Science. 1994;264:569–571. doi: 10.1126/science.7512751. [DOI] [PubMed] [Google Scholar]
- 11.Friedlander M, Brooks PC, Shatter RW, Kincaid CM, Varner JA, Cheresh DA. Definition of two angiogenic pathways by distinct αv integrin. Science. 1995;270:1500–1502. doi: 10.1126/science.270.5241.1500. [DOI] [PubMed] [Google Scholar]
- 12.Horton MA. The αvβ3 integrin “vitronectin receptor”. Int J Biochem Cell Biol. 1997;29:721–725. doi: 10.1016/s1357-2725(96)00155-0. [DOI] [PubMed] [Google Scholar]
- 13.Bello L, Francolini M, Marthyn P, Zhang JP, Carroll RS, Nikas DC, Strasser JF, Villani R, Cheresh DA, Black PM. Alpha(v)beta3 and alpha(v)beta5 integrin expression in glioma periphery. Neurosurgery. 2001;49:380–389. doi: 10.1097/00006123-200108000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Meitar D, Crawford SE, Rademaker AW, Cohn SL. Tumor angiogenesis correlates with metastatic disease, N-myc-amplification, and poor outcome in human neuroblastoma. J Clinical Oncol. 1996;14:405–414. doi: 10.1200/JCO.1996.14.2.405. [DOI] [PubMed] [Google Scholar]
- 15.Gasparini G, Brooks PC, Biganzoli E, Vermeulen PB, Bonoldi E, Dirix LY, Ranieri G, Miceli R, Cheresh DA. Vascular integrin αvβ3: a new prognostic indicator in breast cancer. Clin Cancer Res. 1998;4:2625–2634. [PubMed] [Google Scholar]
- 16.Albelda SM, Mette SA, Elder DE, Stewart RM, Damjanovich L, Herlyn M, Buck CA. Integrin distribution in maliganant melanoma: association of the beta3 subunit with tumor progression. Cancer Res. 1990;50:6757–6764. [PubMed] [Google Scholar]
- 17.Falcioni R, Cimino L, Gentileschi MP, D’Agnano I, Zupi G, Kennel SJ, Sacchi A. Expression of beta 1, beta 3, beta 4, and beta 5 integrins by human lung carcinoma cells of different histotypes. Exp Cell Res. 1994;210:113–122. doi: 10.1006/excr.1994.1017. [DOI] [PubMed] [Google Scholar]
- 18.Sengupta S, Chattopadhyay N, Mitra A, Ray S, Dasgupta S, Chatterjee A. Role of αvβ3 integrin receptors in breast tumor. J Exp Clin Cancer Res. 2001;20:585–590. [PubMed] [Google Scholar]
- 19.Felding-Habermann B, Mueller BM, Romerdahl CA, Cheresh DA. Involvement of integrin alpha V gene expression in human melanoma tumorigenicity. J Clin Invest. 1992;89:2018–2022. doi: 10.1172/JCI115811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zitzmann S, Ehemann V, Schwab M. Arginine-Glycine-Aspartic acid (RGD)-peptide binds to both tumor and tumor endothelial cells in vivo. Cancer Res. 2002;62:5139–5143. [PubMed] [Google Scholar]
- 21.Weber WA, Haubner R, Vabuliene E, Kuhnast B, Webster HJ, Schwaiger M. Tumor angiogenesis targeting using imaging agents. Q J Nucl Med. 2001;45:179–182. [PubMed] [Google Scholar]
- 22.Costouros NG, Diehn FE, Libutti SK. Molecular imaging of tumor angiogenesis. J Cell Biochem Suppl. 2002;39:72–78. doi: 10.1002/jcb.10426. [DOI] [PubMed] [Google Scholar]
- 23.Liu S, Edwards DS. Fundamentals of receptor-based diagnostic metalloradiopharmaceuticals. Topics in Current Chem. 2002;222:259–278. [Google Scholar]
- 24.Van de Wiele C, Oltenfreiter R, De Winter O, Signore A, Slegers G, Dieckx RA. Tumor angiogenesis pathways: related clinical issues and implications for nuclear medicine imaging. Eur J Nucl Med. 2002;29:699–709. doi: 10.1007/s00259-002-0783-8. [DOI] [PubMed] [Google Scholar]
- 25.Liu S, Robinson SP, Edwards DS. Integrin αvβ3 directed radiopharmaceuticals for tumor imaging. Drugs of the Future. 2003;28:551–564. [Google Scholar]
- 26.McDonald DM, Choyke P. Imaging Angiogenesis: from microscope to clinic. Nature Med. 2003;9:713–725. doi: 10.1038/nm0603-713. [DOI] [PubMed] [Google Scholar]
- 27.Haubner R, Wester HR. Radiolabeled tracers for imaging of tumor angiogenesis and evaluation of anti-angiogenic therapies. Curr Pharm Des. 2004;10:1439–1455. doi: 10.2174/1381612043384745. [DOI] [PubMed] [Google Scholar]
- 28.Liu S, Robinson SP, Edwards DS. Radiolabeled integrin αvβ3 antagonists as radiopharmaceuticals for tumor radiotherapy. Topics in Current Chem. 2005;252:117–153. [Google Scholar]
- 29.Chen X. Multimodality imaging of tumor integrin αvβ3 expression. Mini-Rev Med Chem. 2006;6:227–234. doi: 10.2174/138955706775475975. [DOI] [PubMed] [Google Scholar]
- 30.D’Andrea LD, Del Gatto A, Pedone C, Benedetti E. Peptide-based molecules in angiogenesis. Chem Biol Drug Des. 2006;67:115–126. doi: 10.1111/j.1747-0285.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- 31.Meyer A, Auremheimer J, Modlinger A, Kessler H. Targeting RGD recognizing integrins: drug development, biomaterial research, tumor imaging and targeting. Curr Pharm Design. 2006;12:2723–2747. doi: 10.2174/138161206777947740. [DOI] [PubMed] [Google Scholar]
- 32.Liu S. Radiolabeled multimeric cyclic RGD peptides as integrin αvβ3-targeted radiotracers for tumor imaging. Mol Pharm. 2006;3:472–487. doi: 10.1021/mp060049x. [DOI] [PubMed] [Google Scholar]
- 33.Cai W, Chen X. Multimodality imaging of tumor angiogenesis. J Nucl Med. 2008;49:113S–128S. doi: 10.2967/jnumed.107.045922. [DOI] [PubMed] [Google Scholar]
- 34.Huabner R, Wester HJ, Senekowitsch-Schmidtke R, Diefenbach B, Kessler H, Stöcklin G, Schwaiger M. RGD-peptides for tumor targeting: biological evaluation of radioiodinated analogs and introduction of a novel glycosylated peptide with improved biokinetics. J Labelled Compounds & Radiopharmaceuticals. 1997;40:383–385. [Google Scholar]
- 35.Haubner R, Bruchertseifer F, Bock M, Schwaiger M, Wester HJ. Synthesis and biological evaluation of 99mTc-labeled cyclic RGD peptide for imaging integrin αvβ3 expression. Nuklearmedizin. 2004;43:26–32. doi: 10.1267/nukl04010026. [DOI] [PubMed] [Google Scholar]
- 36.Haubner R, Wester HJ, Reuning U, Senekowisch-Schmidtke R, Diefenbach B, Kessler H, Stöcklin G, Schaiger M. Radiolabeled αvβ3 integrin antagonists: a new class of tracers for tumor imaging. J Nucl Med. 1999;40:1061–1071. [PubMed] [Google Scholar]
- 37.Sivolapenko GB, Skarlos D, Pectasides D, Stathopoulou E, Milonakis A, Sirmalis G, Stuttle A, Courtenay-Luck NS, Konstantinides K, Epenetos AA. Imaging of metastatic melanoma utilizing a technetium-99m labeled RGD-containing synthetic peptide. Eur J Nucl Med. 1998;25:1383–1389. doi: 10.1007/s002590050312. [DOI] [PubMed] [Google Scholar]
- 38.Haubner R, Wester HJ, Burkhart F, Senekowisch-Schmidtke R, Weber W, Goodman SL, Kessler H, Schwaiger M. Glycolated RGD-containing peptides: tracer for tumor targeting and angiogenesis imaging with improved biokinetics. J Nucl Med. 2001;42:326–336. [PubMed] [Google Scholar]
- 39.Haubner R, Wester HJ, Weber WA, Mang C, Ziegler SI, Goodman SL, Senekowisch-Schmidtke R, Kessler H, Schwaiger M. Noninvasive imaging of αvβ3 integrin expression using 18F-labeled RGD-containing glycopeptide and positron emission tomography. Cancer Res. 2001;61:1781–1785. [PubMed] [Google Scholar]
- 40.Thumshirn G, Hersel U, Goodman SL, Kessler H. Multimeric cyclic RGD peptides as potential tools for tumor targeting: solid-phase peptide synthesis and chemoselective oxime ligation. Chem Eur J. 2003;9:2717–2725. doi: 10.1002/chem.200204304. [DOI] [PubMed] [Google Scholar]
- 41.Poethko T, Schottelius M, Thumshirn G, Herz M, Haubner R, Henriksen G, Kessler H, Schwaiger M, Wester HJ. Chemoselective pre-conjugate radiohalogenation of unprotected mono- and multimeric peptides via oxime formation. Radiochim Acta. 2004;92:317–327. [Google Scholar]
- 42.Poethko T, Schottelius M, Thumshirn G, Hersel U, Herz M, Henriksen G, Kessler H, Schwaiger M, Wester HJ. Two-step methodology for high yield routine radiohalogenation of peptides: 18F-labeled RGD and octreotide analogs. J Nucl Med. 2004;45:892–902. [PubMed] [Google Scholar]
- 43.Alves S, Correia JDG, Gano L, Rold TL, Prasanphanich A, Haubner R, Rupprich M, Alberto R, Decristoforo C, Snatos I, Smith CJ. In vitro and in vivo evaluation of a novel 99mTc(CO)3-pyrazolyl conjugate of cyclo-(Arg-Gly-Asp-D-Tyr-Lys) Bioconj Chem. 2007;18:530–537. doi: 10.1021/bc060234t. [DOI] [PubMed] [Google Scholar]
- 44.Fani M, Psimadas D, Zikos C, Xanthopoulos S, Loudos GK, Bouziotis P, Varvarigou AD. Comparative evaluation of linear and cyclic 99mTc-RGD peptides for targeting of integrins in tumor angiogenesis. Anticancer Res. 2006;26:431–434. [PubMed] [Google Scholar]
- 45.Su ZF, Liu G, Gupta S, Zhu Z, Rusckowski M, Hnatowich DJ. In vitro and in vivo evaluation of a technetium-99m-labeled cyclic RGD peptide as specific marker of αvβ3 integrin for tumor imaging. Bioconj Chem. 2002;13:561–570. doi: 10.1021/bc0155566. [DOI] [PubMed] [Google Scholar]
- 46.Decristoforo C, Faintuch-Linkowski B, Rey A, vo Guggenberg E, Rupprich M, Hernandez-Gonzales I, Rodrigo T, Haubner R. [99mTc]HYNIC-RGD for imaging integrin αvβ3 expression. Nucl Med Biol. 2006;33:945–952. doi: 10.1016/j.nucmedbio.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 47.Chen X, Park R, Tohme M, Shahinian AH, Bading JR, Conti PS. MicroPET and autoradiographic imaging of breast cancer αv-integrin expression using 18F- and 64Cu-labeled RGD peptide. Bioconj Chem. 2004;15:41–49. doi: 10.1021/bc0300403. [DOI] [PubMed] [Google Scholar]
- 48.Chen X, Park R, Shahinian AH, Tohme M, Khankaldyyan V, Bozorgzadeh MH, Bading JR, Moats R, Laug WE, Conti PS. 18F-labeled RGD peptide: initial evaluation for imaging brain tumor Angiogenesis. Nucl Med Biol. 2004;31:179–189. doi: 10.1016/j.nucmedbio.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 49.Chen X, Park R, Shahinian AH, Bading JR, Conti PS. Pharmacokinetics and tumor retention of 125I-labeled RGD peptide are improved by PEGylation. Nucl Med Biol. 2004;31:11–19. doi: 10.1016/j.nucmedbio.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 50.Chen X, Liu S, Hou Y, Tohme M, Park R, Bading JR, Conti PS. MicroPET imaging of breast cancer αv-integrin expression with 64Cu-labeled dimeric RGD peptides. Mol Imag Biol. 2004;6:350–359. doi: 10.1016/j.mibio.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 51.Chen X, Tohme M, Park R, Hou Y, Bading JR, Conti PS. MicroPET imaging of breast cancer αv-integrin expression with 18F-labeled dimeric RGD peptide. Mol Imaging. 2004;3:96–104. doi: 10.1162/15353500200404109. [DOI] [PubMed] [Google Scholar]
- 52.Wu Y, Zhang X, Xiong Z, Cheng Z, Fisher DR, Liu S, Gambhir SS, Chen X. MicroPET imaging of glioma integrin αvβ3 expression using 64Cu-labeled tetrameric RGD peptide. J Nucl Med. 2005;46:1707–1718. [PubMed] [Google Scholar]
- 53.Zhang X, Xiong Z, Wu Y, Cai W, Tseng JR, Gambhir SS, Chen X. Quantitative PET imaging of tumor integrin αvβ3 expression with 18F-FPRGD2. J Nucl Med. 2006;47:113–121. [PMC free article] [PubMed] [Google Scholar]
- 54.Wu Z, Li Z, Chen K, Cai W, He L, Chin FT, Li F, Chen X. Micro-PET of tumor integrin αvβ3 expression using 18F-labeled PEGylated tetrameric RGD peptide (18F-FPRGD4) J Nucl Med. 2007;48:1536–1544. doi: 10.2967/jnumed.107.040816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang X, Chen X. Preparation and characterization of 99mTc(CO)3-BPy-RGD complex as αvβ3 integrin receptor-targeted imaging agent. Appl Radiat Isotopes. 2007;65:70–78. doi: 10.1016/j.apradiso.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 56.Liu S, Edwards DS, Ziegler MC, Harris AR, Hemingway SJ, Barrett JA. 99mTc-Labeling of a hydrazinonictotinamide-conjugated vitronectin receptor antagonist. Bioconj Chem. 2001;12:624–629. doi: 10.1021/bc010012p. [DOI] [PubMed] [Google Scholar]
- 57.Liu S, Hsieh WY, Kim YS, Mohammed SI. Effect of coligands on biodistribution characteristics of ternary ligand 99mTc complexes of a HYNIC-conjugated cyclic RGDfK dimer. Bioconj Chem. 2005;16:1580–1588. doi: 10.1021/bc0501653. [DOI] [PubMed] [Google Scholar]
- 58.Jia B, Shi J, Yang Z, Xu B, Liu Z, Zhao H, Liu S, Wang F. 99mTc-labeled cyclic RGDfK dimer: initial evaluation for SPECT imaging of glioma integrin αvβ3 expression. Bioconj Chem. 2006;17:1069–1076. doi: 10.1021/bc060055b. [DOI] [PubMed] [Google Scholar]
- 59.Liu S, He Z, Hsieh WY, Kim YS, Jiang Y. Impact of PKM linkers on biodistribution characteristics of the 99mTc-labeled cyclic RGDfK dimer. Bioconj Chem. 2006;17:1499–1507. doi: 10.1021/bc060235l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu S, Hsieh WY, Jiang Y, Kim YS, Sreerama SG, Chen X, Jia B, Wang F. Evaluation of a 99mTc-labeled cyclic RGD tetramer for non-invasive imaging integrin αvβ3-positive breast cancer. Bioconj Chem. 2007;18:438–446. doi: 10.1021/bc0603081. [DOI] [PubMed] [Google Scholar]
- 61.Liu S, Kim YS, Hsieh WY, Sreerama SG. Coligand effects on solution stability, biodistribution and metabolism of 99mTc-labeled cyclic RGDfK tetramer. Nucl Med Biol. 2008;35:111–121. doi: 10.1016/j.nucmedbio.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jia B, Liu Z, Liu ZF, Yu ZL, Yang Z, Zhao HY, He ZJ, Liu S, Wang F. Linker effects on biological properties of 111In-labeled DTPA conjugates of a cyclic RGDfK dimer. Bioconj Chem. 2008;19:201–210. doi: 10.1021/bc7002988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang JJ, Kim YS, He Z, Liu S. 99mTc-labeling of HYNIC-conjugated cyclic RGDfK dimer and tetramer using EDDA as coligand. Bioconj Chem. 2008;19:634–642. doi: 10.1021/bc7004208. [DOI] [PubMed] [Google Scholar]
- 64.Janssen ML, Oyen WJG, Dijkgraaf I, Massuger LF, Frielink C, Edwards DS, Rajopadhye M, Boonstra H, Corstens FH, Boerman OC. Tumor targeting with radiolabeled αvβ3 integrin binding peptides in a nude mouse model. Cancer Res. 2002;62:6146–6151. [PubMed] [Google Scholar]
- 65.Janssen M, Oyen WJG, Massuger LFAG, Frielink C, Dijkgraaf I, Edwards DS, Rajopadyhe M, Corsten FHM, Boerman OC. Comparison of a monomeric and dimeric radiolabeled RGD-peptide for tumor targeting. Cancer Biother Radiopharm. 2002;17:641–646. doi: 10.1089/108497802320970244. [DOI] [PubMed] [Google Scholar]
- 66.Dijkgraaf I, John AW, Kruijtzer JAW, Liu S, Soede A, Oyen WJG, Corstens FHM, Liskamp RMJ, Boerman OC. Improved targeting of the αvβ3 integrin by multimerization of RGD peptides. Eur J Nucl Med Mol Imaging. 2007;34:267–273. doi: 10.1007/s00259-006-0180-9. [DOI] [PubMed] [Google Scholar]
- 67.Dijkgraaf I, Liu S, Kruijtzer JAW, Soede AC, Oyen WJG, Liskamp RMJ, Corstens FHM, Boerman OC. Effect of linker variation on the in vitro and in vivo characteristics of an 111In-labeled RGD Peptide. Nucl Med Biol. 2007;34:29–35. doi: 10.1016/j.nucmedbio.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 68.Line BR, Mitra A, Nan A, Ghandehari H. Targeting tumor angiogenesis: comparison of peptide and polymer-peptide conjugates. J Nucl Med. 2005;46:1552–1560. [PubMed] [Google Scholar]
- 69.Kenny LM, Coombes RC, Oulie I, Contractor KB, Miller M, Spinks TJ, McParland B, Cohen PS, Hui A, Palmieri C, Osman S, Glaser M, Turton D, Al-Nahhas A, Anoagye EO. Phase I trial of the positron-emitting Arg-Gly-Asp (RGD) peptide radioligand 18F-AH111585 in breast cancer patients. J Nucl Med. 2008;49:879–886. doi: 10.2967/jnumed.107.049452. [DOI] [PubMed] [Google Scholar]
- 70.Beer AJ, Haubner R, Goebel M, Luderschmidt S, Spilker ME, Webster HJ, Weber WA, Schwaiger M. Biodistribution and pharmacokineticss of the αvβ3-selective tracer 18F-Galacto-RGD in cancer patients. J Nucl Med. 2005;46:1333–1341. [PubMed] [Google Scholar]
- 71.Haubner R, Weber WA, Beer AJ, Vabulience E, Reim D, Sarbia M, Becker KF, Goebel M, Hein R, Wester HJ, Kessler H, Schwaiger M. Noninvasive visuallization of the activiated αvβ3 integrin in cancer patients by positron emission tomography and [18F]Galacto-RGD. PLOS Medicine. 2005;2:244–252. doi: 10.1371/journal.pmed.0020070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liu S, Edwards DS, Barrett JA. 99mTc-labeling of highly potent small peptides. Bioconj Chem. 1997;8:621–636. doi: 10.1021/bc970058b. [DOI] [PubMed] [Google Scholar]
- 73.Liu S, Edwards DS. 99mTc-labeled small peptides as diagnostic radiopharmaceuticals. Chem Rev. 1999;99:2235–2268. doi: 10.1021/cr980436l. [DOI] [PubMed] [Google Scholar]
- 74.Liu S. 6-Hydrazinonicotinamide derivatives as bifunctional coupling agents for 99mTc-labeling of small biomolecules. Topics in Current Chem. 2005;252:117–153. [Google Scholar]
- 75.Harris TD, Sworin M, Williams N, Rajopadhye M, Damphousse PR, Glowacka D, Poirier MJ, Yu K. Synthesis of stable hydrazones of a hydrazinonicotinyl-modified peptide for the preparation of 99mTc-labeled radiopharmaceuticals. Bioconj Chem. 1999;10:808–814. doi: 10.1021/bc9900237. [DOI] [PubMed] [Google Scholar]
- 76.Liu S, Edwards DS, Harris AR, Ziegler MC, Poirier MJ, Ewels BA, DiLuzio WR, Hui P. Towards developing a non-SnCl2 formulation for RP444: a new radiopharmaceutical for thrombus imaging. J Pharm Sci. 2001;90:114–123. doi: 10.1002/1520-6017(200102)90:2<114::aid-jps2>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 77.Liu S, Edwards DS, Harris AR, Heminway SJ, Barrett JA. Technetium complexes of a hydrazinonicotinamide-conjugated cyclic peptide and 2-hydrazinopyridine: Synthesis and characterization. Inorg Chem. 1999;38:1326–1335. doi: 10.1021/ic980973o. [DOI] [PubMed] [Google Scholar]
- 78.Jain RK. Transport of molecules in the tumor interstitium: a review. Cancer Res. 1987;47:3039–3051. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed biodistribution data and T/B ratios for 99mTc-labeled cyclic RGD peptides are listed in Tables SI – SVI. Figures SI – SIII illustrate typical radio-HPLC chromatograms of 7, 8 and 10, respectively, in saline before injection, in the urine at 30 min p.i., in the urine at 120 min p.i., and in the feces at 120 min p.i. This information is available free of charge via Internet at http://pubs.acs.org.