Abstract
We tested whether routine preprocedure fluoroscopy of the femoral head would improve sheath placement or reduce the incidence of groin complications. Patients were randomized to receive either fluoroscopy or “blind” sheath placement using palpation alone. The location of the femoral sheath was established by femoral artery angiography. Sheath placement in relation to the femoral head, arterial location, and complication rates were compared. Placement was considered “ideal” if the sheath was in the common femoral artery and in the top or middle third of the femoral head. A total of 256 patients were enrolled. There was no difference in average age, body mass index (BMI), or rate of anticoagulation between the groups. There was no major bleeding in either group. The overall risk of minor bleeding was not statistically different. The treatment group showed higher “ideal” placement relative to the femoral head. In patients who had a BMI ≥30 kg/m2, the difference between the groups was statistically significant (treatment 69% vs control 50%). In conclusion, routine femoral fluoroscopy prior to sheath placement in coronary angiography and angioplasty did not significantly alter bleeding or complication rates but did increase the likelihood of ideal placement, especially in obese patients.
The femoral artery is the most common access site used during cardiac catheterization procedures. Although complications occur in <1% of diagnostic cardiac catheterizations, most of the complications occur as a result of arterial access. These complications include bleeding, hematoma, pseudoaneurysms, and arteriovenous fistulas. The most serious complication is a retroperitoneal bleed, which is associated with an arteriotomy above the inferior border of the inferior epigastric artery (1). Most of these complications could potentially be avoided with “ideal” placement of the arterial sheath in the common femoral artery and over the femoral head.
The femoral head can be visualized quickly and easily with negligible amounts of additional radiation. Using fluoroscopy to see the femoral head to aid in locating the femoral artery was described by Grossman in 1974 (2). Garrett et al showed that the common femoral artery courses over the femoral head in 92% of cases, and 99% of the time the bifurcation of the common femoral artery was below the middle of the femoral head (3). By using fluoroscopy to locate the femoral head prior to arterial sheath placement, the operator may increase the likelihood of correct sheath placement in the common femoral artery, especially in obese patients where bony landmarks can be difficult to palpate.
METHODS
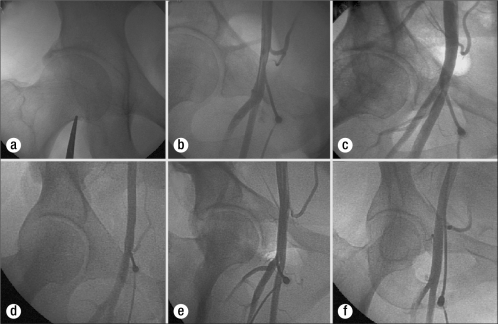
Patients undergoing a diagnostic cardiac catheterization from a femoral artery approach at Baylor University Medical Center over a period of 6 months were randomly assigned to a control group, where fluoroscopy was not used prior to sheath placement, or to a treatment group, where fluoroscopy was used prior to sheath placement to localize the femoral head (Figure 1a).
Figure 1.
(a) Fluoroscopy of the femoral head utilizing forceps to note the position of the inferior border of the femoral head on the patient's skin. (b) Correct placement of the sheath in the common femoral artery. (c) Correct placement of the sheath in relation to the femoral head, with the arterial access incorrectly placed in the superficial femoral artery due to the anatomic variant of a high bifurcation. (d) Correct placement of the sheath in relation to the femoral head with a low hypogastric artery causing incorrect arterial placement in the external iliac artery. (e) Low sheath placement in the profunda femoris artery. (f) High sheath placement in the external iliac artery.
Femoral angiography was performed after sheath placement, and the arterial and bony location of the sheath was recorded. The location of the sheath was considered ideal if it was in the common femoral artery and was over the mid or top portion of the common femoral head (Figure 1b–1f). Patients were monitored after the procedure, and complications of bleeding, hematoma, and pseudoaneurysm were noted.
RESULTS
A total of 256 patients were enrolled and available for analysis. There was no difference between the two groups in use of anticoagulation, body mass index (BMI), age, or gender. No major bleeding or pseudoaneurysms occurred, and there was no significant difference in the incidence of minor bleeding or hematoma. A higher rate of correct placement occurred in the treatment group than in the control group, particularly in obese patients (69% vs 50%). There was no significant difference in correct arterial placement in either group (Table).
Table.
Patient characteristics and placement outcomes in 256 patients receiving either preprocedure fluoroscopy of the femoral head (treatment group) or blind sheath placement (control group) during coronary catheterization
| Variable | Overall (n = 256) | Treatment (n = 130) | Control (n = 126) | P value |
| Patient characteristics | ||||
| Male | 73% | 75% | 71% | NS |
| Average BMI (kg/m2) | 29.10 | 29.21 | 28.98 | NS |
| Receiving anticoagulation | 48% | 48% | 48% | NS |
| Arterial location | ||||
| Common femoral artery | 89% | 87% | 90% | NS |
| External iliac artery | 6% | 8% | 4% | NS |
| Superficial femoral artery | 2% | 2% | 2% | NS |
| Profunda femoris artery | 1% | 0 | 2% | NS |
| Bifurcation | 2% | 3% | 1% | NS |
| Anomalous | 9% | 11% | 6% | NS |
| Complications | ||||
| Bleed/hematoma | 4% | 5% | 2% | NS |
| Sheath placement in relation to the femoral head | ||||
| Mid | 48% | 24% | 24% | NS |
| Top third | 17% | 13% | 4% | NS |
| Bottom third | 29% | 12% | 17% | NS |
| Above | 2% | 1% | 2% | NS |
| Below | 4% | 2% | 2% | NS |
| Correct placement | ||||
| Correct overall | 60% | 65% | 54% | NS |
| Correct in those with BMI <30 | 59% | 62% | 57% | NS |
| Correct in those with BMI ≥30 | 60% | 69% | 50% | 0.02 |
BMI indicates body mass index.
DISCUSSION
Overall, the treatment group was more likely to have ideal placement of the arterial sheath because of correct bony location but not because of correct arterial placement. There was a statistically significant difference favoring femoral head fluoroscopy in obese patients (BMI >30 kg/m2). This may be due in part to the difficulty in palpating the femoral head in obese patients. Obese patients did not have any difference in the number of correct arterial placements, but placement was improved in relation to the femoral head in the group with precatheterization fluoroscopy.
Although no difference was shown in correct arterial placement in this study, the numbers are relatively small and it is possible a significant difference may have been seen with a larger sample size. This would mitigate some of the anatomic variations seen in patients with high bifurcations or a low inferior hypogastric artery.
It is noted that in 20% of patients the common femoral artery bifurcation is above the inferior border of the femoral head. Therefore, utilizing the femoral head as a landmark does not ensure correct arterial placement (3).
With increasing numbers of closure devices being used, placement of the arterial sheath becomes more important. Placement of a closure device may decrease observation time, increase patient turnover, decrease staff hours, and expedite early ambulation. Use of such a device not only improves cost-effectiveness (4) but also improves patient comfort in patients with chronic back pain. In addition, with the feasibility of outpatient percutaneous coronary intervention procedures being evaluated (5), accurate femoral sheath placement becomes more important to facilitate early discharge, as it facilitates the use of these devices.
Inappropriate location of the femoral artery arteriotomy during cardiac catheterization is one factor that may influence the safety of the procedure and can lead to increased complications. Routine fluoroscopy prior to sheath placement in cardiac catheterization can assist in correct placement, especially in obese patients. It does not appear to dramatically reduce complications.
References
- 1.Sherev DA, Shaw RE, Brent BN. Angiographic predictors of femoral access site complications: implication for planned percutaneous coronary intervention. Catheter Cardiovasc Interv. 2005;65(2):196–202. doi: 10.1002/ccd.20354. [DOI] [PubMed] [Google Scholar]
- 2.Grossman M. How to miss the profunda femoris. Radiology. 1974;111(2):482. doi: 10.1148/111.2.482. [DOI] [PubMed] [Google Scholar]
- 3.Garrett PD, Eckart RE, Bauch TD, Thompson CM, Stajduhar KC. Fluoroscopic localization of the femoral head as a landmark for common femoral artery cannulation. Catheter Cardiovasc Interv. 2005;65(2):205–207. doi: 10.1002/ccd.20373. [DOI] [PubMed] [Google Scholar]
- 4.Resnic FS, Arora N, Matheny M, Reynolds MR. A cost-minimization analysis of the angio-seal vascular closure device following percutaneous coronary intervention. Am J Cardiol. 2007;99(6):766–770. doi: 10.1016/j.amjcard.2006.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yee KM, Lazzam C, Richards J, Ross J, Seidelin PH. Same-day discharge after coronary stenting: a feasibility study using a hemostatic femoral puncture closure device. J Interv Cardiol. 2004;17(5):315–320. doi: 10.1111/j.1540-8183.2004.00232.x. [DOI] [PubMed] [Google Scholar]