Abstract
Approximately 60% of deaths in patients with AIDS are a direct result of infection other than HIV. The more severe and life-threatening complications of HIV infection occur in patients with a CD4+ T cell count <200 cells/μL. In the absence of effective retroviral therapy, these infections are associated with a high mortality. We describe a case of disseminated toxoplasmosis discovered at autopsy in a patient with undiagnosed AIDS.
CASE REPORT
A 44-year-old Hispanic man presented in May 2008 with fever (maximum, 104°F), chills, cough (3 months' duration), weight loss (reportedly 50 lbs), abdominal pain, nausea and vomiting, diarrhea, headache, eye pain, and malaise (3 months' duration). He was admitted for evaluation. He was reportedly seen at an outside emergency department 2 days earlier and was treated for presumed bronchitis. On admission, the patient reported no recent travel or significant past medical history. Laboratory results are shown in the Table. Toxic granulations and vacuolated neutrophils were present in the blood. Urine analysis revealed 2+ protein, trace ketone, 1+ blood, positive nitrite, and many bacteria.
Table.
Laboratory results at admission
| Test | Value | Reference range |
| White blood cell count (K/μL) | 7.5 | 4.5–11.0 |
| Lymphocytes (%) | 4 | 20–45 |
| Bands (%) | 13 | <5 |
| Polymorphonuclear leukocytes (%) | 75 | 45–75 |
| Hemoglobin (g/dL) | 14 | 14–18 |
| Hematocrit (%) | 39.2 | 40–52 |
| Platelet count (K/μL) | 155 | 150–400 |
| Sodium (mEq/L) | 132 | 136–145 |
| Potassium (mEq/L) | 3.3 | 3.6–5.0 |
| Calcium (mg/dL) | 7.8 | 8.4–10.2 |
| Total protein (g/dL) | 6.2 | 6.4–8.3 |
| Albumin (g/dL) | 2.9 | 3.5–5.0 |
| Albumin/globulin ratio | 0.9 | 1.1–2.2 |
| Alkaline phosphatase (U/L) | 43 | 40–129 |
| Aspartate aminotransferase (U/L) | 192 | 10–50 |
| Alanine aminotransferase (U/L) | 226 | 10–50 |
| Myoglobin (ng/mL) | >500 | 5–190 |
The patient underwent an extensive infectious and neoplastic workup, with tests for Histoplasma sp., Leptospira sp., Entamoeba histolytica, Toxocara canis, Coccidioides sp., Brucella sp., Rickettsia sp., and hantavirus. A computed tomography scan of the chest found patchy alveolar opacities bilaterally, and a computed tomography scan of the pelvis found a 1-cm-diameter appendix with fluid and no sonographic evidence of an acute intraabdominal process. Blood, urine, and sputum cultures were obtained, and the patient was treated empirically with antibiotics, including levofloxacin, metronidazole, doxycycline, and caspofungin for presumed sepsis. However, the patient's fever persisted and his respiratory function worsened, requiring intubation, mechanical ventilation, and transfer to the intensive care unit. His pulmonary status deteriorated, and he died on hospital day 4.
AUTOPSY RESULTS
At autopsy, the lungs were consolidated, with changes consistent with acute respiratory distress syndrome. Bilateral pleural effusions (100 mL each) were also present. The brain, heart, liver, and spleen were not enlarged and were grossly unremarkable. The gastric mucosa was erythematous with superficial mucosal hemorrhage, and the appendix was softened. The bladder mucosa contained multiple areas of mucosal hemorrhage and a focally raised plaquelike lesion. The paraaortic and hilar lymph nodes were enlarged.
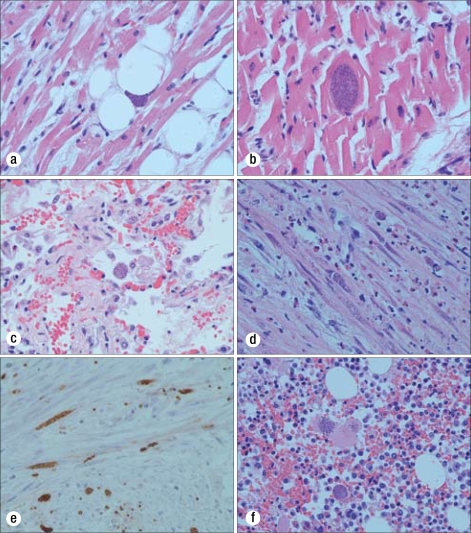
Cytomegalovirus pneumonitis, Pneumocystis jiroveci (carinii) pneumonia, cytomegalovirus adrenalitis, and disseminated toxoplasmosis were identified microscopically, and pulmonary cytomegalovirus was confirmed postmortem by viral culture of the lung tissue. Postmortem antibody testing for HIV was positive and was confirmed by Western blot. Microscopically, Toxoplasma gondii cysts (bradyzoites) and free tachyzoites (trophozoites) were visualized in the heart, lungs, brain, adrenal glands, appendix, stomach, pancreas, bladder, right testis, spleen, gallbladder, lymph nodes, muscle, and bone marrow (Figure).
Figure.
Toxoplasma gondii bradyzoite cysts in the (a, b) heart (×10 and ×40, respectively); (c) lung (×10); (d, e) appendix muscle layer (×40; part e with Toxoplasma immunohistochemical stain); and (f) bone marrow (×40). All stains were hematoxylin and eosin except where noted.
DISCUSSION
Toxoplasmosis, which is caused by Toxoplasma gondii, is found worldwide in humans and in many species of animals and birds (1, 2). More than 60 million people in the United States may be infected with Toxoplasma, and up to one third of the world's population is estimated to carry a Toxoplasma infection (3). The protozoan parasite is transmitted to humans via three routes: (a) ingestion of raw or undercooked contaminated meat; (b) exposure to Toxoplasma gondii oocysts (a form of the organism passed in cat feces through cat litter or through soil by way of gardening or consumption of unwashed fruits or vegetables or contaminated water); and (c) congenital, in which maternal infection is passed transplacentally via blood to the fetus (2, 4).
Immunocompetent persons with a primary infection are usually asymp- tomatic, but latent infection can persist for life (4, 5). In immunosuppressed patients, especially patients with AIDS, the parasite can reactivate and cause disease when the CD4 lymphocyte count falls below 100 cells/μL (6). Patients with AIDS and CD4 counts <100 cells/μL who are Toxoplasma seropositive have a 30% probability of developing reactivated toxoplasmosis if they are not receiving effective prophylaxis; the most common site of reactivation is the central nervous system (1).
In a study by Belanger et al that included 116 confirmed, probable, or possible cases of toxoplasmosis in HIV-positive patients, cerebral toxoplasmosis accounted for 89% of cases; pulmonary infection, 6%; ocular, 3.5%; and disseminated, 1.7% (7). In another series with 199 HIV-infected patients, the prevalence of extracerebral toxoplasmosis was 1.5% to 2% (8). In those select patients, eye involvement occurred in 50%, lung involvement in 26%, two or more extracerebral sites in 11.5%, and peripheral blood, heart, and bone marrow involvement in 3% of cases. Involvement of the bladder, pharynx, skin, liver, lymph nodes, and pericardium was demonstrated in rare cases. Central nervous system disease was identified in 41% of patients (8).
Extracerebral toxoplasmosis is generally difficult to diagnose because of its nonspecific clinical symptoms. Therefore, it is generally identified postmortem, and its prevalence is frequently underestimated (9). The most prominent risk factor for the development of extracerebral toxoplasmosis is advanced immunosuppression (mean CD4 counts of 57 cells/μL). The CD4+ helper T-cell deficit is responsible for uncontrolled parasitic invasion and associated tissue damage. The prognosis of toxoplasmosis in immunosuppressed patients is grim, and the disease is usually fatal if untreated. Improvement may be seen if treatment is started early, but recrudescence is common.
Toxoplasmosis is generally not associated with HIV seroconversion. This phenomenon, although rare, has been reported, as noted in a recent case report by Barbosa et al, in which two patients presented with acute disseminated and severe toxoplasmosis as the first opportunistic disease related to AIDS. In both patients, clinical and laboratory findings were similar to findings for sepsis or septic shock, and death occurred quickly (6). Al-Kassab et al reported similar findings in an HIV patient with a normal clinical examination and normal chest x-ray at presentation but with acute respiratory distress and demise within 5 days (10). A similar patient with acute disseminated T. gondii infection with massive organ involvement during primary HIV infection was also described by Signorini et al (11).
This case is of note because the patient's AIDS/HIV was diagnosed at autopsy. A large number of opportunistic processes have been identified at autopsy in patients with AIDS, yet the precise role of each process in causing death is often unclear (12). Patients whose HIV is either untreated or undiagnosed, such as the patient described here, have a fourfold higher risk of dying in the acute phase of infection.
References
- 1.Heller H. Toxoplasmosis in HIV-infected patients. In: Rose BD, editor. UpToDate. Waltham, MA: UpToDate; 2008. [Google Scholar]
- 2.Montoya JG, Liesenfeld O. Toxoplasmosis. Lancet. 2004;363(9425):1965–1976. doi: 10.1016/S0140-6736(04)16412-X. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . Toxoplasmosis [online fact sheet] Atlanta, GA: CDC; 2007. [Google Scholar]
- 4.Ross DS, Jones JL, Lynch MF. Toxoplasmosis, cytomegalovirus, listeriosis, and preconception care. Matern Child Health J. 2006;10(5 Suppl):S187–S191. doi: 10.1007/s10995-006-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kasper LH, Buzoni-Gatel D. Some opportunistic parasitic infections in AIDS: candidiasis, pneumocystosis, cryptosporidiosis, toxoplasmosis. Parasitol Today. 1998;14(4):150–156. doi: 10.1016/s0169-4758(97)01212-x. [DOI] [PubMed] [Google Scholar]
- 6.Barbosa CJ, Molina RJ, de Souza MB, Silva AC, Micheletti AR, dos Reis MA, de Paula Antunes Teixeira V, Silva-Vergara ML. Disseminated toxoplasmosis presenting as sepsis in two AIDS patients. Rev Inst Med Trop Sao Paulo. 2007;49(2):113–116. doi: 10.1590/s0036-46652007000200009. [DOI] [PubMed] [Google Scholar]
- 7.Belanger F, Derouin F, Grangeot-Keros L, Meyer L, HEMOCO and SEROCO Study Groups Incidence and risk factors of toxoplasmosis in a cohort of human immunodeficiency virus-infected patients: 1988–1995. Clin Infect Dis. 1999;28(3):575–581. doi: 10.1086/515147. [DOI] [PubMed] [Google Scholar]
- 8.Rabaud C, May T, Amiel C, Katlama C, Leport C, Ambroise-Thomas P, Canton P. Extracerebral toxoplasmosis in patients infected with HIV. A French National Survey. Medicine. 1994;73(6):306–314. doi: 10.1097/00005792-199411000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hofman P, Bernard E, Michiels JF, Thyss A, Le Fichoux Y, Liubiere R. Extracerebral toxoplasmosis in the acquired immunodeficiency syndrome (AIDS) Pathol Res Pract. 1993;189(8):894–901. doi: 10.1016/S0344-0338(11)81101-5. [DOI] [PubMed] [Google Scholar]
- 10.al-Kassab AK, Habte-Gabr E, Mueller WF, Azher Q. Fulminant disseminated toxoplasmosis in an HIV patient. Scand J Infect Dis. 1995;27(2):183–185. doi: 10.3109/00365549509019005. [DOI] [PubMed] [Google Scholar]
- 11.Signorini L, Gulletta M, Coppini D, Donzelli C, Stellini R, Manca N, Carosi G, Matteelli A. Fatal disseminated toxoplasmosis during primary HIV infection. Curr HIV Res. 2007;5(2):273–274. doi: 10.2174/157016207780077011. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie R, Travis WD, Dolan SA, Pittaluga S, Feuerstein IM, Shelhamer J, Yarchoan R, Masur H. The causes of death in patients with human immunodeficiency virus infection: a clinical and pathologic study with emphasis on the role of pulmonary diseases. Medicine. 1991;70(5):326–343. doi: 10.1097/00005792-199109000-00004. [DOI] [PubMed] [Google Scholar]