Abstract
Objective
To examine ethnic differences in depressive symptoms and antidepressant treatment in a cohort of patients undergoing diagnostic coronary angiography.
Background
Coronary heart disease (CHD) is the leading cause of mortality in the US, with an excess of mortality in African Americans. Traditional risk factors occur more frequently among African Americans but do not fully account for this increased risk. Elevated depressive symptoms have been shown to be associated with higher morbidity and mortality in CHD patients.
Methods
A consecutive series of 864 patients (727 Caucasians, 137 African Americans) completed the Beck Depression Inventory (BDI) to assess depressive symptoms. Data describing cardiovascular risk factors and type of medications including antidepressants were obtained from chart review at the time of study enrollment.
Results
There was no difference in the severity of depressive symptoms between Caucasians (p =.50); the prevalence of elevated depressive symptoms also was similar for African Americans (35%) and Caucasians (27%) (p =.20). However, the rate of antidepressant use was 21% for Caucasians but only 11.7% for African Americans (p =.016). The odds ratio for ethnicity (African American vs. Caucasian) in predicting antidepressant use was 0.43 (95% CI=0.24–0.76, p=0.004) after adjustment for BDI scores.
Conclusions
African Americans with CHD are less likely to be treated with anti-depressant medications compared to Caucasians, despite having similar levels of depression. The ethnic differences in the psychopharmacological management of depression suggests that more careful assessment of depression, especially in African Americans, is necessary to optimize care of patients with CHD.
Keywords: African-Americans, depression, coronary disease, ethnicity
Coronary heart disease (CHD) is the leading cause of death in both Caucasians and African Americans in the United States and is especially significant for African Americans compared to other ethnic groups. 1–5 This excess in cardiovascular mortality among African Americans may be attributed to such factors as a higher prevalence of traditional risk factors 6 7 and greater likelihood that those risk factors are poorly controlled 8, greater delay in seeking medical care 7, and disparities in medical treatment 9, 10, including differences in health care access and health care utilization, leading to treatment delays and increased disease severity at the time of diagnosis.11 12
Depression has emerged as a new and important psychosocial risk factor in which the prevalence of major depression (MDD) has been estimated to be 15–20% 13 14 with up to an additional 20% of CHD patients reporting elevated depressive symptoms.15 Importantly, depression also is associated with a 2- to 3-fold increase in risk of morbidity and mortality in patients with CHD.16–20 In recognition of the importance of depression, the American College of Cardiology and the American Heart Association recently recommended that depressive symptoms should be routinely assessed (Class I recommendation), so that proper interventions can be instituted (Class IIa recommendation)21 Despite this recommendation, depression is often under-recognized and under-treated, especially in patients with medical illness.22–24
Studies that have compared ethnic differences in non-cardiac populations suggest that African Americans are particularly vulnerable to under-treatment of depression, with treatment rates 33–50% less than those of Caucasians.25–28 Little is known about ethnic differences in the prevalence and pharmacologic treatment of depression in patients with CHD. Therefore, the purpose of this study was to examine racial disparities in depressive symptoms and psychopharmacologic treatment in a cohort of CHD patients undergoing diagnostic coronary angiography.
METHODS
Study Patients
Participants were recruited from the Diagnostic Cardiac Catheterization Laboratory at Duke University Medical Center between April 1999 and June 2002. Patients were part of a larger prospective investigation known as the VAGUS (Very Anxious Group Under Scrutiny) study, which was designed to evaluate the effects of anxiety on mortality in CHD patients. The protocol was approved by the Duke University Medical Center Institutional Review Board and all patients provided written informed consent before participating in the research protocol. Participants had significant coronary artery disease (CAD) defined as at least 75% occlusion of one coronary artery. In addition, patients were required to be in normal sinus rhythm at the time of enrollment, which was necessary to assess heart rate variability (HRV) aspect of the VAGUS study,
Initially, 9162 patients underwent left heart cardiac catheterization and 8028 charts were available for screening. Approximately 75% of the screened patients did not qualify for the study. The two main reasons for exclusion were insignificant CAD (n=2549 patients) and factors affecting HRV (n=2895). Factors affecting HRV included acute myocardial infarction (MI) or revascularization procedure during the previous 30 days (n=2159) and abnormal cardiac rhythm (n=736). An additional 627 patients were not approached because of medical, complications that could compromise patients’ ability to provide written informed consent (e.g., ventilator-dependency, stroke-related aphasia, inability to speak English, and acute psychosis). Approximately half of the remaining eligible patients declined to participate (n=1003). Of the 955 enrolled patients, 34 patients were unable to complete any items on the Beck Depression Inventory (BDI) due to time constraints, leaving 921 patients with useable information. Ethnicity was primarily Caucasian (79%, n=727), with 15% African-Americans (n=137), 5% Native American (n=44), and 1% Asian or Hispanic (n=13). Because of the relatively small number of patients in the Native American, Asian, and Hispanic categories, the present analysis focused only on the subset of 864 patients representing the Caucasian and African-American patients.
Assessment of Depression
Depressive symptomatology was assessed by the Beck Depression Inventory (BDI). 29 The BDI is a 21-item self-report questionnaire that measures characteristic symptoms of depression including negative affect, cognitions, and somatic symptoms. The BDI is widely used in cardiac populations and has been shown to have prognostic value. 15 18
Clinical and Demographic Characteristics
Cardiac catheterization results were used to determine left ventricular ejection fraction (LVEF) and CAD severity. Data describing current comorbid conditions, CHD treatment plan (medical management, percutaneous transluminal coronary angioplasty, or coronary bypass grafting surgery), cardiovascular risk factors (lipids, smoking history, body weight, diabetes, hypertension) and type of medications, including antidepressants and other psychotropic medications, were obtained from patient chart review at the time of study enrollment.
Data analysis
Background characteristics of African Americans and Caucasian Americans were compared using the Pearson Chi-Square test for categorical variables and the Wilcoxon test for continuous data. Five patients had missing data: one patient had missing data for blood pressure; one patient did not provide information about education; and three patients did not have complete cardiac medication data available. These missing data were replaced with the sample median or most prevalent category for the respective variable.
We calculated unadjusted ethnic group difference in antidepressant use and tested these differences using the Pearson Chi-Square test. We further described antidepressant use based upon their BDI score using established criteria:30 “Not Depressed” (BDI < 10); “Mildly Depressed” (BDI 10–18); and “Moderate-Severely Depressed” (BDI > 18). We then estimated a set of logistic regression models in order to examine potential confounders or explanatory mechanisms. Each model specified antidepressant use (Yes vs. No) as the response variable and ethnicity (African American vs. Caucasian) as the predictor of primary interest. Adjustment variables were selected a priori based on previous research and maintained in the model irrespective of statistical significance. The predictors in each model were as follows: Model 1: Ethnic group indicator (African American vs. Caucasian American); Model 2: Ethnic group and continuous BDI score (modeled as a restricted cubic spline with three knots in all models); Model 3: Ethnic group, BDI, age, gender, LVEF, blood pressure, heart failure, Prior MI, Prior CABG, current mode of therapy (medical, PTCA, CABG), smoking status (never, quit, current), and beta blocker use; Model 4: identical to Model 3, but also including a set of interactions, specified a priori including Ethnicity by Gender, Ethnicity by BDI, and Gender by BDI. The interactions were tested using the pooled approach recommended by Harrell.31 Because Model 3 tended to exceed the recommendation for events/predictor ratio32, we also conducted a propensity score analysis.33 The propensity score is a single index capturing ethnic differences on a large number of dimensions. The single index was used as an adjustment variable in the primary logistic regression model. The propensity score was generated using a logistic regression model predicting ethnicity using a large number of background variables. The predictors of ethnicity with the largest magnitude effects, and therefore carrying the greatest weight in the propensity score, were gender, age, education, diastolic blood pressure, and 3-vessel CAD. The individual case probabilities from the logistic propensity model were then linearized (logit-transformed) to create the final propensity score. The propensity score (modeled as a 4-knot restricted cubic spline) was then included in a logistic regression model with ethnicity and BDI predicting antidepressant use, and excluding the 13 cases that had propensity scores that did not overlap across ethnic categories. P-values for the effects in the logistic models were generated by the Wald test.
RESULTS
Background Characteristics
Data were available from 864 CAD patients (727 Caucasians and 137 African Americans) undergoing diagnostic angiography. Table 1 presents the demographic and clinical characteristics for African American and Caucasian patients. The most prominent differences between African American and Caucasians in the sample were that African Americans were younger, had fewer years of formal education and less income, lower LVEF, higher rates of heart failure, higher incidence of hypertension, and higher diastolic blood pressure (DBP).
Table 1.
Descriptive Statistics by Ethnicity
| N | Caucasian N = 727 | African American N = 137 | Combined N = 864 | Test Statistic | |
|---|---|---|---|---|---|
| Current Antidepressant | 864 | 21% | 12% | 20% | , P = 0.0111 |
| BDI Score | 864 | 3 6 10 | 3 6 11 | 3 6 10 | F1,862 = 0.43, P = 0.5112 |
| BDI Category : None | 864 | 73% | 66% | 72% | , P = 0.1711 |
| Mild-Mod | 21% | 26% | 21% | ||
| Mod- Severe | 6% | 9% | 6% | ||
| Gender : Women | 864 | 27% | 41% | 29% | , P = 0.0011 |
| Age yrs | 864 | 55 63 71 | 50 58 66 | 54 62 71 | F1,862 = 20.7, P <0.0012 |
| Education : < HS | 864 | 27% | 49% | 30% | , P< 0.0011 |
| HS/Some Coll. | 51% | 43% | 50% | ||
| Coll./Post Grad. | 22% | 8% | 20% | ||
| Annual Income : <$15K | 770 | 22% | 47% | 26% | , P<0.0011 |
| $15–30K | 22% | 32% | 23% | ||
| $30–50K | 22% | 13% | 21% | ||
| >$50K | 34% | 9% | 30% | ||
| Smoking Status : Current | 864 | 14% | 14% | 14% | , P = 0.1571 |
| Never | 28% | 36% | 29% | ||
| Quit | 58% | 50% | 57% | ||
| 3-Vessel Disease | 864 | 43% | 47% | 44% | , P = 0.3421 |
| LVEF % | 864 | 47 59 65 | 38 51 62 | 45 58 65 | F1,862 = 12.7, P <0.0012 |
| Heart Failure | 864 | 18% | 35% | 21% | , P < 0.0011 |
| Prior MI | 864 | 43% | 38% | 42% | , P = 0.2551 |
| Prior CABG | 864 | 37% | 34% | 36% | , P = 0.5681 |
| Current CAD Tx : Medical | 864 | 55% | 61% | 56% | , P = 0.2861 |
| PTCA | 15% | 15% | 15% | ||
| CABG | 30% | 23% | 29% | ||
| Hypertension | 864 | 78% | 91% | 80% | , P < 0.0011 |
| SBP | 863 | 118 129 140 | 118 130 143 | 118 129 140 | F1.861 = 0.89, P = 0.3452 |
| DBF | 863 | 61 68 74 | 62 70 80 | 61 68 75 | F1,861 = 10.1, P = 0.0022 |
| COPD | 864 | 16% | 18% | 16% | , P = 0.7091 |
| Beta Blockers | 864 | 81% | 81% | 81% | , P = 0.9991 |
represent the lower quartile a, the median b, and the upper quartile c for continuous variables.
N is the number of non-missing values.
Tests used: Pearson test;
Wilcoxon test
One-hundred sixty nine patients were on antidepressant therapy. The classes of antidepressant were: selective serotonin reuptake inhibitor, 67% (n = 111), norepinephrine reuptake inhibitor, 4% (n = 7), serotonin/norepinephrine reuptake inhibitor, 18% (n = 30), and mixed action, trazodone, 2% (n = 4), bupropion, 10% (n = 17). Because low dose norepinephrine reuptake inhibitors may be used for pain management and bupropion for smoking cessation, we reviewed the charts of patients taking these medications to confirm that they were being treated for depression. Nine patients (all Caucasian) were taking bupropion primarily for smoking cessation. Based on chart review, all other patients were on antidepressant therapy for depressive symptoms.
Presence of depressive symptoms
Overall, 27% of the sample had significant depressive symptoms (BDI scores ≥ 10) and an additional 10% were on anti-depressant medications with BDI scores < 10, suggesting that 38% of the sample had significant depression. BDI scores ranged from 0 to 46 (mean: 7.4; median: 6.0, standard deviation: 6.6). Although the median BDI score (median = 6) was identical in both ethnic groups, African Americans tended to be more likely to be classified as mildly (26% v 21%) or moderately-to-severely depressed (9% v 6%) compared to Caucasians (p =.20).
Unadjusted rates of antidepressant use
The overall rates of antidepressant use were 21% (153/727) for Caucasians and 11.7% (16/137) for African Americans (χ2 [1df] = 6, p =.016). Table 2 shows that Caucasians were more likely than African Americans to be on antidepressants in each of the three BDI severity categories. We further considered ethnic and gender differences in antidepressant use by BDI severity category. Among patients with BDI < 10, 14% (n = 56) of the Caucasian men compared to 2% (n = 1) of African American men were on antidepressants, while 21% (n= 28) of the Caucasian women and 19% (n = 7) of African American women were on antidepressants. Among patients with BDI between 10 and 18, 28% (n = 27) of the Caucasian men and 11% (n = 2) of African American men were on antidepressants; 39% (n = 20) of the Caucasian women and 12% (n = 2) of African American women were on antidepressants. Considering patients with BDI> 18, 43% (n = 13) of the Caucasian men but only 22% (n = 2) of African American men were on antidepressants; 64% (n = 9) of the Caucasian women and 67% (n = 2) of African American women were on antidepressants.
Table 2.
Rate of antidepressant use by BDI Seventy and Ethnicity
| BDI Category | Ethnicity | No Antidepressant n = 695
|
Antidepressant n= 169
|
Total n = 864
|
|---|---|---|---|---|
| % of row (n) | % of row (n) | % of entire sample (n) | ||
| None BDI < 10 | Caucasian | 84.2 (449) | 15.8 (84) | 61.7(533) |
| African American | 91.1 (82) | 8.9 (8) | 10.4 (90) | |
|
| ||||
| Mild-Mod. BDI = 10–18 | Caucasian | 68.7 (103) | 31.3 (47) | 17.4(150) |
| African American | 88.6 (31) | 11.4 (4) | 4.1 (35) | |
|
| ||||
| Mod.-Sev. BDI > 18 | Caucasian | 50.0 (22) | 50.0(22) | 5.1 (44) |
| African American | 66.7 (8) | 33.3 (4) | 1.4 (12) | |
None = No significant depressive symptoms
Mild-Mod. = Mild to moderate depressive symptoms
Mod.-Sev. = Moderate to severe depressive symptoms
Logistic regression models: Ethnicity predicting antidepressant use
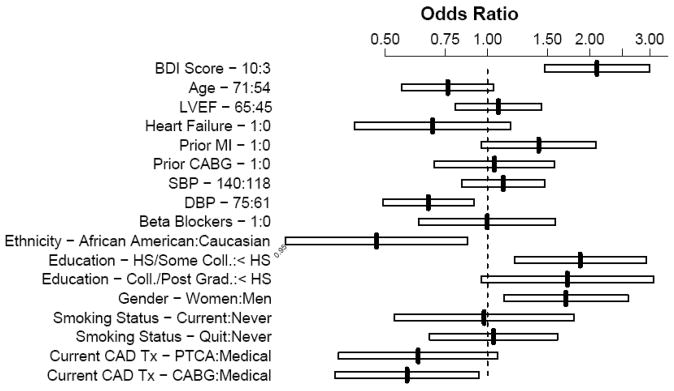
In order to quantify the likelihood of antidepressant use, odds ratios (ORs), expressed as the odds of antidepressant use/odds of no antidepressant use, were calculated by ethnicity and gender. The unadjusted odds ratio for ethnicity (coded African American/Caucasian) was 0.50 (95% CI = 0.29–0.86, p =.013). Adjusting for the continuous BDI score, the OR for ethnicity was 0.43 (95% CI = 0.24–0.76, p =.004). The OR for a 7-point increase in BDI score was 2.11 (95% CI = 1.51–2.96, p =.001). Table 3 shows the p-values for the Wald tests for the fully adjusted logistic model. After adjustment for background characteristics, African Americans were significantly less likely to be on antidepressants: OR = 0.47 (95% CI = 0.25–0.88, p =.020). Figure 1 depicts the point estimate odds ratios and 95% confidence limits from this fully adjusted model. Higher BDI scores, female gender, prior MI, medical treatment versus PTCA or CABG, and lower DBP were also significantly associated with greater odds of antidepressant use. When we removed the nine patients who apparently were prescribed bupropion for smoking cessation the results remained essentially unchanged (OR for ethnicity = 0.50, 95% CI 0.27 – 0.93, p =.030). The pooled test for the three pre-specified interactions, ethnicity by BDI, ethnicity by gender, and BDI by gender was not significant (p =.490), suggesting that the effect of ethnicity may be consistent across gender and BDI severity categories. Finally, adjusting for the propensity score (and removing 13 non-overlapping cases) resulted in a similar estimate for ethnicity: OR= 0.42 (95% CI = 0.22–0.81, p <.009).
Table 3.
Wald Statistics for Logistic Regression Model Predicting Antidepressant Use
| χ2 | d.f. | P | |
|---|---|---|---|
| Ethnicity | 5.68 | 1 | 0.0172 |
| BDI | 41.21 | 2 | < 0.0001 |
| Nonlinear | 0.60 | 1 | 0.4387 |
| Age | 2.87 | 1 | 0.0901 |
| Education | 7.76 | 2 | 0.0207 |
| Gender | 6.16 | 1 | 0.0130 |
| LVEF | 0.25 | 1 | 0.6174 |
| CHF | 1.90 | 1 | 0.1686 |
| Smoking Status | 0.07 | 2 | 0.9651 |
| Mode of CAD Therapy | 6.58 | 2 | 0.0373 |
| Prior MI | 3.08 | 1 | 0.0794 |
| Prior CABG | 0.05 | 1 | 0.8194 |
| SBP | 0.55 | 1 | 0.4584 |
| DBP | 6.49 | 1 | 0.0109 |
| Beta Blockers | 0.00 | 1 | 0.9956 |
| TOTAL | 86.91 | 18 | < 0.0001 |
Figure 1.
Odds ratios and 95% confidence limits from logistic regression model predicting antidepressant use. For continuous predictors, the values to the immediate right of the predictor name in column 1 represent the scaling distance on the predictor. For example, BDI 10:3 in row 1 reflects a comparison of the odds of antidepressant use for a typical patient with a BDI score of 10 to the odds of antidepressant use for a patient with a score of 3, i.e. the OR associated with a 7-point increase on the BDI. Scaling distances for continuous predictors are the interquartile ranges for that predictor. For categorical predictors, the level names to the right of the predictor name represent the levels being compared to generate the OR. For example, Ethnicity – African American: Caucasian indicates that the OR is comparing the odds of antidepressant use among African Americans to the odds of antidepressant use for Caucasians.
DISCUSSION
Considerable health disparities exist in the prevalence, morbidity and mortality associated with CHD.5 34 Cardiovascular diseases by themselves account for more than one third of the differences in life expectancy between blacks and whites35 and African Americans have significantly greater risk of dying from CHD compared to their Caucasian counterparts.36 The reasons for this inequality are multifactorial, including biological, behavioral, and social factors. For example, African Americans have greater prevalence of cardiovascular risk factors including hypertension and diabetes,6 8 which are less likely to be well controlled.8 Because of the accumulating evidence that depression also contributes to increased risk in patients with CHD, the present study examined ethnic differences in depressive symptoms and antidepressant treatment in patients undergoing diagnostic coronary angiography. In this large sample of over 850 patients, evidence of clinically significant depression defined as BDI scores ≥10 or BDI scores <10 but on anti-depressant medication, was found in 38.5 % patients, 40.1% of African Americans and 38.2% of Caucasians. These results are consistent with previous studies, primarily consisting of Caucasians, which showed the prevalence of clinically significant depressive symptoms to occur in one out of every five cardiac patients.15 37
Although we found no ethnic differences in the severity of depressive symptoms, depression appeared to be under-treated especially in African Americans: 35.5% of Caucasians with BDI scores ≥ 10 were treated with antidepressants, compared to only 17% of African Americans. This difference was especially evident in men compared to women, with only 22% of moderately-to-severely depressed African American men on antidepressants compared to 43% of their white counterparts.
There are several possible explanations for the current findings. It has been noted that patients’ race/ethnicity influence physicians’ recognition and treatment of depressive symptoms.25,38 Different causes for this difference in mental health treatment have been suggested, including patients feeling stigmatized by a mental health disorder,39 low patient education and recognition of depressive symptoms, 40 41 patient preferences and/or ability to access and pay for treatment,42 and low provider recognition of depressive symptoms in minority groups.43 Moreover, studies have found that when the diagnosis of a depressive disorder was made, prescription of antidepressants was consistently higher among Caucasians than among minority patients, especially African Americans. 26 28 38 44 For example, Skaer, Sclar, and Robinson44 found that the rates of office visits in which depression was diagnosed and antidepressants prescribed were higher among Caucasians compared to minorities, with rates for African Americans half those for Caucasians. In an analysis of Medicaid claims, Strothers et al.45 reported that 37.1% of depressed African Americans did not receive antidepressant medication compared to 22.4% of Caucasians (p <0.001). In a sample of cardiac patients, Amin et al.14 reported that only 1 out of every 4 patients with moderate to severe depressive symptoms admitted for acute coronary syndrome was recognized as being depressed before their hospital discharge. Minority status, low ejection fraction, and low education were associated with unrecognized depressive symptoms. The odds ratio for unrecognized depressive symptoms for minority status was 6.73 for minorities compared to whites.
Our study had several limitations. Classification of depression was based on self-reported symptoms rather than a standard psychiatric interview. Although the BDI is considered a reliable and valid instrument for measuring the severity of depressive symptoms30, it is not a diagnostic tool. In addition, antidepressant use was obtained from medical records at the time of patients’ diagnostic coronary angiography. No information was available concerning dose of antidepressants or other types of depression treatment that patients may have received. We also are unable to determine if the differential rates of antidepressant treatment in African Americans is a result of under-diagnosis of depression or under-treatment by physicians, or if it is an expression of reluctance of African American patients to discuss their symptoms and request or accept pharmacological treatment. Although African Americans had less education and income compared to Caucasians in this sample, we found little evidence that these indicators of socio-economic status were responsible for the higher rates of anti-depressant use among Caucasians compared to African Americans. That is, although Caucasians had higher educational levels compared to African Americans (p = 0.001), the education by ethnicity interaction for anti-depressant use was not significant (p =.933). Similarly, Caucasians also had higher income levels compared to African Americans (p = 0.001), but there was no evidence of an ethnicity by income interaction (p = 0.685). Among the 770 patients with available income data, antidepressant use among Whites was higher than that of African Americans in each of the four quartiles of income: 1st quartile (<$15,000): 26.9% vs. 14.5%; 2nd quartile: 24.6% vs. 10.8%; 3rd quartile: 20.1% vs 13.3%; 4th quartile (>$50,000): 16.7% vs 0%. Therefore, it is unlikely that differential education or income level was responsible for the ethnic differences in anti-depressant use. Unfortunately, we had limited information about patients’ health insurance, so we still cannot rule out the possibility that African Americans may have been less likely to afford antidepressant medications compared to Caucasians. Finally, we should note that ethnicity was based upon patients’ self-identification. We recognize that categorization of patients into ethnic or racial groups can be imprecise14; we attempted to minimize uncertainty by eliminating the small number of Hispanics and Native Americans from our analyses.
Summary
The need to improve detection and treatment of depression among patients with CHD is widely recognized. And the need to provide efficient and equal healthcare to all patients is a necessity. The federal government’s health plan, Healthy People 2010, has stated as a goal to eliminate any kind of health disparities by race, ethnicity, gender or socio-demographic characteristics healthy people,46 by the year 2010. Results of this study demonstrate that elevated depressive symptoms are common in patients undergoing diagnostic coronary angiography and that a significant proportion of patients with significant depressive symptoms are not treated. Moreover, we noted that African Americans are less likely to be treated with anti-depressant medications compared to their white counterparts, despite having similar levels of depressive symptoms. African American men with high levels of depression are especially likely to be under-treated. The ethnic differences in the psychopharmacological management of depression suggests that more careful assessment of depression, especially in African Americans, is necessary to optimize care of patients with CHD.
Acknowledgments
This study was supported by grant MH 49679 from the National Institutes of Health and grant M01-RR-30 from the General Clinical Research Center Program, National Center for Research Resources, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mehta RH, Marks D, Califf RM, et al. Differences in the clinical features and outcomes in African Americans and whites with myocardial infarction. American Journal of Medicine. 2006;119(1):70 e1–8. doi: 10.1016/j.amjmed.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 2.Gillum RF. Coronary heart disease in black populations. I. Mortality and morbidity. American Heart Journal. 1982;104(4 Pt 1):839–51. doi: 10.1016/0002-8703(82)90021-7. [DOI] [PubMed] [Google Scholar]
- 3.Gillum RF, Mussolino ME, Madans JH. Coronary heart disease incidence and survival in African-American women and men. The NHANES I Epidemiologic Follow-up Study. Annals of Internal Medicine. 1997;127(2):111–8. doi: 10.7326/0003-4819-127-2-199707150-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sempos C, Cooper R, Kovar MG, McMillen M. Divergence of the recent trends in coronary mortality for the four major race-sex groups in the United States. American Journal of Public Health. 1988;78(11):1422–7. doi: 10.2105/ajph.78.11.1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–41. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 6.Maynard C, Fisher LD, Passamani ER, Pullum T. Blacks in the Coronary Artery Surgery Study: risk factors and coronary artery disease. Circulation. 1986;74:64–71. doi: 10.1161/01.cir.74.1.64. [DOI] [PubMed] [Google Scholar]
- 7.Cooper RS, Simmons B, Castaner A, Prasad R, Franklin C, Ferlinz J. Survival rates and prehospital delay during myocardial infarction among black persons. American Journal of Cardiology. 1986;57(4):208–11. doi: 10.1016/0002-9149(86)90892-1. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Ineffective secondary prevention in survivors of cardiovascular events in the U.S. population: Report from the Third National Health and Nutrition Examination Survey. Archives of Internal Medicine. 2001;161:1621–1628. doi: 10.1001/archinte.161.13.1621. [DOI] [PubMed] [Google Scholar]
- 9.Echols MR, Mahaffey KW, Banerjee A, et al. Racial differences among high-risk patients presenting with non-ST-segment elevation acute coronary syndromes (results from the SYNERGY trial) American Journal of Cardiology. 2007;99:315–321. doi: 10.1016/j.amjcard.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Sonel AF, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?) Circulation. 2005;111(10):1225–32. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- 11.Lewis CE, Raczynski JM, Oberman A, Cutter GR. Risk factors and the natural history of coronary heart disease in blacks. Cardiovascular Clinics. 1991;21:29–45. [PubMed] [Google Scholar]
- 12.Syed M, Khaja F, Rybicki BA. Effect of delay on racial differences in thrombolysis for acute myocardial infarction. American Heart Journal. 2000;140:643–650. doi: 10.1067/mhj.2000.109644. [DOI] [PubMed] [Google Scholar]
- 13.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290(2):215–21. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amin AA, Jones AM, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. American Heart Journal. 2006;152(5):928–34. doi: 10.1016/j.ahj.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Davidson KW, Reickman N, Lesperance F. Psychological theories of depression: Potential application for the prevention of acute coronary syndrome recurrence. Psychosomatic Medicine. 2004;66:165–173. doi: 10.1097/01.psy.0000116716.19848.65. [DOI] [PubMed] [Google Scholar]
- 16.Ladwig KH, Kieser M, Konig J, Breithardt G, Borggrefe M. Affective disorders and survival after acute myocardial infarction. Results from the post-infarction late potential study. European Heart Journal. 1991;12(9):959–64. [PubMed] [Google Scholar]
- 17.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 18.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 19.Hance M, Carney RM, Freedland KE, Skala J. Depression in patients with coronary heart disease. A 12-month follow-up. General Hospital Psychiatry. 1996;18(1):61–5. doi: 10.1016/0163-8343(95)00100-x. [DOI] [PubMed] [Google Scholar]
- 20.Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362:604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 21.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) Journal of the American College of Cardiology. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatric Services. 2004;55(12):1379–85. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 24.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 25.Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatric Quarterly. 2007;78:3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- 26.Melfi CA, Croghan TW, Hanna MP, Robinson RL. Racial variation in antidepressant treatment in a Medicaid population. Journal of Clinical Psychiatry. 2000;61(1):16–21. doi: 10.4088/jcp.v61n0105. [DOI] [PubMed] [Google Scholar]
- 27.Minsky S, Vega W, Miskimen T, Gara M, Escobar J. Diagnostic patterns in Latino, African American, and European American psychiatric patients. Archives of General Psychiatry. 2003;60(6):637–44. doi: 10.1001/archpsyc.60.6.637. [DOI] [PubMed] [Google Scholar]
- 28.Sirey JA, Meyers BS, Bruce ML, Alexopoulos GS, Perlick DA, Raue P. Predictors of antidepressant prescription and early use among depressed outpatients. American Journal of Psychiatry. 1999;156(5):690–6. doi: 10.1176/ajp.156.5.690. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Beamesderfer A. Assessment of depression: The depression inventory. In: Pichot P, editor. Modern problems in pharmacopsychiatry. 1974. pp. 151–69. [DOI] [PubMed] [Google Scholar]
- 30.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- 31.Harrell FE. Regression Modeling Strategies: With applications to linear model, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 32.Peduzzi PN, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology. 1996;49:1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 33.Rubin DB. Estimating causal effects in large data sets using propensity scores. Annal of Internal Medicine. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 34.Murray CJ, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Medicine/Public Library of Science. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005;111(10):1332–6. doi: 10.1161/01.CIR.0000158134.24860.91. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC) Prevalence of heart disease--United States, 2005. MMWR - Morbidity & Mortality Weekly Report. 2007;56(6):113–8. [PubMed] [Google Scholar]
- 37.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C. Depression as a risk factor for coronary artery disease: Evidence, mechanisms, and treatment. Psychosomatic Medicine. 2004;66:305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 38.Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB. Who is at risk of nondetection of mental health problems in primary care? Journal of General Internal Medicine. 2000;15(6):381–8. doi: 10.1046/j.1525-1497.2000.12088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooper-Patrick L, Powe NR, Jenckes MW, Gonzales JJ, Levine DM, Ford DE. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12(7):431–8. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 41.Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Social Science & Medicine. 1987;24(3):187–96. doi: 10.1016/0277-9536(87)90046-3. [DOI] [PubMed] [Google Scholar]
- 42.Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. Journal of General Internal Medicine. 2000;15(8):527–34. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu TW, Snowden LR, Jerrell JM, Nguyen TD. Ethnic populations in public mental health: services choice and level of use. American Journal of Public Health. 1991;81(11):1429–34. doi: 10.2105/ajph.81.11.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Skaer TL, Sclar DA, Robison LM, Galin RS. Trends in the rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992–1997. Clinical Therapeutics. 2000;22(12):1575–89. doi: 10.1016/s0149-2918(00)83055-6. [DOI] [PubMed] [Google Scholar]
- 45.Strothers HS, III, Rust G, Minor P, Fresh E, Druss B, Satcher D. Disparities in antidepressant treatment in Medicaid elderly diagnosed with depression. Journal of the American Geriatrics Society. 2005;53:456–461. doi: 10.1111/j.1532-5415.2005.53164.x. [DOI] [PubMed] [Google Scholar]
- 46.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion--Healthy People 2010. Nasnewsletter. 2000;15(3):3. [PubMed] [Google Scholar]