Abstract
H5N1 highly pathogenic avian influenza viruses evolved into several clades, leading to appreciably distinct antigenicities of their hemagglutinins. As such, candidate H5N1 pre-pandemic vaccines for human use should be sought. Here, to evaluate fundamental immunogenic variations between H5N1 vaccines, we prepared four inactivated H5N1 test vaccines from different phylogenetic clades (clade 1, 2.1, 2.2, and 2.3.4) in accordance with the WHO recommendation, and tested their cross-clade immunity in a mouse model by vaccination followed by challenge with heterologous virulent viruses. All H5N1 vaccines tested provided full or partial cross-clade protective immunity, except one clade 2.2-based vaccine, which did not protect mice from clade 2.3.4 virus challenge. Among the test vaccines, a clade 2.1-based vaccine possessed the broadest-spectrum cross-immunity. These results suggest that currently stockpiled pre-pandemic vaccines, especially clade 2.1-based vaccines, will likely be useful as backup vaccines in a pandemic situation, even one involving antigenic-drifted viruses.
1. Introduction
Since the outbreak in humans of H5N1 influenza A virus in 1997, these viruses have continued to exert a growing toll, with more than 240 confirmed fatal human cases (http://www.who.int/csr/disease/avian_influenza/en/). With the re-emergence of H5N1 virus in humans in 2003, the epidemic regions have expanded from Asia to Europe, the Middle-East and Africa, raising concerns over a possible influenza pandemic [1]. In the event of such a pandemic, vaccination is one of the most potent methods of protection against this deadly threat. Outbreaks and the pandemic potential of H5N1 viruses have, for this reason, led to stockpiling of H5N1 pre-pandemic inactivated vaccines for human use in many countries.
The considerable diversity in hemagglutinin (HA) antigenicity among the H5N1 viruses, which transpired as a result of naturally occurring genetic alterations, has led to the creation of distinct clades and subclades [2]. It is difficult to predict which H5N1 virus could become a pandemic virus. Moreover, current H5N1 inactivated vaccines show low immunogenicity in humans [3], such that antigenic matching of vaccine viruses to a pandemic virus would be required for efficient protection. Therefore, the World Health Organization (WHO) now recommends the stockpiling of a panel of vaccines with HA antigenic variations, including clade 1 viruses, which have circulated mainly in Southeast Asia, as well as clade 2.1, 2.2, and 2.3.4 viruses, which are circulating predominantly in Indonesia, Asia, Europe and Africa, and Asian countries including China, respectively, as pre-pandemic vaccines [4]. Previously, the HA antigenicities of H5N1 viruses were characterized by using polyclonal and monoclonal antibodies, revealing clade/subclade-dependent antigenic variations, which included cross-reactivity to each other to various extents [4–9]. However, systemic evaluation of the immunogenic relationship of H5N1 vaccines, including cross-clade protection, has not been carried out using animal models, with the exception of some attributive cross-protection analyses between limited clades, such as clade 1 and 2.1 viruses [6, 10–15].
In this study, we prepared four H5N1 test vaccines, associated with clade 1, 2.1, 2.2, and 2.3.4 viruses, immunized mice with each vaccine and then challenged them with homologous as well as heterologous virulent viruses of different clades to evaluate fundamental immunogenic variations between H5N1 viruses in a mouse model.
2. Materials and methods
2.1. Cells
Madin-Darby canine kidney (MDCK) cells were grown in minimal essential medium (MEM) with 5% newborn calf serum. 293T human embryonic kidney cells were maintained in Dulbecco’s modified Eagle’s minimal essential medium (DMEM) with 10% fetal calf serum. Cells were maintained at 37 °C in 5% CO2.
2.2. Viruses
The H5N1 A/Vietnam/30259/04 (VN30259; clade 1), A/Indonesia/3006/05 (Indo3006; clade 2.1), A/whooper swan/Mongolia/4/05 (Mongolia4; clade 2.2), and A/Vietnam/30850/05 (VN30850; clade 2.3.4) viruses were selected as test vaccine strains. Each of these test vaccines possesses only a single amino acid difference in its HA1 relative to that of the WHO-recommended vaccine strain of each corresponding clade [S123P substitution from A/Vietnam/1194/04 (clade1), P141S from A/Indonesia/5/05 (clade2.1), D54N from A/whooper swan/Mongolia/244/05 (clade 2.2), and V265M from A/Anhui/1/05 (clade 2.3.4)], strongly suggesting essentially the same or very closely related antigenicity between our strains and the reference strains. The four H5N1 and A/Aichi/2/68 (H3N2; Aichi) strains were propagated in 10-day-old embryonated chicken eggs at 37 °C for 48 h, after which time the allantoic fluids containing viruses were harvested. All experiments with these infectious viruses were carried out in a Biosafety Level 3 containment laboratory. The WHO-recommended vaccine seed virus, NIBRG-14 (PR8/VN1194 6:2 reassortant containing modified avirulent-type HA and NA derived from the A/Vietnam/1194/04 strain), was the kind gift of Drs. J. Wood and J. Robertson at the National Institute for Biological Standards and Control, UK.
2.3. Construction of plasmids and reverse genetics
To generate reassortants of influenza A viruses, we used plasmid-based reverse genetics [16]. Viral RNA was extracted from the allantoic fluids by using a commercial kit (ISOGEN LS, Nippon Gene) and was converted to cDNA by using reverse transcriptase (SuperScript III; GIBCO-BRL) and primers containing the consensus sequences of the 3-prime ends of the RNA segments for the H5 viruses. The full-length cDNAs were then PCR-amplified with ProofStart polymerase (QIAGEN) and segment-specific primer pairs, and cloned into a plasmid under the control of the human polymerase I promoter and the mouse RNA polymerase I terminator (PolI plasmids). By inverse PCR using back-to-back primer pairs followed by ligation, we altered the HA gene sequences encoding the cleavage site of the wild-type VN30259, Indo3006, Mongolia4 (RERRRKKR), and VN30850 (RERRRKR) viruses to create the avirulent-type sequence (RETR), as described previously [17]. We also constructed PolI-VN30259NA, PolI-Mong4NA, PolI-Indo3006NA, and pPolI-VN30850NA plasmids containing the NA genes, using RT-PCR with N1-specific primers. All of these constructs were sequenced to verify the absence of unwanted mutations. Primer sequences are available upon request.
We also used our previously produced series of PolI constructs, derived from PR8(UW), for reverse genetics [18]. Plasmids expressing PR8 NP, PA, PB1, or PB2 under the control of the chicken β-actin promoter were used for all reverse genetics experiments. Briefly, PolI plasmids and protein-expressing plasmids were mixed with a transfection reagent, Trans-IT 293T (Panvera), incubated at room temperature for 15 min, and then added to 293T cells. Transfected cells were incubated in Opti-MEM I (GIBCO-BRL) for 48 h. Supernatants containing infectious viruses were then harvested and propagated in 10-day-old embryonated chicken eggs at 37 °C for 48 h, after which time the allantoic fluids containing virus were harvested and stored at −80 °C until use.
2.4. Properties of viral replication in embryonated chicken eggs
Virus was inoculated into the allantoic cavity of embryonated chicken eggs (10-day-old), and incubated at 33 °C for 48 h. Virus in the allantoic fluids was then titrated by using an MDCK plaque assay to determine plaque forming unit (PFU)/ml of virus.
2.5. Monoclonal antibody production
Female BALB/c mice (4-week-old) were immunized intraperitoneally twice with the purified vaccine viruses plus Ribi adjuvant (Corixa Corp.), and then boosted with the same antigen intravenously 4 weeks later. Three days after boosting, spleens from the mice were collected, homogenized into single cell suspensions, and fused with Sp2/0-Ag14 myeloma. Hybridomas were screened for monoclonal antibod (mAb) production by using a hemagglutination-inhibition (HI) assay with chicken red blood cells. Hybridoma-producing mAbs were then cloned by limiting dilutions. Mouse mAbs were prepared by injecting hybridomas into the peritoneal cavity of BALB/c mice and collecting the ascites.
2.6. Preparation of inactivated test vaccines
Virus was propagated in the allantoic fluids of embryonated chicken eggs and purified concisely through a 25% sucrose cushion by ultracentrifugation in an SW32Ti rotor (Beckman) at 27,000 rpm (100,000 × g) for 2 hr at 4 °C. Pellets were resuspended in phosphate-buffered saline (PBS). The HA concentration of each virus was determined as previously described [6, 18]. Briefly, the protein concentration of the purified viruses was measured by using a Micro BCA Protein assay kit (PIERCE). Proteins of the purified viruses were then separated by SDS-polyacrylamide gel electrophoresis on a 10%–20% gel and stained with Coomassie brilliant blue, demonstrating more than 95% purity of the virus (data not shown). The gel image was captured and analyzed by using a CS analyzer (ATTO, Tokyo), and the ratio of HA protein to total viral protein was determined. Purified viruses were diluted to 1μg of HA in PBS and treated with 1% formalin (final concentration; 0.1%) at 4 °C for 1 week for inactivation of infectivity. Virus inactivation was confirmed by the absence of detectable infectious virus following inoculation of the vaccines into eggs.
2.7. Experimental infections
Four-week-old female BALB/c mice were subcutaneously inoculated with each vaccine as 0.2 ml of formalin-inactivated virus (15 μg of HA) in PBS. For challenge experiments, mice were intranasally infected with 100 MLD50 (50% mouse lethal dose) of wild-type H5N1 viruses (1 × 103, 1.8 × 104, 7.5 × 102, or 1 × 103 PFU for VN30259, Indo3006, Mongolia4, or VN30850 virus, respectively) under anesthesia with sevoflurane 4 weeks after the immunization. The mice were monitored daily for survival for the next 14 days. Three days later, several of the challenged mice were euthanized to determine the virus titers in their lungs and nasal turbinates. Serum samples were collected from surviving mice on day 14 post-infection.
2.8. Statistical analysis
All comparisons of the infectivity titers relied on Student’s t-test with two tailed analysis to determine statistically significant differences.
3. Results
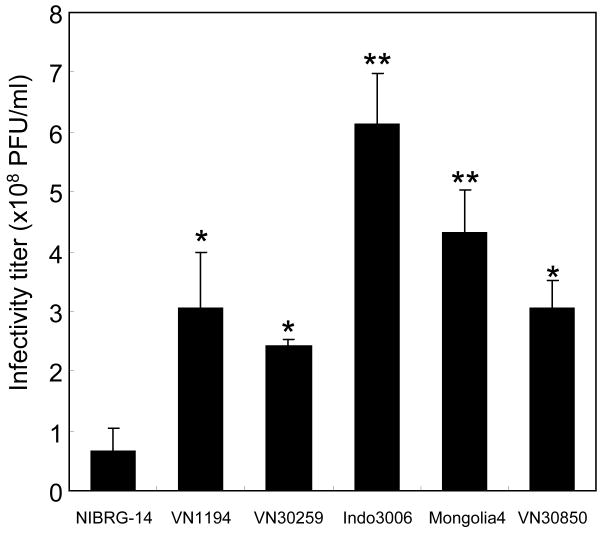
3.1. Growth properties of PR8/H5N1 6:2 reassortants in embryonated chicken eggs
We successfully generated four PR8/H5N1 6:2 reassortants bearing modified avirulent-type HA (mHA) and NA derived from different phylogenetic clade H5N1 viruses, namely VN30259 (clade 1), Indo3006 (clade 2.1), Mongolia4 (clade 2.2), and VN30850 (clade 2.3.4), by reverse genetics. We assessed their growth properties in embryonated chicken eggs, which is the main substrate for influenza vaccine production (Fig. 1). The virus NIBRG-14 [bearing mHA and NA derived from VN1194 and its remaining genes from PR8(Cambridge)] exhibited significantly poorer growth than our 6:2 reassortant (VN1194) that possesses identical mHA and NA to that of NIBRG-14 but has PR8(UW) as its background, reproducing our previous result of more than 4-fold greater growth of our reassortant relative to NIBRG-14 [18]. Similarly, all four reassortants with the PR8(UW) background grew significantly more efficiently compared to NIBRG-14 (p<0.01, Student’s t-test). Of these, the Indo3006 and Mongolia4 viruses replicated with much higher titers than even the VN1194 virus (p=0.001 and p=0.025, respectively). These results support out previous findings that PR8(UW) is superior to PR8(Cambridge) as a donor virus for the construction of H5N1 vaccine seeds.
Fig. 1.
Growth properties of vaccine seed viruses in eggs. Viral titers (PFU/ml) of the PR8/H5N1 6:2 reassortants were determined 48 h post-inoculation. Data are reported as mean titers with standard deviations for N ≥ 3 eggs inoculated with each virus. Viruses with significant growth enhancement compared with NIBRG-14 or VN1194 (p<0.05, Student t-test with two-tail analysis) are shown by an asterisk (*) or double asterisk (**), respectively.
3.2. Analysis of antigenic cross-reactivity of H5N1 viruses using mAbs
As an initial analysis of H5N1 virus HA antigenicity, mAbs were raised against each clade virus and their HI reactivity to heterologous viruses of different clades was tested (Table 1). The mAb-containing mouse ascites were treated with receptor-destroying enzyme (RDEII, Denka Seiken) prior to the HI assay. Viruses of each clade reacted with mAbs produced against viruses of the same clade with high titers, indicating clade-dependent antigenicity. In addition, cross-reactivity among the mAbs was observed beyond the clades; for example mAb A1A1, raised against clade 1 virus, and mAb G2H, raised against clade 2.2 virus, both reacted with every clade virus tested, demonstrating the presence of a common antigenic epitope. However, the cross-reactive titers were not always high to all clades; for example, A1A1 reacted more poorly to Mongolia4 virus and G2H to VN30850 than to other clade viruses, suggesting some limitation to the common epitope among H5N1 viruses. By contrast, high cross-reactive HI titers suggested the presence of definitively common epitopes between clade 1 and 2.2 viruses (with mAb A3C9), or clade 2.1 and 2.2 viruses (with E4E6). Overall, our data confirm the presence of HA antigenic variations among H5N1 viruses.
Table 1.
Antigenic characterization of H5N1 vaccine viruses using monoclonal antibodies in an HI assay.
| HI titer of monoclonal antibodya |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virus | Clade | α-VN1203 (clade 1) | α-VN30262 (clade 1) | α-VN3030 (clade 1) | α-Indo3006 (clade 2.1) | α-Mongolia4 (clade 2.2) |
α-VN30850 (clade 2.3.4) |
||||||||||
| A1A1 | A1C1 | A1H3 | A3C9 | A3D9 | C1G12 | C3E10 | C4D11 | D2B2 | D3E9 | E2C12 | E4A4 | E4B2 | E4E6 | G2Hb | F1F1 | ||
| VN30259 | 1 | ≥8192 | ≥8192 | ≥8192 | ≥8192 | ≥8192 | 2048 | ≥8192 | 512 | ≥8192 | ≥8192 | 64 | <16 | 16 | <16 | 512 | <16 |
| Indo3006 | 2.1 | 4096 | 512 | 256 | <16 | <16 | 16 | 512 | <16 | 64 | 128 | 4096 | 2048 | 2048 | ≥8192 | 512 | <16 |
| Mongolia4 | 2.2 | 128 | <16 | <16 | ≥8192 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | ≥8192 | 512 | <16 |
| VN30850 | 2.3.4 | 4096 | 1024 | 256 | <16 | 64 | 32 | 256 | <16 | 1024 | 256 | <16 | <16 | 128 | <16 | 16 | 2048 |
HI titers to homologous viruses are indicated in bold-face.
Monoclonal antibody was obtained from cell culture supernatant.
3.3. Protective immunity of test vaccines to heterologous lethal challenge by H5N1 virus
Despite the antigenic variations revealed by our mAb analysis, we wanted to further assess the extent of the cross-protective immunity of our H5N1 test vaccines. We, therefore, immunized mice with each whole-virion inactivated vaccine and challenged them with homologous or heterologous viruses of several clades (Fig. 2). Since we want to evaluate the authentic immunogenicity of the vaccines, we did not use any adjuvants in this experiment. In all groups, vaccinated mice completely resisted the lethal challenge of each homologous virus; no mouse died, whereas all of the control mice immunized with PBS or H3N2 virus vaccine (Aichi) died within 9 days of the challenge. In terms of cross-protection, 50% of VN30259 (clade1) vaccine-immunized mice died following VN30850 (clade 2.3.4) virus challenge, although all of them survived challenges with the other two H5N1 viruses [Indo3006 (clade 2.1) and Mongolia4 (clade 2.2) viruses]. Indo3006 (clade 2.1) vaccine-immunized mice completely resisted lethal challenge with all H5N1 viruses, including the three heterologous ones. Mongolia4 (clade 2.2) vaccine-immunized mice succumbed to VN30850 (clade 2.3.4) virus challenge, but survived challenges with the other two clade viruses. As was seen with the VN30259 (clade 1) and Mongolia4 (clade 2.2) vaccines, a proportion of VN30850 (clade 2.3.4) vaccine-immunized mice succumbed to VN30259 (clade 1) and Mongolia4 (clade 2.2) virus challenge (50% and 25% of mice died, respectively). These results demonstrate the presence of cross-protective immunity among these H5N1 viruses, although we did observe several cases of partial cross-protective immunity, for example with clade 2.3.4-based vaccination. Of note, a complete lack of cross-protection was observed with clade 2.2-based vaccination followed by clade 2.3.4 virus challenge.
Fig.2.
Survival of vaccinated mice following lethal challenge with H5N1 viruses. Groups of four mice were immunized with inactivated vaccines of VN30259 (A), Indo3006 (B), Mongolia4 (C), VN30850 (D), PBS control (F), and H3N2 virus Aichi (E). Four week after immunization, the mice were intranasally infected with 100 MLD50 of wild-type H5N1 viruses; VN30259 (×), Indo3006 (^), Mongolia4 (▴), or VN30850 (□). Mice were monitored daily for 14 days to determine mortality rates.
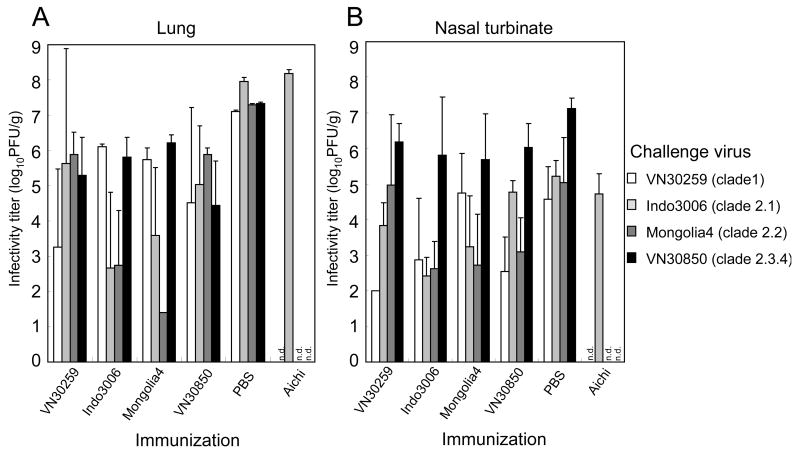
For further evaluation of cross-protective effects, we determined virus titers of lungs and nasal turbinates in mice challenged with H5N1 viruses on day 3 post-infection (Fig. 3). Virus titers in the lungs of all vaccinated mice were 10 times lower than those of PBS control mice, indicating the presence of cross-protective immunity. As expected, the titers of homologous virus-challenged mice were lower, albeit not significantly in some cases, than those of heterologous virus-challenged mice, indicating that a reduction in virus titer in the lung may be an indicator for the extent of vaccine immunogenicity. Interestingly, significantly lower titers were observed in the lungs of Indo3006-vaccinated/Mongolia4-challenged mice (p<0.05; compared to both Indo3006-vaccinated/VN30259-challenged and Indo3006-vaccinated/VN30850-challenged mice) and in Mongolia4-vaccinated/Indo3006-challenged mice (p<0.05; compared to Mongolia4-vaccinated/VN30850-challenged mice), suggesting strong cross-protective immunity between these two viruses (clade 2.1 and 2.2 viruses). In the nasal turbinates, similar trends in virus titers to those seen in the lungs were observed, except for the VN30850-challenged mice, in which a high titer was evident even with homologous vaccination. Notably, the VN30850 virus replicated much better than the other three H5N1 viruses in the control (PBS) mice. These results indicate that vaccination of the inactivated H5N1 test vaccines could be effective to suppress virus growth in the lungs, but to only a limited extent the in nasal turbinates of the mice.
Fig.3.
Replication of wild-type H5N1 challenge viruses in the lungs and nasal turbinates of the mice immunized with homologous or heterologous H5N1 vaccines at day 3 post-challenge. Virus titers (PFU/ml) of each challenge virus in the lungs (A) and nasal turbinates (B) were determined by use of MDCK cells. Each bar indicates mean titers with standard deviations for N ≥ 3 samples from each mouse group immunized with the indicated test vaccine.
In addition, we collected mouse sera from mice that survived immunization/challenge with each homologous vaccine/virus, at 14 days post-challenge. Using these sera, we examined the antigenic cross-reactivities among H5N1 viruses in our HI assay (Table 2). The collected sera were treated with RDE prior to the experiement. Each serum reacted to the homologous antigens with HI titers ranging from 64 to 512. Strong HI cross-reactivity was observed between anti-Indo3006 (clade 2.1) and anti-Mongolia4 (clade 2.2) viruses. By contrast, there were no HI cross-reactivities detected between VN30850 (clade 2.3.4) and VN30259 (clade 1) or Indo3006 (clade 2.1) viruses. For other heterologous pairs of virus antigens and antisera, faint cross-reactivities were observed, albeit in a one-way manner for most pairs. These results partially support the survival data shown in Figure 2, although some mice survived even without detectable HI cross-reactive antibodies in their sera post-challenge.
Table 2.
HI antibody titers in antisera against H5N1 viruses.
| HI titers of anti-influenza seraa |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| α-VN30259
|
α-Indo3006
|
α-Mongolia4
|
α-VN30850
|
||||||||||||||
| Virus | Clade | mouse
|
mouse
|
mouse
|
mouse
|
||||||||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | ||
| VN30259 | 1 | 64 | 512 | 512 | 256 | <16 | 16 | 32 | 32 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 |
| Indo3006 | 2.1 | <16 | <16 | <16 | <16 | 256 | 128 | 256 | 256 | 64 | 16 | 64 | 128 | <16 | <16 | <16 | <16 |
| Mongolia4 | 2.2 | <16 | 128 | <16 | 16 | 128 | 128 | 128 | 128 | 128 | 256 | 128 | 128 | <16 | 32 | <16 | <16 |
| VN30850 | 2.3.4 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | <16 | 64 | 64 | 128 | 256 |
Homologous HI titers are indicated in bold face.
4. Discussion
In this study, we produced four H5N1 inactivated vaccines with PR8/H5N1 6:2 reassortants from isolates of different phylogenetic clades (clade 1, 2.1, 2.2, and 2.3.4), based on the WHO-recommended reverse genetics strategy, and assessed their cross-clade antigenicity/immunogenicity by using serological assays and a mouse vaccination/challenge model..Although we detected clear variations in viral HA antigenicity of the H5N1 viruses by serological analyses, any H5N1 test vaccine, except one clade 2.2-based vaccine, gave full or partial protection from lethal challenge with heterologous viruses of different clades, providing cross-clade immunity. These results suggest the utility of currently stockpiled pre-pandemic vaccines as backup vaccines in a pandemic situation even in the face of antigenic drift.
The stockpiling of pre-pandemic vaccines for the worldwide population is desired as we face the pandemic threat of H5N1 viruses. To this end, a more robust system for vaccine manufacturing is also key [19]. We previously reported that our H5N1 vaccine seed viruses with the PR8(UW) donor system replicates much better in chicken embryonated eggs, the only currently approved substrate for influenza vaccine production, than does the WHO-recommended reference seed NIBRG-14 with the PR8(Cambridge) donor [18]. Here, we again found that our vaccine seeds, accommodating mHA and NA derived from the H5N1 isolates of other clades, showed better growth in eggs than the NIBRG-14, confirming the superiority of PR8(UW) as a donor for H5N1 vaccines over PR8(Cambridge).
To assess the cross-clade HA antigenicity of the H5N1 vaccines, we first conducted an HI test with a panel of mAbs, and then with polyclonal sera obtained from vaccinated/challenged mice. Taken together, our results clearly indicate HA antigenic variations and cross-antigenicities among the clades of H5N1 viruses. In particular, we observed the most closely related antigenicity between clade 2.1 and 2.2 viruses, which was supported by cross-protective effects in mice. The broad immunity of these clade vaccines might, therefore, be expected to cover a large proportion of the population. Testing this concept would require the similar evaluation of human sera from vaccinated or infected individuals.
As a pre-clinical test for cross-clade immunity of H5N1 vaccines, here, we used a mouse model due to its practicality for influenza vaccine study; however, additional studies using ferrets or non-human primate models should be conducted to authenticate our observations. We did not use any adjuvant for immunization with the whole-virion inactivated vaccines to avoid any bias for the evaluation of vaccine immunogenicity itself, although it has been established by preclinical and clinical testing that adjuvants such as MF59 and Alum enhance the immunogenicity of some H5N1 inactivated vaccines [20–22]. Here, we found that subcutaneous immunization with a single 15 μg dose of our non-adjuvanted vaccines rendered complete protection from lethal challenge with homologous viruses, prompting us to conduct cross-protective experiments with heterologous viruses of other clades in the same manners. The results showed that Indo3006 (clade 2.1) vaccine-immunized mice fully survived not only homologous but also heterologous virus challenge, suggesting that the Indo3006 (clade 2.1)-based vaccine may possess high cross-reactive immunogenicity to other H5N1 viruses of different clades, tested in this study, as supported by the reciprocal results that all the mice immunized with other clade H5N1 vaccines fully survived Indo3006 virus challenge. In particular, virus titers in the organs of the challenged mice and serological assays demonstrated the most closely related antigenicity between Indo3006 (clade 2.1) and Mongolia4 (clade 2.2) viruses, compared to other clade combinations. By contrast, the VN30850 (clade 2.3.4)-based vaccine showed low cross-immunity to the other viruses tested except Indo3006 (clade 2.1), as confirmed by serological analyses. Clade 1 and 2.1 vaccines have been stockpiled as pre-pandemic vaccines in many countries [4] and now clade 2.2 and 2.3.4 vaccines are also being produced and stockpiled. Our results suggest that stockpiling of clade 2.3.4 should take priority over clade 2.2 vaccines, to cover a wide range of H5 antigenicities.
As a matter of course, there might be concern with the appearance of antigenic-drifted viruses, whose antigenicity mismatches those of the vaccine viruses. In this study, we generated four vaccines based on isolates in 2004 and 2005 from different phylogenetic clades. Currently, not only clade 1, 2.1, 2.2, and 2.3.4 viruses but also other clade viruses (such as clade 2.3.2 virus) have circulated in Southeast Asia [4, 9]. Previous reports showed that clade 2.3.2 viruses were antigenically distinct from the four clade viruses tested in this study [4, 9]. Thus, we need to continue to enrich the panel of stockpiled vaccines. Meanwhile, within the same clade, antisera raised against isolates in 2004 or 2005 viruses react to newer isolates (from 2006 or 2007) [4], suggesting that current stockpiled vaccines based on clade 1, 2.1, 2.2, and 2.3.4 would be effective at least for new isolates of those clades.
Although we did not use any adjuvant for immunization with our H5N1 test vaccines in this study, clinical studies indicate that adjuvants may be essential to compensate for the low immunogenicity of H5N1 vaccines in humans [20–24]. In other words, adjuvantation with H5N1 vaccines may be required for their cross-clade immunity in humans [24]. Our mAb analyses, and those of others, suggest the presence of a common protective epitope among many H5N1 viruses [9], although this epitope may not be the primary target of the host immune response, as suggested by our finding that some vaccines failed to fully protect animals from lethal challenge with heterologous viruses. Therefore, it is likely that adjuvantation even with the clade 2.3.4 vaccines may be needed to induce cross-clade immunity to other clade viruses, contrary to the present result. Nonetheless, we need to continue our efforts to increase the immunogenicity of H5N1 vaccines in the absence of adjuvants. One option is to use live attenuated H5N1 vaccines, which have been already produced, and are now in clinical trials. Such vaccines have the potential to enhance immunogenicity and efficiently induce cross-immunity to heterologous viruses, since mucosal IgA antibodies induced by a live virus infection have been reported to be more cross-reactive than serum IgG antibodies induced by inactivated vaccines [14, 25].
Our present data indicate that immunization with H5N1 inactivated vaccines reduces virus yields in the lungs of infected animals and decreases mortality, but may not reduce virus yields in the nasal turbinates of some strains. Indeed, it is interesting to note that the VN30850 (clade 2.3.4) challenge virus replicated with higher viral titers (significantly in most cases; p<0.05; except for 30259-vaccinated/Mongolia4-challenged, Mongolia4-vaccinated/VN30259-challenged, and VN30850-vaccinated/VN30850-challenged cases) than those of the other three viruses in the nasal turbinates of not only the control (PBS) mice but also the vaccinated mice, including homologous vaccine-immunized mice. By contrast, this phenomenon was not observed in the lungs. In such a case, vaccination may have no effect on human-to-human virus transmission in a pandemic situation. In our previous report, an H5N1 virus possessing a lysine residue at position 627 of PB2 replicated with a higher viral titer in mouse nasal turbinate than its counterpart possessing a glutamate residue at this position [26]. Of the four strains used here, VN30850, VN30259, and Mongolia4 viruses possess lysine at this position, whereas Indo3006 possesses glutamate, indicating that the outstanding growth of the VN30850 virus in nasal turbinates likely resulted from some still undefined factor(s).
In conclusion, we found that the clade 2.1-based vaccine possesses the broadest-spectrum cross-immunity among H5N1 viruses tested in this study, compared to other clade-based vaccines, and propose the preferential stockpiling of this clade of pre-pandemic vaccines.
Acknowledgments
We thank Drs. J.M. Wood and J.S. Robertson (National Institute for Biological Standards and Control, UK), for NIBRG-14 virus, and S. Watson for editing the manuscript. This work was supported, in part, by Grants-in-Aid for Specially Promoted Research and for Scientific Research (B); by a Contract Research Fund for Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases; and by the Special Coordination Funds for Promoting Science and Technology from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, and by National Institute of Allergy and Infectious Diseases Public Health Service research grants, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Horimoto T, Kawaoka Y. Influenza: lessons from past pandemics, warnings from current incidents. Nat Rev Microbiol. 2005;3(8):591–600. doi: 10.1038/nrmicro1208. [DOI] [PubMed] [Google Scholar]
- 2.WHO. H5N1 Evolution Working Group poster, Toronto, 2007. [cited; Available from: http://www.who.int/entity/csr/disease/influenza/nomen.ppt]
- 3.Treanor JJ, Campbell JD, Zangwill KM, Rowe T, Wolff M. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. N Engl J Med. 2006;354(13):1343–51. doi: 10.1056/NEJMoa055778. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Antigenic and genetic characterization of H5N1 viuses and candidate H5N1 vaccine viruses developed for potential use as human vaccines, 2008. [cited; Available from: http://www.who.int/entity/csr/disease/avian_influenza/guidelines/H5VaccineVirusUpdate20080214.pdf]
- 5.Chen H, Smith GJ, Li KS, Wang J, Fan XH, Rayner JM, et al. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc Natl Acad Sci U S A. 2006;103(8):2845–50. doi: 10.1073/pnas.0511120103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ninomiya A, Imai M, Tashiro M, Odagiri T. Inactivated influenza H5N1 whole-virus vaccine with aluminum adjuvant induces homologous and heterologous protective immunities against lethal challenge with highly pathogenic H5N1 avian influenza viruses in a mouse model. Vaccine. 2007;25(18):3554–60. doi: 10.1016/j.vaccine.2007.01.083. [DOI] [PubMed] [Google Scholar]
- 7.Kaverin NV, Rudneva IA, Govorkova EA, Timofeeva TA, Shilov AA, Kochergin-Nikitsky KS, et al. Epitope mapping of the hemagglutinin molecule of a highly pathogenic H5N1 influenza virus by using monoclonal antibodies. J Virol. 2007;81(23):12911–7. doi: 10.1128/JVI.01522-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashyap AK, Steel J, Oner AF, Dillon MA, Swale RE, Wall KM, et al. Combinatorial antibody libraries from survivors of the Turkish H5N1 avian influenza outbreak reveal virus neutralization strategies. Proc Natl Acad Sci U S A. 2008;105(16):5986–91. doi: 10.1073/pnas.0801367105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu W, Chen Y, Wang P, Song W, Lau S, Rayner J, et al. Antigenic profile of avian H5N1 viruses in Asia from 2002 to 2007. J Virol. 2008;82(4):1798–807. doi: 10.1128/JVI.02256-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baras B, Stittelaar KJ, Simon JH, Thoolen RJ, Mossman SP, Pistoor FH, et al. Cross-protection against lethal H5N1 challenge in ferrets with an adjuvanted pandemic influenza vaccine. PLoS ONE. 2008;3(1):e1401. doi: 10.1371/journal.pone.0001401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruat C, Caillet C, Bidaut A, Simon J, Osterhaus AD. Vaccination of macaques with adjuvanted formalin-inactivated influenza A virus (H5N1) vaccines: protection against H5N1 challenge without disease enhancement. J Virol. 2008;82(5):2565–9. doi: 10.1128/JVI.01928-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watanabe T, Watanabe S, Kim JH, Hatta M, Kawaoka Y. Novel approach to the development of effective H5N1 influenza A virus vaccines: use of M2 cytoplasmic tail mutants. J Virol. 2008;82(5):2486–92. doi: 10.1128/JVI.01899-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kistner O, Howard MK, Spruth M, Wodal W, Bruhl P, Gerencer M, et al. Cell culture (Vero) derived whole virus (H5N1) vaccine based on wild-type virus strain induces cross-protective immune responses. Vaccine. 2007;25(32):6028–36. doi: 10.1016/j.vaccine.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suguitan AL, Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, et al. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 2006;3(9):e360. doi: 10.1371/journal.pmed.0030360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bright RA, Carter DM, Crevar CJ, Toapanta FR, Steckbeck JD, Cole KS, et al. Cross-clade protective immune responses to influenza viruses with H5N1 HA and NA elicited by an influenza virus-like particle. PLoS ONE. 2008;3(1):e1501. doi: 10.1371/journal.pone.0001501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neumann G, Watanabe T, Ito H, Watanabe S, Goto H, Gao P, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci U S A. 1999;96(16):9345–50. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horimoto T, Takada A, Fujii K, Goto H, Hatta M, Watanabe S, et al. The development and characterization of H5 influenza virus vaccines derived from a 2003 human isolate. Vaccine. 2006;24(17):3669–76. doi: 10.1016/j.vaccine.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Horimoto T, Murakami S, Muramoto Y, Yamada S, Fujii K, Kiso M, et al. Enhanced growth of seed viruses for H5N1 influenza vaccines. Virology. 2007;366(1):23–7. doi: 10.1016/j.virol.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horimoto T, Kawaoka Y. Strategies for developing vaccines against H5N1 influenza A viruses. Trends Mol Med. 2006;12(11):506–14. doi: 10.1016/j.molmed.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Bresson JL, Perronne C, Launay O, Gerdil C, Saville M, Wood J, et al. Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: phase I randomised trial. Lancet. 2006;367(9523):1657–64. doi: 10.1016/S0140-6736(06)68656-X. [DOI] [PubMed] [Google Scholar]
- 21.Lin J, Zhang J, Dong X, Fang H, Chen J, Su N, et al. Safety and immunogenicity of an inactivated adjuvanted whole-virion influenza A (H5N1) vaccine: a phase I randomised controlled trial. Lancet. 2006;368(9540):991–7. doi: 10.1016/S0140-6736(06)69294-5. [DOI] [PubMed] [Google Scholar]
- 22.Bernstein DI, Edwards KM, Dekker CL, Belshe R, Talbot HK, Graham IL, et al. Effects of adjuvants on the safety and immunogenicity of an avian influenza H5N1 vaccine in adults. J Infect Dis. 2008;197(5):667–75. doi: 10.1086/527489. [DOI] [PubMed] [Google Scholar]
- 23.Leroux-Roels I, Borkowski A, Vanwolleghem T, Drame M, Clement F, Hons E, et al. Antigen sparing and cross-reactive immunity with an adjuvanted rH5N1 prototype pandemic influenza vaccine: a randomised controlled trial. Lancet. 2007;370(9587):580–9. doi: 10.1016/S0140-6736(07)61297-5. [DOI] [PubMed] [Google Scholar]
- 24.Leroux-Roels I, Bernhard R, Gerard P, Drame M, Hanon E, Leroux-Roels G. Broad clade 2 cross-reactive immunity induced by an adjuvanted clade 1 rH5N1 pandemic influenza vaccine. PLoS ONE. 2008;3(2):e1665. doi: 10.1371/journal.pone.0001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu X, Edwards LE, Desheva JA, Nguyen DC, Rekstin A, Stephenson I, et al. Cross-protective immunity in mice induced by live-attenuated or inactivated vaccines against highly pathogenic influenza A (H5N1) viruses. Vaccine. 2006;24(44–46):6588–93. doi: 10.1016/j.vaccine.2006.05.039. [DOI] [PubMed] [Google Scholar]
- 26.Hatta M, Hatta Y, Kim JH, Watanabe S, Shinya K, Nguyen T, et al. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 2007;3(10):1374–9. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]