Abstract
Background
Generally, the safety of transfusion terapies for patients depends in part on the distribution of the blood products. The prevention of adverse events can be aided by technological means, which, besides improving the traceability of the process, make errors less likely. In this context, the latest frontier in automation and computerisation is the remote-controlled, automated refrigerator for blood storage.
Materials and methods
Computer cross-matching is an efficient and safe method for assigning blood components, based on Information Technology applied to typing and screening. This method can be extended to the management of an automated blood refrigerator, the programme of which is interfaced with the Transfusion Service’s information system. The connection we made in our Service between EmoNet® and Hemosafe® enables real-time, remote-controlled management of the following aspects of blood component distribution: a) release of autologous and allogeneic units already allocated to a patient, b) release of available units, which can be allocated by remote-control to known patients, in the presence of a valid computer cross-match, c) release of O-negative units of blood for emergencies.
Results
Our system combines an information database, which enables computer cross-matching, with an automated refrigerator for blood storage with controlled access managed remotely by the Transfusion Service. The effectiveness and safety of the system were validated during the 4 months of its routine use in the Transfusion Service’s outpatient department.
Conclusions
The safety and efficiency of the distribution of blood products can and must be increased by the use of technological innovations. With the EmoNet®/Hemosafe® system, the responsibility for the remote-controlled distribution of red blood cell concentrates remains with the chief of the Transfusion Services, through the use of automated computer procedures and supported by continuous training of technicians and nursing staff.
Keywords: transfusion safety, remote-control, computer cross-match
Introduction
Mistaken identification of recipients and of the units of blood components to transfuse is still the most frequently reported error to the main, international haemovigilance systems. The frequency of such errors, which occur once for every 10,000 units transfused1, can be reduced by various strategies (Table I), such as the use of uniform working procedures, continuous training of staff, and identification of people responsible for transfusion procedures2,3. Another strategy is to use computer systems and barcodes, which are currently employed internationally and in Italy in many stages of the transfusion process, such as identification of the samples on which to carry out pretransfusion tests, labelling units of blood components in compliance with precise legislation4 and identification of the recipient5. The main advantage related to the use of this technology has been the development of computerised management of units and their correct identification and allocation to patients6,7; it has also improved the safety and trackability of the process8 and enabled “type and screen”9 procedures to be introduced into routine practice, as a replacement for the traditional cross-matching10, for all individuals without unusual antibodies11–14. Computerisation has also reduced the permanence of units in the blood refrigerator and reduced their wastage due to expiration15, as well as the number of tests performed per patient transfused, in that the units allocated are those that are actually transfused16.
Table I.
Strategies used to prevent transfusion errors
| Quality system management |
| 1. Working procedures |
| 2. Specific member of ward/department responsible for transfusions |
| Technological approaches |
| 1. Mechanical barriers |
| 2. Barcodes |
| 3. Computerisation |
| 4. Automatic interfaced equipment |
| 5. Anthropometric readers |
| 6. Portable computers and radiofrequency devices |
| 7. Automated infusion pumps |
| 8. Automated blood stores |
The use of informatics seems to be a valid aid for the solution of another very important problem in the field of transfusion medicine, that is, the management of blood components in hospitals that do not have a Transfusion Service or in areas of the hospital located at a great distance from the Transfusion Centre17. The solution to this problem could, in fact, be the use of a remote-controlled, “self-service” refrigerated blood storage, connected by a computer interface to the Transfusion Service’s information system.
At the Transfusion Service of the Carlo Poma Hospital in Mantova, we planned and tested an interface between the EmoNet® transfusion management software and the Hemosafe® remote-controlled, automated, refrigerated blood store, verifying the procedural conditions necessary to make it possible to allocate blood by remote control and enable direct procurement of the units by nursing staff. This report contains the preliminary data from this study, the aim of which was to enable safe allocation of compatible units in hospital areas at a distance from the Transfusion Centre.
Materials and methods
The computer cross-match
The blood bank information system used in our Centre is EmoNet® by INSIEL, which enables computer cross-matching to be carried out following a codified algorithm. Based on the barcode of the accepted sample, the software prevents the allocation of ABO incompatible blood and checks the congruence of the historical data by controlling the results of tests conducted on different samples and at different times.
The software allocates a unit, choosing the one that is most compatible with regards to ABO/Rh blood groups and closest to the end of its shelf-life. Furthermore, at the time of releasing the unit, the programme checks that the allocation label has been attached to the correct bag, by reading the four barcodes: the world donation code (CDM) and blood component-bag-use code (EMC/BAG/USE), which are on the unit, and the unique identification code (CAI) and control code (CDMN), which are on the allocation label. This ‘triple check’ between the CDM and the other three barcodes guarantees that the allocation label is attached to the correct unit.
The automated refrigerated blood storage
The blood storage used in this study was the automated HemoSafe® refrigerator produced by Angelantoni Industrie S.p.A, connected to the EmoNet® management system. This refrigerator stores red blood cells and guarantees controlled release of the units through a computer program. The refrigerator can hold 150 units, contained in 15 individual compartments on 10 rotating shelves. The system can release: a) units of autologous or homologous blood already allocated by the ‘type and screen’ procedure and carrying a double label, that is, the unit’s label (CDM + EMC/BAG/USE) and the allocation label (CDMN + EMC/BAG/USE + CAI), b) compatible units in the refrigerator that have not yet been allocated to any patients, c) universally compatible units of O negative blood. As the fridge is filled, the system carries out all the necessary controls concerning the validity and the expiry of the units, and the time taken for the transport of the unit from the main refrigerator in the Transfusion Centre to the peripheral site; the system also checks the validity of the allocation with respect to established rules (computer cross-matching or serological compatibility tests), and checks the allocation label with the “triple check” at release.
Furthermore, at the time of release, verifications related to the allocation of units and to the release of units in emergencies are carried out.
EmoNet®/Hemosafe® integration
The operations of withdrawing and delivering units are guided and controlled by the EmoNet® system, in order to maintain the same levels of safety and the same rules as those imposed by the Transfusion Service (the computer cross-match rules); the only function than can be carried out independently by Hemosafe® is the release of O Rh-negative blood to use in the case of emergencies without compatibility tests. Regarding the remote allocation of units, EmoNet®, besides checking the validity of the “type and screen”, lists the compatible units in Hemosafe®, according to a predetermined order based on management logics (levels of ABO/Rh compatibility, expiry date of the unit) established by an algorithm produced by the EmoNet® manager. The first unit proposed by EmoNet® as compatible, with its exact location in the Hemosafe® fridge, can only be distributed by the system if there is a transfusion request for a subject with a unique identification code (CAI) already linked with the request. A printer connected to the Hemosafe® fridge prints the allocation label (Figure 1), which is identical to the one that is printed in the Transfusion Centre at the time of withdrawing the blood; this allows the staff member who withdraws the allocated unit to carry out the “triple check” with the label on the bag (Figure 2) using the the Hemosafe® refrigerator’s barcode reader. During the allocation procedure, the validity of the unit, the expiry of the pretransfusion tests associated with the request and any treatments related to the transfusion request (filtration, irradiation or other) are checked.
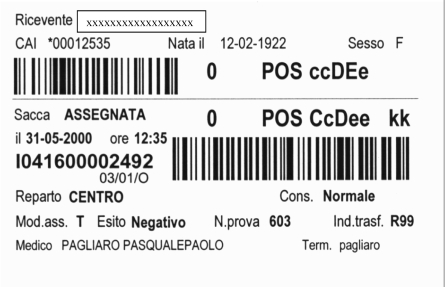
Figure 1.
An example of allocation label.
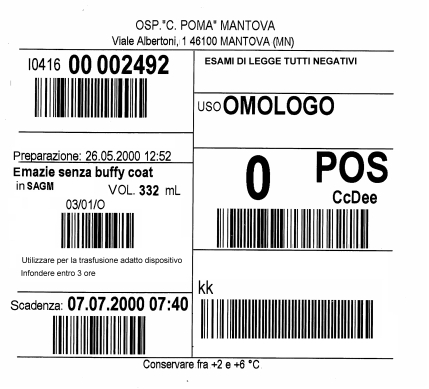
Figure 2.
The blood unit label with the barcodes necessary for computer cross-match procedure.
Unused units released from Hemosafe® can be replaced by the staff in the peripheral site within a determined time, maintaining the allocation of the unit for the same patient; otherwise, the unit can only be cancelled by the Transfusion Service. The integrated EmoNet®/Hemosafe® system also allows movement of units between refrigerated blood stores, with temporal tracking of the movements and of the validity of the units. The functional analysis and development of the software were performed by the INSIEL and Angelantoni companies, based on specifications provided by the Transfusion Service (Table II). The refrigerator’s computer is accessible for remote maintenance servicing by the Angelantoni company via internet.
Table II.
Summary of the specifications of the EmoNet®/Hemosafe® interface
|
Practical use of the automated, remote-controlled blood storage
The system is used directly by the nursing staff in the transfusion outpatient clinic connected to our Service for the transfusion of patients with chronic blood disorders who are receiving multiple transfusions (thalassaemia, myelodysplasia). After the request and the relevant samples have been sent to the Transfusion Centre and the ‘type and screen’ tests have been performed, the user of the system is identified (Figure 3). This user is granted access to the compartment of the Hemosafe® fridge that contains the compatible unit allocated by the EmoNet® software. The user prints the release form and those related to the controls before the transfusion. The refrigerator is emptied and refilled with the units of blood each week. The operations carried out by the nursing staff are defined by precise working instructions for nurses (Table III), in an Improvement Plan named Systems under Trial in the Quality of Service Management System, which is certified for its compliance with ISO 9001 regulations (Certificate CSQ n°9122.POMA).
Figure 3.
the user, after identification, accesses to the compartment of the Hemosafe® fridge.
Table III.
Instructions for the use of Hemosafe® (following logging in with user name and password)
| Loading the fridge with units of blood |
|
| Withdrawals of bags allocated by EmoNet® |
|
| Withdrawal of an O Negative unit for an emergency |
|
Method of evaluation
All the operations carried out by Hemosafe® were checked by the staff of the Transfusion Centre and, at the time of the transfusion, by both the nurse and a doctor. Any errors of identification of the patient transfused and the related units were recorded, including those in abnormal situations, such as deliberate attempts to make a mistake, either regarding to the recipient or the allocated units.
Results
In the 4 months (March-June 2006) of routine use of Hemosafe® in the transfusion outpatient clinic, 43 patients were transfused with a total of 235 units of pre-filtered red blood cell concentrates. For ten patients (transfused with 88 units) the allocation criterion was serological compatibility (cross-matching test), while for the other 33 (receiving a total of 247 units) ‘type and screen’ allocation (by computer cross-matching) was used. In addition, five units of serologically compatible units and nine units allocated with the computer cross-match method were cancelled for clinical reasons by the Transfusion Service. In no cases were pre-deposited autologous units distributed. Each week the red blood cell units available in Hemosafe® were renewed, replacing the units that had been transfused and those closest to their expiry date. For the compatible units allocated, the refrigerated blood storage was refilled as needed on the basis of booking of compatible units for multiply transfused patients.
During this period there were no reports of any errors or transfusion reactions, independently of the way the units were allocated. Only once was it necessary to unblock the refrigerator mechanically in order to manually withdraw two units that had passed their shelf-life, left by error in Hemosafe® during one of the periodic filling and emptying sessions.
Discussion
The safety of transfusions depends on the correct performance of all the stages of this complex process18,19, which starts with the collection of blood from a donor and ends with the transfusion of a compatible blood component to a recipient. Many strategies20,21,22 have been proposed to reduce errors. One way of improving transfusion safety is to exploit technological advances, even if many of these (nanotechnology, radiofrequency-based identification systems) are complex and require particular equipment and cannot, therefore, yet be proposed for large-scale use. Given these problems, the main aim is to implement a practical and simple system, which has been designed to prevent errors and make it easy to do the right thing and difficult to do the wrong one3. Among the various possibilities, the use of ‘intelligent’ blood storages23,24,25, connected to management software, seems to be a promising system for reducing errors related to the incorrect identification of the units to be transfused or of the recipient of the allocated units. This problem is particularly important in remote areas of a hospital in which there is substantial use of transfusions (such as an accident and emergency department or a haematology day hospital) or in small hospitals without a Transfusion Service.
The preliminary experience of the Transfusion Service of Carlo Poma Hospital in Mantova has shown that a simple system, such as the Hemosafe® refrigerated blood storage, connected to EmoNet® transfusion management software, is an efficient and safe method for remote-controlled withdrawal and delivery of units of blood by ward nursing staff, without requiring the presence of the graduate staff and technicians of the Transfusion Service. The full benefit of this system should also be verified in emergency situations, such as those occurring in the accident and emergency department, which, because of their characteristic working methods, are more at risk of errors related to the identification of patients and units of blood components.
References
- 1.Linden JV, Wagner K, Voytovich AE, et al. Transfusion errors in New York State: an analysis of ten years’ experience. Transfusion. 2001;40:1207–13. doi: 10.1046/j.1537-2995.2000.40101207.x. [DOI] [PubMed] [Google Scholar]
- 2.EU Directive 2002/98/EC. Available at:http//europa.eu.int/
- 3.Dzik WH, Corwin H, Goodnough LT, et al. Patient safety and blood transfusion: new solutions. Transfus Med Rev. 2003;17:169–80. doi: 10.1016/s0887-7963(03)00017-8. [DOI] [PubMed] [Google Scholar]
- 4.Rockville (MD): U.S. Department of Health and Human Services, Food and Drug Administration, Center for Biologics Evaluation and Research; 1999. United States industry consensus standard for the uniform labeling of blood components using ISBT 128. version 1.2.0. http://webstore.uni.com/unistore/public/productdetails?productId=UNI1052900!EIT. [Google Scholar]
- 5.Pagliaro P, Rebulla P. Transfusion recipient identification. Vox Sang. 2006;91:97–101. doi: 10.1111/j.1423-0410.2006.00783.x. [DOI] [PubMed] [Google Scholar]
- 6.Butch SH. Computerization in the Transfusion Service. Vox Sang. 2002;83:105–10. doi: 10.1111/j.1423-0410.2002.tb05279.x. [DOI] [PubMed] [Google Scholar]
- 7.Miyata S, Kawai T, Yamamoto S, et al. Network computer-assisted transfusion-management system for accurate blood component-recipient identification at the bedside. Transfusion. 2004;44:364–372. doi: 10.1111/j.1537-2995.2004.00652.x. [DOI] [PubMed] [Google Scholar]
- 8.Friedman BA, Oberman HA, Chadwick AR, et al. The maximal surgical blood order schedule and surgical blood use in the United States. Transfusion. 1976;16:380–7. doi: 10.1046/j.1537-2995.1976.16476247063.x. [DOI] [PubMed] [Google Scholar]
- 9.Klein HG, editor. AABB Standards for Blood Banks and Transfusion Services (Standards) 17. Bethesda: American Association of Blood Banks; 1996. p. 33. 15.100; 15.120. [Google Scholar]
- 10.Shulman IA, Maffei LM, Johnson ST, Steiner EA. CAP Today. 1996;10:85–86. [Google Scholar]
- 11.Pinkerton PH, Coovadia AS, Goldstein J. Frequency of delayed haemolytic transfusion reaction following antibody screening and immediate-spin crossmatching. Transfusion. 1992;32:814–7. doi: 10.1046/j.1537-2995.1992.32993110751.x. [DOI] [PubMed] [Google Scholar]
- 12.Butch SH, Judd WJ, Steiner EA, et al. Electronic verification of donor-recipient compatibility: the computer crossmatch. Transfusion. 1994;34:105–9. doi: 10.1046/j.1537-2995.1994.34294143935.x. [DOI] [PubMed] [Google Scholar]
- 13.Judd WJ. Requirements for the electronic crossmatch. Vox Sang. 1998;74 (Suppl 2):409–17. doi: 10.1111/j.1423-0410.1998.tb05450.x. [DOI] [PubMed] [Google Scholar]
- 14.Kuriyan M, Fox E. Pretransfusion testing without serological crossmatch: approaches to ensure patient safety. Vox Sang. 2000;78:113–8. doi: 10.1159/000031160. [DOI] [PubMed] [Google Scholar]
- 15.Georgsen J, Kristensen T. From serological to computer cross-matching in nine hospitals. Vox Sang. 1998;74 (Suppl 2):419–25. doi: 10.1111/j.1423-0410.1998.tb05451.x. [DOI] [PubMed] [Google Scholar]
- 16.Arslan O. Electronic crossmatching. Transf Med Rev. 2006;20:75–9. doi: 10.1016/j.tmrv.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Cheng G. Experiences with “self service” electronic blood banking. Vox Sang. 1998;74 (Suppl 2):427–29. doi: 10.1111/j.1423-0410.1998.tb05452.x. [DOI] [PubMed] [Google Scholar]
- 18.Dzik WH. Emily Cooley Lecture 2002: transfusion safety in the hospital. Transfusion. 2003;43:1190–8. doi: 10.1046/j.1537-2995.2003.00523.x. [DOI] [PubMed] [Google Scholar]
- 19.Serious Hazard of Transfusion: annual report 2004. Available at: http://www.shotuk.org/
- 20.Leape L. Error in medicine. JAMA. 1994;272:1851–7. [PubMed] [Google Scholar]
- 21.Reason J. Human Error. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- 22.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err Is Human: Building a Safer Health System. National Academy Press; Washington: 2000. [PubMed] [Google Scholar]
- 23.Cheng G, Chiu DSM, Chung ASM, et al. A novel system to providing compatible blood to patients during surgery: “self service” electronic blood banking by nursing staff. Transfusion. 1996;36:347–50. doi: 10.1046/j.1537-2995.1996.36496226151.x. [DOI] [PubMed] [Google Scholar]
- 24.Cox C, Enno A, Deveridge S, et al. Remote electronic blood release system. Transfusion. 1997;37:960–4. doi: 10.1046/j.1537-2995.1997.37997454025.x. [DOI] [PubMed] [Google Scholar]
- 25.Wong KF, Kwan AMY. Virtual blood banking: a 7-year experience. Am J Clin Pathol. 2005;124:124–8. doi: 10.1309/13CUJ61YRB50B1CT. [DOI] [PubMed] [Google Scholar]