Abstract
Chronic infection of a seminal vesicle cyst is an extremely rare disorder worldwide. To date, only two cases, which were diagnosed initially by the use of contrast-enhanced CT or non-enhanced MR imaging, have been reported in the literature. We report here a case of a 78-year-old man with chronic infection of a seminal vesicle cyst to illustrate the usefulness of the pelvic contrast-enhanced MRI in making a definitive diagnosis of the rare disorder. In addition, a brief review of the relevant literature is presented.
Keywords: Chronic infection, Seminal vesicle, Cyst, Magnetic resonance (MR)
Chronic infection of a seminal vesicle cyst is an uncommon entity that is usually associated with ipsilateral renal agenesis. Due to the nonspecific nature of the associated signs and symptoms, such as pelvic vague pain, the diagnosis of chronic infection of a seminal vesicle cyst is frequently difficult. CT or MR imaging for the cystic entity can be helpful for the diagnosis. To the best of our knowledge, only two cases of the disorder where the initial diagnosis was determined from contrast-enhanced CT or non-enhanced MRI findings have been reported (1-2).Contrast-enhanced MR imaging of the cystic lesion has not been described in the literature. We report here the radiological findings of a seminal vesicle cyst to illustrate the usefulness of pelvic enhanced MR imaging in making this difficult diagnosis.
CASE REPORT
A 78-year-old man presented to an urologist with urinary frequency and nocturia (three or four times per night) for five years, and without a history of vague pelvic pain. A digital rectal examination determined a slight enlargement of the prostate.
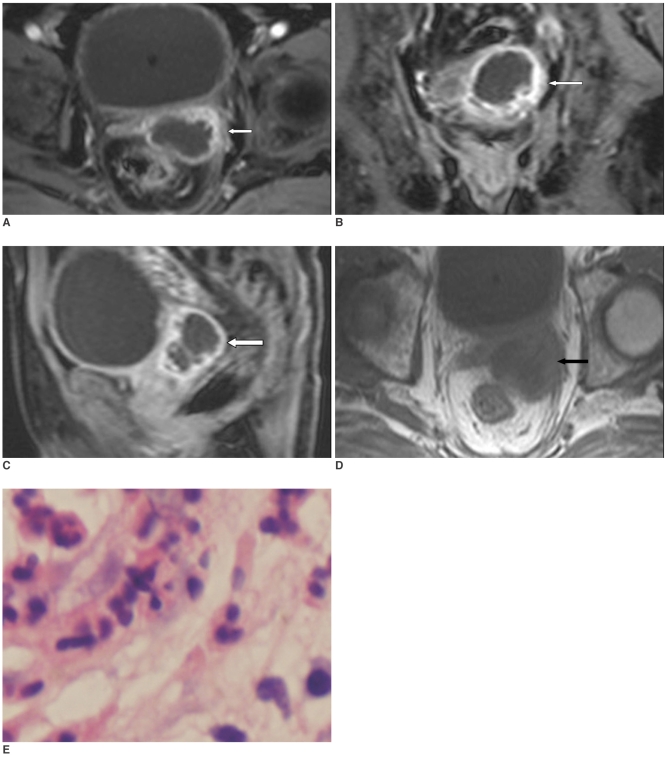
An MRI examination of the pelvis was performed. The study was performed with a 1.5 T MRI unit (Sonata, Siemens Medical Systems, Erlangen, Germany), with three main pulse sequences including a T1-weighted plain scan, a T1-weighted enhanced scan and a T2-weighted scan. Pelvic MR imaging revealed the presence of a cystic softtissue mass in the region of the left seminal vesicle on all views (Figs. 1A-D), which was well visualized and was inseparable from the seminal vesicle. The diameters of the cystic mass were 5.4×3.9×4.2 cm. The cystic lesion had a thick irregular wall. In addition, the cystic wall had low to intermediate signal intensity on T1-weighted images (TR/TE = 510/12) and intermediate to high signal intensity on T2-weighted images (TR/TE = 3900/93), whereas the content of the cystic lesion had low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. On axial, coronary, and sagittal T1-weighted images (TR/TE = 124/2.47, 120/2.47 and 120/2.47, respectively) with intravenous injection of contrast material, enhancement of the cystic wall was marked and inhomogenous; thus, the wall became more apparent. However, the contents of the cystic lesion were non-enhanced. Contrast-enhanced MRI well depicted that the cystic mass encroached upon the left posterolateral urinary bladder wall and the left rectal wall. In addition, the prostate was slightly enlarged with no definite abnormalities.
Fig. 1.
Seminal vesicle cyst infection in 78-year-old man.
A-D. Pelvic MRI demonstrates that cystic wall of lesion in left seminal vesicle is irregularly thick, and it is enhanced markedly and inhomogenous on axial, coronal and sagittal T1-weighted enhanced images (A-C) (white arrows), as compared with depiction on axial T1-weighted image (D) (black arrow).
E. Photomicrography of histological specimen shows inflammatory corpuscles composed of lymphocytes, neutrophilic leukocytes and plasmocytes (×40).
Subsequently, chronic infection of a seminal vesicle cyst was pathologically confirmed initially after transrectal fine-needle aspiration. Microscopy revealed that the cystic lesion was composed of inflammatory granulation tissue, with a histiocytic reaction and the presence of neutrophil granulocytes. The patient underwent a vesiculectomy of the left seminal vesicle with a laparoscope. Laparoscopy provided an excellent visualization of the retrovesical space, and the operative findings were a cystic soft-tissue mass in the region of the left seminal vesicle that invaded the left posterolateral urinary bladder wall and the left rectal wall. The cystic lesion was dissected and removed. From a histological examination, multiple foci of intramural chronic inflammation were demonstrated (Fig. 1E). The patient was then discharged on postoperative day 4.
DISCUSSION
Congenital cysts of the seminal vesicle are related with a developmental anomaly of the mesonephric duct (3). Malformation of the distal mesonephric duct leads to atresia of ejaculatory duct, which eventually results in cystic enlargement of seminal vesicles. However, chronic infection of a seminal vesicle cyst is thought to be caused by inflammatory obstruction within the seminal vesicles (4).
Patients with seminal vesiculitis typically present with vague pain in the lower abdomen, perineum, scrotum, inguina or lower back. Due to the multiplicity of symptoms and low morbidity, the diagnosis of seminal vesiculitis has been frequently difficult (4). Moreover, some seminal vesicle cystic lesions may remain asymptomatic, or may be associated with symptoms related to voiding or prostatitis (5). Thus, the diagnosis becomes more difficult, and seminal vesicle lesions may be discovered only incidentally, as in the present case with our patient with chronic infection of a seminal vesicle cyst.
Imaging techniques, such as vesiculography, CT, transrectal ultrasonography and MRI have allowed the depiction of a possible chronic infection of a seminal vesicle cyst. As most of the above-mentioned procedures can afford a better definition of cyst characteristics, its contents and anatomic relations, the procedures are helpful for diagnosis (5, 6). However, the limitations of vesiculography, CT and transrectal ultrasonography are well recognized. Vesiculography requires general anesthesia, opening of the scrotal sac, and needle puncture of the vas deferens (4). Both vesiculography and CT have potential side effects from radiation exposure to the reproductive ducts and the instillation of iodinate contrast medium. The use of transrectal sonography has limitations in the spatial resolution and soft-tissue contrast, and the use of the transrectal transducer is considered somewhat invasive by some patients (7).
The use of MRI may be superior to the use of the above-mentioned imaging techniques. First, MRI does not have the potential side effects of radiation exposure or allergic response to iodinate contrast medium, and MRI is a noninvasive procedure for the diagnosis of a chronic infection of a seminal vesicle cyst. Second, MRI can provide more information regarding tissue characteristics. For example, fluid content, high protein content or hemorrhage within the cystic lesions can be easily determined by using various pulse sequences.
However, the use of non-enhanced pelvic MRI to image a seminal vesicle disorder is insufficient to provide a reliable diagnosis. Non-enhanced pelvic MRI cannot depict the features of the microcirculation of the cystic wall. On T1-weighted images with intravenous injection of contrast material, enhancement of an infected wall of a seminal vesicle cyst can be marked. In contrast, no enhancement of the non-infected wall of the cyst can be seen on enhanced images. Therefore, it is difficult to discriminate chronic infection of a seminal vesicle cyst from a non-infected cyst using non-enhanced MRI.
In the present case, the patient with chronic infection of a seminal vesicle cyst underwent multiplanar MR imaging with intravenous administration of paramagnetic contrast material. Due to the composition of inflammatory granulation tissue including blood capillaries, the chronic infected wall of the seminal vesicle cyst was enhanced markedly, and had a more sharply defined margin as seen on the enhanced images than as seen on the non-enhanced images. These radiological findings illustrated that the use of enhanced MRI may be superior in demonstrating the features of the cystic wall of the lesion, and the accuracy for detecting chronic infection of a seminal vesicle cyst may be enhanced. In addition, the anatomic relations of the seminal vesicle cyst with chronic infection with other structures were better visualized on T1-weighted enhanced images than on the non-enhanced images. Consequently, the appearances on enhanced MRI permitted effective surgical excision of the left seminal vesicle cyst with chronic infection with a laparoscope, and the patient did recover after the treatment.
In conclusion, we have reported the first documented case of chronic infection of a seminal vesicle cyst that was initially diagnosed using contrast-enhanced MRI. The morphological appearance of the rare disorder on contrast-enhanced MRI is helpful for the definitive diagnosis, and contrast-enhanced MRI is often required to obtain sufficient information prior to making an appropriate therapeutic decision.
References
- 1.Patel PS, Wilbur AC. Cystic seminal vesiculitis: CT demonstration. J Comput Assist Tomogr. 1987;11:1103–1104. doi: 10.1097/00004728-198711000-00046. [DOI] [PubMed] [Google Scholar]
- 2.Maganto E, Fernandez A, Rodriguez JM, Salinas F, Garcia R, Mateos A, et al. Infected cyst of the seminal vesicle associated with malformation of the upper urinary tract and contralateral vesiculitis. Embryonal and clinical aspects. Arch Esp Urol. 1989;42:621–627. [PubMed] [Google Scholar]
- 3.Kenney PJ, Leeson MD. Congenital anomalies of the seminal vesicles:spectrum of computed tomographic findings. Radiology. 1983;149:247–251. doi: 10.1148/radiology.149.1.6611933. [DOI] [PubMed] [Google Scholar]
- 4.Dunnick NR, Ford K, Osborne D, Carson CC, 3rd, Paulson DF. Seminal vesiculography:limited value in vesiculitis. Urology. 1982;20:454–457. doi: 10.1016/0090-4295(82)90482-4. [DOI] [PubMed] [Google Scholar]
- 5.Al-Saeed O, Sheikh M, Kehinde EO, Makar R. Seminal vesicle masses detected incidentally during transrectal sonographic examination of the prostate. J Clin Ultrasound. 2003;31:201–206. doi: 10.1002/jcu.10158. [DOI] [PubMed] [Google Scholar]
- 6.Arora SS, Breiman RS, Webb EM, Westphalen AC, Yeh BM, Coakley FV. CT and MRI of congenital anomalies of the seminal vesicles. AJR Am J Roentgenol. 2007;189:130–135. doi: 10.2214/AJR.06.1345. [DOI] [PubMed] [Google Scholar]
- 7.Carter SS, Shinohara K, Lipshultz LI. Transrectal ultrasonography in disorders of the seminal vesicles and ejaculatory ducts. Urol Clin North Am. 1989;16:773–790. [PubMed] [Google Scholar]