Abstract
Background
Differences in the association of socioeconomic status (SES) with obesity may underlie racial/ethnic disparities in obesity that increase dramatically across the transition to adulthood in the US.
Objective
To examine racial/ethnic differences in the influence of life course SES on longitudinal obesity patterns from adolescence to adulthood.
Methods
Latent class analysis was used on a nationally representative, diverse sample of 12,940 adolescents followed into young adulthood (mean age=21.7 years) to identify life course SES group profiles based on SES data in adolescence and young adulthood. Gender-stratified multinomial logistic regression models estimated the association of SES groups with obesity incidence and persistence versus staying non-obese.
Results
No significant interactions with race/ethnicity were observed, though racial/ethnic minorities had the highest obesity risk across SES groups. Racial/ethnic-pooled associations between disadvantaged SES exposure and higher obesity risk were strong but differed by gender. Males with a disadvantaged background who experienced early transitions into the labor force, marriage and residential independence had the highest risk of obesity incidence (RRR=1.64; 95%CI: 1.12, 2.40), while females exposed to persistent adversity were at highest risk (RRR=3.01, 95%CI: 1.95, 4.66). In general, SES group membership had a stronger relationship with obesity persistence than incidence.
Conclusions
The relationship between SES and obesity patterns is similar across race/ethnicity and differs by gender during the transition to adulthood. However, stronger associations with obesity persistence and enduring racial/ethnic disparities in obesity risk across SES groups suggest that these social factors play a larger role in disparities earlier in the life course.
Keywords: Social class, Minority groups, Obesity, Young adults, US
INTRODUCTION
Higher obesity in US racial/ethnic minorities has been linked to their disproportionate representation in low socioeconomic status (SES) groups.[1, 2] However, the simple inverse relationships between SES and obesity do not necessarily apply in racial/ethnic minorities,[3, 4] suggestive of disparities in the health benefits conferred from high SES due to discrimination.[5, 6] Racial/ethnic disparities in obesity are of particular interest during the transition from adolescence to adulthood, characterized by dramatic obesity incidence and divergent racial/ethnic trends,[7, 8] but have been largely understudied due to challenges in defining SES during this period.
The complex relationship between race/ethnicity, SES and obesity during the transition to adulthood can be better understood using the life course approach, which posits that factors acting early in life accumulate and/or interact with later life factors to influence adult health.[9-11] Parental SES is a reasonable proxy for SES during adolescence, since most offspring are still dependent on their parents at this time point. However, most studies use parental SES as a proxy for SES exposure over the entire transition and thus miss the nuances of inter-generational SES transmission, which may differ by race/ethnicity. Measures of life course SES that combine parental SES in adolescence with the SES the respondents define for themselves as young adults can capture variations in SES exposure of critical importance for obesity development.
A common approach to combining SES information in the life course literature uses a “social mobility” framework, defining groups by their change in SES over time.[12-15] However, the number of groups required to exhaustively represent all combinations of more than one or two SES variables per time point can get prohibitively large for analytic purposes.[16] Thus, although most researchers agree the SES construct comprises multiple dimensions,[17-19] social mobility measures typically are restricted to traditional, single indicators of income, education or occupation at each time point. Although such measures may reasonably capture the SES of parents in the relative stability of middle adulthood, these measures are problematic during the less stable young adult period when misclassification is possible. For example, delayed transitions in schooling or employment may result in misclassification as downwardly mobile, while early transitions into the workforce may lead to misclassification as upwardly mobile.[20]
We examined the relationship of SES with obesity in a racial/ethnically diverse sample of adolescents followed over five years into adulthood. Profiles of SES exposure over this early life course period were identified using latent class analysis (LCA), a model-based technique that defines groups with distinct patterns of responses to multiple observed indicators.[21, 22] This method was well-suited for characterizing a cumulative, multidimensional measure of early adult life course SES based on the young adult’s own social position and the SES of their parents. We hypothesized that there would be racial/ethnic differences in the associations of life course SES groups with obesity development across the transition from adolescence to adulthood due to structural barriers preventing minorities from translating higher SES into health benefits.
METHODS
Study population and design
The National Longitudinal Study of Adolescent Health (Add Health) is a longitudinal, nationally representative, school-based study of U.S. adolescents in grades 7 through 12 in Wave I (1994-1995;), followed with multiple interview waves into young adulthood (Wave III: 2001-2002), and collected under protocols approved by the Institutional Review Board of the University of North Carolina. A sample of 132 high schools and middle schools was selected to be representative of U.S. schools with respect to region of country, urbanicity, school size, school type and race/ethnicity. Adolescents were sampled from school enrollment rosters to participate in detailed, in-home surveys; in Wave I, a parent or guardian was also interviewed. The survey design and sampling frame have been described elsewhere.[23]
The analysis sample was drawn from the pool of young adults interviewed in both Waves I and III with longitudinal, post-stratification sample weights (N=14,322), excluding pregnant (n=292) or seriously disabled (limited in walking one block or having a physical condition that keeps them from working; n=188) respondents at Wave III because of the impact of these conditions on height and weight, as well as those missing data on the longitudinal obesity outcome (n=747) or model covariates (n=155). Our final sample included 12,940 respondents (47% female) comprising four major racial/ethnic groups: non-Hispanic whites (n=7,144), non-Hispanic blacks (n=2,693), Hispanics (n=2,113) and Asians (n=990), aged 18 to 28 years (mean=21.8 years) at Wave III. The excluded sample had a higher proportion of females and blacks.
SES variables
Our desire to capture the inherent multidimensionality of the SES construct and heterogeneity of SES combinations across generations was balanced by convergence difficulties of the latent class model with increasing numbers of items. A large set of indicators reflecting the wide range of parental and young adult SES-related variables measured in Add Health was iteratively reduced to select variables with the potential to influence weight status through intermediate behavioral factors (diet, physical activity), representing three domains of SES that uniquely identify social status: (1) material endowments, including earned and investment income, property and freely exchangeable assets, (2) skills and knowledge, and (3) the status, power and abilities of one’s social network, or material, human and social capital, respectively.[19] We defined 11 indicators of parental SES from parental and adolescent surveys (Wave I) and 14 indicators of young adult SES (Wave III) (see Appendix). Our prior research guided the inclusion of variables of particular relevance to young adulthood (e.g., current enrollment in higher education, social capital and economic hardship).[Scharoun-Lee under review]
Other variables
Obesity Patterns
Measured and self-reported height and weight were available to define obesity in Wave III (young adulthood), whereas only self-reported measures were available for Wave I (adolescence). To maximize sample size and for comparability across waves, we used self-reported values at both time points,[24] which also allowed inclusion of missings due to weight measurement refusal or those in excess of scale capacity. Add Health self-report values correctly classify a large proportion of the respondents.[25] Young adult obesity was defined using the adult BMI obesity cut-point (30 kg/m2).[26] Adolescent obesity was defined using the International Obesity Task Force (IOTF) reference, which statistically links childhood and adolescent BMI centiles to the adult BMI cut-point and provides the only comparative reference data for defining longitudinal obesity patterns across the transition from adolescence to adulthood.[27]
Demographics
Self-designated race/ethnicity from Wave I was used to classify respondents into mutually-exclusive categories of non-Hispanic white, non-Hispanic black, Hispanic and Asian or Pacific Islander, or white, black, Hispanic and Asian. Gender and age (as of last birthday) were self-reported at Wave III.
Statistical analysis
We hypothesized that there would be racial/ethnic differences in associations between life course SES and obesity development because minorities do not experience the same returns as whites on higher SES achievement.[5, 6] We tested this hypothesis by assessing the interaction of race/ethnicity with SES in models of obesity.
Latent class analysis (LCA). LCA was used to identify the number, size and characteristics of latent classes necessary to capture the heterogeneity of cumulative life course SES experience in young adults based on a diverse array of SES traits of the parental household in adolescence (Wave I) and the SES that the young adult created for themselves (Wave III).[28, 29] We used Mplus Version 4.0,[30] correcting for clustering of respondents and using post-stratification sample weights to account for unequal probability of selection.[31]
The final LCA model was selected using several criteria, including: 1.) the visual plot of log-likelihoods of similarly specified models across numbers of classes, selecting models where the log-likelihoods no longer show a substantial improvement in fit [32]; 2.) the Bayesian Information Criterion (BIC), a widely used goodness of fit criterion for comparing models regardless of underlying distribution, with smaller values representing more parsimonious models [33]; and 3.) interpretability of model solution parameters, with attention to the meaningful interpretation of the response profiles for each class, uniqueness of classes and non-triviality of class size.[32, 33] These criteria supported a 5-class model solution, correctly classifying 90 to 95% of individuals in each of the five latent classes. The parameters from this final model solution were used to classify respondents into “life course SES groups” who share a common profile of parental and young adult SES characteristics. For ease of presentation, we used distinguishing characteristics to assign brief labels to these groups, i.e. “persistent disadvantage,” “disadvantage with autonomy,” “material advantage,” “educational advantage” and “highest overall advantage.”
Multivariate modeling of obesity patterns. Multinomial (polytomous) logistic regression models were used to estimate the likelihood of (1) becoming obese (incidence); (2) staying obese (persistence); or (3) becoming non-obese (reversal; n=227, results not shown), relative to (4) staying non-obese associated with life course SES group membership using Stata, version 9.2.[34] Coefficients from these models were exponentiated to obtain estimates of the relative risk ratio (RRR) of each obesity outcome as a function of the SES group.[34] Posterior probabilities of membership in each latent class or “group” were entered into the model as categories of a nominal exposure variable, omitting the most advantaged group (referent).[35] Given gender differences in obesity and the influence of SES on obesity, all models were gender-stratified. Within gender, we assessed effect modification by race/ethnicity to explicitly test for racial/ethnic differences in the association of each SES group with specific obesity patterns. Only significant SES group by race interactions (p<0.10 for Wald test of interaction terms) were retained. Model coefficients were then used to predict age-adjusted obesity patterns for each life course SES category. Survey procedures in Stata were used to correct for unequal probability of selection, underestimation of variance due to clustered sample design, and non-response bias due to attrition from Wave I to Wave III.
RESULTS
Salient characteristics of the five life course SES groups identified using latent class analysis are summarized in Table 1. Findings show the great variation and depth of the life course SES profiles, ranging from “persistent disadvantage,” which was most likely to be economically deprived, coming from poor, single mother households in adolescence and maintaining the cycle of hardship into adulthood, to “highest overall advantage,” which was most likely to have professional, high income, two-parent households in adolescence and the highest education, occupation and financial access in young adulthood.
Table 1.
Brief description of life course SES groups defined using latent class analysis in analysis sample (N=12,940) from Wave I (1994-1995) and Wave III (2000-2001) of the National Longitudinal Study of Adolescent Health
| Life course SES | % (n) | Description |
|---|---|---|
|
Persistent disadvantage Age (yrs): 22.1 Female (%): 45.6 |
17.7 (2,223) | Parental SES
Young adult SES
|
|
Disadvantage with autonomy Age (yrs): 22.1 Female (%): 44.9 |
15.0 (2,057) | Parental SES
Young adult SES
|
|
Material advantage Age (yrs): 21.7 Female (%): 44.1 |
28.5 (3,438) | Parental SES
Young adult SES
|
|
Educational advantage Age (yrs): 21.9 Female (%): 53.2 |
13.8 (1,989) | Parental SES
Young adult SES
|
|
Highest overall advantage Age (yrs): 21.7 Female (%): 59.9 |
25.0 (3,223) | Parental SES
Young adult SES
|
While whites and Asians were most likely to be in advantaged groups, blacks and Hispanics were most represented in “persistent disadvantage” and “disadvantage with autonomy” respectively (Table 2). Obesity incidence exceeded 10% for all except for Asians; persistence was also considerable. Blacks had the highest obesity trends, followed by Hispanics.
Table 2.
Distribution of life course SES groups and obesity characteristics across race/ethnicity in analysis sample (N=12,940) from Wave I (1994-1995) and Wave III (2000-2001) of the National Longitudinal Study of Adolescent Health*
| Race/ethnicity % (SE) |
|||||
|---|---|---|---|---|---|
| Characteristic | Total n=12,940 | White n=7,144 | Black n=2,693 | Hispanic n=2,113 | Asian n=990 |
| Life course SES | |||||
| Persistent disadvantage | 17.7 (1.2) | 13.4 (1.0) | 36.2 (2.6)‡ | 22.3 (2.1)‡ | 7.2 (1.8)‡ |
| Disadvantage with autonomy | 15.0 (0.9) | 12.7 (0.8) | 10.0 (1.0)‡ | 38.5 (3.0)‡ | 18.8 (2.9) |
| Material advantage | 28.5 (1.2) | 31.1 (1.4) | 19.1 (1.1)‡ | 17.3 (1.7)‡ | 25.2 (3.0) |
| Educational advantage | 13.8 (0.5) | 12.4 (0.5) | 24.0 (1.6)‡ | 10.5 (1.1) | 13.6 (1.6) |
| Highest overall advantage | 25.0 (1.8) | 30.4 (2.1) | 10.6 (1.7)‡ | 11.4 (1.6)‡ | 35.1 (3.1) |
| Obesity status† | |||||
| Adolescent obesity | 8.7 (0.4) | 7.9 (0.5) | 12.6 (0.9)‡ | 9.8 (1.1) | 4.0 (1.4)‡ |
| Young adult obesity | 18.3 (0.7) | 16.9 (0.9) | 24.9 (1.5)‡ | 20.3 (1.3)‡ | 11.2 (2.5)‡ |
| Obesity patterns** | |||||
| Obesity incidence (-/+) | 11.4 (0.5) | 10.6 (0.6) | 15.0 (1.2) ‡ | 12.7 (1.1) | 7.7 (1.5) |
| Obesity persistence (+/+) | 6.9 (0.4) | 6.3 (0.5) | 9.9 (0.8)‡ | 7.6 (0.7) | 3.5 (1.3)‡ |
| Obesity reversal (+/-) | 1.8 (0.2) | 1.6 (0.2) | 2.7 (0.5)‡ | 2.2 (0.6) | 0.5 (0.2)‡ |
| Stay non-obese (-/-) | 79.9 (0.7) | 81.5 (0.9) | 72.4 (1.3)‡ | 77.5 (1.5)‡ | 88.3 (2.6)‡ |
Weighted and corrected for clustering
Adolescent obesity assessed at Wave I; Young adult obesity assessed at Wave III
p<0.05 for within-latent class difference between “white” and indicated race/ethnicity
Longitudinal obesity patterns summarized as follows: “-” represents non-obese and “+” represents obese in the format “(Wave I/Wave III)”
We observed no significant interactions between life course SES and race/ethnicity for obesity incidence in males (p=0.38) or females (p=0.60). Racial/ethnic-specific estimates suggest similar conclusions for obesity persistence, but sparse data in Hispanics and Asians precluded statistical interaction assessment across the total sample. However, we observed no significant differences in obesity persistence between blacks and whites (p>0.10), for whom we had sufficient data. Thus, using racial/ethnic-pooled, multinomial logistic regression models, we estimated the relative risk of obesity incidence and persistence versus staying non-obese (outcome referent) for each SES group relative to “highest overall advantage” (exposure referent) (Table 3). We observed strong racial/ethnic-pooled associations between “disadvantaged” life course SES experiences and higher obesity risk, though the nature of high-risk disadvantage differed by gender. “Disadvantage with autonomy” was the only group significantly associated with higher risk of obesity incidence for males (RRR=1.64; 95%CI: 1.12, 2.40), whereas, for females, the estimates for all groups excluded the null, with strongly positive associations for the “persistent disadvantage” group. In general, SES group membership had stronger associations with obesity persistence than incidence.
Table 3.
Estimated associations between ‘life course SES” group and obesity patterns from multinomial logistic regression models* in analysis sample (N=12,940) from Wave I (1994-1995) and Wave III (2000-2001) of the National Longitudinal Study of Adolescent Health
| RRR (95%CI)† |
||
|---|---|---|
| Life course SES | Obesity Incidence | Obesity Persistence |
| Males | ||
| Persistent disadvantage | 1.18 (0.82, 1.70) | 1.98 (1.25, 3.15) |
| Disadvantage with autonomy | 1.64 (1.12, 2.40) | 3.02 (1.82, 5.03) |
| Material advantage | 1.31 (0.88, 1.95) | 2.45 (1.61, 3.73) |
| Educational advantage | 1.37 (0.90, 2.11) | 2.51 (1.49, 4.24) |
| Highest overall advantage | 1.00 | 1.00 |
| Females | ||
| Persistent disadvantage | 3.01 (1.95, 4.66) | 3.56 (2.01, 6.30) |
| Disadvantage with autonomy | 2.42 (1.64, 3.58) | 3.71 (2.03, 6.77) |
| Material advantage | 2.58 (1.79, 3.71) | 2.17 (1.19, 3.96) |
| Educational advantage | 1.73 (1.10, 2.73) | 1.69 (0.95, 3.01) |
| Highest overall advantage | 1.00 | 1.00 |
Gender-stratified, age-adjusted multinomial logistic regression models estimating relative risk ratio of obesity incidence (becoming obese from Wave I to Wave III) or obesity persistence (staying obese from Wave I to Wave III) versus staying non-obese (outcome referent) across the transition from adolescence to adulthood associated with membership in each life course SES group versus “highest overall advantage” (exposure referent)
RRR: Relative risk ratio, CI: Confidence interval
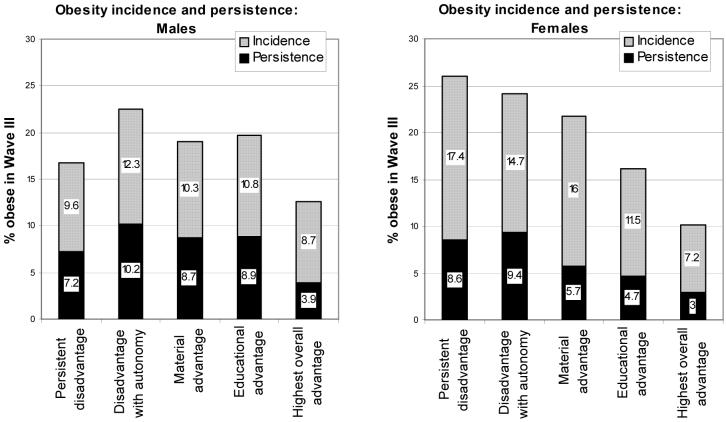
The model results are further illustrated in Figure 1. For males, the “disadvantage with autonomy” group had the highest total obesity, whereas, members of “persistent disadvantage” had the second lowest predicted incidence and persistence. For females, in contrast, membership in “persistent disadvantage” conferred the highest overall risk of young adult obesity, primarily due to substantial incidence.
Figure 1.
Predicted* total young adult obesity, split into incidence and persistence from Wave I (1994-1995) to Wave III (2000-2001) for males (left panel) and females (right panel) from the National Longitudinal Study of Adolescent Health, across life course SES groups
*Coefficients from multinomial logistic regression models estimating relative risk of longitudinal obesity patterns in males and females were used to predict the probability of obesity incidence (becoming obese from Wave I to Wave III) and persistence (staying obese from Wave I to Wave III) for a 22-year old of specified race/ethnicity and life course SES groups, holding all other variables constant.
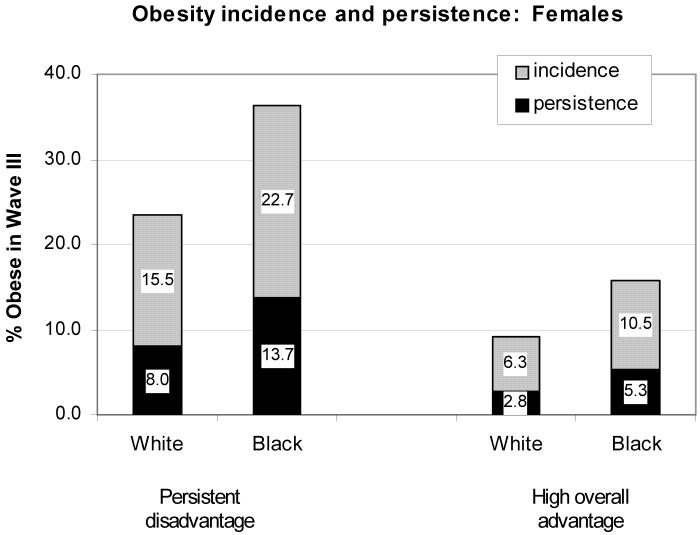
Although a large proportion of both white and black females in the “persistent disadvantage” SES group experienced obesity incidence and persistence across the transition to adulthood, the overall risk for blacks was clearly higher (Figure 2). A similar pattern was seen for the privileged life course SES experience of the “highest overall advantage” group.
Figure 2.
Predicted* longitudinal obesity patterns from Wave I (1994-1995) to Wave III (2000-2001) for white and black females from the National Longitudinal Study of Adolescent Health, across selected life course SES groups
*Coefficients from the multinomial logistic regression model estimating relative risk of longitudinal obesity patterns in females were used to predict the probability of obesity incidence (becoming obese from Wave I to Wave III) and persistence (staying obese from Wave I to Wave III), for a 22-year old female of specified race/ethnicity and life course SES groups, holding all other variables constant.
DISCUSSION
Using latent class analysis in US adolescents transitioning to adulthood, we captured the heterogeneity of cumulative SES exposure in five “life course SES” groups representing distinct profiles of parental and young adult SES. Although we observed a promising absence of racial/ethnic differences in the association of life course SES with obesity development during this period, substantial disparities endured, manifested as a consistently higher burden of obesity in racial/ethnic minorities across SES groups. In the pooled racial/ethnic sample, strongly positive associations between “disadvantaged” life course SES exposure and obesity risk were observed, with variation across gender. Notably stronger associations for obesity persistence versus incidence support an earlier influence of life course SES on obesity development.
We expected racial/ethnic minority respondents would not receive the same health benefits from SES as whites, given the societal discrimination that devalues SES attainment in minorities.[5, 36] Institutionalized racism, in particular, can create structural barriers that restrict the benefits of SES achievements for racial/ethnic minorities.[37] Thus, we hypothesized that societal discrimination would restrict the ability of racial/ethnic minorities to translate advantaged early life course SES into better health. However, based on our findings, we could not reject the possibility that the association between SES and obesity is similar across race/ethnicity. Although our complex measure of early life course SES may have minimized differences in obesity associations by capturing a substantial proportion of the heterogeneity between racial/ethnic groups, the observed similarities in the health benefits of SES across race/ethnicity during the transition to adulthood provides a promising contrast to the literature in adults. The minimal impact of discrimination during this life course stage suggests that this may be an opportune time to halt further widening of racial/ethnic disparities in health.
However, the overall burden of obesity was consistently higher in historically underprivileged racial/ethnic minorities versus whites across several life course SES groups, including those heavily represented by minorities (e.g. “persistent disadvantage”). SES factors captured in our measure may influence racial/ethnic differences in obesity earlier than our baseline adolescent assessment. Furthermore, the stronger relationships for persistence versus incidence in the pooled racial/ethnic sample suggest that SES started influencing the process of obesity development prior to adolescence and helped maintain obesity during the transition, thus supporting a “cumulative” life course framework.[38, 39] We need to look prior to this transitional period to understand the higher rates of obesity in racial/ethnic minorities, supporting the need for early preventive efforts.
Gender differences in the influence of disadvantage on obesity merit further comment. Elevated obesity risk for both sexes growing up in working-poor households and transitioning early into marriage and lower status jobs (i.e. “disadvantage with autonomy”) highlights this SES profile as particularly high risk for all young adults. In contrast, “persistent disadvantage” was associated with strongly increased obesity incidence among females only. Given the influence of maternal SES on weight change in young adult women,[12] it is possible that impoverished single mothers transmit improper weight loss or dieting attempts to their female offspring, resulting in dramatic obesity incidence. A full understanding of the complex dimensions of SES across generations can help identify groups at risk and the timing of effects.
Our study had many strengths, including the use of the complex LCA methodology to classify life course SES exposure, a diverse sample and detailed parental and adolescent data from an understudied life cycle period known for high obesity risk. However, this work was not without limitations. Although posterior probabilities from the LCA model can be used to allocate individuals to their most likely group, the majority of individuals have a non-zero probability of membership in every group identified. Further, individual variability within LCA groups may result in less accurate classifications for a small number of individuals in each group. Timing of measures was another limitation. Since our parental SES indicators were assessed during adolescence and thus could only approximate earlier exposure to socioeconomic conditions, we were unable to fully capture the influence of early SES experiences on obesity development prior to the baseline adolescent assessment. However, our examination of longitudinal obesity patterns did disentangle influences that occur during the transition to adulthood versus before adolescence.
The impact of excluding pregnant females at Wave III on sample selectivity was a concern. SES exposure patterns increased the likelihood of “persistent disadvantage” classification while pregnancy increased the likelihood of “obesity incidence” classification in these excluded females (data not shown). Ultimately, this exclusion reduced the potential for bias due to an artificial inflation of the association between persistent disadvantage and obesity incidence. Furthermore, the excluded pregnant sample did not differ from the analysis sample in racial/ethnic composition, and thus their exclusion was not likely to influence conclusions about disparities. We also considered excluding females with a history of pregnancy before Wave III. Given the weight gain and retention associated with pregnancy,[40-42] females with a history of earlier pregnancy were likely become obese in adolescence and maintain obesity into adulthood. However, results from a secondary analysis (data not shown) suggest that excluding the 25% of females with earlier pregnancies would reduce the precision of estimates and bias our analysis in an unpredictable manner, supporting our original exclusion based on pregnancy at Wave III only.
Overall, we observed an absence of racial/ethnic differences in the association of complex profiles of life course SES with obesity development during the transition to adulthood, a promising contrast to the literature in older adults. However, disparities persisted, manifested in higher obesity trends in racial/ethnic minorities across SES groups. Gender differences in the type of disadvantaged SES exposure most associated with obesity risk underscore the importance of complex characterizations of life course SES for detecting group differences in the study of health. The stronger associations with persistence and enduring racial/ethnic disparities in obesity risk across SES groups suggests that the characteristics captured by these groups play a larger role in disparities earlier in the life course.
WHAT THIS PAPER ADDS
What is already known on this subject?
Racial/ethnic minority adolescents have higher rates of obesity than whites in the US at all levels of parental socioeconomic status (SES), and these disparities increase dramatically across the transition to adulthood.
Little is known on racial/ethnic differences in the combined influence of parental SES and the SES young adults create for themselves on obesity development during this complex, understudied transitional period.
What does this study add?
The cumulative “life course SES” exposure of individuals in the midst of the complex transition to adulthood in the US can be captured in distinct combinations of parental and young adult SES.
Parental family structure and the timing of residential and financial autonomy in young adulthood distinguish subgroups of SES “disadvantage,” with gender differences in the relative influence of these types of disadvantage on longitudinal obesity patterns.
Policy implications
The strong associations of our cumulative early SES measure with obesity do not differ by race/ethnicity, but racial/ethnic disparities in obesity endure, suggesting that we need to look prior to this transitional period to understand the higher rates of obesity in racial/ethnic minorities, supporting the need for early preventive efforts.
However, the minimal impact of discrimination on the health benefits conferred from SES during this life course stage also suggests that this may be an opportune time to halt further widening of racial/ethnic disparities in health.
ACKNOWLEDGEMENTS
This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (www.cpc.unc.edu/addhealth/contract.html).
Funding: This analysis was supported by NICHD (Ruth L. Kirshstein (NRSA) F31-HD049334-01; K01-HD044263). Additional funding came from NIH (R01-HD39183; R01 HD041375), the UNC-CH Center for Environmental Health and Susceptibility (CEHS) (NIH P30-ES10126), the UNC-CH Clinic Nutrition Research Center (NIH DK56350), and the Carolina Population Center.
Appendix
Description of parental and young adult SES variables used in latent class analysis to define life course SES from Wave I (1994-1995) and Wave III (2000-2001) of the National Longitudinal Study of Adolescent Health
| Variable Name | Description | Coding | |
|---|---|---|---|
| Parental SES | |||
| Continuous | Mean | ||
| Household income | Regression imputed family income variablea,b | 0-300, in thousands | 42 |
| Hrs work/wk-Mom | Hrs/week mom works (Wave 1); 0=no mom or no joba | 0-168 | 32 |
| Hrs work/wk-Dad | Hrs/week dad works (Wave 1); 0=no dad or no joba | 0-168 | 30 |
| Binary/Nominal | % | ||
| Two parent HH | Two biological parent householda,b? | 0=no, 1=yes | 0.50 |
| Insurance 12 mo | Have you (parent)had health insurance last 12 months?a | 0=no, 1=yes | 0.81 |
| Parent Pub Assist‡ | # sources Public Assistancea | 0=none, 1=some | 0.29 |
| Social capital‡ | Sum of total social capital varsa | 0=none, 1=some | 0.50 |
| Mom Professional | Is mom a professional? a,b,c | 0= no, 1=yes | 0.24 |
| Dad Professional | Is dad a professional? a,b,c | 0= no, 1=yes | 0.24 |
| Mom ed <HS | Highest mother’s education variablea,b,c | 1=<HS | 0.18 |
| Mom ed HS grad | 2=HS | 0.57 | |
| Mom ed Some college | 3=Some college+ | 0.25 | |
| Dad ed <HS | Highest father’s education variablea,b,c | 1=<HS | 0.18 |
| Dad ed HS grad | 2=HS | 0.53 | |
| Dad ed Some college | 3=Some college | 0.17 | |
| Dad ed Grad/Prof | 4=Grad/prof. school | 0.12 | |
| Young adult SES | |||
| Continuous | Mean | ||
| Personal income | Young adult income using best guess assignment when “don’t know”; truncated at 99th percentile | 0-300, in thousands | 13.6 |
| Years of education | Highest grade/year completed (Wave 3) | 6 to 22 | 13.2 |
| Binary/Nominal | % | ||
| Ever married | # of marriages (Wave 3) | 0=none, 1=1+ | 0.19 |
| Live with parent | Live with parents (Wave 3) | 0=no, 1=yes | 0.41 |
| In school | Currently in college (AA/BA) | 0=not 1=in school | 0.36 |
| Vocational school | Currently in vocational school (Wave 3) | 0=no, 1=yes | 0.24 |
| Savings account | Do you have a savings account (Wave 3) | 0=no, 1=yes | 0.64 |
| Income from family | Do you get income from your family/friends (Wave 3) | 0=no, 1=yes | 0.40 |
| Own residence | Do you own a residence? (Wave 3) | 0=no, 1=yes | 0.12 |
| Credit card | Do you have a credit card? (Wave 3) | 0=no, 1=yes | 0.59 |
| Health insurance | Do you currently have health insurance (Wave 3) | 0=no, 1=yes | 0.76 |
| Hardship‡ | # sources pub assist and hardship (Wave 3) | 0 = none, 1 = 1+ | 0.36 |
| Social capital‡ | # volunteer org and social capital activities (Wave 3) | 0 = none, 1 = 1+ | 0.31 |
| 1=not working | 0.31 | ||
| 2=blue collar | 0.13 | ||
| Job description | Young adult job description (Wave 3) | ||
| 3=sales and service | 0.37 | ||
| 4=manage/prof. | 0.19 | ||
Source data: Parent questionnaire
Source data: In-home questionnaire
Source data: In-school questionnaire
Footnotes
Competing interests: There are no potential or real conflicts of financial or personal interest with the financial sponsors of the scientific project.
Publisher's Disclaimer: Licence statement: “The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in JECH editions and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence (http://jech.bmj.com/ifora/licence.pdf)”.
In accordance with NIH policy, we will deposit our accepted manuscript (not the final published version) into PubMed Central.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999-2004. Jama. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–75. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 3.Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obes Res. 2003;11:121–9. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 4.Kimm SY, Obarzanek E, Barton BA, et al. Race, socioeconomic status, and obesity in 9- to 10-year-old girls: the NHLBI Growth and Health Study. Ann Epidemiol. 1996;6:266–75. doi: 10.1016/s1047-2797(96)00056-7. [DOI] [PubMed] [Google Scholar]
- 5.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Shuey KM, Willson AE. Cumulative Disadvantage and Black-White Disparities in Life-Course Health Trajectories. Research on Aging. 2008;30:200–225. [Google Scholar]
- 7.Gordon-Larsen P, Adair LS, Nelson MC, et al. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr. 2004;80:569–75. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- 8.De Spiegelaere M, Dramaix M, Hennart P. The influence of socioeconomic status on the incidence and evolution of obesity during early adolescence. Int J Obes Relat Metab Disord. 1998;22:268–74. doi: 10.1038/sj.ijo.0800581. [DOI] [PubMed] [Google Scholar]
- 9.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med. 1997;337:1889–95. doi: 10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- 10.Smith GD, Hart C. Life-course socioeconomic and behavioral influences on cardiovascular disease mortality: the collaborative study. Am J Public Health. 2002;92:1295–8. doi: 10.2105/ajph.92.8.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuh D, Ben-Shlomo Y, Lynch J, et al. Life course epidemiology. J Epidemiol Community Health. 2003;57:778–83. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ball K, Mishra GD. Whose socioeconomic status influences a woman’s obesity risk: her mother’s, her father’s, or her own? Int J Epidemiol. 2006;35:131–8. doi: 10.1093/ije/dyi216. [DOI] [PubMed] [Google Scholar]
- 13.Langenberg C, Hardy R, Kuh D, et al. Central and total obesity in middle aged men and women in relation to lifetime socioeconomic status: evidence from a national birth cohort. J Epidemiol Community Health. 2003;57:816–22. doi: 10.1136/jech.57.10.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennett GG, Wolin KY, James SA. Lifecourse socioeconomic position and weight change among blacks: The Pitt County study. Obesity (Silver Spring) 2007;15:172–81. doi: 10.1038/oby.2007.522. [DOI] [PubMed] [Google Scholar]
- 15.James SA, Fowler-Brown A, Raghunathan TE, et al. Life-course socioeconomic position and obesity in African American Women:the Pitt County Study. Am J Public Health. 2006;96:554–60. doi: 10.2105/AJPH.2004.053447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. BMC Public Health. 2005;5:7. doi: 10.1186/1471-2458-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ball K, Mishra G, Crawford D. Which aspects of socioeconomic status are related to obesity among men and women? Int J Obes Relat Metab Disord. 2002;26:559–65. doi: 10.1038/sj.ijo.0801960. [DOI] [PubMed] [Google Scholar]
- 18.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 19.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–84. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- 20.Shanahan MJ, Porfeli EJ, Mortimer JT, et al. Subjective age identity and the transition to adulthood: When do adolescents become adults? In: Settersten RA, Furstenberg FF, Rumbaut RG, editors. On the Frontier of Adulthood: Theory, Research, and Public Policy. University of Chicago Press; Chicago: 2004. [Google Scholar]
- 21.Lazarsfeld P, Henry N. Latent structure analysis. Houghton-Mifflin; New York: 1968. [Google Scholar]
- 22.McCutcheon AC. Latent Class Analysis. Sage Publications; Beverly Hills: 1987. [Google Scholar]
- 23.Harris K, Florey F, Tabor J, et al. The National Longitudinal Study of Adolescent Health: research design. 2003 Available from: http://www.cpc.unc.edu/projects/addhealth/design.html.
- 24.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring) 2007;15:2357–64. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]
- 25.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–8. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 26.NHLBI Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res. 1998;6(suppl) [PubMed] [Google Scholar]
- 27.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. Bmj. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clogg CC. Latent class models. In: Arminger G, Clogg CC, Sobel ME, editors. Handbook of statistical modeling for the social and behavioral sciences. Plenum; New York: 1995. pp. 311–359. Ch. 6. [Google Scholar]
- 29.Hagenaars J, McCutcheon AC. Applied latent class analysis models. Cambridge University Press; New York: 2002. [Google Scholar]
- 30.Muthen LK, Muthen BO. Mplus User’s Guide. Fourth Edition Muthen & Muthen; Los Angeles, CA: 19982006. [Google Scholar]
- 31.Asparouhov T. Sampling Weights in Latent Variable Modeling. Structural Equation Modeling. 2005;12:411–434. [Google Scholar]
- 32.Nylund KL. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 33.Schwartz G. Estimating the dimensions of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- 34.StataCorp . Stata Statistical Software:release 9.2. Stata Corporation; College Station, TX: 2007. [Google Scholar]
- 35.Pastor DA, Barron KE, Miller BJ, et al. A latent profile analysis of college students’ achievement goal orientation. Contemporary Educational Psychology. 2006;32:8–47. [Google Scholar]
- 36.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;7:322–33. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- 37.Hayward MD, Miles TP, Crimmins EM, et al. The Significance of Socioeconomic Status in Explaining the Racial Gap in Chronic Health Conditions. American Sociological Review. 2000;65:910–930. [Google Scholar]
- 38.Hart CL, Smith GD, Blane D. Inequalities in mortality by social class measured at 3 stages of the lifecourse. Am J Public Health. 1998;88:471–4. doi: 10.2105/ajph.88.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh-Manoux A, Ferrie JE, Chandola T, et al. Socioeconomic trajectories across the life course and health outcomes in midlife: evidence for the accumulation hypothesis? Int J Epidemiol. 2004;33:1072–9. doi: 10.1093/ije/dyh224. [DOI] [PubMed] [Google Scholar]
- 40.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 2000;22:261–74. doi: 10.1093/oxfordjournals.epirev.a018038. [DOI] [PubMed] [Google Scholar]
- 41.Harris HE, Ellison GT, Holliday M. Is there an independent association between parity and maternal weight gain? Ann Hum Biol. 1997;24:507–19. doi: 10.1080/03014469700005272. [DOI] [PubMed] [Google Scholar]
- 42.Linne Y, Barkeling B, Rossner S. Long-term weight development after pregnancy. Obes Rev. 2002;3:75–83. doi: 10.1046/j.1467-789x.2002.00061.x. [DOI] [PubMed] [Google Scholar]